-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Utility of QRS isointegral maps in Left ventricular hypertrophy
Cardiac hypertrophy is an increase in the mass of the heart because of the enlargement of existing muscle fibres. It can be diagnosed in different ways including electrocardiographic body surface mapping. The aim of this paper is to give a brief qualitative and quantitative overview of the QRS isointegral maps in the left ventricular hypertrophy based on our original results as well as on published results. Electrocardiograms were recorded and QRS isointegral maps were constructed using the 24-lead system after Barr in different groups of patients with hypertension and patients with echocardiographically established left ventricular hypertrophy. Values of patients´ map extrema were compared with those of control subjects without cardiovascular diseases and also correlated with selected echocardiographic parameters. Increased as well as decreased values of extrema were found in patients compared to controls. Several extrema correlated well with left ventricular echocardiographic dimensions. In our studies, we found no significant changes of the QRS complex between controls and patients, although the peak-to-peak values increased with increasing left ventricular mass. This is in good agreement with some published data obtained with different lead systems. The disagreement in the results of other papers could be caused by differently defined groups of patients, a different aetiology of hypertrophy, racial differences, the possible influence of obesity, sex, and/or age. Despite these facts, considering both anatomical and electrical remodelling in the left ventricular hypertrophy, electrocardiographic body surface mapping is a useful method for the evaluation of such patients. The obtained detailed information can be valuable in understanding electrophysiological changes and consequences in left ventricular hypertrophy, and current clinical management of patients.
Keywords:
body surface potential mapping, isointegral map, QRS complex, hypertension, left ventricular hypertrophy
Authors: Katarína Kozlíková
Authors place of work: Medical Faculty of Comenius University in Bratislava, Bratislava, SR ; Institute of Medical Physics, Biophysics, Informatics and Telemedicine
Published in the journal: Lékař a technika - Clinician and Technology No. 1, 2015, 45, 21-26
Category: Původní práce
Summary
Cardiac hypertrophy is an increase in the mass of the heart because of the enlargement of existing muscle fibres. It can be diagnosed in different ways including electrocardiographic body surface mapping. The aim of this paper is to give a brief qualitative and quantitative overview of the QRS isointegral maps in the left ventricular hypertrophy based on our original results as well as on published results. Electrocardiograms were recorded and QRS isointegral maps were constructed using the 24-lead system after Barr in different groups of patients with hypertension and patients with echocardiographically established left ventricular hypertrophy. Values of patients´ map extrema were compared with those of control subjects without cardiovascular diseases and also correlated with selected echocardiographic parameters. Increased as well as decreased values of extrema were found in patients compared to controls. Several extrema correlated well with left ventricular echocardiographic dimensions. In our studies, we found no significant changes of the QRS complex between controls and patients, although the peak-to-peak values increased with increasing left ventricular mass. This is in good agreement with some published data obtained with different lead systems. The disagreement in the results of other papers could be caused by differently defined groups of patients, a different aetiology of hypertrophy, racial differences, the possible influence of obesity, sex, and/or age. Despite these facts, considering both anatomical and electrical remodelling in the left ventricular hypertrophy, electrocardiographic body surface mapping is a useful method for the evaluation of such patients. The obtained detailed information can be valuable in understanding electrophysiological changes and consequences in left ventricular hypertrophy, and current clinical management of patients.
Keywords:
body surface potential mapping, isointegral map, QRS complex, hypertension, left ventricular hypertrophyIntroduction
Cardiac hypertrophy is an increase in the mass of the heart because of the enlargement of existing muscle fibres. It may be localized to separate parts of the ventricles or may be diffuse. Ventricular hypertrophy can be divided into concentric or eccentric hypertrophy when the chamber size is normal or dilated, respect-tively. Left ventricular hypertrophy is a compensatory response to a chronically increased workload on the heart. It can be caused by different reasons, for example, pressure or volume overload, coronary artery disease, myocardial fibrosis, mutation in genes [1; 13; 14].
The principal method to diagnose left ventricular hypertrophy is the echocardiography, while the cheapest method is the electrocardiography. The electrocardiographic evaluation is due to electrical remodelling in cardiac hypertrophy that can be connected with prolongation of the action potential duration, which may affect the whole QT interval in the surface electrocardiograms.
Identification of left ventricular hypertrophy using 12-lead electrocardiographic criteria is based primarily on QRS amplitudes in one or more leads (the Sokolow-Lyon index, the Cornell voltage criteria) or includes additional factors such as QRS duration, secondary
ST-T wave abnormalities or left atrial abnormalities (Cornell product, Romhilt-Estes point score) [13]. However, all are limited by poor sensitivity at acceptable levels of specificity. The product of QRS voltage and duration, as an approximation of the time-voltage area (the time-voltage integral) can improve the accuracy of the 12-lead electrocardiography for the evaluation of left ventricular hypertrophy [19]. Nevertheless, there still remain two main limitations of all these criteria:- Only a limited number of leads covering only a small part of the chest is used;
- Increased values of examined parameters in the case of hypertrophy versus cases without hypertrophy are assumed.
Increased as well as decreased voltages and time-voltage integrals were found in multi-lead electrocardiographic measurements – in body surface potential mapping – when the electrodes are placed over the whole chest including back. This non-invasive method offers much more possibilities for qualitative and quantitative data evaluation than does the standard ECG and, therefore, offers more information about the electrical state of the heart. Because of the increased number of sensors, it provides more complete picture of cardiac electric activity, even with details comparable to information obtained from invasive methods.
The aim of this paper is to give a brief overview of the isointegral maps during the complete QRS complex (body surface potential mapping) in left ventricular hypertrophy based on our original results as well as on published results.
Methods
Body Surface Potential Mapping
Electrocardiographic body surface mapping is a non-invasive method enabling the imaging volume distribution of the electric voltage (isopotential maps) and distribution of quantities derived from it (voltage-time integrals – isointegral maps – or times – isochronous maps) on the body surface [8].
The isopotential maps give very detailed information about the electric events in the heart. Their main disadvantage is that a large number of maps (even over one hundred per one QRS complex) have to be constructed and analysed. This can be avoided when using isointegral maps [8] that show the distributions of time integrals of electric voltages on the body surface during a given time interval, in our case the QRS complex (see Fig. 1). When the signal of each lead is integrated over time (areas over the zero isointegral line are taken as positive, areas below the zero isointegral line as negative), it produces a cumulative temporal potential at each spatial location:
where Ii is the voltage-time integral in the i-th location during the time interval [t1; t2] (in our case from the beginning till the end of the QRS complex) and Ui(t) is the electric voltage (potential) [8].
Isointegral maps of the QRS complex (IIM QRS) in healthy subjects (subjects without signs of cardiovascular diseases) display typical features: the upper part of the chest is mainly negative, the lower chest is positive (see Fig. 1 and 2). The zero isointegral line between the positivity and the negativity resembles a (deformed) sinus curve. The minimum is located mainly on the left upper chest, the maximum mainly over the precordium leftward to the minimum. Although these IIM QRS were obtained using a limited 24-lead system after Barr [3], similar patterns were published with different lead systems.
Fig. 1: An example of a QRS isointegral map of a healthy man (top) and a healthy woman (bottom). Each rectangle represents the chest surface; the left half corresponds to the anterior torso, the right half to the back. The border between the light green and the darker green colour corresponds to the zero isointegral line. The step between isointegral lines is 4 mV·ms. 
Echocardiographic Examination
The diagnosis of left ventricular hypertrophy was based on echocardiographic examination using the M-mode [6]. Left ventricular mass (LVM given in grammes (g)) was computed according to the formula:
where IVSDd is the thickness of the interventricular septum, LVIDd is the internal diameter of the left ventricle, LVPWd is the thickness of the left ventricular posterior wall. All values are measured during the diastole and given in centimetres.
The presence of the left ventricular hypertrophy (LVH) was evaluated according the left ventricular mass index (LVMI in g/m2) based on body surface area (BSA) [4; 6; 16]:
According to this criterion (quantitative values may differ as given later) and to the relative wall thickness (RWT - the sum of the septal wall thickness and the posterior wall thickness divided by left ventricular internal diastolic diameter):
patients may be classified into four groups based on the ventricular geometry as follows [4]:
- normal geometry: LVH not present, RWT < 0.45;
- concentric remodelling: LVH not present, RWT ≥ 0.45;
- concentric hypertrophy: LVH present, RWT ≥ 0.45;
- eccentric hypertrophy: LVH present, RWT < 0.45.
Results
In the first mentioned study [12], the electrocardiograms were recorded and body surface maps constructed in 38 patients with essential hypertension (24 men; 50 ± 10 years (y) old, range 25 – 68 y), which were divided into two groups: 15 patients without left ventricular hypertrophy (HT group: 9 men; 48 ± 11 y) and 23 patients with left ventricular hypertrophy (LVH group: 15 men; 51 ± 10 y). Hypertension was defined as prevailing systolic blood pressure exceeding 140 mmHg and/or diastolic blood pressure exceeding 90 mmHg, or antihypertensive therapy lasting for more than three months. Left ventricular hypertrophy was based on the left ventricular mass index: LVMI ≥ 125 g/m2 in men, LVMI ≥ 110 g/m2 in women [4; 6]. Significantly higher values of evaluated echocardiographic characteristics were obtained for the LVH group than for the HT group [12]. Patients with angina pectoris, myocardial infarction, and/or any conduction disturbances were excluded from this study. Mean maps were recorded and constructed for each examination from single beat maps as described earlier [8]. The patients’ data were compared with 12 control subjects (group C: 5 men; 43 ± 10 y, range 30 – 56 y) with no history of cardiovascular diseases, normal blood pressure, and normal electrocardiographic and echocardiographic findings.
The mean QRS isointegral maps of all evaluated groups revealed a smooth dipolar distribution (see Fig. 2). In the control group, positive time integrals covered the majority of the left anterior chest and the inferior part of the torso with maximum located in the left precordial area. Negative time integrals were in the upper half of the right chest and on the back with minimum located in the left parasternal area, located always higher than the maximum.
Fig. 2: Group mean QRS isointegral maps of the control group, of the HT group and of the LVH group (from top to bottom, respectively). 
In the HT group, the distribution of mean maps was similar, but the positive time integrals covered a smaller part of the chest, mainly the left half. The maxima were located in approximately the same positions as in the controls, but the minimum in the IIM QRS was located rightwards and upwards to the level of the maximum. The zero line between positive and negative time integrals became more vertical. This verticality was stressed in patients with left ventricular hypertrophy, where the whole right chest (anterior and posterior) was negative. Both extrema were at the same horizontal level (the 4th intercostal space). There were no significant differences between the mean absolute extrema of the QRS isointegral maps, although the peak-to-peak values increased with increasing left ventricular mass (see Tab.1).
Tab. 1. Extreme values of IIM QRS (mean ± standard deviation). 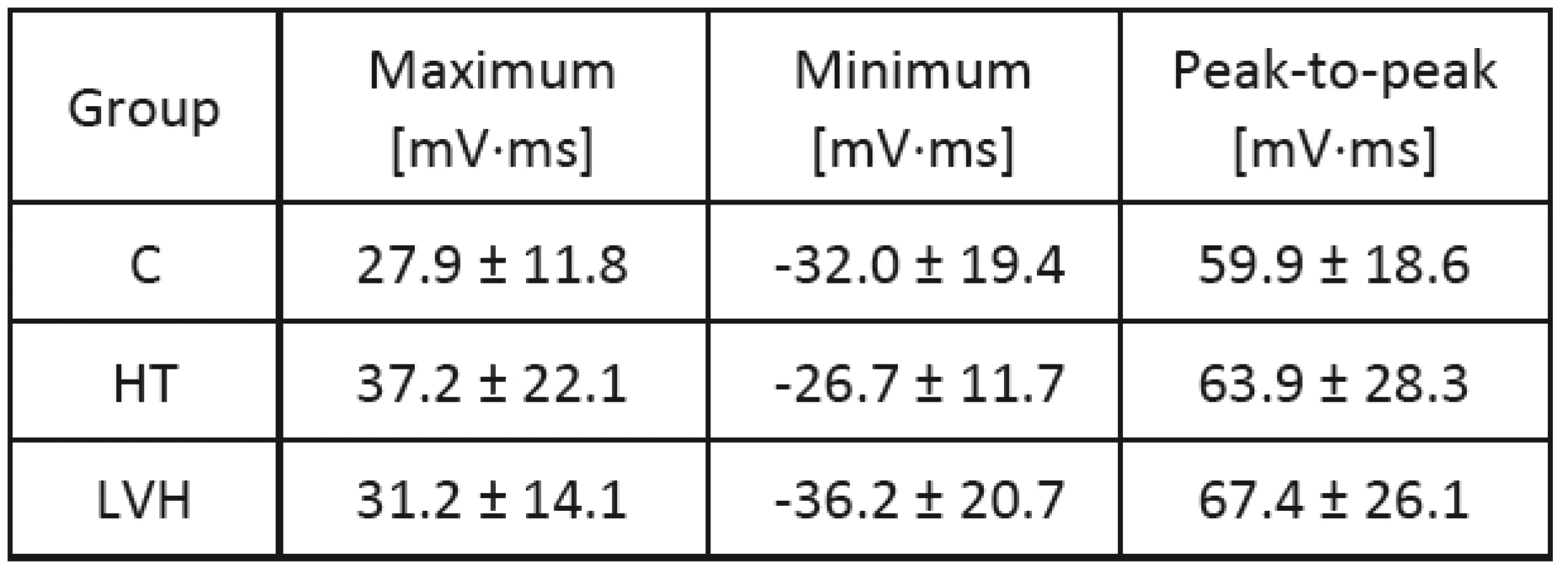
We also studied [10] the extrema of the QRS complex isointegral maps in relation to chosen echocardiographic parameters in a group of 31 hyper-tensive patients with and without left ventricular hypertrophy (age 52 ± 12 y, 12 women). All patients had clinically stated long-time hypertension (systolic blood pressure at least 140 mmHg and/or diastolic blood pressure at least 90 mmHg). Eighteen patients had left ventricular hypertrophy according to the left ventricular mass index [4].
Echocardiographic examinations were done using the M-mode. Following diastolic heart dimensions we measured: thickness of the interventricular septum and the left ventricular posterior wall and the left ventricular internal diameter, all measured during the diastole. We calculated the relative wall thickness, left ventricular mass and the left ventricular mass index as mentioned earlier.
The 24–lead system after Barr was used to record and to construct mean QRS isointegral maps evaluated through 6 to 14 heartbeats according to the heart rate [3; 8]. We used linear regression analysis to correlate the values of maximum, minimum and peak-to-peak values of the mean isointegral maps with selected echocardiographic parameters [9].
The group mean extrema values were [10]: maxima 34.6 ± 17.7 mV∙ms; minima - 28.8 ± 16.2 mV∙ms and peak-to-peak values 63.4 ± 26.9 mV∙ms. Statistically significant regressions of map extrema (in mV∙ms) with echocardiographic parameters (in cm) and the corresponding correlation coefficients (r) are given in Tab. 2.
Tab. 2. Significant correlations between map extrema and echocardiographic parameters in IIM QRS. 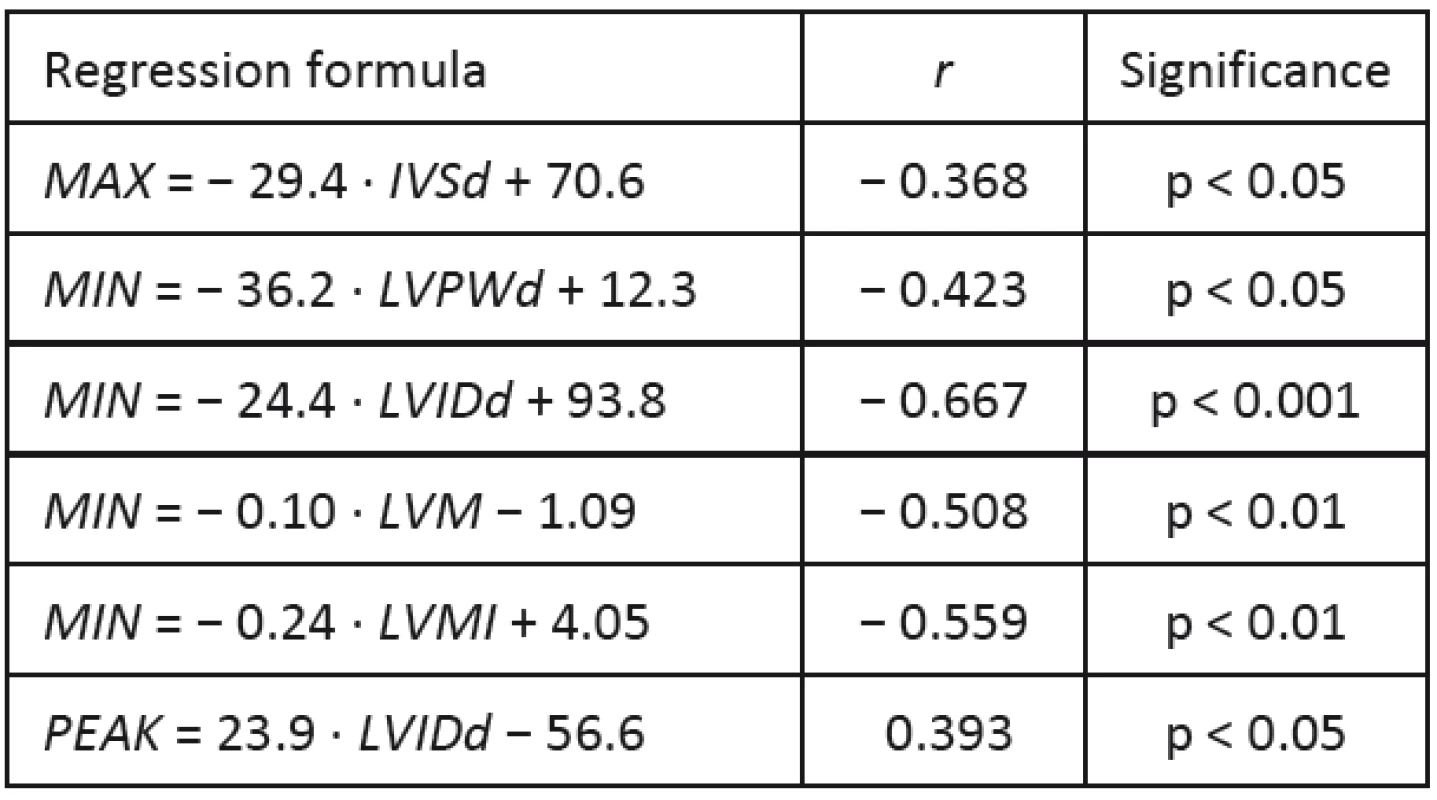
There was no correlation between any of the IIM QRS extrema and the RWT. On the other side, most echocardiographic parameters correlated with the minima. The only correlation of the thickness of the interventricular septum during diastole with the IIM QRS maxima was negative. Best correlation was obtained between the IIM QRS minima and the left ventricular internal diastolic diameter.
In the next study, we examined 33 patients (20 men) with hypertension [11]. From them a subgroup with concentric left ventricular hypertrophy was chosen, which consisted of 12 patients (55 ± 12 years old, 7 men). Their IIM QRS were compared with a control group involving 22 subjects (32 ± 14 years old, 14 men) with no history of any cardiovascular disease and normal 12-lead electrocardiographic findings.
Mean isointegral maps in concentric LVH showed smooth dipolar distributions, but the IIM QRS displayed vertical orientation of zero line and negativities over the left chest with more separated maxima and minima. All extrema of mean maps in left ventricular hypertrophy were always significantly smaller (in absolute value) than those of the control group. We found lower minima (less negative) in concentric left ventricular hypertrophy isointegral maps compared to the controls’ maps.
Discussion
When using isointegral maps instead of isopotential maps, we achieve a great deal of data compression, but at the cost of some information loss, namely the time sequence of activation. On the other hand, we can emphasise those phenomena that would have only low amplitudes (at the noise level) in isopotential maps, but last for longer time.
Regardless the used lead system or mapping device, we can identify common typical characteristics of isointegral maps described by distributions of positive and negative voltage, number of extremes and their values and positions, for example [14; 15]. These parameters may significantly differ for physiological and pathological states.
Isointegral maps of the QRS complex have been used to monitor the physiological ventricular activity in children and in adult population as well as in chosen pathological states or in electric stimulations. In healthy subjects (without signs of cardiovascular diseases) the upper part of the chest is mainly negative, the lower chest is positive (see Fig. 1 and 2). The zero isointegral line between the positivity and the negativity resembles a (deformed) sinus curve. The minimum is located mainly on the left upper chest, the maximum mainly over the precordium leftward to the minimum. Although these IIM QRS were obtained using a limited 24-lead system after Barr [3], similar patterns were published with different lead systems.
Increased and decreased extreme values in isointegral maps were published in patients with increased left ventricular mass in comparison to healthy subjects. The types of included hypertrophies from the geometrical point of view were not discussed there, so both concentric and eccentric hypertrophy could be involved as well as left ventricular remodelling.
Igarashi et al. [7] studied 42 men having essential hypertension (systolic blood pressure over 160 mmHg, and/or diastolic blood pressure over 95 mmHg),
32 – 72 years old, divided into three groups due to increasing left ventricular mass: group A (LVM = 188 ± 20 g), group B (LVM = 247 ± 19 g), and group C (LVM = 373 ± 59 g). They found significantly increased IIM QRS maxima in groups B and C compared to group A and to controls (40 men, 22 – 55 years old). The next studied extrema revealed no significant differences. Because of different left ventricular mass group values it is not possible to compare the published data with our results more exactly. Differences could also be caused by higher blood pressure than in our study and due to sex difference.Corlan and de Ambroggi [5] studied 16 patients with hypertrophy due to aortic stenosis having left ventricular index LVMI = 182 ± 51 g/m2 (LVH: 8 men, 68 ± 13 y). Their maps were compared with 35 controls (C: 25 men, 33 ± 10 y). Significantly increased peak-to-peak values were found in IIM QRS (C: 69.3 ± 26.2 mV∙ms versus LVH: 164.1 ± 68.1 mV∙ms, p < 0.0001). As no data concerning blood pressure were given it is not possible to compare the data more exactly.
Oikarinen et al. [18] studied 42 patients with left ventricular hypertrophy (25 men, 63 ± 12 y; LVM = 344 ± 93 g, LVMI = 181 ± 45 g/m2), among them 27 patients with aortic valve stenosis and 15 with essential hypertension. Their maps were compared with 11 controls (8 men, 55 ± 7 y). The area maps they used were constructed in a different way than in our studies and all the other mentioned studies – Oikarinen et al. took all areas during the QRS complex to be positive, regardless the polarity of the voltage. Therefore, a direct comparison is again not possible, although significant differences between LVH group and control maps were found (higher values in patients).
Ventricular remodelling may cause left ventricular hypertrophy in myocardial infarction patients. This phenomenon was studied by Mozos et al. [17]. Thirty two patients with post-infarction stable chronic heart failure underwent a 64-electrode body surface mapping (isointegral QRS maps) and a 2-D echocardiography. According to the 2D-echocardiography, the mean left ventricular mass was 304 ± 42 g and the left ventricular hypertrophy was present in 50 % patients. Isointegral maxima increased and the minima were more negative in patients with left ventricular hypertrophy (35 ± 16 mV∙ms versus 60 ± 21 mV∙ms, p = 0.0085;
- 25 ± 15 mV∙ms versus - 69 ± 14 mV∙ms, p = 0.0067). Isointegral QRS maxima correlated best with the left ventricular mass (r = 0.73).There are some special features of left ventricular hypertrophy after myocardial infarction considering the myocardial infarction location. Only the opposite side of the myocardium can become hypertrophic (because of remodelling), therefore, not a circular left ventricular hypertrophy develops. Old anterior myocardial infarctions decrease the anterior negative electric potentials on the electrocardiograms and cause secondary posterior wall hypertrophy. Posterobasal necrosis can result in high positive potentials on the anterior chest leads. These different electric effects of the different infarction locations were noticed on the isopotential and isointegral body surface maps [17].
Sobieszczanska et al. [20] studied 43 patients with systemic arterial hypertension (52 ± 8 years old; 29 men). At the beginning of the study, the mean left ventricular mass was 212 ± 13 g with the LVMI < 106 g/m2 for women and LVMI < 114 g/m2 for men taken as normal. The QRS isointegral maps were referred to the corresponding maps obtained from the control group of the 30 healthy age - and gender-matched subjects showing no clinical evidence of cardiovascular impairments using a 87-lead body surface mapping system. The IIM QRS maxima were comparable at the beginning of the study in both groups.
After 4 years, the left ventricular mass increased significantly in 28 patients (252 ± 8 g) and a concentric left ventricular hypertrophy developed. In these patients, significantly higher IIM QRS maxima were found than in those whose left ventricular mass remained at the starting level (214 ± 19 g): 167 ± 12 mV∙ms versus 137 ± 12 mV∙ms. This can be explained by the fact that the hypertrophied left ven-tricle muscle presents the characteristic pathological molecular, cellular, biochemical and functional alter-nations. Structurally changed myocardium generates a stronger cardiac electric field and reveals the distinct conductivity properties with inhomogeneous spread of activation [2].
In our studies, we found no significant changes of the QRS complex between controls and patients, although the peak-to-peak values increased with increasing left ventricular mass. This is in good agreement with some published data [5; 7]. However, we found significantly decreased mean extrema in both HT and LVH groups. The differences between HT and LVH group were not significant.
The disagreement in the results could be caused by differently defined groups of patients, a different aetiology of hypertrophy, racial differences, the possible influence of obesity, sex, and/or age, since all these factors may affect the QRS amplitudes as well as the QRS duration [14]. The different lead systems used may also partially the results.
Conclusion
According to the obtained results we assume that the mass increase of the left ventricle is not enough to increase the electric potential on the body surface during depolarisation. As the obtained results probably display also different heart geometry and different heart-chest geometry, more detailed studies have to be performed including not only the left ventricular mass but also its geometry.
Considering both anatomical and electrical remodelling in the left ventricular hypertrophy, elect-rocardiographic body surface mapping is a useful method for the evaluation of such patients. The obtained detailed information can be valuable in understanding electrophysiological changes and consequences in left ventricular hypertrophy, and current clinical management of patients.
Acknowledgement
The study has been supported by the research grant VEGA No. 1/0727/14 of the Ministry of Education, Science, Research and Sport, Slovak Republic.
Katarína Kozlíková, Assoc. Prof., RN., PhD.
Institute of Medical Physics, Biophysics, Informatics and Telemedicine
Medical Faculty of Comenius University in Bratislava Sasinkova 2, SK 81372 Bratislava, Slovak Republic
E-mail: katarina.kozlikova@fmed.uniba.sk
Phone: +421 259 357 533
Zdroje
[1] Bachárová, L., Estes, E. H. Electrocardiographic diagnosis of left ventricular hypertrophy: depolarization changes. Journal of Electrocardiology, 2009, vol. 42, no 3, p. 228–232.
[2] Bachárová, L., Kyselovič, J. Electrocardiographic diagnosis of left ventricular hypertrophy: is the method obsolete or should the hypothesis be reconsidered? Medical Hypotheses, 2001, vol. 57, no. 4, p. 487–490.
[3] Barr, R. C., Spach, M. S., Herman-Giddens, G. S. Selection of the number and positions of measuring locations for electrocardiography. IEEE Transactions of Biomedical Engineering, 1971, vol. 18, no. 2, p. 125–138.
[4] Bulas, J., Murín, J., Kozlíková, K. Echokardiografická charakteristika hypertrofie ľavej komory srdca. (Echocar-diographic characteristics of left ventricular hypertrophy). Kardiológia/Cardiology, 1998; vol. 7, no. 2, p. 92–98.
[5] Corlan, A. D., De Ambroggi, L. New quantitative methods of ventricular repolarization analysis in patients with left ventricular hypertrophy. Italian Heart Journal, 2000, vol. 1, no. 8, p. 542–548.
[6] Devereux, R. B. Detection of Left Ventricular Hypertrophy by M-Mode Echocardiography. Anatomic Validation, Standardization and Comparison to Other Methods. Hypertension 1987, vol. 9, no. Suppl. II, p. II19–II26.
[7] Igarashi, H., Kubota, I., Ikeda, K. et al. Body surface mapping for the assessment of left ventricular hypertrophy in patients with essential hypertension. Japanese Circulation Journal, 1987; vol. 51, no. 3, p. 284–292.
[8] Kozlíková, K. Povrchové integrálové mapy, ich charakte-ristiky a metódy kvantitatívnej analýzy. (Body surface integral maps, their characteristics and methods of quantitative analysis). Bratislavské lekárske Listy 1990, vol. 91, no. 11, p. 815–823.
[9] Kozlíková, K., Martinka, J. Základy spracovania biomedi-cínskych meraní II. Asklepios, Bratislava, 2009. 204 pp. ISBN 978-80-7167-137-4.
[10] Kozlíková, K., Martinka, J., Bulas, J., Murín, J. QRS complex isointegral maps and left ventricular dimensions. Measurement Science Review, 2003, vol. 3, Section 2, p. 107–110.
[11] Kozlíková, K., Martinka, J., Murín, J. IIM QRS in concentric left ventricular hypertrophy. International Journal of Bioelectromagnetism, 2003, vol. 5, no. 1, p. 199–200.
[12] Kozlíková, K., Martinka, J., Murín, J., Bulas, J. Amplitudes of isointegral maps during ventricular repolarisation in hypertension and left ventricular hypertrophy. Scripta Medica, 2005, vol. 78, no. 5, p. 291–298.
[13] Macfarlane, P. W., Okin, P. M., Veitch Lawrie, T. D., Milliken, J. A. Enlargement and hypertrophy. In: Macfarlane, P.W., van Oosterom, A., Pahlm, O. et al. (Eds.) Comprehensive electrocardiology. Springer, London, 2011, p. 607–649. ISBN 978-1-84882-045-6.
[14] Mirvis, D. M. Electrocardiography: A Physiologic Approach. Mosby-Year Book Inc., St. Louis, 1993. ISBN
0–8016-7479-4.
[15] Montague, T. J., Smith, E. R., Cameron, D. A. et al. Isointegral analysis of body surface maps: surface distribution and temporal variability in normal subjects. Circulation, 1981, vol. 63, n. 5, p. 1166–1172.
[16] Mosteller, R. D. Simplified Calculation of Body Surface Area. New England Journal of Medicine, 1987, vol. 317, no. 17, p. 1098.
[17] Mozos, I., Hancu, M., Jost, N. Isointegral body surface maps and left ventricular hypertrophy in post-infarction heart failure patients. Acta Physiologica Hungarica, 2012, vol. 99, no. 1, p. 19–24.
[18] Oikarinen, L., Karvonen, M., Viitasalo, M. et al. Electrocardiographic assessment of left ventricular hyper-trophy with time-voltage QRS and QRST-wave areas. Journal of Human Hypertension, 2004; vol. 18, no. 1, p 33–40.
[19] Okin, P. M., Roman, M. J., Devereux, R. B. et al. Time-voltage QRS area of the 12-lead electrocardiogram. Detection of left ventricular hypertrophy. Hypertension 1998; 31(4): 937–942.
[20] Sobieszczanska, M., Kalka, D., Jagielski, J. et al. QRS isointegral maps in a follow-up of the patients with hypertensive left ventricular hypertrophy. In: Hiraoka, M., Ogawa, S., Kodama, I. et al. (Eds.) Advances in Electrocardiology. World Scientific, New Jersey, 2004, p. 544–547. ISBN 981-256-107-2.
Štítky
Biomedicína
Článok vyšiel v časopiseLékař a technika

2015 Číslo 1-
Všetky články tohto čísla
- EXPERIMENTAL MODAL ANALYSIS OF ULTRASONIC SURGICAL WAVEGUIDES USING EFFECT OF INVERSE MAGNETOSTRICTION
- Preliminary testing of flexible electrodes for biosignal measurement: abrasion resistance
- Utility of QRS isointegral maps in Left ventricular hypertrophy
- Přístupy ke sledování nákupů zdravotnických přístrojů
- Non-destructive testing of artificial joints with defects by eddy current method
- Lékař a technika
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Přístupy ke sledování nákupů zdravotnických přístrojů
- Non-destructive testing of artificial joints with defects by eddy current method
- EXPERIMENTAL MODAL ANALYSIS OF ULTRASONIC SURGICAL WAVEGUIDES USING EFFECT OF INVERSE MAGNETOSTRICTION
- Preliminary testing of flexible electrodes for biosignal measurement: abrasion resistance
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy







