-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Arthroscopy-assisted osteosynthesis of triplane fracture – case report
Authors: Jakub Malý 1; Lubomír Kopp 1,2; Karel Edelmann 1
Authors place of work: Krajská zdravotní, a. s. – Masarykova nemocnice v Ústí nad Labem, Klinika úrazové chirurgie, Traumacentrum 1; Ústav anatomie 2. LF UK, Praha 2
Published in the journal: Úraz chir. 26., 2018, č.1
Summary
Triplane fractures are rare injuries of the transitional period of skeletal maturation, where the physeal growth plate is not yet fully closed. Computed tomography plays an essential role in the diagnostics, the most important procedure in the therapy of displaced fractures are a reduction of the articular surface performed under visual control and stable fixation with interfragmetary compression. Arthroscopy-assisted osteosynthesis fulfils the requirements of being a minimally invasive procedure, while preserving the possibility of visual control of the reduction, and seems to be a suitable alternative to other techniques. Anatomical reduction of the articular surface is crucial for proper healing without deformities, growth disturbances and resulting complications in adolescence. A disadvantage of the arthroscopically assisted osteosynthesis lies in its equipment demands and the required level of erudition of the surgical team. Hence, these injuries shall be centralised at specialized departments.
Keywords:
Triplane fracture – arthroscopy – osteosynthesis
INTRODUCTION
Triplane fractures of the distal tibia are characterized with a triplane fracture line in the transversal, sagittal and coronal dimension, affecting the epiphysis and metaphysis of the skeleton. They belong among fractures of the transition age in adolescents, between 12 and 15 years of age, occurring before the complete closure of growth plates. The incidence varies between 5 and 10 % of intra-articular fractures in children, and is more common in boys [13]. The most frequently observed mechanism of injury is a forced dorsal flexion and external rotation, caused with an externally applied force [3, 5, 16]. The basis for occurrence of this fracture is an asymmetric closure of the growth plate, when the growth plate gradually closes laterally from the medial side, and the anterolateral part is closed as the latest [9]. The individual fracture lines depend on the degree of maturity and closure of the physeal growth plate.
Depending on the number of fragments, we distinguish among two-fragment, three-fragment and four-fragment fractures. The injury may also include a distal fibular fracture, which is not added to the number of fragments. The fragments may be formed with anterolateral distal tibial epiphysis, anteromedial epiphysis, posterior complex consisting of the posteromedial epiphysis, with a metaphyseal processus, and broken off medial malleolus. According to the fracture line at the medial malleolus, Shin et al. further divide the fractures into two sub-groups – extra-articular or intra-articular; these are further categorized according the placement towards the bearing area of the upper ankle [12]. Apart from a plain radiograph in two perpendicular planes, also computed tomography plays and important role in the diagnostics of this injury, which reveals all fracture lines and helps with a precise diagnostics and subsequent planning of suitable treatment [5, 8, 16].
Triplane fractures with intra-articular shift of fragments smaller than 2 mm may be treated conservatively, with a short-term immobilization of the ankle for the period of 4–6 weeks, under X-ray controls performed in one-week intervals [4].
Each fracture with an intra-articular shift of the fracture line exceeding 2 mm requires anatomical reduction, using the closed or open technique [5, 6, 16].
Closed reduction of the fracture is performed under general anaesthesia, with muscle relaxation. The reduction manoeuvre should not be performed repeatedly, due to the possibility of causing further trauma, haemorrhage and damaging the growth plate. Adequate reduction in all planes is usually achieved in 30–50 % of cases, and needs to be verified with a post-reduction CT image [4].
Surgical management is necessary in cases of persisting dislocation of fragments [4]. Various surgical techniques may be used, the first and the least invasive one is a closed reduction and percutaneous fixation using compression screws. Another technique is the below-presented arthroscopy-assisted reduction and fixation. The third technique, which is however the least considerate to soft tissues, is an open reduction and internal fixation.
Possible complications of the treatment may be a result of insufficient diagnostics, with overlooking associated injuries, which most frequently include fractures of the proximal humerus and Maisonneuve fracture. Other possible complications include a preliminary closure of the growth plate, with a secondary retardation of the tibial growth and a tibiofibular growth discrepancy and resulting deformity of the ankle joint [2, 4]. Post-traumatic arthritis is observed most frequently due to leaving an intra-articular dislocation greater than 2 mm, or angular rotation of more than 10° [10]. Specifically in triplane fractures, the syndrome of extensor retinaculum may occur, which presents a unique type of compartment syndrome, when the anterior metaphyseal fragment compresses the muscle bellies of m. extenzor pollicis longus and m. peroneus tertius with n. peroneus profundus against the upper extensor retinaculum. The condition is manifested with pains, swelling and decreased sensitivity in the first interdigital area [2].
Description of the case
The patient was a 16-year-old man who sustained an injury after his friend fell on his right foot. Primarily, a plane radiograph of the ankle joint in two perpendicular planes was performed at the local hospital, with the resulting diagnosis of a tibial pilon fracture, with intra-articular dislocation exceeding 2 mm and epiphysiolysis of the lateral malleolus of the Salter Harris type I. The patient was treated with plaster LU splints and crutches. Further examination and final treatment at a higher-level department was recommended.
At our centre, HRCT imaging of the ankle joint was performed, with reconstructions, based upon which we determined the diagnosis of triplane four-fragment fracture (Fig. 1). The local condition was satisfactory upon admission, with minimal swelling of the crus and the malleolus, without bullae or defects. Peripheral areas were without neurocirculatory deficit.
Fig. 1. HRCT examination of the malleolus was performed at our department; based upon the findings, we determined the diagnosis of triplane four-fragment fracture 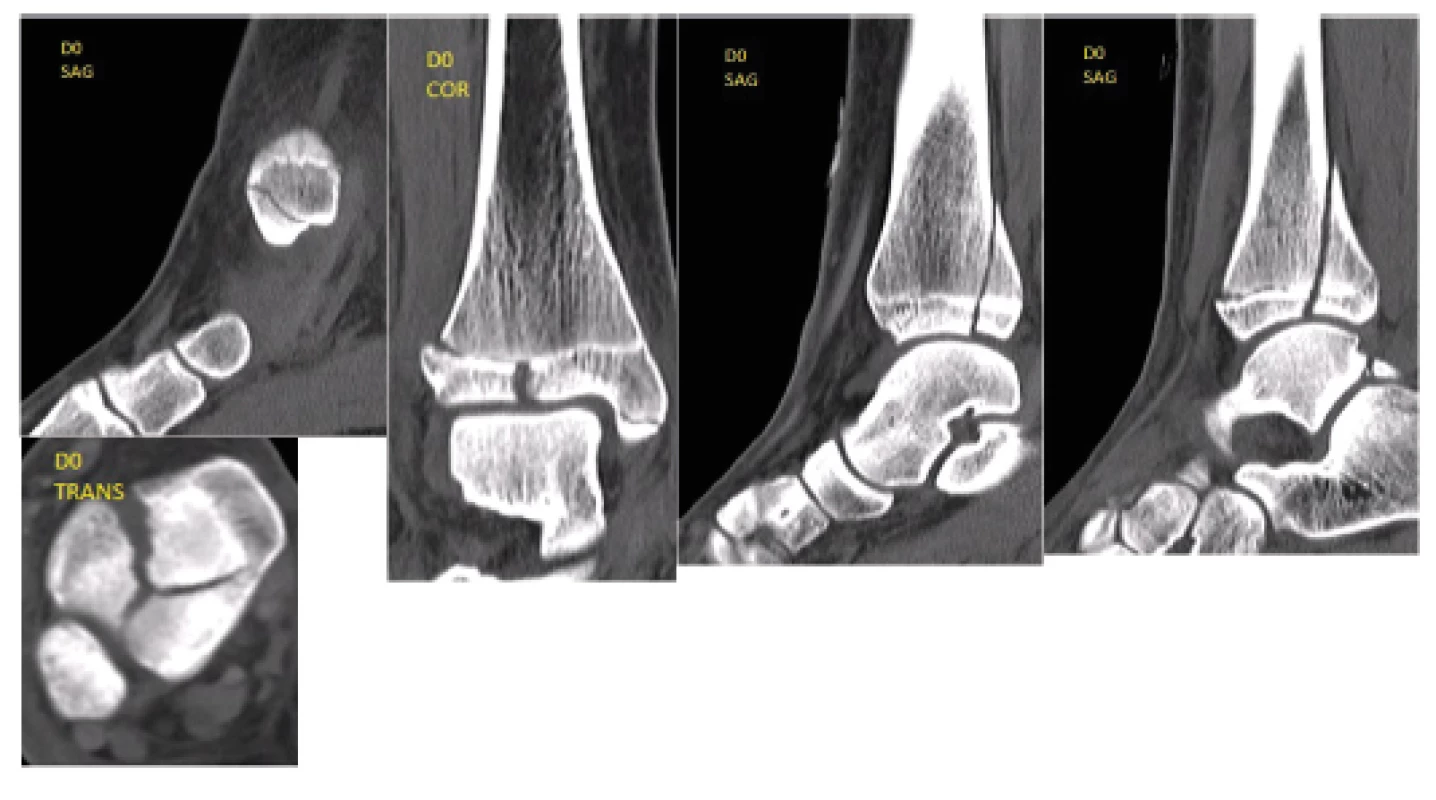
Considering the dislocation and position of the fracture, we decided for the surgical management. Considering its minimally invasive character and the perioperative possibility of controlling the reposition of the articular surface, we chose the arthroscopy-assisted osteosynthesis. The surgery was performed on the third day after injury. A common arthroscopy tower was used, with 30-degree optics, 4 mm wide, and the filling pressure of 60 mm H2O. The entries in the upper ankle were standard anteromedial and anterolateral. The fracture was treated with headless dosed compression titanium screws HCS 4.5 mm (DePuy Company, Johnson and Johnson), the advantage of which is the possibility of being driven below the level of the articular cartilage, without the need of possible later extraction. The procedure was performed by a physician experienced in arthroscopy, lasted 45 minutes and was performed in a bloodless field; the period of X-ray radiation during the procedure was 15 seconds.
During the surgical procedure, the most important point was the visually controlled anatomical reduction of the articular surface. After inserting the optics and flushing of the haemarthrosis, the posterior lane was gradually reduced, as the biggest fragment, which was subsequently fixed with two HCS screws inserted from secondary incisions. Fixation of the anterolateral fragment with one HCS screw followed. The articular surface was congruent, with sufficient compression at the fracture line (Fig. 2). The medial malleolus was fixed using identical technique. The fibular fracture was treated with percutaneously inserted Kirschner wires 1.5 mm wide, also Redon drain was placed into the joint. The plaster fixation was retained as a protective measure.
Fig. 2. The articular surface was congruent, with a sufficient compression at the fracture line 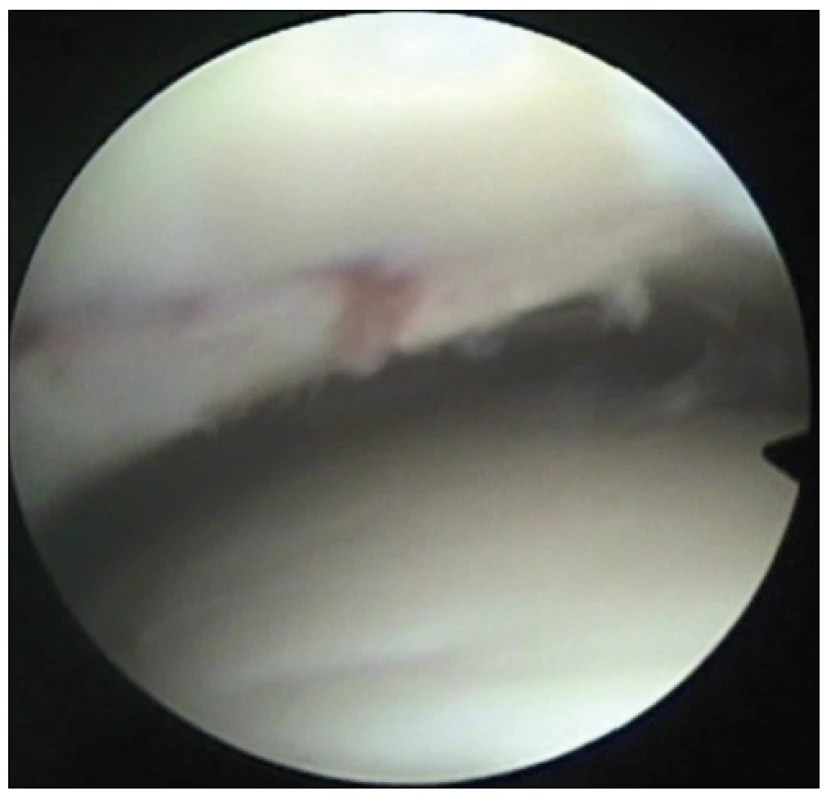
The drain was extracted on the first postoperative day, with minimal swelling present. Control radiographs and CT examination with multiplanar reconstructions were performed, which confirmed a very good position of the fragments (Fig. 3). The patient was without any subjective complaints on the second postoperative day. The wounds healed without any complications, the Kirschner wires were extracted from the lateral malleolus five weeks after the procedure. Also, guided physiotherapy of the ankle joints was initiated at this period, partial load bearing on the extremity was permitted. A complete healing was apparent on radiographs during outpatient controls after 12 weeks, with a preserved congruence of the articular surface, full load bearing was allowed. The patient was observed at our clinic, with radiographic controls, until the growth plates have fully closed, i.e. for the period of further 16 months (Fig. 4).
Fig. 3. Control CT examination with multiplanar reconstructions, which confirmed a very good position of the fragments 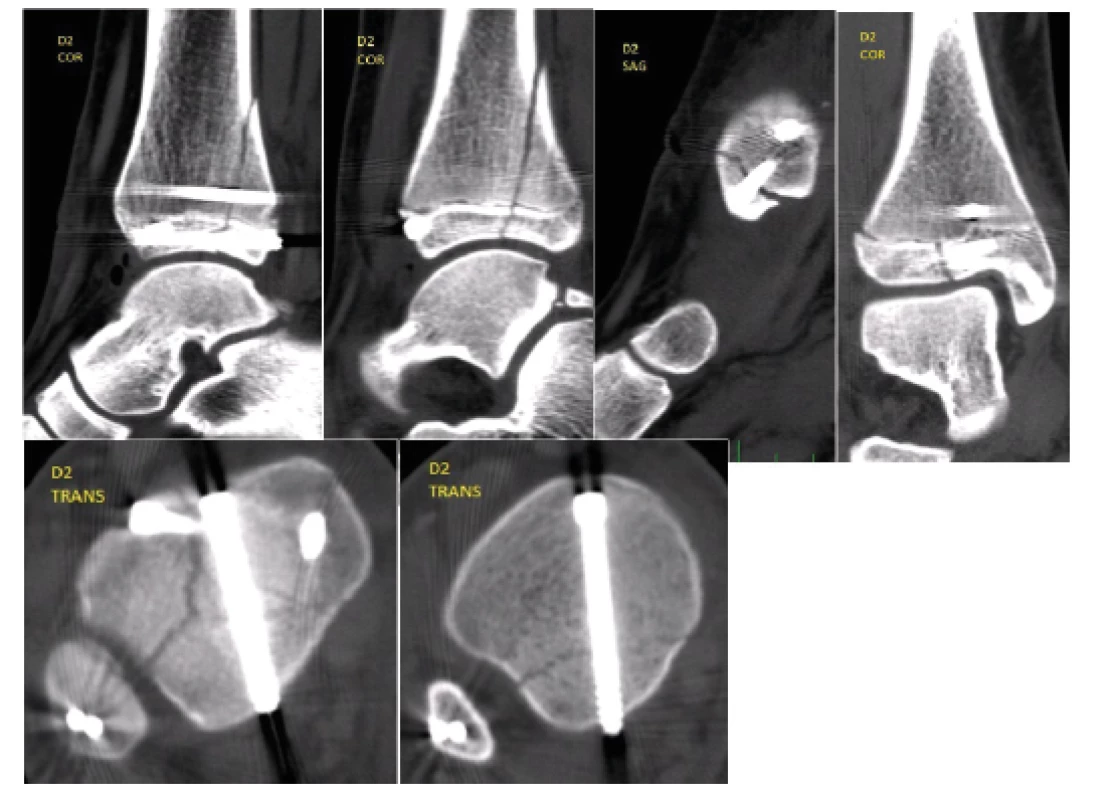
Fig. 4. The patient was clinically observed until the growth plates have fully closed, i.e. for the period of further 16 months 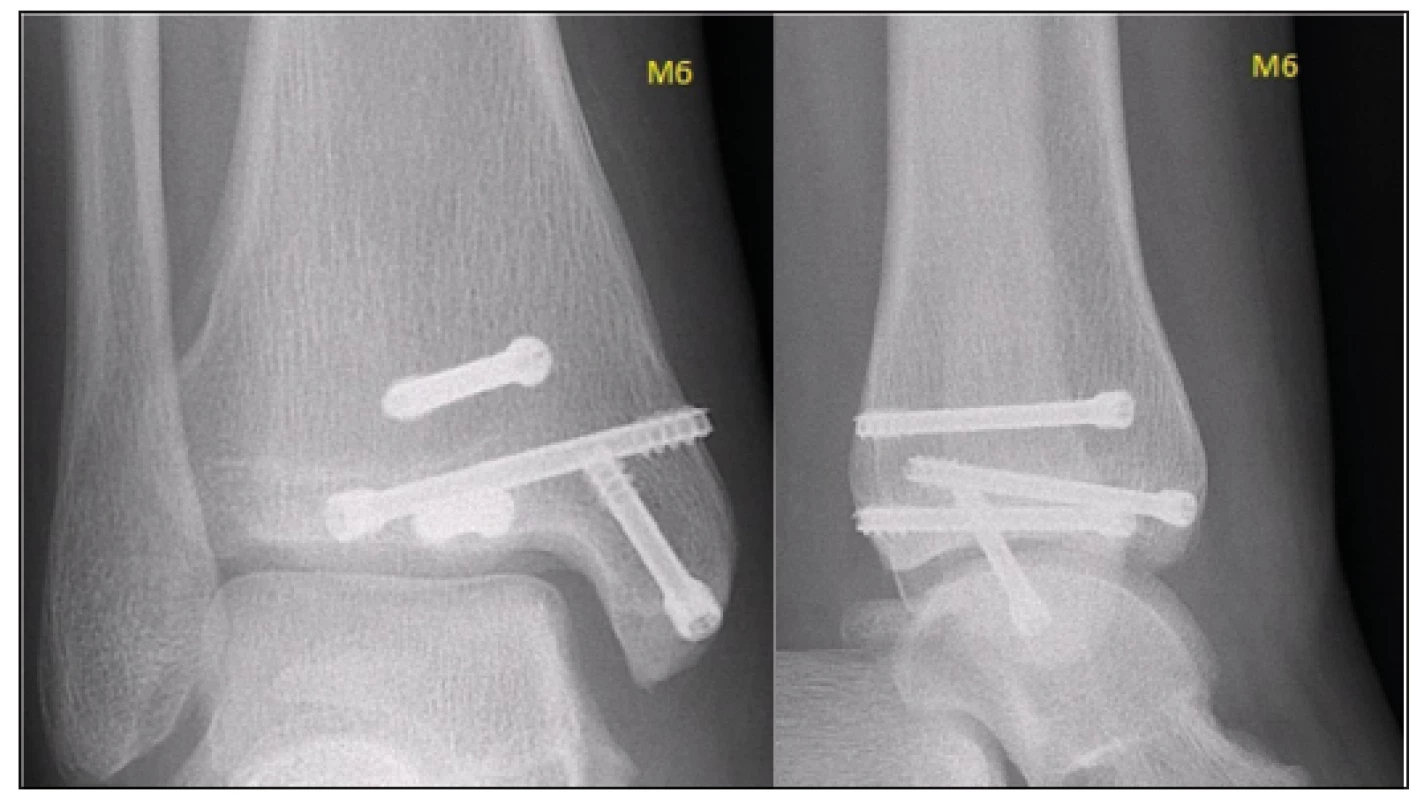
Discussion
The presented case report clearly demonstrates the advantages of arthroscopy-assisted osteosynthesis, which, contrary to the technique of percutaneous fixation, enables perioperative monitoring of quality of the articular surface reduction and assessing the potential cartilage damage. When compared with open reduction and internal fixation, the risk of damaging the physis, resulting in bone growth disorders, is significantly reduced, together with the risk of post-injury arthrofibrosis [7, 15].
A relative disadvantage of the arthroscopy-assisted osteosynthesis when compared with the open technique is the requirement for specialized instrumentation, more specifically a high-quality arthroscopy tower. Equally important is the erudition of the operating surgeon – arthroscopist. The ideal solution seems to be a centralization of these relatively rare injures to larger centres, with sufficient experience in arthroscopy-assisted osteosyntheses in the area of smaller and larger joints. One of these departments may also be a traumacentre with a well-functioning arthroscopy team.
The risk of preliminary growth plate closure is the greatest with the Salter-Harris fractures type III-IV; however, a clinically relevant preliminary growth plate closure following a triplane fracture is rare, as most patients are already close to bone maturity at the time of injury, and more significant consequences arise from the dislocation of the articular surface, with resulting complications, such as arthrofibrosis or arthritis [1, 2, 14].
Some authors postulate that the risk of preliminary growth plate closure is not influenced by the number of attempts of closed reduction, initial dislocation of the fracture, nor the treatment technique [1, 11]; nevertheless, especially with juvenile fractures and fractures occurring at the transition age, it is necessary to respect the principles of biological treatment and surgery.
Conclusion
Computed tomography plays an irreplaceable role in the preoperative diagnostics of triplane fractures and planning of surgery. The treatment is based upon anatomical reduction of the articular surface under visual control and stable fixation with compression screws. Arthroscopy-assisted osteosynthesis fulfils the requirements of mini-invasiveness, with a preserved possibility of visual control of the reduction, and seems to be a suitable alternative to other techniques. The performance of this procedure is technically and personally demanding, and should be concentrated into specialized departments.
MUDr. Jakub Malý
Zdroje
- BARMADA, A., GAYNOR, T, MUBARAK, SJ. Premature physeal closure following distal tibia physeal fractures: a new radiographic predictor. J Pediatr Orthop. 2013, 32, 733–739. ISSN 1539-2570
- DENNING, JR. Complications of Pediatric Foot and Ankle Fractures. Orthop Clin N Am. 2017, 48, 59–70. ISSN 0030-5898/17
- HORNER, K., TAVAREZ, M. Pediatric Ankle and Foot Injuries. Clinical Pediatric Emergency Medicine. 2016, 17, 38–52. ISSN 1522-8401
- JOHN, L Abt., VINOD, KP. Triplane fracture, Medscape. last update May 01 2017,[cit. 2018-08-10]. Anglická verze. Dostupná z WWW: <https://emedicine.medscape.com/article/1269816-overview>
- KAY, RM., MATTHYS, GA. Pediatric ankle fractures: evaluation and treatment. J Am Acad Orthop Surg. 2001, 9, 268–278. ISSN 1940-5480
- KLING Jr, TF., BRIGHT, RW., HENSINGER, RN. Distal tibial physeal fractures in children that may require open reduction. J Bone Joint Surg Am. 1984, 66, 647–657. online ISSN 1535-1386
- McGILLION, S., JACKSON, M., LAHOTI, O. Arthoscopically assisted percutaneous fixation of triplane fracture of the distal tibia. J Pediatr Orthop B. 2007, 16, 313–316. online ISSN 1473-5865
- NENOPOULOS, A. et al. The role of CT in diagnosis and treatment of distal tibial fractures with intra-articular involvement in children. Injury Int J Care Injured. 2015, 46, 2177–2180. ISSN 0020-1383
- PEŠL, T., HAVRÁNEK, P. Etiopatogeneza zlomenin hlezna přechodného období. Úraz chir. 2010, 18, 41–45. ISSN 1211-7080
- RAPARIZ, JM., OCETE, G., GONZALEZ-HERRANZ, P. et al. Distal tibial triplane fractures: long term follow-up. J Pediatr Orthop. 1996, 16, 113–118. online ISSN 1539-2570
- RUSSO, F., MOOR, MA., MUBARAK, SJ. et al. Salter Harris II fracture of the distal tibia: does surgical management reduce the risk of premature physeal closure? J Pediatr Orthop. 2013, 33, 524–529. online ISSN 1539-2570
- SHIN, AY., MORAN, ME., WENGER, DR. Intramalleolar triplane fractures of the distal tibial epiphysis. J Pediatr Orthop. 1997, 17, 352–355. online ISSN 1539-2570
- SCHNETZLER, KA., HOERNSCHEMEYER, DE. The pediatric triplane ankle fracture. J Am Acad Orthop Surg. 2007, 15, 738–747. online ISSN 1940-5480
- SPIEGEL, PG., COOPERMAN, DR., LAROS, GS. Epiphyseal fractures of the distal esnd of the tibia and fibula. A retrospective study of two hundred and thirty-seven cases in children. J Bone Joint Surg Am. 1978, 60, 1046–1050. online ISSN 1535-1386
- WHIPPLE, TL., MARTIN, DR. et al. Arthroscopic Treatment of Triplane Fractures of the Ankle. Arthroscopy: The Journal of Arthroscopic and Related Surgery. 1993, 9, 456–463. ISSN 0749-8063
- WUERZ, TH., GURD, DP. Pediatric physeal ankle fracture. J Am Acad Orthop Surg. 2013, 21, 234–244. online ISSN 1940-5480
Štítky
Chirurgia všeobecná Traumatológia Urgentná medicína
Článok vyšiel v časopiseÚrazová chirurgie
Najčítanejšie tento týždeň
2018 Číslo 1- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Kombinace metamizol/paracetamol v léčbě pooperační bolesti u zákroků v rámci jednodenní chirurgie
- Antidepresivní efekt kombinovaného analgetika tramadolu s paracetamolem
- Srovnání analgetické účinnosti metamizolu s ibuprofenem po extrakci třetí stoličky
- Možnosti využití metamizolu v léčbě akutních primárních bolestí hlavy
Najčítanejšie v tomto čísle- Surgical treatment of diaphyseal humeral fractures
- Developmental morphology of the elbow joint in relation to injuries of the paediatric skeleton
- Post-traumatic peritonitis
- Arthroscopy-assisted osteosynthesis of triplane fracture – case report
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



