-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
COST ANALYSIS OF TWO TYPES OF THE LUMBAR SPINE STABILIZING SURGERY
Authors: Martina Caithamlová 1; Markéta Moláková 1; Michal Filip 2; Miroslav Barták 3; Ivo Květ 1; Vladimír Rogalewicz 1
Authors place of work: CzechHTA, Department of Biomedical Technology, Faculty of Biomedical Engineering, Czech Technical University in Prague, Kladno, Czech Republic 1; Department of Neurosurgery, Tomas Bata Regional Hospital, Zlín, Czech Republic and Department of Rehabilition, Faculty of Medicine, University of Ostrava, Ostrava, Czech Republic 2; Department of Addictology, First Faculty of Medicine, Charles University in Prague and General University Hospital in Prague, Czech Republic 3
Published in the journal: Lékař a technika - Clinician and Technology No. 1, 2019, 49, 21-30
Category: Original research
Summary
The study is aimed at quantifying the actual costs related to the MAST (Minimal Access Spine Technique) operative technique with the MIDLF (Midline Lumbar Fusion) instrumentation as compared to the costs related to the classic technique with transpedicular instrumentation complemented with PLIF (Posterior Lumbar Interbody Fusion) in the treatment of a degenerative disc disease in the lumbar spine. The costs were calculated using the Activity-Based Costing method. The total costs for the surgery of one segment amount to CZK 166,371 for MIDLF, and CZK 160,160 for PLIF. The cost difference of CZK 6,210.46 primarily accounts for higher costs associated with separately charged materials consumed in MIDLF. Further, the study pointed out the fact that the actual costs necessary for both operative techniques are underfinanced in terms of reimbursements from the public health insurance system.
Keywords:
spine surgery – MAST – MIDLF – PLIF – costs – Activity-Based Costing
Introduction
In medical terms, lumbar spine surgeries represent interventions with a medium to serious risk level. However, they are also relatively frequent due to the aging population, but also to the general lifestyle trends. A series of causes are associated with lumbar spine disorders from physical wear and tear through injuries to tumors and infections. The problems associated with lumbar spine result in patient´s significantly lower quality of life (including potential reoperations), pain and limited possibilities of participation in the professsional and/or social life. As summed up by Katz [1] or Parker et al. [2], socioeconomic factors are important risk factors for lumbar pain and disability. The total costs of low-back pain in the United States exceed USD 100 billion per year. Two-thirds of these costs are indirect, due to lost wages and reduced productivity. Thus, a greater part of the costs is incurred outside the healthcare system. The surgery may repair either one lumbar spine segment or more segments simultaneously, using several techniques differing from each other in costs and efficiency. Due to the costs arising both in the healthcare sector and outside it, attention should be paid to the costing issues related to lumbar spine stabilizing surgery [3].
As a contribution to the ongoing discussion, the presented study quantifies actual costs associated with two types of lumbar spine operative techniques differing mainly by a different insertion of transpedicular screws into the vertebral bodies of the operated segment (PLIF or MIDLF) applying the Activity-Based Costing (ABC) calculation method. The study focuses solely on the surgery of one segment of the lumbar spine. Real data were obtained from the Tomas Bata Regional Hospital in Zlín (TBRH).
The problem associated with traditional calculation methods is that they do not show the costs actually incurred for a specific healthcare intervention, since they assign indirect costs in the relation to direct costs, but not to their actual consumption. In view of this, an increasing number of hospitals experiment with the ABC calculation method [4–6]. ABC [7] is based on the presumption that resources are consumed by activities to produce outputs or products and services. It focuses on the allocation of indirect costs to products and services, which was traditionally done on an arbitrary basis. ABC is useful in two situations: areas with large and growing indirect costs, and areas with a large variety in products, customers or processes [7]. ABC-based methods in the spine care are recommended e.g. by Kaplan and Haas [8], who claim that accurate cost measurement can be achieved by implementing Time-Driven Activity-Based Costing (TDABC), an approach that helps clinicians identify opportunities to reduce costs of delivering spine care without adversely affecting patient outcomes. Together with value-based healthcare (VBHC), TDABC is presently considered a potential tool for enhancing the cost analysis of healthcare [9]. This study presents our contribution to the discussion about the benefits of the ABC method.
In terms of costeffectiveness analyses, some foreign studies are available examining various economic aspects of the care delivery process in the area of lumbar spine surgery [8, 10–12].
Parker et al. [2] found that spine treatments are on average costeffective, however, they may have a wide variability in costs at the individual patient level. Twitchell et al. [13] analyzed the proportion of various types of costs in 276 patients. Most patients (82.2%) underwent 1-level fusion. Thirteen patients (4.7%) had major complications and eleven (4.1%) had minor complications. The minimally invasive technique (p=0.002), length of stay (p=0.0001), and the number of operated levels (p=0.0001) predicted costs in a multivariable analysis. Supplies and implants (55%) and facility costs (36%) accounted for most of the expenditure.
McGirt et al. [14] concluded that nearly a quarter of interventions performed in 2010–2014 used minimally invasive technologies within a representative sampling registry of elective interbody lumbar spine fusion procedures spanning 27 US states. The interbody lumbar fusion was associated with significant and sustained improvements in all measured health domains. When used by a wide spectrum of spine surgeons in everyday nonresearch settings, the use of minimally invasive technologies was associated with reduced intraoperative blood loss, but only a half-day reduction in the mean length of the hospital stay. The minimally invasive surgery was not associated with any improved perioperative safety measures or 12-month outcomes. Although minimally invasive technologies may increase some in-hospital care efficiencies, their clinical outcomes are similar to open surgery [14].
Cost-effectiveness studies included in the review of Lubelski et al. [15] generally supported the hypothesis that there are no significant differences between open surgery and minimally invasive lumbar approaches. However, these conclusions are preliminary because there was a paucity of high-quality evidence. Much of the evidence lacked details on the methodology for modelling, related assumptions, justification of the economic model chosen, and the sources and types of included costs and consequences.
Vertuani et al. [16] compared the situation in the UK and Italy; the minimally invasive approach proved to be dominant to the open surgery, yielding both cost savings and improved health-related quality of life (HRQOL). Cost savings were driven mainly by a shorter length of the hospital stay, reduced blood loss, and fewer complications such as surgical site infections. The total cost saving per procedure was EUR 973 for Italy and EUR 1,666 for the UK, with a HRQOL improvement of 0.04 QALY over 2 years, while the model proved to be robust.
In the clinical perspective, the studied operative techniques (the minimally invasive approach with the MIDLF instrumentation, and the open surgery with transpedicular instrumentation complemented with PLIF) were compared in a series of studies, e.g. [17–21]. In PLIF, screws are inserted into the vertebral body in the lateral medial direction. The screws are placed along the axis of the pedicles of transverse processes and their diameter ranges around 6.5 mm. This method provides greater mechanical stability than MIDLF, and, therefore, it is often used with younger patients. In MIDLF, screws are placed into the vertebral body in the medium lateral direction. Spondylolisthesis surgeons use it more with older patients, and it is considered an alternative to the classic open surgery for some diagnoses. Unlike the classic open transpedicular stabilization, the main advantage of this technique is a safer way of inserting short screws into vertebral bodies thanks to the medium lateral trajectory in the direction from the spinal canal and a less invasive surgical access. It saves paravertebral muscles and neurovascular structures in the vicinity of the upper joint process of the operated segment. The patient should profit from reduced blood loss during the surgery and less pain in the postoperative period. This should lead to the patient’s shorter hospital stay with more intensive rehabilitation and a faster return to normal life.
The beginnings of the MILDF instrumentation, which ranks among MAST (minimal access spine technologies), go back to 2011, when Medtronic presented MILDF at the North American Spine Society Meeting. In the same year, this instrumentation was put into clinical practice in the USA. In the Czech Republic, MIDLF is regularly used by the Tomas Bata Regional Hospital in Zlín and the University Hospital Hradec Králové. The first Czech surgery was performed in November 2013 in TBRH. Since 2014, this hospital has served as a MIDLF operative technique teaching centre [22]. Over the period 2013–2017, this technique was used in 54 patients in TBRH, while 65 patients underwent the classic technique surgery.
All the clinical studies conducted to date have only been compiled on a short-term to medium-term basis. A long-term clinical study that would validate the benefits of MIDLF in a long-term perspective and for a larger group of patients is presently still lacking. Such long-term studies are currently in progress [23].
The goal of this study is a quantification of the actual costs related to the MAST (Minimal Access Spine Technique) operative technique with the MIDLF (Midline Lumbar Fusion) instrumentation as compared to the costs related to the classic technique with transpedicular instrumentation complemented with PLIF (Posterior Lumbar Interbody Fusion) in the treatment of a degenerative disc disease in the lumbar spine.
Data set
A singlecentre retrospective observation study comparing the costs of two lumbar spine operative techniques—MIDLF and PLIF—was conducted. The data set incorporated all patients operated on the lumbar spine using the above techniques in TBRH in 2016. Table 1 presents basic data related to both arms of the study. Table 2 lists a detailed summary of complications that may occur for both compared methods. Data from Table 1 and Table 2 served as the main input to the cost calculations.
Tab. 1. Summary comparison of MIDLF and PLIF (TBRH data for 2016). 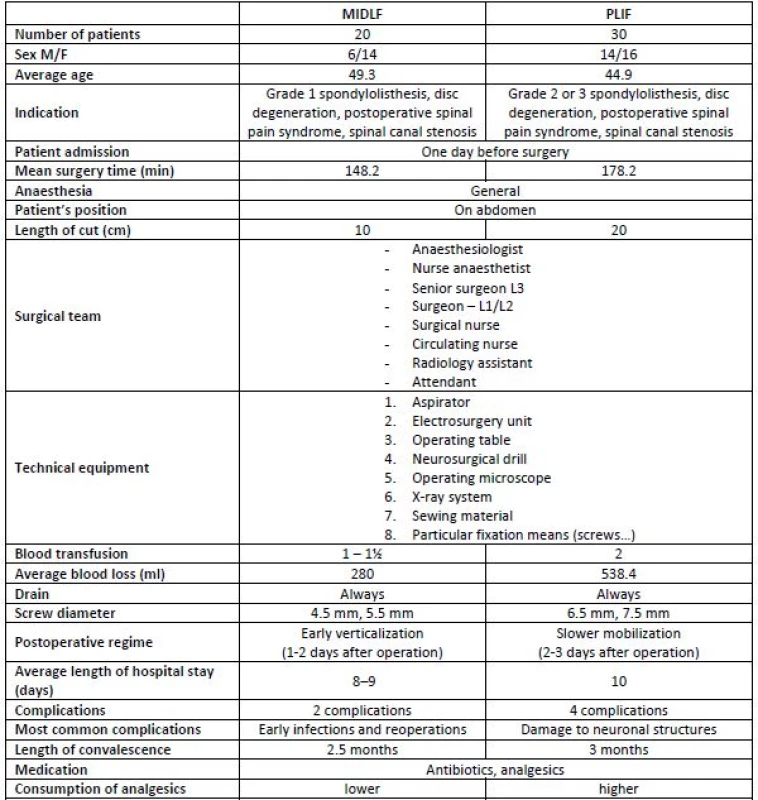
Source: Own processing Tab. 2. Number of complications in TBRH in 2016. 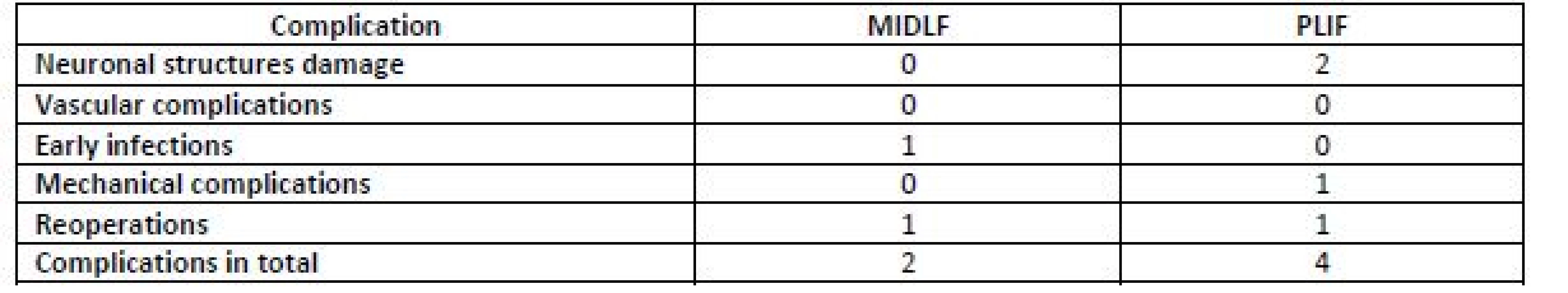
Source: Own processing Methodology: Activity-Based Costing
Activity-Based Costing (ABC) was applied to figure out the actual costs. It is based on assigning costs to individual activities through which the costs can subsequently be assigned to individual cost objects. One of the benefits of ABC is the correct specification of overhead costs and their more accurate distribution according to activities, which leads to acquiring a wide scope of information about costs, interventions, activities, and cost objects, which is further used for the management of costs and restructuring of activities and processes [24]. In simplified terms, the ABC procedure may be summarized into the following steps [25]:
Assignment of indirect costs to individual predefined activities, which occurs on the basis of the cost drivers. Cost drivers specify the cost recalculation from accounting entries to particular activities.
Determination of total costs per particular activities, identification of cost drivers of the activities and quantification of costs per an activity unit.
Identification of costs per cost objects or performances, customers and/or services expressed as costs per an activity unit and the number of these units.
The study started with an identification of costs entering the calculation. These were unit costs directly allocated to the intervention, and all overhead costs. The data were collected mostly from the Neurosurgical Department and Central Operating Theatres of TBRH, some data were also drawn from the hospital infor-mation system, annual reports and financial statements. The costs were subsequently assigned to individual activities; cost drivers of activities were identified, and costs per activity unit quantified. Finally, activity costs were assigned to cost objects.
Results
The following cost classification was chosen:
- Direct costs that can be directly assigned to a particular activity.
- Infrastructure costs, i.e. administration and management costs.
- Indirect costs, i.e. costs relating to the Department, which, however, cannot be directly assigned to an individual activity.
In 2016, the total costs incurred in TBRH were CZK 2,151,843,000. The share of the Neurosurgical Department was CZK 55,134,010 (2.56%). These figures stem from TBRH financial statements and will later enter our calculations.
The basic activities were identified based on expert consultations. The entire process of patient’s passage through the Department is shown in Fig. 1.
Fig. 1. Patient’s passage through the department. Source: Own processing. 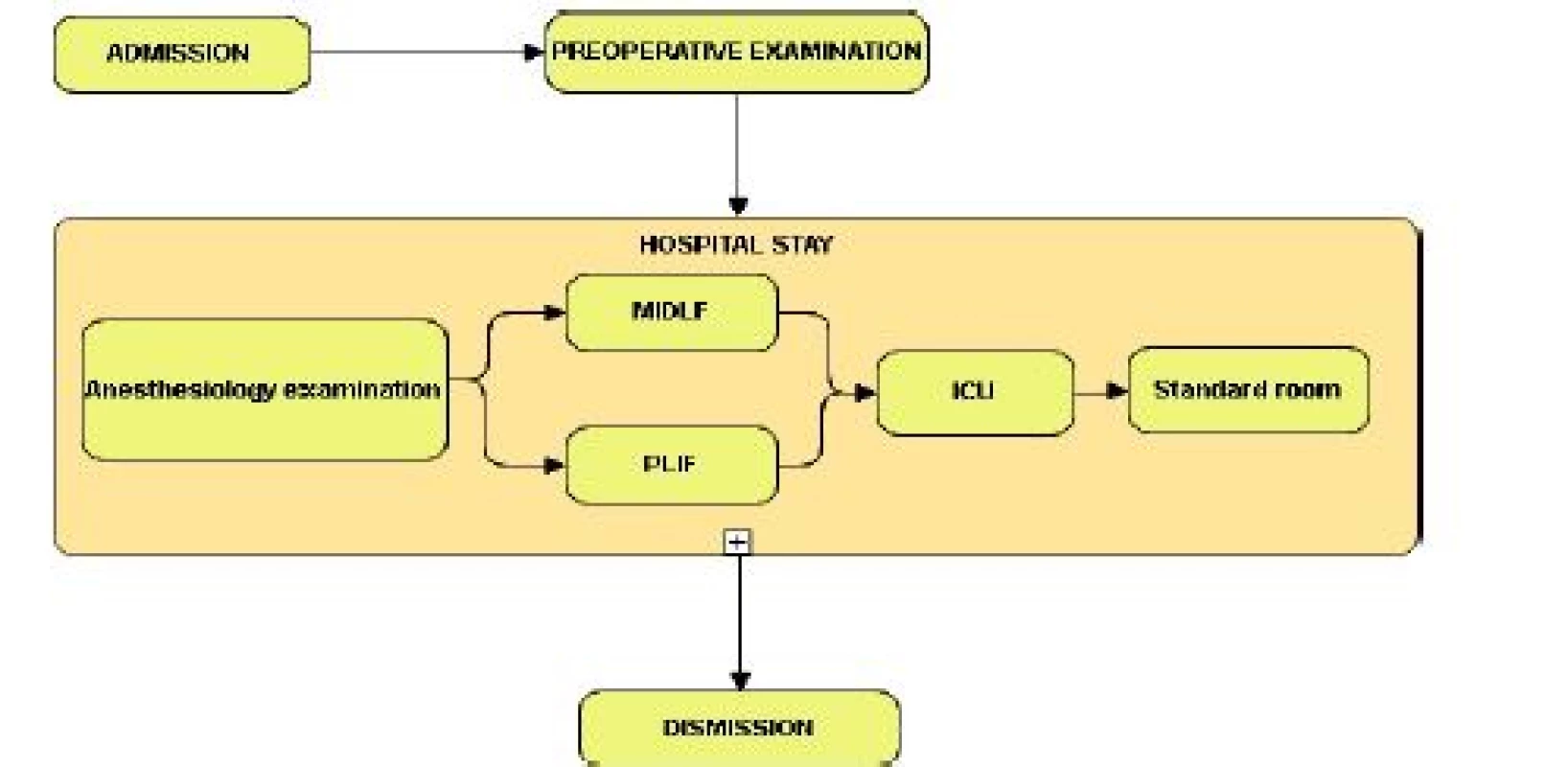
Activity 1 represents patient’s admission. The admission for both considered surgeries is always planned. All necessary preoperation examinations are carried out in the outpatient part of the Department. The corresponding costs are for the most part affected by the total costs of admissions (TC), the total number of patients admitted to the Department per year (TPpY), and the number of patients admitted to the Department for the purpose of undergoing the surgeries considered in this study (TPH). The calculation of these costs was made using the formula (1).
In Activity 2—the preoperative examination—the costs were affected by the total costs relating to the respective activity (TC), the total number of patients at the Department per year (TPpY), and the total number of indicated patients (TPI). The calculation followed a formula analogical to (1).
The hospital stay is described in Activity 3. Patients are admitted to the hospital one day before the intervention. During their stay in the hospital, patients undergo the necessary preoperative and postoperative examinations and care. The hospital stay takes place in a standard ward except for the first one or two days after the surgery when the patients stay in the intensive care unit. The patients are delivered due care by nurses continuously for 24 hours a day (in the cost calculation, a qualified estimate was used to identify the average time spent by nurses with each patient to be 4 hours per day), while the surgeons always check the patient during their planned ward round. Again, the costs of this activity are affected by the total costs relating to the respective activities (TC), but in relation to the total number of bed-days for the whole hospital (TBDH) and for the considered operative technique (TBDOT), i.e. either PLIF or MIDLF. The costs were calculated using the formula (2):
Activity 4 represents the anaesthesiology examination. The calculation followed a procedure analogical to Activities 1 and 2, i.e. applying the formula (1).
Activity 5 is the surgery itself. The preparation of patients for both compared interventions does not differ. The patient undergoes the preoperative preparation where the prevention of the thromboembolic disease must be ensured. This activity costs are affected by the particular identified costs and the surgery time, both for
PLIF and MIDLF. The costs identified within this activity were quantified for one minute of the surgery, and then multiplied by the average surgery time. The costs per surgery also include separately charged materials and separately charged pharmaceuticals (see Table 3).
Tab. 3. Direct costs (separately charged materials and pharmaceuticals). 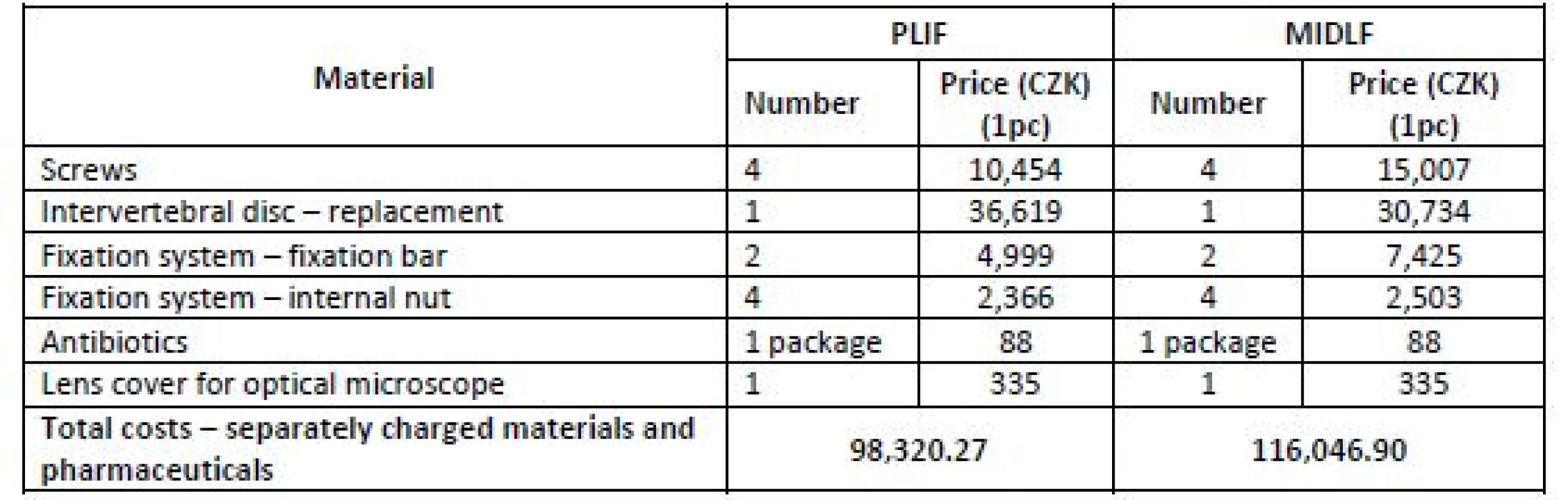
Source: Own processing Activity 6 represents the discharge process. The calculation is again conditioned by the total costs relating to the respective activity, the total number of patients per year and the number of patients for the considered operative technique. The calculation was analogical to activities 1, 2 and 4.
Assignment of costs to activities
In the next step, costs were allocated to individual activities. The activity cost matrix was used that schematically displays the relationships between individual types of costs and activities. Simultaneously, it serves as a tool of the reverse analysis of costs allocated to individual activities performed.
The costs of some type are distributed according to their actual links to individual activities that caused them. This was achieved by using cost drivers (time analysis of work performance, direct assignment, qualified estimate, unit of measurement). Table 4 presents the average duration of individual activities and the number of participating staff. The assignment of infrastructure costs was performed in the same way, i.e. using the activity cost matrix [25].
Tab. 4. Average times of individual activities. 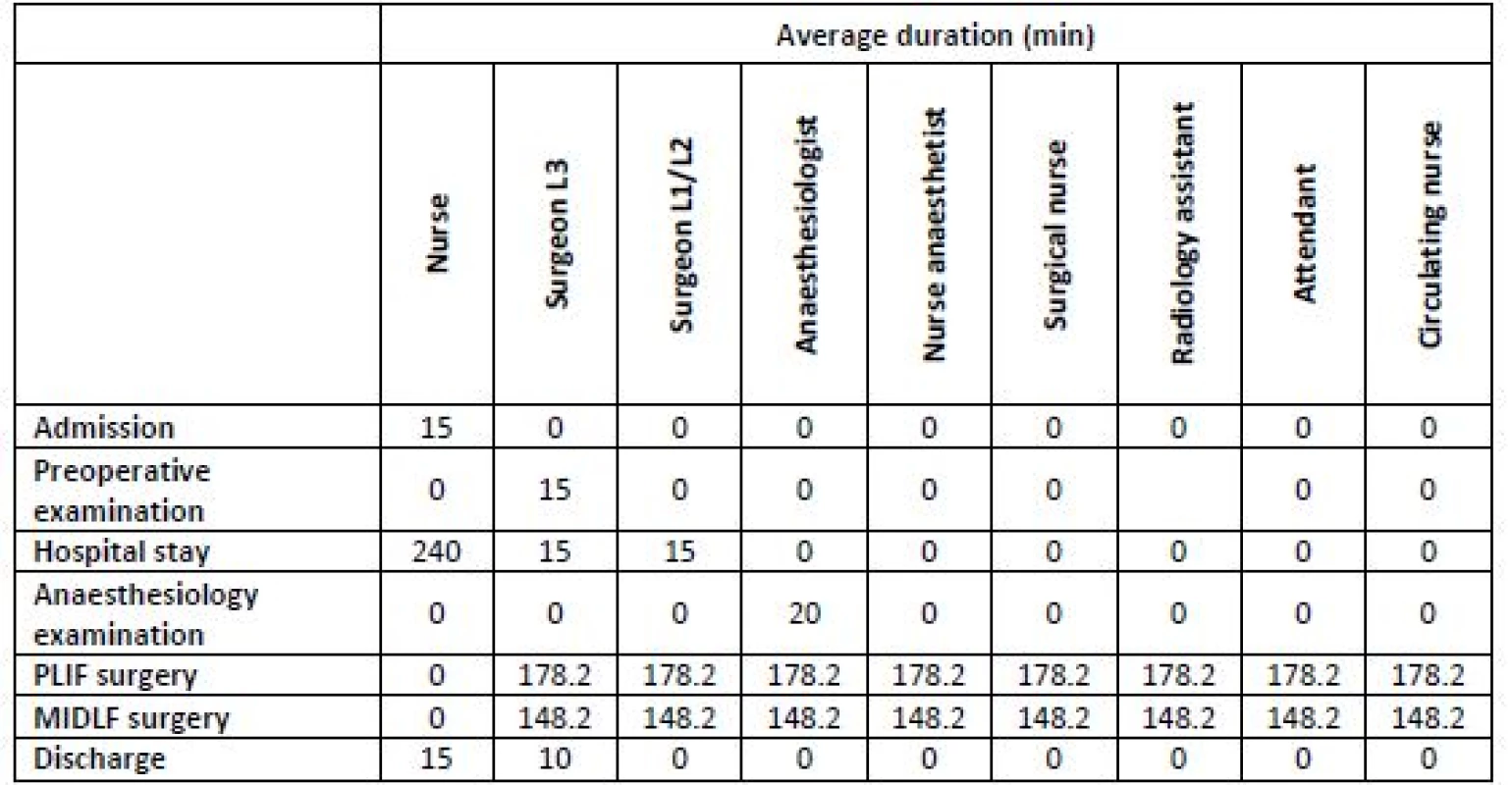
Source: Own processing Quantification of costs per unit of activity
Then the cost drivers of activities were defined. The calculation of costs per an activity unit proceeded using the formula
where CNAi
are the total costs incurred for the respective activity, and MVAi
the output measure of the respective activity. The cost drivers are listed in Table 5.
Tab. 5. List of cost drivers. 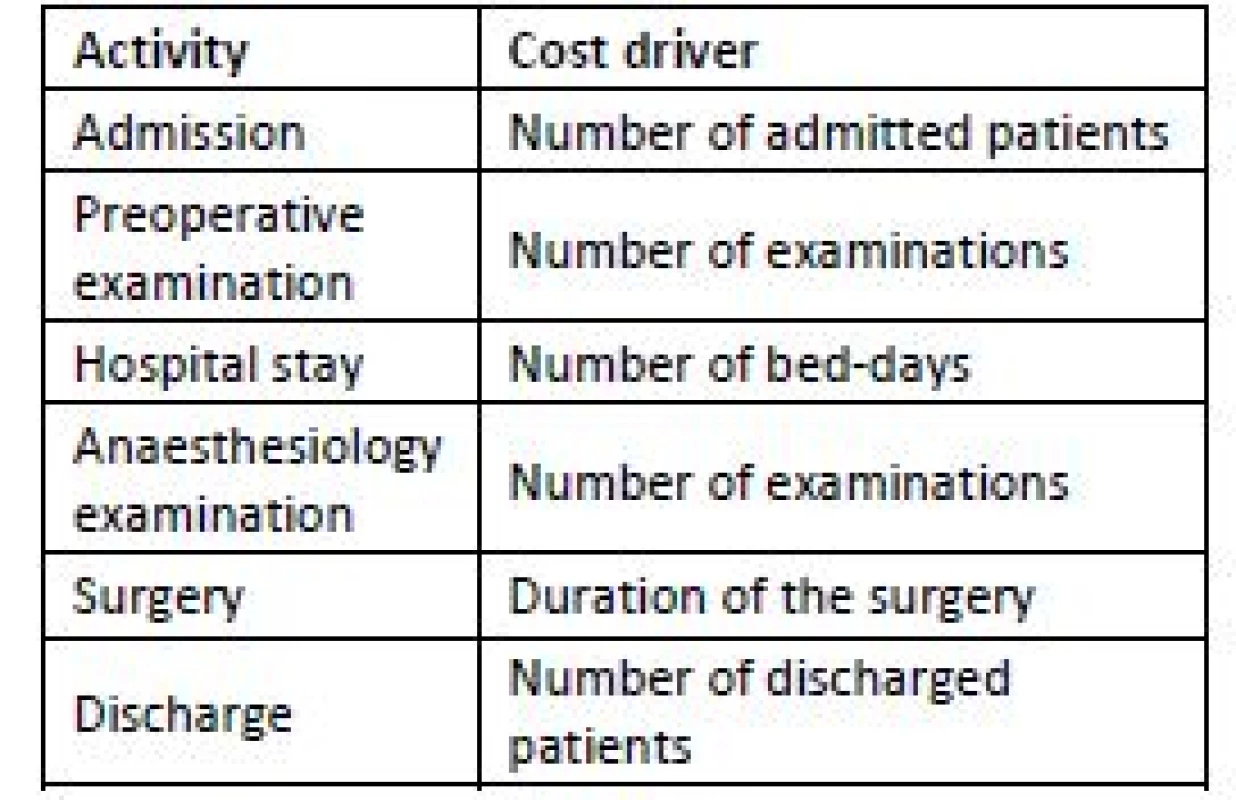
Source: Own processing The calculation of unit costs is presented in Tab. 6.
Tab. 6. Unit costs per activity. 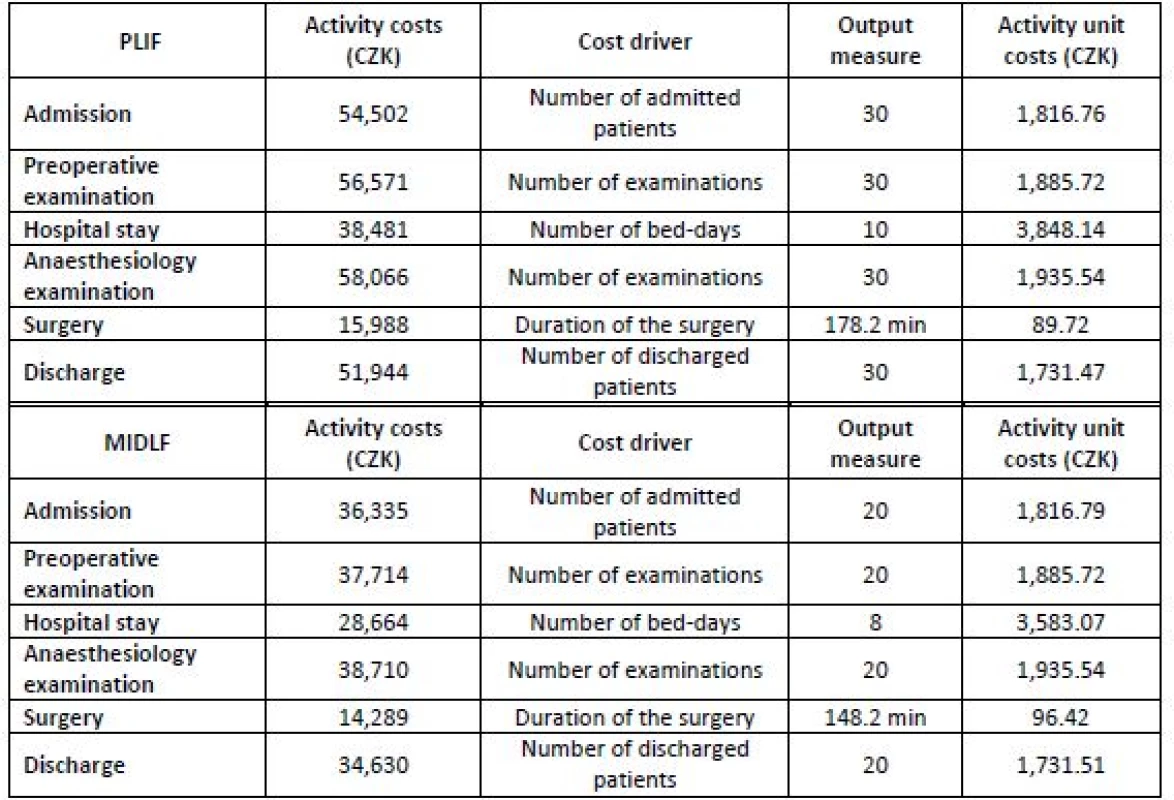
Source: Own processing Assignment of costs to the cost objects
The particular operative technique was always chosen as the cost object. Thus, one cost object is PLIF, and the other cost object is MIDLF. Based on the data from the preceding steps, the total costs of individual operative techniques can be identified (see Table 7).
Tab. 7. Calculation worksheet (one patient). 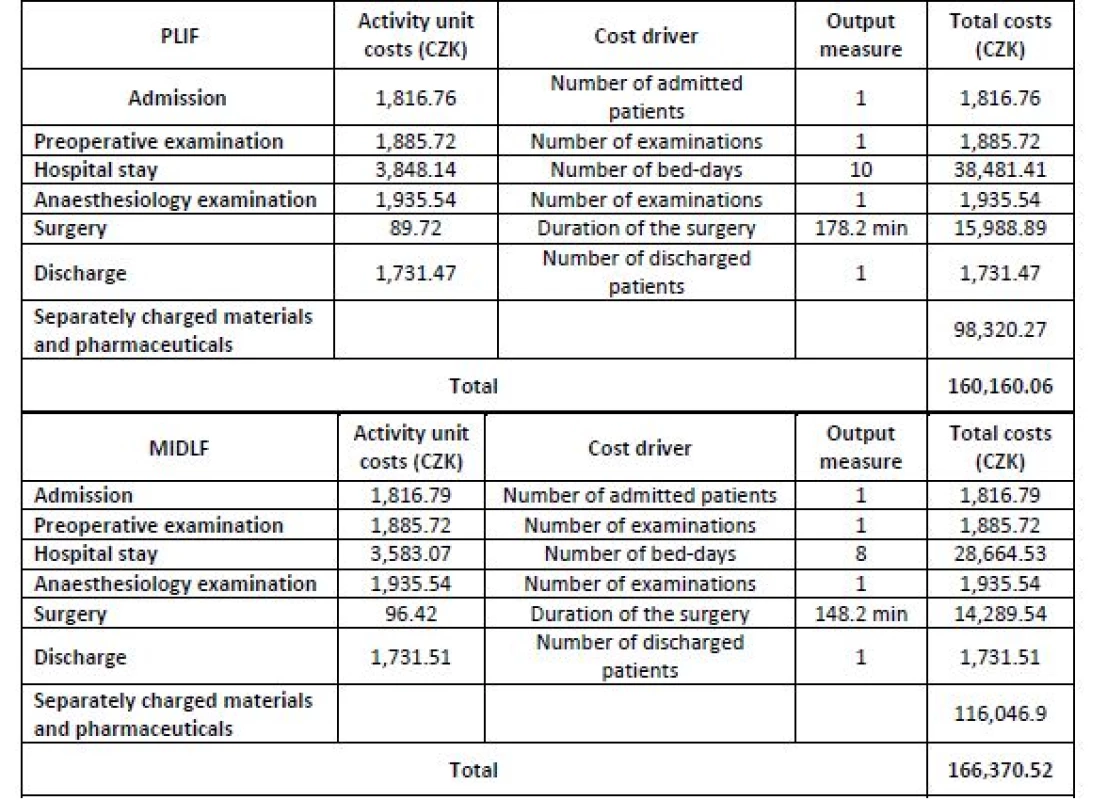
Source: Own processing Finally, the actual costs of the PLIF and MIDLF operative techniques were compared against the reimbursement amount paid by health insurance companies. Although most hospitals are reimbursed using the DRG system in the Czech Republic, TBRH has not used it in the case of spine surgery yet. Thus, the reimbursement has been accomplished based on a combination of the package price and reported care in the form of points. The information on the delivered care was obtained from TBRH calculation worksheets for health insurance companies. It was split into four basic parts: (i) Patient’s category evaluation, where the value in points corresponds to the severity of disability; for both considered operative techniques, the “patient requiring greater supervision” category (evaluated by 150 points) was reported. (ii) Number of days of the hospital treatment, corresponding to 1,203 points in both operative techniques. (iii) The interventions delivered to the patient within the surgery. In the case of MIDLF, this accounted for 18,290 points (=CZK), in the case of PLIF, it was 15,740 points (CZK). (iv) The list of separately charged materials and pharmaceuticals; they are listed in Tab. 8.
Tab. 8. List of separately charged materials and pharmaceuticals reimbursed from health insurance companies. 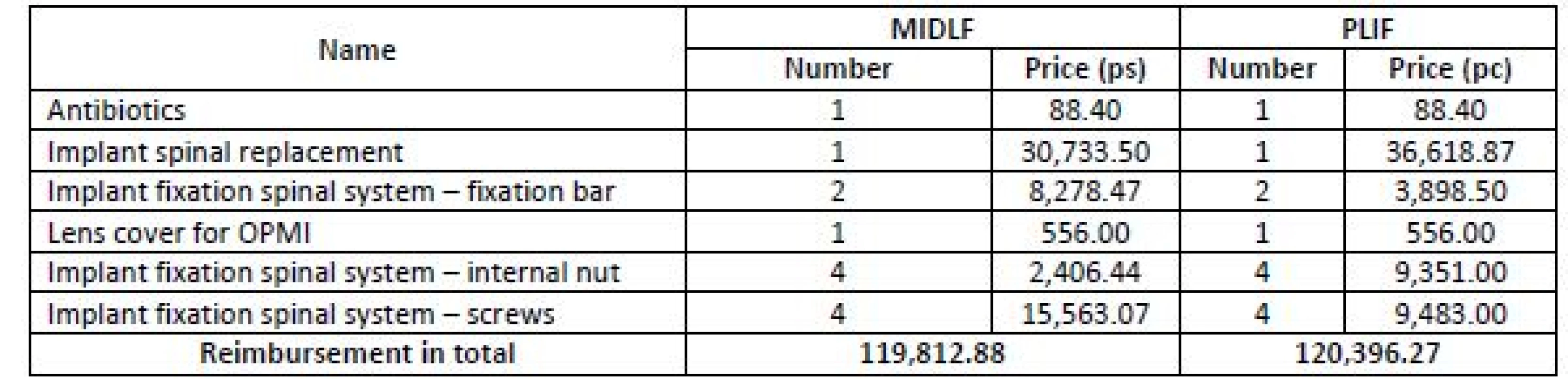
Source: Own processing The total reimbursement from health insurance companies for both operative techniques is presented in Table 9.
Tab. 9. Overview of the total reimbursement from health insurance companies (in CZK). 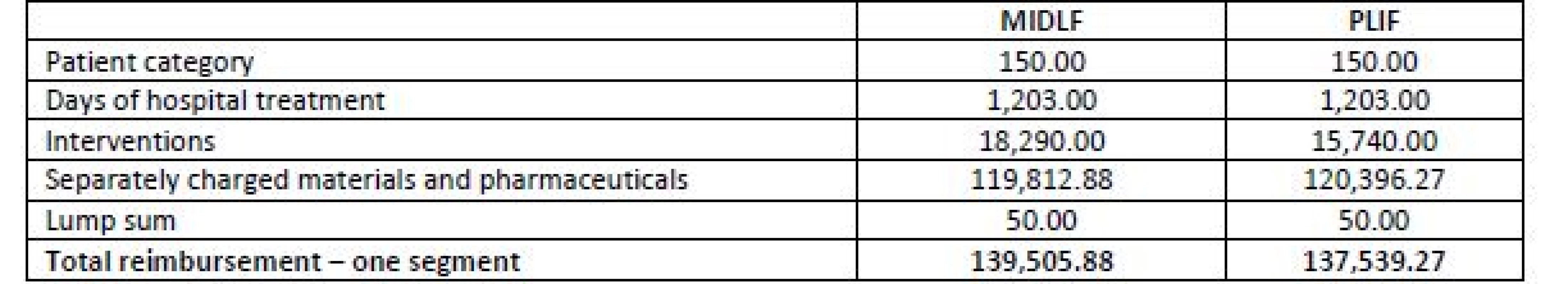
Source: Own processing Subsequently, the actual costs calculated above (Table 7) were compared against the reimbursements from health insurance companies (see Table 10).
Tab. 10. Comparison of actual costs with reimbursements from health insurance companies for an operation of one segment (in CZK). 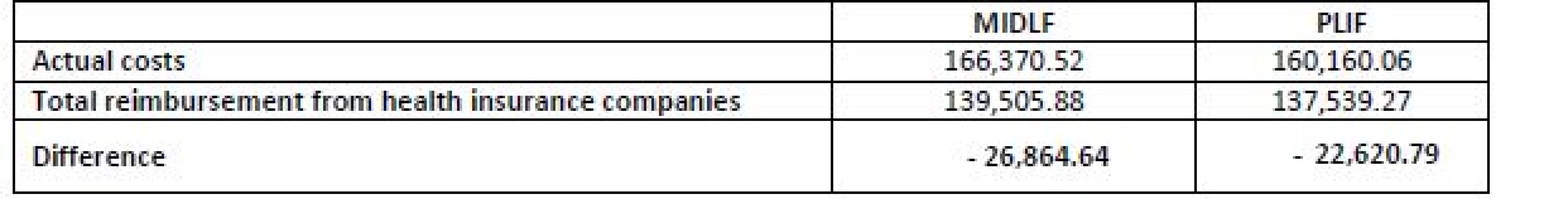
Source: Own processing Discussion
The results imply that MIDLF is by CZK 6,210 more costly than PLIF. The resulting clear difference is primarily caused by the fact that MIDLF incorporates higher costs for separately charged materials. PLIF entails a higher consumption of analgesics and a longer average time of hospital stay, but even so its costs do not exceed the costs of MIDLF. It is obvious from the literature review that the MIDLF technique benefits undoubtedly outweigh the price of the procedure even despite the limitations of its use.
The patients undergoing these surgeries are referred mainly with the following diagnoses:
- grade 1 spondylolisthesis,
- grade 2 spondylolisthesis,
- disc degeneration,
- postoperative back pain syndrome,
- spine stenosis,
where grade 2 spondylolisthesis is not operated using MIDLF, but is only indicated for PLIF due to mechanically stronger anchoring of transpedicular screws. The disorder most frequently indicated for MIDLF is grade 1 spondylolisthesis [17–19].
In TBRH, the mean surgery time for MIDLF ranges around 148 minutes, while for PLIF it is around 178 minutes [14–16]. It must be noted that this time may vary for each patient, particularly in the case of complications substantially extending the duration of the surgery.
Following the surgery performed by any of the operative techniques in TBRH, the patient undergoes a 1–2-day hospital stay at the ICU, being subsequently transferred to the standard ward. The time of discharge home differs by two days on average, where the patients treated by MIDLF are discharged earlier. There is also a difference in the possible time of return to normal life, which again is more favourable for MIDLF. In TBRH, MIDLF has shortened the hospital stay by up to one third.
The costs associated with both operative techniques were calculated for the surgery of one segment of the lumbar spine. The acquired data showed that the health insurance company reimburses TBRH with CZK 137,539 in the case of PLIF, and CZK 139,506 for MIDLF. In both cases, the reimbursement is lower than the actual costs incurred by the hospital; thus, both operative techniques make a loss for the hospital. Consequently, the hospital is forced to cover the uncompensated costs from the resources coming from other interventions that have higher reimbursement from health insurance companies than the real costs.
The limitations of this study must be acknowledged. The results are based on one-year data from a single centre. This was due to the fact that TBRH is the leading hospital providing MIDLF in the Czech Republic, and most MIDLF surgeries done in the Czech Republic in 2016 were recorded in this hospital. Since the surgery costs may differ significantly for individual patients, the sample size is quite small and the results should be verified by a longer and larger research. On the other hand, different sample sizes in both study arms (20 for the MIDLF and 30 for the PLIF) did not seriously affect the resulting average cost estimates. The calculations are based on 2016 prices (i.e. the year of the clinical data collection). No significant changes in costs and reimbursements took place in the Czech Republic since that time; hence, the results (especially the comparisons) can be still considered valid in the end of 2018.
Conclusion
The study has revealed that MIDLF represents a slightly more expensive operative technique than PLIF. The study has further pointed out to the fact that actual costs of both operative techniques are underfinanced in terms of reimbursements from the public health insurance system. The study involved a relatively low number of patients from a single hospital; thus, the results cannot be considered fully conclusive. With a higher number of patients, the fixed costs for individual interventions would be reduced. It would also be desirable to conduct a cost utility study on this topic which would assess the benefits of MIDLF from the patients’ point of view.
Conflict of interest
The authors declare that they are not aware of any conflict of interest related to the presented study.
Martina Caithamlová
Katedra biomedicínské techniky
Fakulta biomedicínského inženýrství
České vysoké učení technické v Praze
nám. Sítná 3105, CZ-272 01 Kladno
E-mail: martina.caithamlova@fbmi.cvut.cz
Phone: +420 224 359 931
Zdroje
- Katz JN. Lumbar Disc Disorders and Low-Back Pain: Socioeconomic Factors and Consequences. JBJS. 2006;88.
- Parker SL, Chotai S, Devin CJ, Tetreault L, Mroz TE, Brodke DS, Fehlings MG, McGirt MJ. Bending the Cost Curve-Establishing Value in Spine Surgery. Neurosurgery. 2017;80:S61-9.
- Allen RT, Garfin SR. The Economics of Minimally Invasive Spine Surgery The Value Perspective. Spine. 2010;35:S375-82.
- Fialova S, Popesko B. Calculations and cost management in Czech hospitals. International Conference on Accounting, Auditing, and Taxation (ICAAT 2014). 2014;145-55.
- Zelman WN, McCue MJ, Glick ND. Financial management of health care organizations: an introduction to fundamental tools, concepts, and applications. 3rd ed. Jossey-Bass. San Francisco; 2009.
- Folland S, Goodman AC, Stano M. The economics of health and health care. 8th ed. Routledge. New York, NY; 2017.
- Oseifuah EK. Activity based costing (ABC) in the public sector: benefits and challenges. Problems and Perspectives in Management. 2014;4 : 581-8.
- Kaplan RS, Haas D. Defining, measuring, and improving value in spine care. Seminars in Spine Surgery. 2018;30 : 80-3.
- Keel G, Savage C, Rafiq M, Mazzocato P. Time-driven activity-based costing in health care: A systematic review of the literature. Health Policy. 2017;121 : 755‑63.
- Fujimori T, Miwa T, Iwasaki M, Oda T. Cost-effectiveness of posterior lumbar interbody fusion in the Japanese universal health insurance system. Journal of Orthopaedic Science. 2018;23 : 299-303.
- Goz V, Weinreb JH, Schwab F, Lafage V, Errico TJ. Comparison of complications, costs, and length of stay of three different lumbar interbody fusion techniques: an analysis of the Nation-wide Inpatient Sample database. Spine Journal. 2014;14 : 2019-27.
- Bydon M, Macki M, Abt NB, Witham TF, Wolinsky JP, Gokaslan ZL, Bydon A, Sciubba DM. The cost-effectiveness of interbody fusions versus posterolateral fusions in 137 patients with lumbar spondylolisthesis. Spine Journal. 2015;15 : 492-8.
- S. Twitchell, Karsy M, Reese J, Guan J, Couldwell WT, Dailey A, Bisson EF. Assessment of cost drivers and cost variation for lumbar interbody fusion procedures using the Value Driven Outcomes database. Neurosurgical Focus. 2018;44.
- McGirt MJ, Parker SL, Mummaneni P, Knightly J, Pfortmiller D, Foley K, Asher AL. Is the use of minimally invasive fusion technologies associated with improved outcomes after elective interbody lumbar fusion? Analysis of a nationwide prospective patient-reported outcomes registry. Spine Journal. 2017;17 : 922‑32.
- Lubelski D, Mihalovich KE, Skelly AC, Fehlings MG, Harrop JS, Mummaneni PV, Wang MY, Steinmetz MP. Is Minimal Access Spine Surgery More Cost-effective Than Conventional Spine Surgery?. Spine. 2014;39:S65‑74.
- Vertuani S, Nilsson J, Borgman B, Buseghin G, Leonard C, Assietti R, Quraishi NA. A Cost-Effectiveness Analysis of Minimally Invasive versus Open Surgery Techniques for Lumbar Spinal Fusion in Italy and the United Kingdom. Value in Health. 2015;18 : 810-6.
- Mizuno M, Kuraishi K, Umeda Y, Sano T, Tsuji M, Suzuki H. Midline Lumbar Fusion with Cortical Bone Trajectory Screw. Neurologia Medico-Chirurgica. 2014;54 : 716-21.
- Bielecki M, Kunert P, Prokopienko M, Nowak A, Czernicki T, Marchel A. Midline lumbar fusion using cortical bone trajectory screws. Preliminary report. Videosurgery and Other Mini-invasive Techniques. 2016;11 : 156-63.
- Dabbous B, Brown D, Tsitlakidis A, Arzoglou V. Clinical outcomes during the learning curve of MIDline Lumbar Fusion (MIDLFA (R)) using the cortical bone trajectory. Acta Neurochirurgica. 2016;158 : 1413-20.
- Rodriguez A, Neal MT, Liu A, Somasundaram A, Hsu W, Branch CL. Novel placement of cortical bone trajectory screws in previously instrumented pedicles for adjacent-segment lumbar disease using CT image-guided navigation. Neurosurgical Focus. 2014;36.
- Linzer P, Filip M, Jurek P, Salek T, Gajdos M, Jarkovsky J. Comparison of biochemical response between the minimally invasive and standard open posterior lumbar interbody fusion. Neurologia I Neurochirurgia Polska. 2016;50 : 16-23.
- Frolová I. Zlínští neurochirurgové učili polské kolegy novou operační metodu [Neurosurgeons from Zlín taught their Polish colleagues a new surgical method] [Internet]. 2015. Available from: http://zlin.cz.
- Medtronic Spinal and Biologics. A Prospective, 5-Year Global Study on MAST™ Minimally Invasive Fusion Procedures for the Treatment of the Degenerative Lumbar Spine (MASTERS-D2). [last updated 2019 Jan 16]. In: ClinicalTrials.gov [Internet]. Bethesda (MD): U.S. National Library of Medicine. 2000. Available from: https://clinicaltrials.gov/ct2/show/NCT026175 63ClinicalTrials.gov Identifier: NCT02617563.
- Popesko B, Novák P. Application of ABC method in hospital management. In: Thomas G, Fleaurant C, Panagopoulos T, Chevassus-Lozza E, Strouhal J, editors. Recent researches in economics and management transformation. Proceedings of the 6th IASME/WSEAS International Conference on Economy and Management Transformation (EMT '11); 2011 Nov 17-19; Angers, France. WSEAS Press; 2011. p. 73–78.
- Popesko B, Novák P, Tučková Z, Fialová Š, Strouhal J. Kalku-lace nákladů ve zdravotnických organizacích [Cost calculation in healthcare facilities]. Wolters Kluwer. Praha; 2014.
Štítky
Biomedicína
Článok vyšiel v časopiseLékař a technika

2019 Číslo 1-
Všetky články tohto čísla
- DESIGN, MANUFACTURE AND TESTING OF RABBIT IMPLANTATION STRUCTURES FOR PRECLINICAL EXAMINATIONS
- APPLICATION OF SENSORY SYSTEMS TO MOVE DOGS WITH VISUAL IMPAIRMENT
- COST ANALYSIS OF TWO TYPES OF THE LUMBAR SPINE STABILIZING SURGERY
- CERAMIC ARCHITECTURES AS MODELS FOR 3D PRINTED TISSUE ENGINEERING APPLICATIONS
- OPTIMIZATION OF ZIRCONIA INKS TO FABRICATE 3D POROUS SCAFFOLDS BY ROBOCASTING
- Lékař a technika
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- OPTIMIZATION OF ZIRCONIA INKS TO FABRICATE 3D POROUS SCAFFOLDS BY ROBOCASTING
- COST ANALYSIS OF TWO TYPES OF THE LUMBAR SPINE STABILIZING SURGERY
- CERAMIC ARCHITECTURES AS MODELS FOR 3D PRINTED TISSUE ENGINEERING APPLICATIONS
- DESIGN, MANUFACTURE AND TESTING OF RABBIT IMPLANTATION STRUCTURES FOR PRECLINICAL EXAMINATIONS
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy






