-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
The effect of smoking and elderly age on digital replantation – a multivariate analysis
Authors: M. Makeľ 1,2; A. Sukop 1; P. Waldauf 3
; A. Whitley 4,5; A. Hora 6; R. Kaiser 7
Authors place of work: Department of Plastic Surgery, University Hospital Královské Vinohrady, Third Faculty of Medicine, Charles University, Prague, Czech Republic 1; Department of Anatomy, First Faculty of Medicine, Charles University, Prague, Czech Republic 2; Department of Anaesthesia and Intensive Care Medicine, University Hospital Královské Vinohrady, Third Faculty of Medicine, Charles University, Prague, Czech Republic 3; Department of Surgery, University Hospital Královské Vinohrady, Third Faculty of Medicine, Charles University, Prague, Czech Republic 4; Department of Anatomy, Second Faculty of Medicine, Charles University, Prague, Czech Republic 5; Third Faculty of Medicine, Charles University, Prague, Czech Republic 6; Department of Neurosurgery and Neurooncology, First Faculty of Medicine, Charles University and Military University Hospital Prague, Czech Republic 7
Published in the journal: ACTA CHIRURGIAE PLASTICAE, 65, 2, 2023, pp. 54-58
doi: https://doi.org/10.48095/ccachp202354Introduction
Traumatic digital amputations are becoming more frequent in elderly patients due to increasing life expectancy and population aging [1,2]. Although digital amputations bring functional and psychological problems to every age group, it is often questioned among plastic surgeons whether to perform a replantation in elderly patients or not [3]. On one hand, replantation may provide improvements to the quality of life; on the other hand, there is a higher rate of comorbidities in this patient group, which may lead to microvascular changes in the digits resulting in replantation failure [4,5].
Old age alone as a risk factor for replantation failure is not mentioned in the official indication criteria. Nonetheless, as it is sometimes considered to be a reason for not performing replantation because of its association with a higher incidence of comorbidities [5,6].
Smoking is also considered by many surgeons to be a predictive factor of necrosis [7] despite contradictory results in the literature [4,8,9].
To evaluate the effect of both of these factors on replantation failure and thus to clarify their role in surgical decision making, we performed a retrospective, single centre study of patients who underwent replantation after traumatic finger amputations.
Methods
Study characteristics
We divided patients into two groups according to age. Group A consisted of patients aged < 60 years and group B consisted of patients aged ≥ 60 years. Group A consisted of 125 (74%) cases and group B consisted of 44 (26%) cases. Successful replantation was defined as intact circulation in the replanted digit at two weeks after surgery without signs of necrosis. Early failure was defined as necrosis at two weeks after surgery.
Long term results were recorded at a minimum of 6 months after surgery and were evaluated with the modified Chen criteria. Chen 1 was defined as a range of motion (ROM) exceeding 60% of normal and complete recovery of sensibility. Chen 2 was defined as a ROM exceeding 40% of normal with nearly complete recovery of sensibility. Chen 3 was defined as a ROM exceeding 30% with partial recovery of sensibility. Chen 4 was defined as viable digit without function.
In cases where additional surgeries were performed (e.g. tenolysis or osteotomy), the Chen criteria were assessed 6 months after the last surgery. Chen 1 and 2 were considered as successful functional results. In two cases delayed necrosis occurred, one patient suffered with severe prolonged osteomyelitis and in one case revision amputation was performed at the request of the patient due to insufficient function. These cases were allocated to the necrosis group.
Surgical procedure, rehabilitation and evaluation of function
Surgical procedures were performed under general anaesthesia or regional anaesthesia. General anaesthesia was preferred for paediatric patients, whereas supraclavicular blocks were used more frequently for elderly patients. The condition of the amputated digit was assessed pre-operatively and important structures were marked under a microscope. Debridement and dissection of the proximal stump followed and the bone fracture was stabilised with two Kirschner wires. Tendon repair was performed before the microscopic part of the surgery. Care was given while dissecting the extensor tendons not to injure the venous structures on the dorsal aspect of amputated finger. Usually, one arterial anastomosis was performed, vein grafts were used if an intimal lesion occurred, which was observed most frequently in crush injuries or ring avulsions. Both peripheral nerves were repaired, and the volar skin was closed. On the dorsal site, two venous anastomoses were performed, and the skin was closed above the anastomoses. After reperfusion, a fish-mouth incision was performed on the apex of the distal phalanx for additional blood outflow as prevention of venous congestion. Patients were monitored in the intensive care unit postoperatively. They received daily unfractionated heparin and acetylsalicylic acid. Frequent controls of perfusion in the replanted digits were performed by trained intensive care unit nurses.
One week after surgery, passive rehabilitation was commenced if no complications occurred. Full active movement began 6 weeks after surgery under the guidance of physiotherapists specialised in hand physiotherapy. ROM and sensitivity (2-point discrimination test) were evaluated 6–12 months after surgery.
Statistical analysis
Fisher’s exact tests were used to compare immediate results (success or failure at 2 weeks) and long-term outcomes (Chen’s criteria at a minimum of 6 months) between the two age groups. Logistic regression multivariate analysis was used to investigate the influence of age, smoking, mechanism of injury and zone of injury on immediate results and long-term outcomes.
Results
Over a 10-year period from 2011 to 2021, a total of 169 replantations of digits of the upper extremity were performed in 118 patients at the Department of Plastic Surgery of the University Hospital Královské Vinohrady in Prague by various microsurgeons. Amputated fingers partially attached to the body and cases of critical ischemia were excluded from the study. Average patient age was 42.18 (± 18.36 SD). Most of the amputated digits were from male patients (151 digits, 89.3%) with only 18 replanted digits (10.7%) in female patients. Ninety-eight cases (58%) were caused by circular saw injuries, 56 (32%) by other sharp objects, eight cases were avulsion injuries, and nine cases (5.3%) were caused by other mechanisms (these included ring amputations and mangled fingers).
Among the 153 cases with known smoking status, 107 (69.9%) were non-smokers and 46 (30.1%) were smokers.
The index finger was the most frequently injured finger (51 cases (30.2%)), followed by the thumb (41 cases (24.3%)), the middle finger (40 cases (23.7%)), the ring finger (26 cases (15.4%)) and the little finger (11 cases (6.5%)). Zone II (T2 for the thumb) was the most common site of amputation, with a total of 119 cases (70.4%). Amputations in zone III occurred in 29 cases (17.2%) and amputations in zone I occurred in 21 cases (12.4%).
Additional surgeries (such as tenolysis and osteotomy) were performed in 40 cases (23.7%).
Comorbidities that could potentially cause vascular changes and lead to surgical complications, such as diabetes mellitus, hypertension, atherosclerosis and hyperlipoproteinemia, were recorded in 120 cases (71.1%).
Short-term outcomes
From the total cohort of 169 replanted digits, 130 (76.9%) survived the first two weeks completely and 39 (23.1%) exerted necrosis. In group A there were 96 cases (76.8%) of successful replantation and 29 cases (23.2%) of early necrosis. In group B there were 34 successful replantations (77.3%) and 10 cases (22.7%) of early necrosis. Univariate analysis comparing both parameters did not show any statistical difference (P = 0.9) between them (Tab. 1).
Tab. 1. Univariate analysis by age (< 60 vs. ≥ 60 years). 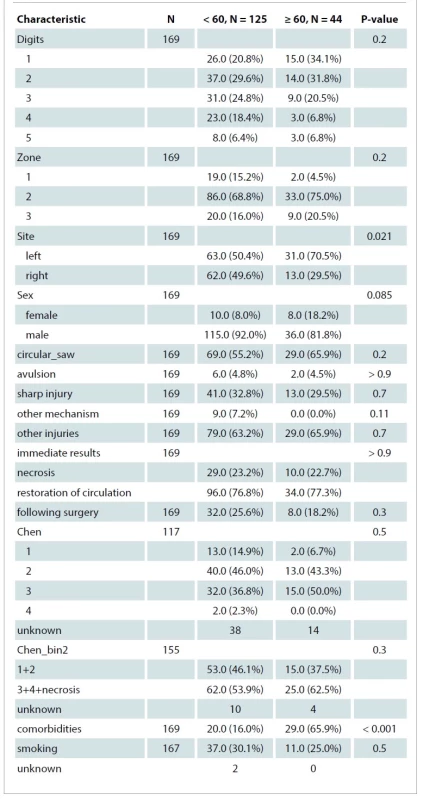
Long-term outcomes
Chen scores 1 and 2, which were considered successful results, were achieved in 53 (46.1%) cases in group A and 15 (37.5) cases in group B. Chen scores 3 and 4, as well as cases of necrosis, occurred in 62 cases (53.9%) in group A and 25 cases (62.5%) in group B. In 14 cases long term outcomes were not available due to loss to follow-up. There was no statistical difference between the two groups when compared using univariate analysis (P = 0.3) (Tab. 1).
Multivariate analysis
The number of comorbidities was significantly different between the two groups (P < 0.001) Multivariable logistic regression analysis revealed that neither smoking nor the age did significantly affect the successful rate in short-term (P = 0.294) or long-term outcomes (P = 0.207) (Fig. 1,2).
Fig. 1. Replantation success rate, short-term outcome (interaction between age and smoking). 
Fig. 2. Replantation success rate, long-term outcome (interaction between age and smoking). 
Discussion
Results of our study supported the opinion that age by itself should not be considered as contraindication to digital replantation, despite an increased frequency of comorbidities in this patient age group.
Gi-Doo Kwon et al. performed a large study on 144 patients aged ≥ 60 years. They found a statistically larger number of cases of necrosis in the age groups 65–69 years and 70–75 years [4]. In our study only five patients were ≥ 65 years, three of them achieved successful restoration of circulation and necrosis occurred in two patients. Concerning long-term results, two out of three patients achieved Chen 3 and one achieved Chen 1. A separate statistical analysis was not performed on these patients due to their small number.
Barzin et al. studied 15,413 digital replantations, among them 616 in patients aged ≥ 60 years and did not find any statistical difference between these patients and the younger patients [3]. However, Haw-Yen Chiu et. al found a significant influence of age on long term results in restoration of sensibility [10].
Prediction of success of digital replantation depends on many complex factors including mechanism of injury, level of amputation, comorbidities and overall patient status [4].
Smoking in the absence of other risk factors should not be considered a contraindication. There was no statistical difference in success rate in immediate results between smokers and non--smokers in our study. This is supported by other various studies [4,8,9]. However, smoking should be prohibited immediately after replantation surgery due to negative effect on the microcirculation [11].
The overall success rate in our study is 76%, which is lower than in other studies, reporting success rates of 80–90% [12,13]. A potential reason for this could be our patient selection. Patients included in the study suffered total amputation, where no connection between the hand and the amputated finger existed. Even small skin, soft tissue or tendinous connection can include small venous drainage and thus help prevent venous congestion [14]. This is the reason why the overall success rate in subtotal amputations is higher than for total amputations [6].
Furthermore, most of the injuries were caused by circular saw with the various extent of soft tissue damage. Damaged arterial margins often require resection, sometimes even venous grafting. Insufficient resection may lead to the vasospasms, thrombosis and replantation failure [15,16].
Concerning long term outcomes, low functional results could be caused by the fact that only 23.1% of patients underwent additional surgeries that can significantly raise the functional status of the replanted finger [17]. The relative low number of zone I replantations is the result of the patient’s desire to perform revision amputation instead of replantation due to the faster return to work. Patients often cannot afford to stay in hospital for longer periods of time required for the therapy after replantation. The desire, expressed after detailed explanation of both procedures, is respected by all surgeons in our department.
This might also be the main cause of low percentage of additional surgeries enhancing the functional outcome of replanted fingers. It requires time for healing and further series of rehabilitation sessions.
Conclusion
Age and smoking should not be considered as decisive factors during decision making. Some studies suggest that up to the age of 65 years, there is no statistical difference in the digit survival rate. However, from the age of 69 years, a higher rate of necrosis may occur. The decision whether to replant or not should be considered individually in every patient with respect to their desires.
Disclosure
There are no conflicts of interest in relation with the theme, creating and publication of this manuscript. There was no financial support during the preparation of the article. All procedures performed in this study involving human participants were in accordance with ethical standards of the institutional and/or national research committee and with the Helsinki declaration and its later amendments or comparable ethical standards.
Roles of authors: Michal Makeľ – author of the manuscript; Adam Hora – data collection; Adam Whitley – manuscript revision, data analysis; Petr Waldauf – statistical analysis; Andrej Sukop – project supervisor.
Michal Makeľ, MD
Šrobárova 50
111 50 Praha 10
Czech Republic
e-mail: makelm@fnkv.cz
Submitted: 9. 10. 2022
Accepted: 12. 6. 2023
Zdroje
1. Beltran-Sanchez H., Soneji S., Crimmins EM. Past, present, and future of healthy life expectancy. Cold Spring Harb Perspect Med. 2015, 5(11): a025957.
2. Chang DH., Ye SY., Chien LC., et al. Epidemiology of digital amputation and replantation in Taiwan: a population-based study. J Chin Med Assoc. 2015, 78(10): 597–602.
3. Barzin A., Hernandez-Boussard T., Lee GK., et al. Adverse events following digital replantation in the elderly. J Hand Surg Am. 2011, 36(5): 870–874.
4. Kwon GD., Ahn BM., Lee JS., et al. The effect of patient age on the success rate of digital replantation. Plast Reconstr Surg. 2017, 139(2): 420–426.
5. Barbary S., Dap F., Dautel G. Finger replantation: surgical technique and indications. Chir Main. 2013, 32(6): 363–372.
6. Soucacos PN. Indications and selection for digital amputation and replantation. J Hand Surg Br. 2001, 26(6): 572–581.
7. Waikakul S., Sakkarnkosol S., Vanadurongwan V., et al. Results of 1018 digital replantations in 552 patients. Injury. 2000, 31(1): 33–40.
8. Nishijima A., Yamamoto N., Yanagibayashi S., et al. The effect of smoking on necrosis rate in digital replantation and revascularization with prostaglandin E1 therapy: a retrospective study. Plast Reconstr Surg. 2016, 138(4): 848–853.
9. He JY., Chen SH., Tsai TM. The risk factors for failure of an upper extremity replantation: is the use of cigarettes/tobacco a significant factor? PLoS One. 2015, 10(10): e0141451.
10. Chiu HY., Shieh SJ., Hsu HY. Multivariate analysis of factors influencing the functional recovery after finger replantation or revascularization. Microsurgery. 1995, 16(10): 713–717.
11. van Adrichem LN., Hovius SE., van Strik R., et al. The acute effect of cigarette smoking on the microcirculation of a replanted digit. J Hand Surg Am. 1992, 17(2): 230–234.
12. Morrison WA., O´Brien BM., MacLeod AM. Evaluation of digital replantation – a review of 100 cases. Orthop Clin North Am. 1977, 8(2): 295–308.
13. Weiland AJ., Villarreal-Rios A., Kleinert HE., et al. Replantation of digits and hands: analysis of surgical techniques and functional results in 71 patients with 86 replantations. Clin Orthop Relat Res. 1978, 133 : 195–204.
14. Lindfors N., Raatikainen T. Incidence, epidemiology, and operative outcome of replantation or revascularisation of injury to the upper extremity. Scand J Plast Reconstr Surg Hand Surg. 2010, 44(1): 44–49.
15. Regas I., Saizonou I., Pichonnat M., et al. Influence of the level of arterial resection on the replanting and revascularization results in hand surgery: prospective study over 22 months. Hand Surg Rehabil. 2021, 40(5): 660–669.
16. Sebastin SJ., Chung KC. A systematic review of the outcomes of replantation of distal digital amputation. Plast Reconstr Surg. 2011, 128(3): 723–737.
17. Sabapathy SR., Bhardwaj P. Secondary procedures in replantation. Semin Plast Surg. 2013, 27(4): 198–204.
Štítky
Chirurgia plastická Ortopédia Popáleninová medicína Traumatológia
Článok vyšiel v časopiseActa chirurgiae plasticae
Najčítanejšie tento týždeň
2023 Číslo 2- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Kombinace metamizol/paracetamol v léčbě pooperační bolesti u zákroků v rámci jednodenní chirurgie
- Antidepresivní efekt kombinovaného analgetika tramadolu s paracetamolem
- Srovnání analgetické účinnosti metamizolu s ibuprofenem po extrakci třetí stoličky
- Metamizol v terapii akutních bolestí hlavy
-
Všetky články tohto čísla
- Healthy and functional hand – the miracle of evolution
- The effect of smoking and elderly age on digital replantation – a multivariate analysis
- Outcome measurement in hand surgery – a brief overview
- Electrical burns in adults
- Median nerve entrapments in the forearm – a case report of rare anterior interosseous nerve syndrome
- Objective and subjective assessment of Dupuytren's contracture
- Advantages of simultaneous radial nerve and tendon reconstruction – a case report
- CORRIGENDUM
- Data on paediatric burn mortality from a single centre over 32 years
- Roman Bánsky (ed.): Clefts
- Addressing the obesity challenge in plastic surgery – the role of liraglutide
- Acta chirurgiae plasticae
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Electrical burns in adults
- Objective and subjective assessment of Dupuytren's contracture
- The effect of smoking and elderly age on digital replantation – a multivariate analysis
- Median nerve entrapments in the forearm – a case report of rare anterior interosseous nerve syndrome
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



