-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Place and Cause of Death in Centenarians: A Population-Based Observational Study in England, 2001 to 2010
Background:
Centenarians are a rapidly growing demographic group worldwide, yet their health and social care needs are seldom considered. This study aims to examine trends in place of death and associations for centenarians in England over 10 years to consider policy implications of extreme longevity.Methods and Findings:
This is a population-based observational study using death registration data linked with area-level indices of multiple deprivations for people aged ≥100 years who died 2001 to 2010 in England, compared with those dying at ages 80-99. We used linear regression to examine the time trends in number of deaths and place of death, and Poisson regression to evaluate factors associated with centenarians’ place of death. The cohort totalled 35,867 people with a median age at death of 101 years (range: 100–115 years). Centenarian deaths increased 56% (95% CI 53.8%–57.4%) in 10 years. Most died in a care home with (26.7%, 95% CI 26.3%–27.2%) or without nursing (34.5%, 95% CI 34.0%–35.0%) or in hospital (27.2%, 95% CI 26.7%–27.6%). The proportion of deaths in nursing homes decreased over 10 years (−0.36% annually, 95% CI −0.63% to −0.09%, p = 0.014), while hospital deaths changed little (0.25% annually, 95% CI −0.06% to 0.57%, p = 0.09). Dying with frailty was common with “old age” stated in 75.6% of death certifications. Centenarians were more likely to die of pneumonia (e.g., 17.7% [95% CI 17.3%–18.1%] versus 6.0% [5.9%–6.0%] for those aged 80–84 years) and old age/frailty (28.1% [27.6%–28.5%] versus 0.9% [0.9%–0.9%] for those aged 80–84 years) and less likely to die of cancer (4.4% [4.2%–4.6%] versus 24.5% [24.6%–25.4%] for those aged 80–84 years) and ischemic heart disease (8.6% [8.3%–8.9%] versus 19.0% [18.9%–19.0%] for those aged 80–84 years) than were younger elderly patients. More care home beds available per 1,000 population were associated with fewer deaths in hospital (PR 0.98, 95% CI 0.98–0.99, p<0.001).Conclusions:
Centenarians are more likely to have causes of death certified as pneumonia and frailty and less likely to have causes of death of cancer or ischemic heart disease, compared with younger elderly patients. To reduce reliance on hospital care at the end of life requires recognition of centenarians’ increased likelihood to “acute” decline, notably from pneumonia, and wider provision of anticipatory care to enable people to remain in their usual residence, and increasing care home bed capacity.
Please see later in the article for the Editors' Summary
Published in the journal: Place and Cause of Death in Centenarians: A Population-Based Observational Study in England, 2001 to 2010. PLoS Med 11(6): e32767. doi:10.1371/journal.pmed.1001653
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1001653Summary
Background:
Centenarians are a rapidly growing demographic group worldwide, yet their health and social care needs are seldom considered. This study aims to examine trends in place of death and associations for centenarians in England over 10 years to consider policy implications of extreme longevity.Methods and Findings:
This is a population-based observational study using death registration data linked with area-level indices of multiple deprivations for people aged ≥100 years who died 2001 to 2010 in England, compared with those dying at ages 80-99. We used linear regression to examine the time trends in number of deaths and place of death, and Poisson regression to evaluate factors associated with centenarians’ place of death. The cohort totalled 35,867 people with a median age at death of 101 years (range: 100–115 years). Centenarian deaths increased 56% (95% CI 53.8%–57.4%) in 10 years. Most died in a care home with (26.7%, 95% CI 26.3%–27.2%) or without nursing (34.5%, 95% CI 34.0%–35.0%) or in hospital (27.2%, 95% CI 26.7%–27.6%). The proportion of deaths in nursing homes decreased over 10 years (−0.36% annually, 95% CI −0.63% to −0.09%, p = 0.014), while hospital deaths changed little (0.25% annually, 95% CI −0.06% to 0.57%, p = 0.09). Dying with frailty was common with “old age” stated in 75.6% of death certifications. Centenarians were more likely to die of pneumonia (e.g., 17.7% [95% CI 17.3%–18.1%] versus 6.0% [5.9%–6.0%] for those aged 80–84 years) and old age/frailty (28.1% [27.6%–28.5%] versus 0.9% [0.9%–0.9%] for those aged 80–84 years) and less likely to die of cancer (4.4% [4.2%–4.6%] versus 24.5% [24.6%–25.4%] for those aged 80–84 years) and ischemic heart disease (8.6% [8.3%–8.9%] versus 19.0% [18.9%–19.0%] for those aged 80–84 years) than were younger elderly patients. More care home beds available per 1,000 population were associated with fewer deaths in hospital (PR 0.98, 95% CI 0.98–0.99, p<0.001).Conclusions:
Centenarians are more likely to have causes of death certified as pneumonia and frailty and less likely to have causes of death of cancer or ischemic heart disease, compared with younger elderly patients. To reduce reliance on hospital care at the end of life requires recognition of centenarians’ increased likelihood to “acute” decline, notably from pneumonia, and wider provision of anticipatory care to enable people to remain in their usual residence, and increasing care home bed capacity.
Please see later in the article for the Editors' SummaryIntroduction
People aged 100 years or over are a rapidly growing demographic group worldwide. In 2011, centenarians globally numbered 317,000. They are projected to grow to 3,224,000 by 2050, reaching 17,795,000 at the end of the century [1]. In the UK, this group has steadily increased since 1956 with numbers roughly doubling every 10 years [2],[3] and estimated to reach over half a million by 2066 [4]. Throughout Europe women centenarians outnumber men, but with evidence of levelling with comparative gains in male life expectancy [2].
The risk of requiring a care home placement increases with advancing age. In the US, 58% of people aged over 95 years die in a care home; 28% die in hospital [5]. In contrast in the UK, although 51% aged over 90 years require long-term care at the end of life (EoL) (e.g., a care home 40%) [6], only 38% die in a care home while 52% die in hospital [7]. The proportion of hospital deaths in advanced age is similar to the whole population (50%) [8]. A main driver of the cost of end of life care (EoLC) is hospital admission in the last weeks of life, accounting for 33% of the mean total cost per patient [9]. Older people’s preference for place of death is outside of hospital [10] in a “homely” environment characterised by familiarity, autonomy, and presence of loved ones. “Homeliness” is associated with the attributes of the setting and may be a communal facility (e.g., a care home), and not limited to one’s own residence [11]. The EoLC Strategy for England advocates improving EoLC across all care settings, notably care homes, by enhancing the timeliness, responsiveness, and co-ordination of care [12].
Few studies consider the explicit health and social care needs of centenarians [13],[14] compared to younger cohorts of older people or the implications of extreme longevity for policy and service delivery [15]. An important factor in informing EoLC policy and practice is examination of cause of death data as a predictor of place of death using for example death registration data [16]. However, analysing data on centenarians is relatively uncommon. Most studies do not consider those aged 100 years or over as a separate cohort even though their longevity is remarkable. National and international studies have analysed death registration data to inform ageing strategies for the oldest old, but seldom differentiate centenarians within this group [6],[7],[17]–[19] or are disease specific, for example, cancer [20].
No study to our knowledge has considered trends in place of death and associations for centenarians. The increasing trend of extreme longevity for men and women requires detailed investigation to inform policy and service provision [15]. Death registration data in the UK is considered of sufficiently high quality to support policy development and implementation [21]. This study aims to examine trends in place of death and associations for centenarians in England over 10 years to consider implications of extreme longevity for health and social care and variation with cohorts aged 80 to 99 years.
Methods
We carried out a population-based observational study (Checklist S1) [22].
Ethics Statement
Following Office for National Statistics (ONS) procedures a Data Access Agreement was signed detailing data management and protection, and Individual Approvals granted after assessment of researchers accessing the ONS data (YH, WG, and IJH). The study used anonymous records and no ethical approval was required in accordance with the Information Commissioner’s Office guidelines, ONS procedures, and King’s College London Research Ethics Committee.
Data Sources
We used ONS death registration data for England 2001–2010. The database details decedents’ age, gender, marital status, usual residence, place of death and year of death, underlying cause of death, and contributing causes of death (up to 15) using International Classification of Diseases Tenth Revision (ICD-10) [23].
We linked the ONS death registration database with area level data on: deprivation, settlement type of place of residence, and care home bed capacity. The linkage with index of multiple deprivation indices (IMD) 2010 [24] was based on Lower Super Output Area (LSOA) of the decedents’ usual residence. The IMD 2010 is a composite measure of deprivation used at the LSOA level and summarised as quintiles based on national rankings [24]. Settlement type (e.g., urban, town, or village) was generated from usual residential address at LSOA level. Data linkage between ONS place of residence with data from the Care Quality Commission (http://www.cqc.org.uk) identified the number of care home beds (nursing home and residential care homes) per 1,000 population by decedents’ local authority district.
Inclusion Criteria
Inclusion criteria comprised individuals aged ≥100 years at time of death and who died in England between 2001 and 2010 (inclusive) from all causes of death, excluding external causes of accident or violence [23]. For comparison, data from the same timeframe using the same exclusion criteria were included for those who died age 80–99.
Main Outcome
The place of death was grouped into five categories: hospital, nursing home, residential care home, at home, or elsewhere. Care homes provide 24-hour long-term care, categorised in the UK as with nursing (nursing home) or without (residential care home) [25]. Care homes without nursing provide personal care and residents’ health needs and access to specialist services are served by primary health care services, notably general practitioners (physicians in primary care) and community nurses [26],[27].
Explanatory Variables
We examined factors associated with place of death [28]. Explanatory variables were grouped as individual level data: (1) demographic factors (age, gender and marital status, usual residence); (2) illness related (ICD-10 codes for the top eight underlying causes of death and contributing causes of death); and regional level (3) environmental (deprivation, settlement type [e.g., rural, urban], number of care homes per 1,000 population). Detail of usual residence of a decedent is supplied by the informant to the registrar. Since 1993 the informant decides which address to give if more than one is applicable. For example, an informant may consider that the deceased was not resident in a communal establishment (e.g., a care home) where the death occurred and provides a private address to the registrar even though the deceased had lived in the communal establishment for several months [23].
Data Analysis
We used simple linear regression to analyse trends in centenarians’ place of death from 2001 to 2010, place of death and cause of death, and descriptive analysis to explore demographic characteristics, causes of death, contributing causes, and environmental factors (e.g., deprivation indices, died in usual residence). Causes of death were classified as: prominent specific disease types (e.g., pneumonia ICD-10 J12-J118), or disease group (e.g., other respiratory ICD-10 J [others]). Uncommon causes of death were collapsed into “other” (those identified as outside the prominent ICD-10 codes). Prominent groups were entered into the bivariate analysis using frequency tables and descriptive statistics (e.g., proportions and 95% confidence intervals) to explore place of death and variation by gender, marital status, causes of death, number of contributing causes, deprivation, region, and settlement (urban/rural). Findings informed candidate variables for regression modelling on associations with place of death with ten candidate variables grouped as individual level data: (1) demographic; (2) illness; and (3) regional level environmental data. We used multivariable Poisson regression with robust error variance to calculate proportional ratios (PRs) [29], to investigate factors associated with hospital death versus care home (nursing home or residential home), or at home. Age remained in the model as a continuous variable. We report p-values and confidence intervals to enable inferences to centenarian populations outside England and to future centenarian cohorts. We checked residuals to test model specification [30]. We used descriptive analysis to compare cause of death and place of death by age from 80 to ≥100 divided into 5 year age bands. All analysis was undertaken using R version 2.15.1 [31].
Results
The number of centenarian deaths per year in England increased by 56% (95% CI 53.8%–57.4%) in 10 years from 2,823 in 2001 to 4,393 in 2010. The 10 year cohort comprised 35,867 people with a median age of 101 years (range: 100–115 years) at time of death, who were mainly women (86.7%) and widowed (85.0%) (Table 1). Areas of highest deprivation had the lowest proportion of centenarian deaths with consequent regional variance by level of deprivation. The north east of England had the lowest proportion of centenarian deaths (4.3%) (Table 1).
Tab. 1. Demographic characteristics of all centenarian deaths in England 2001–2010. 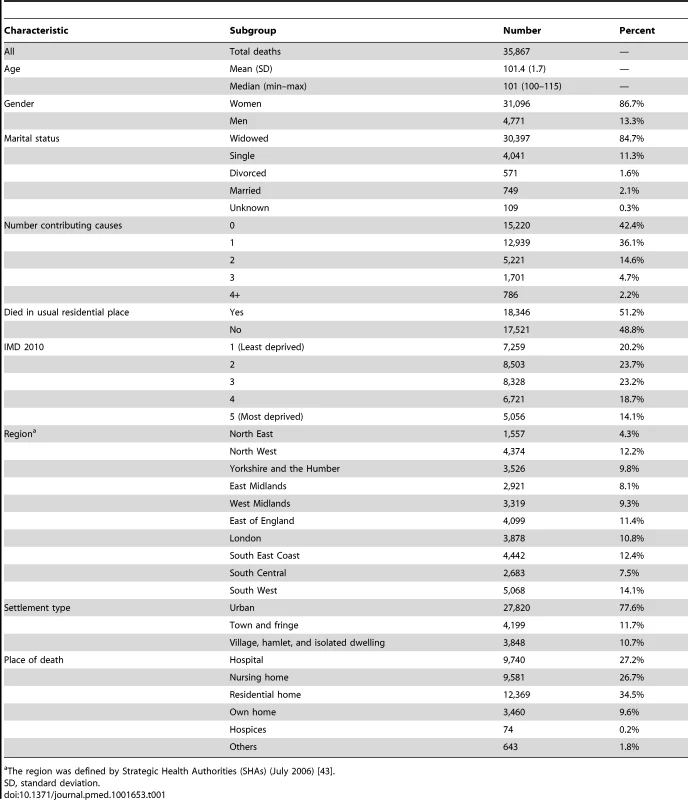
The region was defined by Strategic Health Authorities (SHAs) (July 2006) [43]. Most centenarians died in a residential care home (34.5%, 95% CI 34.0%–35.0%) or nursing home (26.7%, 95% CI 26.3%–27.2%); few died at home (9.6%, 95% CI 9.3%–10.0%) or in a hospice (0.2%, 95% CI 0.2%–0.3%). Over a quarter (27.2%, 95% CI 26.7%–27.6%) died in hospital (Table 1). Nearly half died outside their usual address (48.8%, 95% CI 48.3%–49.4%). Trends in place of death significantly changed in two places: nursing homes decreased (−0.36% annually, 95% CI −0.63% to −0.09%, p = 0.014), but changes in raw numbers were small (n = 845 in 2001; n = 1,118 in 2010); and own home increased (0.24% annually, 95% CI 0.18%–0.29%, p<0.001), but the raw numbers were small (n = 241 in 2001 to n = 463 in 2010) (Figure 1). Little variation was evident in the proportion dying in hospital (0.25% annually, 95% CI −0.06% to 0.57%, p = 0.09) or residential care homes (−0.01% annually, 95% CI −0.19% to 0.17%, p = 0.88).
Fig. 1. Centenarian deaths by place of death 2001–2010 (<i>n</i>, %). Bar number = % proportion. 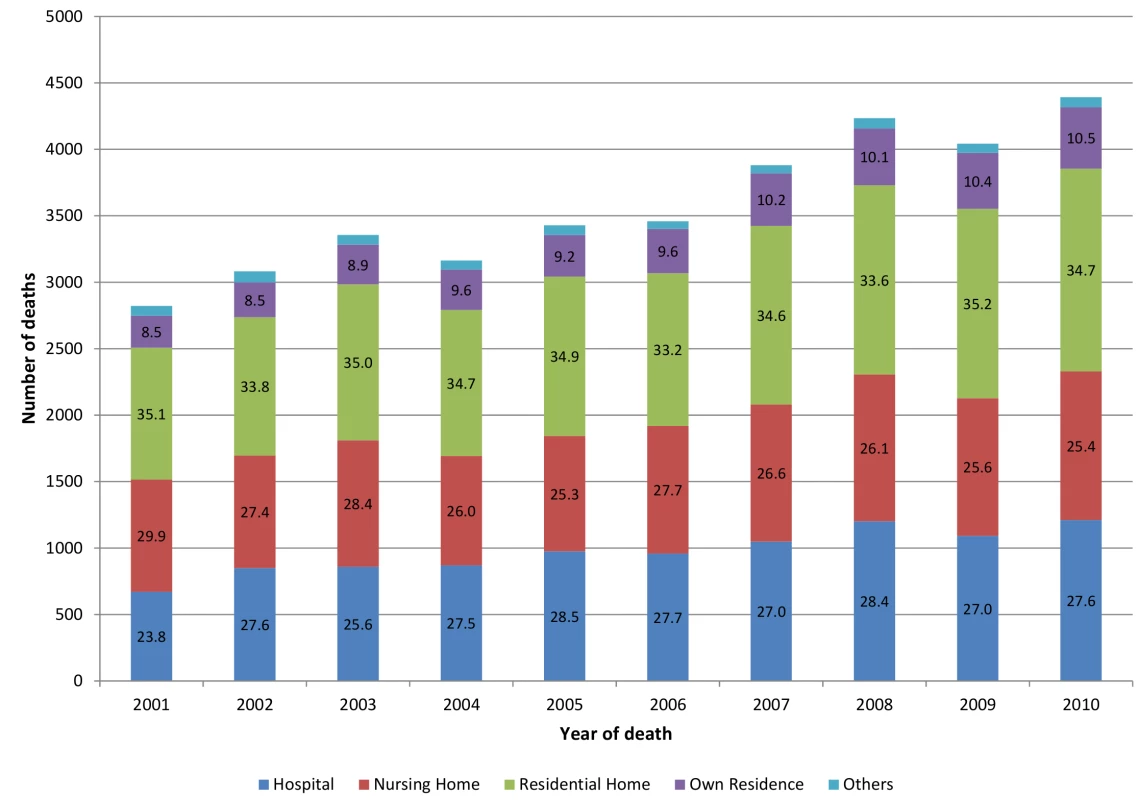
Seven disease groups classified by ICD-10 disease groups accounted for 90.2% (95% CI 89.9%–90.5%) of centenarians’ underlying cause of death with the remainder classified as “other” (9.8%, 95% CI 9.5%–10.1%) (Table 2). The prominent causes of death comprised: pneumonia (17.7%, 95% CI 17.3%–18.1%) and other respiratory diseases (6.0%, 95% CI 8.3%–8.9%); cerebrovascular (10.0%, 95% CI 9.7%–10.3%); ischaemic heart diseases (8.6%, 95% CI 8.3%–8.9%) and other circulatory diseases (9.8%, 95% CI 9.5%–10.1%); dementia and Alzheimer disease (5.7%, 95% CI 5.4%–5.9%); cancer (4.4%, 95% CI 4.2%–4.6%); senility “old age” (28.1%, 95% CI 4.2%–4.6%). “Old age” formed the largest ICD-10 grouping (28.1%, 95% CI 27.6%–28.5%) (Table 2). However, trends in certifying death as “old age” showed a decreasing trend over 10 years, notably in hospital (−0.87% annually, 95% CI −1.09 to −0.65%, p<0.001) with increasing use of dementia (0.34% annually, 95% CI 0.14%–0.54%, p = 0.004).
Tab. 2. Centenarian cause of death by place of death in England 2001–2010. 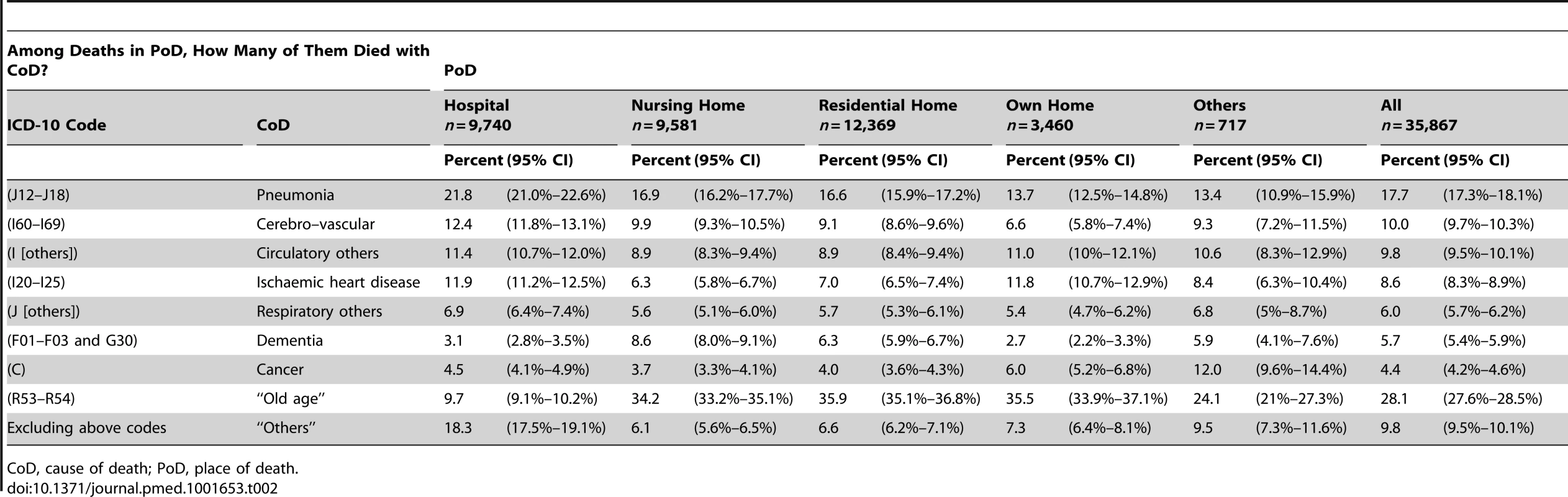
CoD, cause of death; PoD, place of death. The main causes of death varied by place of death. Pneumonia (21.8%, 95% CI 21.0%–22.6%) accounted for the largest group of hospital deaths, while across non-hospital settings “old age” formed the largest category and then pneumonia (Table 2). Cancer accounted for a small proportion of deaths across care settings, except in “other” settings (including hospices), accounting for 12.0% (95% CI 9.6%–14.4%) of deaths. Dementia accounted for few deaths either as an underlying cause (5.7%, 95% CI 5.4%–5.9%) or as a contributing cause (4.4%, 95% CI 4.2%–4.7%). Overall, recording multiple contributing causes of death was uncommon; most individuals had none (42.4%, 95% CI 41.9%–42.9%) or one (36.1%, 95% CI 35.6%–36.6%) (Table 1). Commonest contributing causes were: circulatory (12.1%, 95% CI 11.7%–12.5%), pneumonia (12.0%, 95% CI 11.6%–12.4%), “others” (9.0%, 95% CI 8.7%–9.4%), and dementia (4.4%, 95% CI 4.2%–4.7%). “Old age” formed the largest group (47.5%, 95% CI 46.9%–48.1%). Overall, 75.6% of centenarian death certifications stated “old age” as either an underlying cause (28.1%) or contributing cause (47.5%).
The main causes of death changed with increasing age (Table 3). Centenarians had relatively lower rates of chronic diseases as causes of death compared to the younger cohorts. In the youngest cohort aged 80–85 years ischaemic heart disease accounted for 19.0% (95% CI 18.9%–19.0%) of death certifications, compared to 8.6% (95% CI 8.3%–8.9%) for centenarians. Centenarians were certified as dying more often from pneumonia (17.7%, 95% CI 17.3–18.1) and “old age” (28.1%, 95% 27.7%–28.5%), compared to the youngest cohort (pneumonia 6%, 95% CI 5.9%–6.0%; “old age” 0.9%, 95% CI 0.9%–0.9%). Cause of death and place of death changed markedly in extreme old age compared to the “younger” age bands. Death from pneumonia in hospital increased 3-fold for centenarians to 21.8% (95% CI 21.0%–22.6%) from 7.3% (95% CI 7.2%–7.3%) for those aged 80–84 years (Table 4). Correspondingly, common causes of death in hospital prevalent in “younger” age groups declined in extreme old age, notably Ischemic heart disease and cancer (Table 4). Dying outside of hospital from “old age” increased markedly with advancing age. Over a third (34.2%, 95% CI 33.2%–35.1%) of centenarian deaths in nursing homes were certified as “old age” compared to only 2.4% (95% CI 2.3%–2.5%) for 80–84 year olds (Table 5). Dementia as cause of death decreased with advancing age in settings outside of hospital (Tables 5–8).
Tab. 3. All causes of death by age group. 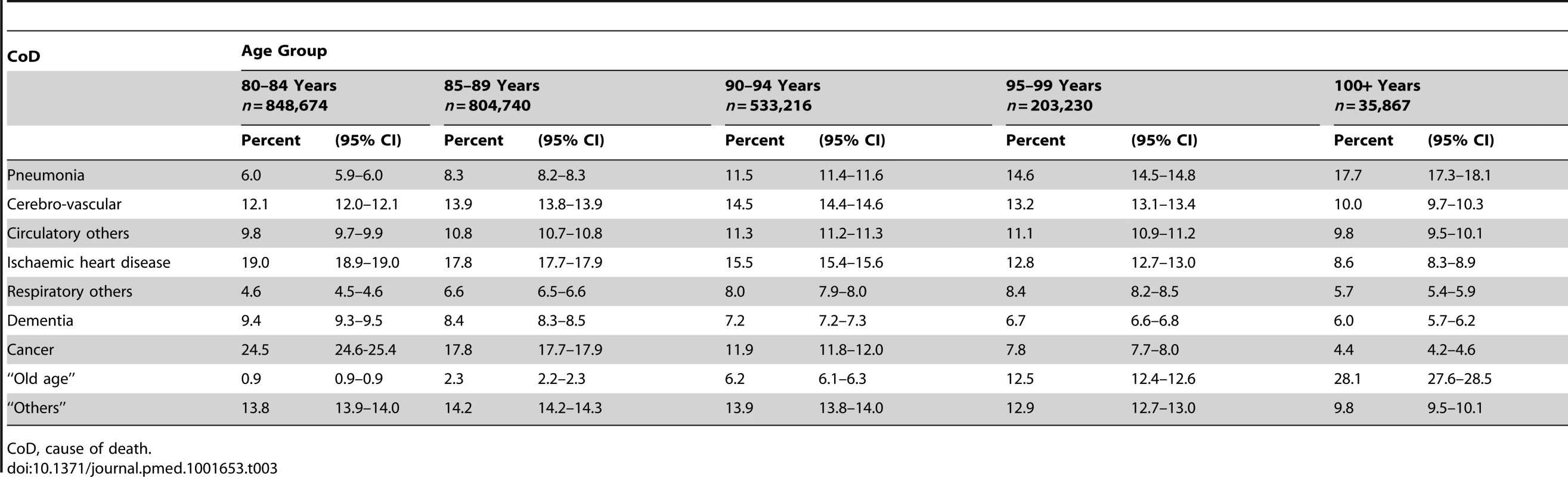
CoD, cause of death. Tab. 4. Cause of death by age bands and hospital as place of death. 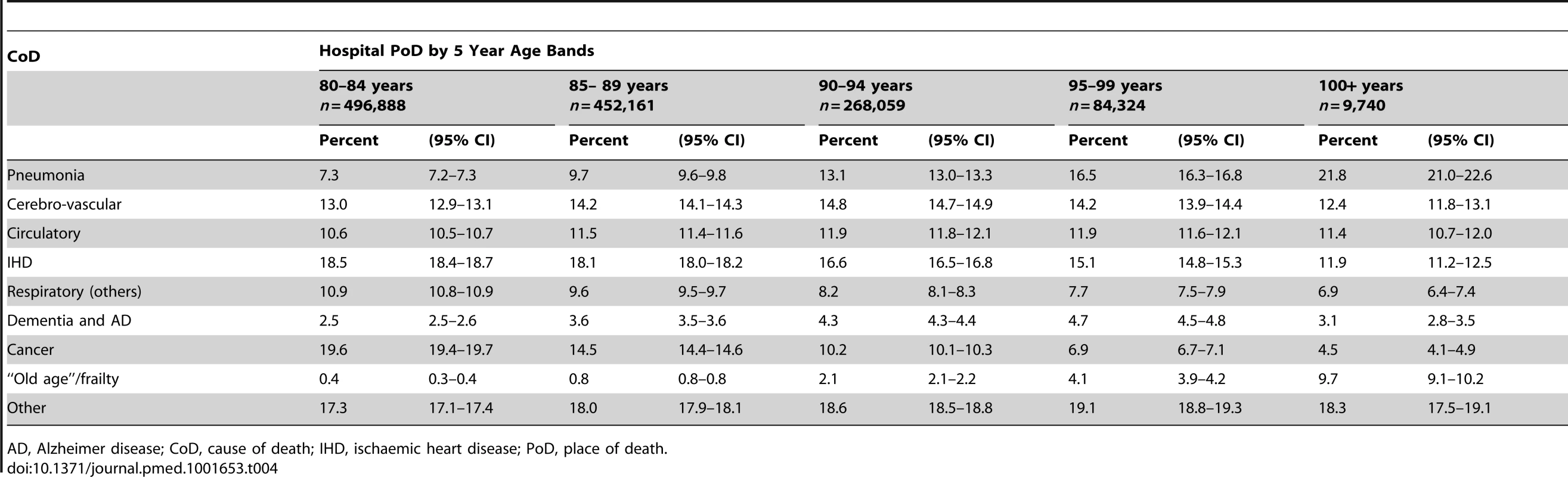
AD, Alzheimer disease; CoD, cause of death; IHD, ischaemic heart disease; PoD, place of death. Tab. 5. Cause of death by age bands and nursing home as place of death. 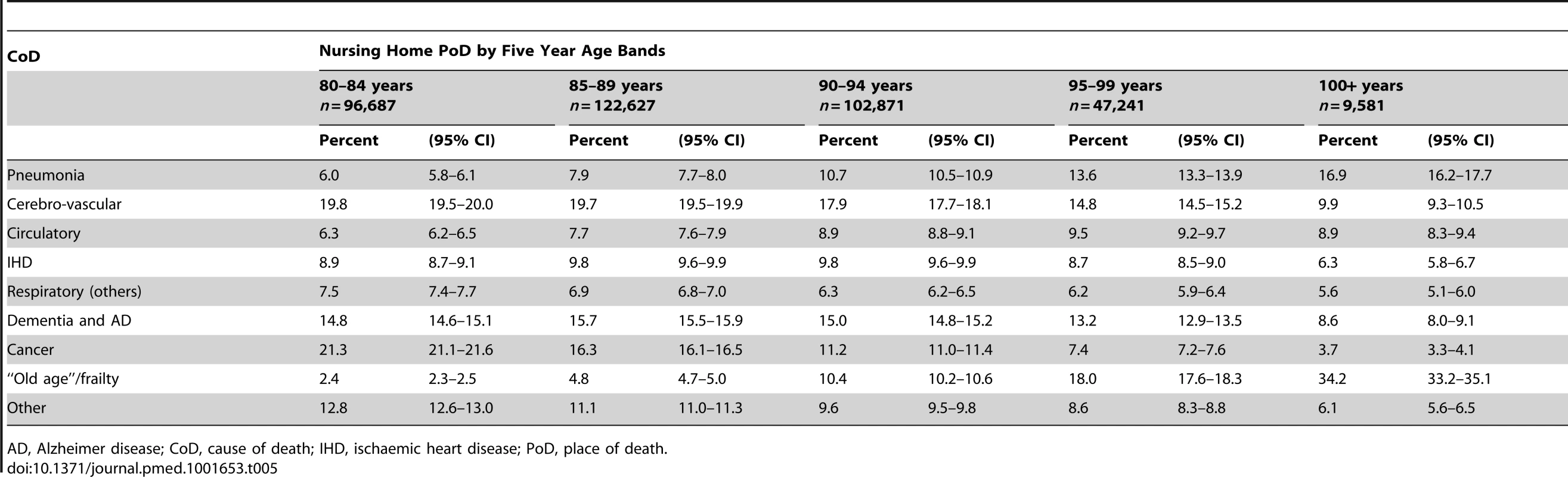
AD, Alzheimer disease; CoD, cause of death; IHD, ischaemic heart disease; PoD, place of death. Tab. 6. Cause of death by five year age band and residential home as place of death. 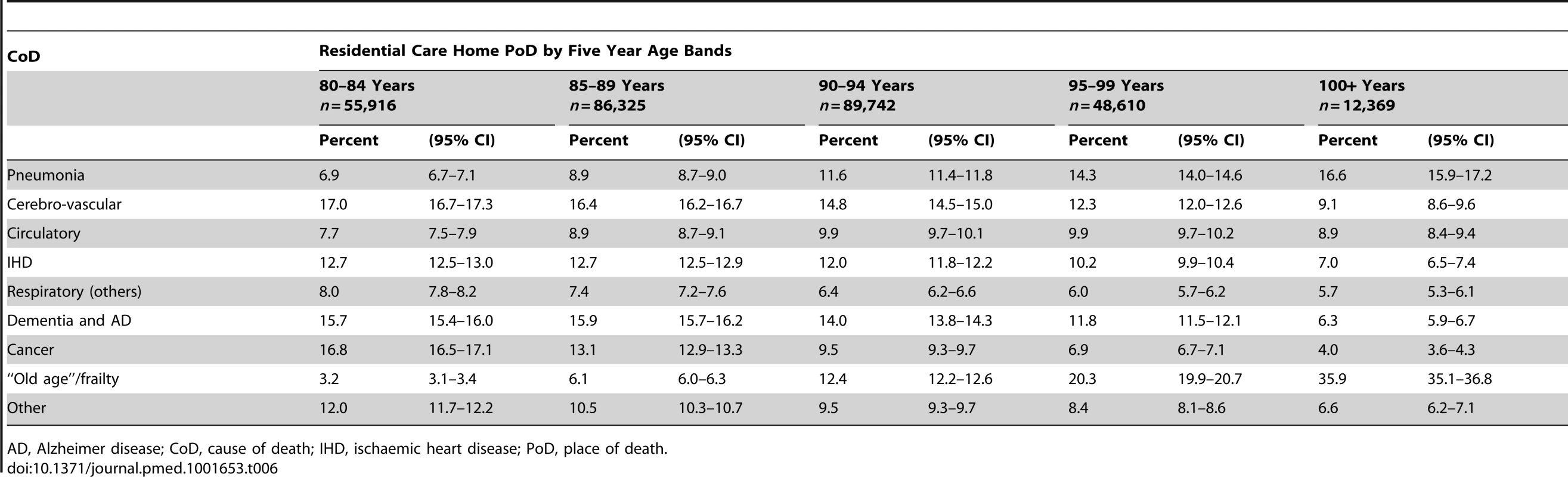
AD, Alzheimer disease; CoD, cause of death; IHD, ischaemic heart disease; PoD, place of death. Tab. 7. Cause of death by age bands and own home as place of death. 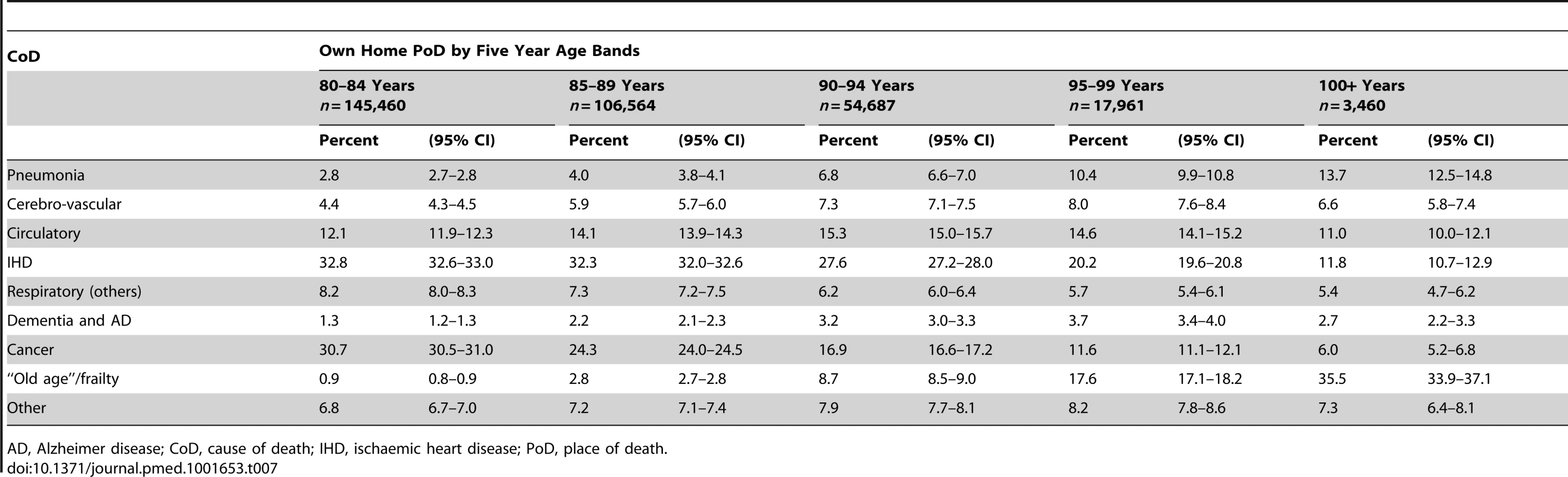
AD, Alzheimer disease; CoD, cause of death; IHD, ischaemic heart disease; PoD, place of death. Tab. 8. Cause of death by five year age band and “other” place of death. 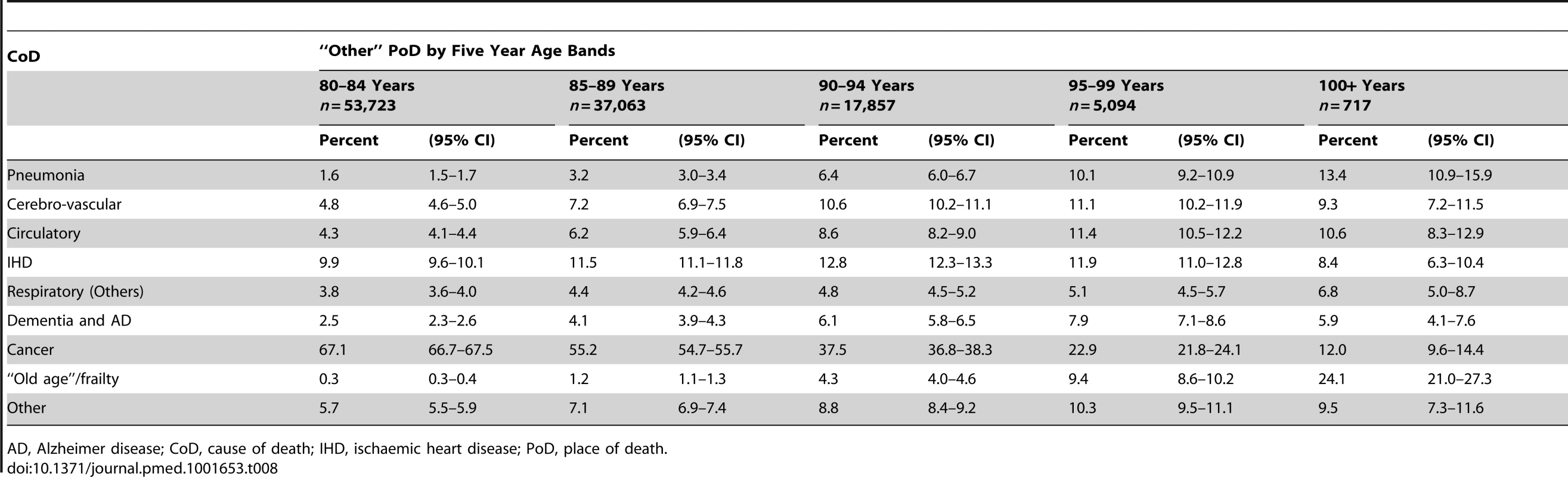
AD, Alzheimer disease; CoD, cause of death; IHD, ischaemic heart disease; PoD, place of death. Factors Associated with Centenarians’ Place of Death
Demographic factors
Women were more likely to die outside of hospital in a community setting of a care home (with or without nursing) and own residence, compared with men (Table 9). Marital status was not associated with place of death (Table 9).
Tab. 9. Proportion ratios and 95% CI of variables associated with place of death (hospital reference group) in England 2001–2010. 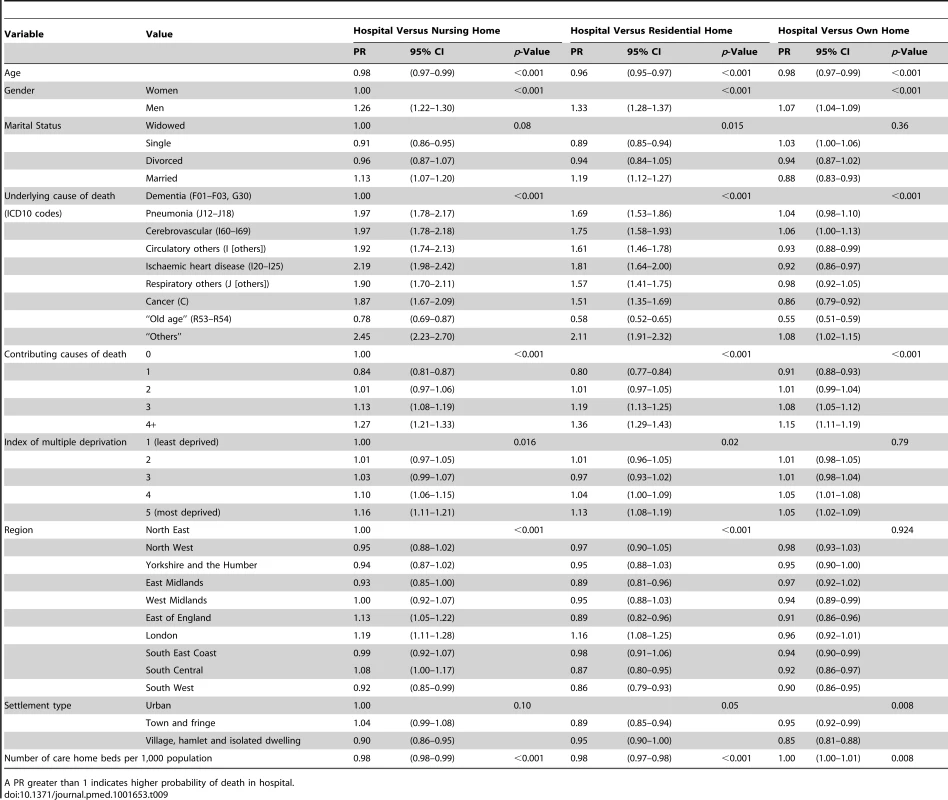
A PR greater than 1 indicates higher probability of death in hospital. Illness factors
Underlying causes of death (reference group: dementia) were associated with place of death (p<0.001; Table 9). Compared to people with dementia, people with an underlying cause of death from cancer (PR 0.86, 95% CI 0.79–0.92), ischaemic heart disease (PR 0.92, 95% CI 0.86–0.97), or other circulatory diseases (PR 0.93, 95% CI 0.88–0.99) were less likely to die in hospital than at home (Table 9). Only “old age” as a cause of death compared to people dying from dementia was associated with being less likely to die in hospital compared with a nursing home (PR 0.78, 95% CI 0.69–0.87) or residential care home (PR 0.58, 95% CI 0.52–0.65, p<0.001). Dying with a more cumulative picture of disease with certification of ≥4 contributing causes of death was associated with dying in hospital rather than a care home, either with nursing (PR 1.27, 95% CI 1.21–1.33) or without (PR 1.36, 95% CI 1.29–1.43). Conversely, those dying with a single contributing cause were less likely to die in hospital and more likely to die in a care home with nursing (PR 0.84, 95% CI 0.81–0.87) or without (PR 0.80, 95% CI 0.77–0.84), or in their own residence (PR 0.91, 95% CI 0.88–0.93).
Environmental factors
Higher numbers of care home beds were associated with fewer hospital deaths and more deaths in care homes (with nursing PR 0.98, 95% CI 0.98–0.99, p<0.001; or without nursing PR 0.98, 95% CI 0.97–0.98, p<0.001). The main difference between dying in hospital and care home type pertained to a higher prevalence of dementia in nursing homes (21.3% versus 16.5%) (Table 9). Once removed from the model, minimal differences were observed between cause of death and care home type (Chi2 13.98, degrees of freedom (df) = 7, p = 0.051).
Place of death was associated with level of deprivation and settlement type. Areas most deprived showed greatest association with dying in hospital rather than in a community setting (Table 9). Dying outside of hospital in one’s own residence related to usual residence of urban versus rural settlement (PR 0.85, 95% CI 0.81–0.89) or town/fringe (PR 0.95, 95% CI 0.92–0.99).
Discussion
This is the first study to our knowledge to examine trends in place of death for centenarians and the associated factors. Centenarians are a group who have outlived chronic diseases common as causes of death amongst “younger” older cohorts. Centenarians are a group whose death is often certified as from frailty/”old age” and pneumonia. Over three-quarters of death certifications stated “old age” as either an underlying or contributing cause of death. Nearly one in five died with pneumonia accompanied by contributing causes of chronic conditions, notably “old age.” Centenarians’ dying forms a picture of frailty exacerbated by the presence of a common stressor amongst older people of acute lung infection.
Patterns of cause of death changed with increasing age; this has implications in understanding differences in illness trajectories by age and has policy and service implications. The proportion of deaths from pneumonia increased with advancing age. In adults aged 70–84 years a comparatively small proportion were certified with pneumonia as the underlying cause of death (4.0%, 70–74 years [7]; 6.0%, 80–84 years). This number increased over 3-fold for centenarians (17.7%) and was commonly accompanied by increasing frailty and co-morbidities [32]. Centenarians’ experiences of living and dying with frailty are one of increased likelihood of “acute” decline from a stressor event accompanied by a background of frailty with declining physical function and vulnerability to a poor outcome following a stressor event, for example, an infection [33],[34].
An imperative for policy and services is the recognition of centenarians’ increased likelihood of “acute” decline and wider provision of advance care planning and anticipatory care with goals to promote quality of life and avoidance of crisis-driven interventions, notably hospital admission in the dying phase [35]. Wider recognition is required of the heterogeneous nature of illnesses’ trajectories that change with increasing longevity and service response to accommodate living with increasing frailty and vulnerability to acute decline. Wider recognition of centenarians’ high risk to a stressor event, notably pneumonia, amidst increasing chronic conditions [32], and frailty [37] could better tailor care provision that anticipates and plans for vulnerability to points of marked deterioration in health status and poor outcome. Illness trajectories for “frail” older people confer a marked deterioration in the last month of life [37],[38]. EoLC programmes and services need to anticipate and plan for the heterogeneity of decline experienced by frail elders [37], the intrinsic uncertainty as to how best to measure severity [34], and recognise when deterioration may precede the dying phase or be reversible. Studies report practitioners’ difficulties in recognising nearness to EoL for older people [39],[40]. A way forward is care not limited by prognostication, but directed by personal goals that seek to promote quality of life and anticipate frail elders’ vulnerability to “acute” deterioration in health status [34],[41].
Over the 10 years, trends in place of death little changed. More than one in four centenarians (27.2%) died in hospital. Most continued to die in a nursing or residential care home with little variation by cause of death. A small increasing proportion died at home. This finding follows patterns observed for people aged over 85 years who since 2006 have seen a reversal of a 30 year trend of declining death at home across all age groups[42], but this is mainly seen for people with cancer, not those with non-malignant conditions [43],[44].
The risk of dying in hospital for centenarians was associated with interplay between illness factors of cause of death, particularly pneumonia and ischaemic heart disease, and increasing contributing causes; individual factors, notably gender and environmental aspects, particularly higher level of deprivation and lower care home bed capacity. These findings support studies on place of death for older people that illustrate that gender, cause of death, socioeconomic status, and care home bed capacity have an important and complex effect on the likelihood of dying in hospital [5],[7],[19],[45]. Dying from cancer was associated with dying in one’s own home, but not with dying in a care home with or without nursing.
The rising number of centenarians and continued use of hospital care at the EoL indicates an urgent need to ensure adequate long-term care [20],[46]–[48] and responsive community care services to support people living with extreme longevity in these care settings. Compared to place of death for people aged 90 years or over in other European countries, the proportion dying in hospital in England is high and those dying in care homes low. For example, in the Netherlands and Finland most people aged over 90 years die in a long-term care setting (e.g., a nursing home) (90.6% [49] and 76.2% [50], respectively); few die in hospital (16.3% [51] and 13.6% [50], respectively). The increasing number of care home beds is positively associated with less likely death in hospital [49], but this alone is insufficient to explain the marked differences in place of death by age across European countries. Variations in health care service provision to care homes by country likely contribute to differences observed [25],[49],[52]. Better health care provision could enable people to remain in their usual residence and reduce hospital admission at the EoL—a major cost driver in EoLC [53].
Little variation between cause of death and dying in a care home with or without nursing has service implications, particularly for residential care homes that are social care settings reliant on primary health care services to meet residents’ health needs [26],[27]. The study’s findings suggest there is an equal if not greater need for EoLC in social care settings and adds weight to calls for improved EoLC in all settings. National EoLC interventions for care homes are mainly implemented in those with on site nursing. For example the Gold Standards Framework for Care Homes details EoLC interventions and staff training [54], although widely implemented with over 300 accredited care homes most are registered as a nursing home [55]. Moreover, most centenarians died from conditions rarely associated with the provision of specialist palliative care [56], with comparatively few dying from cancer and many from “old age.” These findings indicate centenarians’ reliance on general practitioners (a general physician) and community nurses to support EoLC provision, particularly in residential care homes. Gage and colleagues assert care home residents frequently experience a poor "fit" between their needs, and often ad hoc health care support hampered by limited strategic planning [26] and recognition of complex health needs associated with extreme longevity.
Strengths and Limitations
Centenarians are a group often overlooked by policy makers and researchers. The study’s findings report analysis of a large unique dataset enabling detailed understanding on variations in cause of death by place of death for centenarians. The data comprise actual deaths over a specified time period for a specified group. The influence of variation in life expectancy on longevity is an area that requires further consideration to situate this work within, for example, the lower proportion of centenarian deaths in areas of greater deprivation, which reflects variance in life expectancy by region and level of deprivation.
Place of death formed the main outcome in the data analysis and associations, notably with cause of death. Although UK death certificate data are considered high quality [21], they do not encompass place of care or preferences for care in the period before death. The findings indicate associations with place of death, but prospective and longitudinal research is required to examine care and preferences in the preceding period to death. Certifying death is a complex medical process influenced notably by clinical uncertainty and family members of the deceased [57]. The many deaths certified as “old age” in community settings may relate both to diagnostic uncertainty with likely limited medical work up, or desirability for workup [37], and to protect the family with certification of death as “old age” as understandable and non-reversible. However, certifying death using ill-defined ICD-10 codes of malaise and fatigue (R53) or senility (R54) “old age” limits interpretation of cause of death and guidance of health strategies and programmes [21]. These ill-defined codes describe a symptom group rather than a defined disease [21]; a symptom group conceptualised as “frail” [33]. No associated causes of death are indicated for decedents where “old age” is the underlying cause of death. Underreporting of associated causes of death is likely. The ONS rule for death registration data dictates that if a contributing cause is stated this transposes “old age” as the underlying cause of death.
Future areas of research concern prospective cohort work on living and dying with advancing frailty to understand trajectories of disability in the last year of life to develop a conceptual model of living and dying with extreme longevity to inform health and social care policy. Replication of Mitchell and colleague’s [58] prospective cohort study of individuals with dementia to encompass “frailty” and extreme longevity is required.
In conclusion, dying in hospital from an “acute” cause or stressor event is common for centenarians in England. A policy imperative is the recognition of centenarians’ seemingly “hidden needs” of increased likelihood of “acute” decline and wider provision of anticipatory care to enable people to remain in their usual residence and reduce reliance on hospital care at the EoL. Increasing care home bed capacity could further reduce reliance on hospital care. The recognition of “acute” death amidst chronic contributing conditions illustrates the difficulties for people living and dying with extreme longevity. To better tailor care services requires prospective cohort work to examine the clinical course of extreme longevity and associated frailty.
Supporting Information
Zdroje
1. United Nations DoEaSA, Population Division (2011) World Population Prospects: The 2010 Revision. New York: United Nations.
2. Office for National Statistics (2011) Estimates of Centenarians in the UK, 2010. Population aged 100 years and over, UK, 1965–2010. Newport, South Wales: Office for National Statistics.
3. ThatcherAR (1992) Trends in numbers and mortality at high ages in England and Wales. Popul Stud (Camb) 46 : 411–426.
4. Department for Work and Pensions (2011) Number of Future Centenarians by Age Group. London: Department for Work and Pensions.
5. GruneirA, MorV, WeitzenS, TruchilR, TenoJ, et al. (2007) Where people die: a multilevel approach to understanding influences on site of death in America. Med Care Res Rev 64 : 351–378.
6. FlemingJ, ZhaoJ, FarquharM, BrayneC, BarclayS (2010) Place of death for the ’oldest old': >/ = 85-year-olds in the CC75C population-based cohort. British Journal of General Practice 60 : 275–282.
7. National End of Life Care Intelligence Network (2010) Deaths in Older Adults in England. Bristol: South West Public Health Observatory.
8. National End of Life Care Intelligence Network (2010) Variations in Place of Death in England. Inequalitties or appropriate consequences of age, gender and cause of death? Bristol: National End of Life Care Intelligence Network.
9. DumontS, JacobsP, FassbenderK, AndersonD, TurcotteV, et al. (2009) Costs associated with resource utilization during the palliative phase of care: a Canadian perspective. Palliat Med 23 : 708–717.
10. Gomes B, Higginson IJ, Calanzani N, Cohen J, Deliens L, et al.. (2012) Preferences for place of death if faced with advanced cancer: a population survey in England, Flanders, Germany, Italy, the Netherlands, Portugal and Spain. Annals of Oncology. 2012/02/22 ed.
11. GottM, SeymourJ, BellamyG, ClarkD, AhmedzaiS (2004) Older people's views about home as a place of care at the end of life. Palliative Medicine 18 : 460–467.
12. Department of Health (2008) End of Life Care Strategy - promoting high quality care for adults at the end of life. London: Crown.
13. HutnikN, SmithP, KochT (2012) What does it feel like to be 100? Socio-emotional aspects of well-being in the stories of 16 Centenarians living in the United Kingdom. Aging Ment Health 16 : 811–818.
14. KochT, PowerC, KralikD (2007) Researching with centenarians. Int J Older People Nurs 2 : 52–61.
15. Serra V, Watson J, Sinclair D, Kneale D (2011) 'Living Beyond 100': A report on centenarians. London: International Longevity Centre-UK.
16. CohenJ, BilsenJ, MiccinesiG, LofmarkR, Addington-HallJ, et al. (2007) Using death certificate data to study place of death in 9 European countries: opportunities and weaknesses. BMC Public Health 7 : 283–292.
17. AhmadS, O'MahonyMS (2005) Where older people die: a retrospective population-based study. QJM 98 : 865–870.
18. LazenbyJM, OlshvevskiJ (2012) Place of death among Botswana's oldest old. Omega (Westport) 65 : 173–187.
19. MitchellSL, TenoJM, MillerSC, MorV (2005) A National Study of the Location of Death for Older Persons with Dementia. Journal of the American Geriatrics Society 53 : 299–305.
20. LockA, HigginsonI (2005) Patterns and predictors of place of cancer death for the oldest old. BMC palliative care 4 : 6.
21. MathersCD, FatDM, InoueM, RaoC, LopezAD (2005) Counting the dead and what they died from: an assessment of the global status of cause of death data. Bull World Health Organ 83 : 171–177.
22. ElmEv, AltmanDG, EggerM, PocockSJ, GøtzschePC, et al. (2007) Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 335 : 806–808.
23. Office for National Statistics (2009) Mortality statistics: Deaths registered in 2009. Newport, South Wales: Office for National Statistics.
24. Mclennan D, Barnes H, Noble M, Davies J, Garratt E (2011) The English Indices of Deprivation 2010. London: Department for Communities and Local Government.
25. Froggatt K, Reitinger E, Heimerl K, Hockley J, Brazil K, et al.. (2013) Palliative Care in Long-Term Care Settings for Older People: EAPC Taskforce 2010–2012. European Association of Palliative Care.
26. GageH, DickinsonA, VictorC, WilliamsP, CheynelJ, et al. (2012) Integrated working between residential care homes and primary care: a survey of care homes in England. BMC Geriatr 12 : 71.
27. GoodmanC, WoolleyR, KnightD (2003) District nurse involvement in providing palliative care to older people in residential care homes. Int J Palliat Nurs 9 : 521–527.
28. GomesB, HigginsonIJ (2006) Factors influencing death at home in terminally ill patients with cancer: systematic review. BMJ 332 : 515–521.
29. DeddensJA, PetersenMR (2008) Approaches for estimating prevalence ratios. Occupational and Environmental Medicine 65 : 501–506.
30. GelmanA (2004) Exploratory data analysis for complex models. Journal of Computational and Graphical Statistics 13 : 755–779.
31. Ihaka R, Gentleman R (2012) The R Project for Statistical Computing. R version 2.15.3 ed. http://www.r-project.org/index.html.
32. BarnettK, MercerSW, NorburyM, WattG, WykeS, et al. (2012) Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet 380 : 37–43.
33. FriedLP, TangenCM, WalstonJ, NewmanAB, HirschC, et al. (2001) Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 56: M146–156.
34. CleggA, YoungJ, IliffeS, RikkertMO, RockwoodK (2013) Frailty in elderly people. Lancet 381 : 752–762.
35. MathieE, GoodmanC, CrangC, FroggattK, IliffeS, et al. (2012) An uncertain future: the unchanging views of care home residents about living and dying. Palliat Med 26 : 734–743.
36. Falaschetti E (2002) The Health Survey for England 2000: the general health of older people and their use of health services. London.
37. GillTM, GahbauerEA, HanL, AlloreHG (2010) Trajectories of disability in the last year of life. N Engl J Med 362 : 1173–1180.
38. LunneyJR, LynnJ, FoleyDJ, LipsonS, GuralnikJM (2003) Patterns of functional decline at the end of life. JAMA 289 : 2387–2392.
39. MitchellSL, KielyDK, HamelMB (2004) Dying with advanced dementia in the nursing home. Archives of Internal Medicine 164 : 321–326.
40. AbarshiEA, EchteldMA, Van den BlockL, DonkerGA, DeliensL, et al. (2011) Recognising patients who will die in the near future: a nationwide study via the Dutch Sentinel Network of GPs. Br J Gen Pract 61: e371–378.
41. MitchellSL, MillerSC, TenoJM, KielyDK, DavisRB, et al. (2010) Prediction of 6-month survival of nursing home residents with advanced dementia using ADEPT vs hospice eligibility guidelines. JAMA 304 : 1929–1935.
42. GomesB, HigginsonIJ (2008) Where people die (1974–2030): past trends, future projections and implications for care. Palliative Medicine 22 : 33–41.
43. GaoW, HoYK, VerneJ, GlickmanM, HigginsonIJ, et al. (2013) Changing patterns in place of cancer death in England: a population-based study. PLoS Med 10: e1001410.
44. GomesB, CalanzaniN, HigginsonIJ (2012) Reversal of the British trends in place of death: Time series analysis 2004–2010. Palliat Med 26 : 102–107.
45. Van RensbergenG, NawrotTS, Van HeckeE, NemeryB (2006) Where do the elderly die? The impact of nursing home utilisation on the place of death. Observations from a mortality cohort study in Flanders. BMC Public Health 6 : 178.
46. Royal College of Physicians, Royal College of Nursing, British Geriatric Society (2000) The health and care of older people in care homes: a comprehensive interdisciplinary approach London: Royal College of Physicians.
47. HigginsonIJ, AstinP, DolanS (1998) Where do cancer patients die? Ten-year trends in the place of death of cancer patients in England. Palliative medicine 12 : 353–363.
48. ZhaoJ, BarclayS, FarquharM, KinmonthAL, BrayneC, et al. (2010) The oldest old in the last year of life: population-based findings from Cambridge city over-75s cohort study participants aged 85 and older at death. J Am Geriatr Soc 58 : 1–11.
49. HouttekierD, CohenJ, BilsenJ, Addington-HallJ, Onwuteaka-PhilipsenBD, et al. (2010) Place of death of older persons with dementia. A study in five European countries. J Am Geriatr Soc 58 : 751–756.
50. AaltonenM, FormaL, RissanenP, RaitanenJ, JylhaM (2010) Transitions in health and social service system at the end of life. European Journal of Ageing 7 : 91–100.
51. CohenJ, BilsenJ, Addington-HallJ, LofmarkR, MiccinesiG, et al. (2008) Population-based study of dying in hospital in six European countries. Palliat Med 22 : 702–710.
52. HouttekierD, CohenJ, BilsenJ, Addington-HallJ, Onwuteaka-PhilipsenB, et al. (2010) Place of death in metropolitan regions: metropolitan versus non-metropolitan variation in place of death in Belgium, The Netherlands and England. Health Place 16 : 132–139.
53. TenoJM, GozaloPL, BynumJP, LelandNE, MillerSC, et al. (2013) Change in end-of-life care for Medicare beneficiaries: site of death, place of care, and health care transitions in 2000, 2005, and 2009. JAMA 309 : 470–477.
54. Kinley J, Froggatt K, Bennett MI (2012) The effect of policy on end-of-life care practice within nursing care homes: A systematic review. Palliat Med DOI: 10.1177/0269216311432899
55. National Gold Standards Framework Centre (2012) Gold Standards Framework in care homes
56. AbarshiE, EchteldMA, Van den BlockL, DonkerG, DeliensL, et al. (2010) The oldest old and GP end-of-life care in the Dutch community: a nationwide study. Age Ageing 39 : 716–722.
57. McAllumC, St GeorgeI, WhiteG (2005) Death certification and doctors' dilemmas: a qualitative study of GPs' perspectives. Br J Gen Pract 55 : 677–683.
58. MitchellSL, TenoJM, KielyDK, ShafferML, JonesRN, et al. (2009) The clinical course of advanced dementia. N Engl J Med 361 : 1529–1538.
Štítky
Interné lekárstvo
Článok vyšiel v časopisePLOS Medicine
Najčítanejšie tento týždeň
2014 Číslo 6- Parazitičtí červi v terapii Crohnovy choroby a dalších zánětlivých autoimunitních onemocnění
- Intermitentní hladovění v prevenci a léčbě chorob
- Statinová intolerance
- Co dělat při intoleranci statinů?
- Monoklonální protilátky v léčbě hyperlipidemií
-
Všetky články tohto čísla
- Evidence for the Selective Reporting of Analyses and Discrepancies in Clinical Trials: A Systematic Review of Cohort Studies of Clinical Trials
- Health Care in Danger: Deliberate Attacks on Health Care during Armed Conflict
- Melanocytic Nevi as Biomarkers of Breast Cancer Risk
- Blood Transfusions following Trauma: Finding an Evidence-Based Vein
- Antiretroviral Therapy for Refugees and Internally Displaced Persons: A Call for Equity
- Association between Cutaneous Nevi and Breast Cancer in the Nurses' Health Study: A Prospective Cohort Study
- Efficacy of Pneumococcal Nontypable Protein D Conjugate Vaccine (PHiD-CV) in Young Latin American Children: A Double-Blind Randomized Controlled Trial
- Pediatric Oncology as the Next Global Child Health Priority: The Need for National Childhood Cancer Strategies in Low- and Middle-Income Countries
- Place and Cause of Death in Centenarians: A Population-Based Observational Study in England, 2001 to 2010
- HIV among People Who Inject Drugs in the Middle East and North Africa: Systematic Review and Data Synthesis
- Association between Melanocytic Nevi and Risk of Breast Diseases: The French E3N Prospective Cohort
- Patient-Safety-Related Hospital Deaths in England: Thematic Analysis of Incidents Reported to a National Database, 2010–2012
- Pushback: The Current Wave of Anti-Homosexuality Laws and Impacts on Health
- HIV Treatment-as-Prevention Research at a Crossroads
- Red Blood Cell Transfusion and Mortality in Trauma Patients: Risk-Stratified Analysis of an Observational Study
- PLOS Medicine
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Melanocytic Nevi as Biomarkers of Breast Cancer Risk
- Antiretroviral Therapy for Refugees and Internally Displaced Persons: A Call for Equity
- Efficacy of Pneumococcal Nontypable Protein D Conjugate Vaccine (PHiD-CV) in Young Latin American Children: A Double-Blind Randomized Controlled Trial
- Blood Transfusions following Trauma: Finding an Evidence-Based Vein
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



