-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Delivery modes and the neonatal outcomes of low birth-weight neonates in a Brazilian reference health center
Neonatální výsledky u novorozenců nízké porodní hmotnosti v brazilském referenčním centru polikliniky
Cíl:
Tato studie srovnává neonatální výsledky u novorozenců s nízkou porodní hmotností narozených buď císařským řezem, nebo vaginálně.Typ studie:
Retrospektivní kohortová studie.Název a sídlo pracoviště:
Maternity of Hospital – Irmandade Santa Casa de Misericórdia de São Paulo, Brazílie.Metodika:
Analýza zahrnuje živě rozené novorozence z jednočetného těhotenství s porodní váhou <2000 g z období od října 1999 do července 2013. Informace o časném novorozeneckém období, stejně tak jako informace o Apgar skóre v 1. a 5. minutě života byly získány z databáze novorozenecké jednotky intenzivní péče.Výsledky:
Všech 830 novorozenců bylo zařazeno na základě kritérií pro danou studii. Z celkového počtu 830 narozených dětí se 519 (62,5%) novorozenců narodilo císařským řezem a 311 (37,5%) novorozenců bylo porozeno vaginálně. Byl zjištěn statisticky významný rozdíl ve výskytu novorozeneckých komplikací, a to s lepšími výsledky u novorozenců narozených vaginálně. Výjimkou byla skupina novorozenců o porodní hmotnosti pod 1500 g. V této skupině váhové kategorie byl vyšší výskyt krvácení do mozku a úmrtí před propuštěním z nemocnice. Rovněž byl vyšší výskyt syndromu respirační tísně a intraventrikulárního krvácení u novorozenců narozených vaginálně, a to ve všech hmotnostních kategoriích. Při srovnání Apgar skóre byl statisticky významný rozdíl mezi způsobem vedení porodu s lepšími výsledky u dětí narozených vaginálně. S výjimkou skupiny novorozenců o porodní hmotnosti nižší než 1000 g, kde byly zjištěny opačné výsledky.Závěr:
U novorozenců váhové kategorie 1000–2000 g nebyl zjištěn přínos porodu císařským řezem. Nicméně benefit z císařského řezu byl pozorován u novorozenců ve váhové kategorii méně než 1000 g.Klíčová slova:
vaginální porod, císařský řez, nízká porodní hmotnost, intrakraniální krvácení, syndrom respirační tísně
Authors: R. Negrini *; L. C. Assef *; Da Silva Costa F.†; Araujo Júnior E.§
Authors place of work: Department of Gynecology and Obstetrics, Hospital da Irmandade Santa Casa de Misericórdia de São Paulo, São Paulo-SP, Brazil † Department of Perinatal Medicine, Royal Women’s Hospital, and Department of Obstetrics and Gynecology, University of Melbourne, *
Published in the journal: Ceska Gynekol 2015; 80(5): 366-371
Summary
Objective:
This study compared the neonatal results of low weight neonates born by cesarean and vaginal delivery.Design:
A retrospective cohort study.Setting:
Maternity of Hospital - Irmandade Santa Casa de Misericórdia de São Paulo, Brazil.Methods:
The analysis included the neonates born alive, of unique pregnancy, <2000 g from October 1999 to July 2013. To obtain the information about the neonatal period, as well as their Apgar score in the 1st and 5th min of life, a search in the database of a neonatal intensive care unit was performed.Results:
In total, 830 neonates were included as per the study criteria. Of these, 519 (62.5%) were born by cesarean delivery and 311 (37.5%) by vaginal delivery. There was a statistically significant difference in the incidence of neonatal complications, with better results in the neonates born by vaginal delivery, except for the group with neonates <1500 g. In this group, there was a higher incidence of intracranial hemorrhage and death before discharge from the hospital. There was also a higher incidence of respiratory distress syndrome and intraventricular hemorrhage in neonates born by vaginal delivery, in all weight groups. Comparing the Apgar scores, there was a statistically significant difference between the delivery modes, with better results observed in the ones born by vaginal delivery. However, the opposite was observed in the group with neonates <1000 g.Conclusion:
There was no indication of cesarean delivery benefits in neonates 1000–2000 g. However, the opposite was observed when the neonates were <1000 g.Keywords:
vaginal delivery, caesarean section, low birth weight, intracranial hemorrhage, respiratory distress syndromeINTRODUCTION
Low birth-weight is associated with a series of neonatal complications [16], particularly in neonates weighing <1500 g. Particularly important complications are intraventricular hemorrhage, respiratory distress syndrome, necrotizing enterocolitis, and neonatal death [9].
The delivery mode is considered responsible for some of these complications, and therefore the rate of cesarean delivery (CD) has greatly increased over the last two decades, especially in the case of low birth-weight neonates. In the United States, since 2005, more than half of all low birth-weight neonates were born by CD [10]. According to Deulofeut et al. [2], there is an association between CD and better neonate perinatal results. In contrast, in a retrospective non-randomized cohort study, Werner et al. [16] concluded that neonates delivered by CD had a higher incidence of respiratory distress syndrome and a lower Apgar score at 5 min than at 7 min, as compared with those born by vaginal delivery (VD) (odds ratio = 1.49, 95% confidence interval = 1.25–1.76; and odds ratio = 1.42, 95% confidence interval = 1.07–1.87, respectively). These results show uncertainty about the benefits of CD.
Many other studies have compared the perinatal results of very low birth-weight (<1500 g) neonates born by VD and CD, with conflicting results regarding the possible occurrence of intraventricular hemorrhage and neonatal death [8, 11, 14, 17]. Durie et al. [3], for example, reported that the rates of intraventricular hemorrhage, necrotizing enterocolitis, and neonatal death, did not differ significantly between neonates born by VD or CD.
Because there is no apparent consensus in the literature regarding the best delivery mode for low weight neonates, the present study investigated the relationship between delivery mode and neonatal outcome in neonates weighing ≤2000 g. The evaluated outcomes were the Apgar score, and the incidence of respiratory distress syndrome, intracranial hemorrhage, necrotizing enterocolitis, and neonatal death during the first days of life.
MATERIALS AND METHODS
Data from the neonates born alive, singletons, weighing <2000 g, and born by VD and CD, from October 1999 to July 2013 (n = 1343), was obtained from the medical records of the Maternity of Hospital da Irmandade Santa Casa de Misericórdia de São Paulo. Their Apgar scores at the 1st and 5th min of life were also obtained from this database. The results for the neonatal period were obtained from the database of the neonatal intensive care unit (NICU) of the same institution.
The exclusion criteria were as follows: neonates with known congenital anomalies (n = 54) and birth weight <800 g (n = 173), due to the possibility that the delivery modes would increase the mortality and morbidity of these neonates in an independent manner. Cases where the data of interest, such as hospital discharge date, Apgar score, and gestational age, was missing from the database (delivery books and summary chart for neonates in the NICU), were also excluded (n = 286).
To improve the data analysis, the gestational age of each neonate was summarized as weeks. For example, a neonate with 31 weeks and 5 days was considered to be in the 31st week.
The birth weight was stratified into groups according to the classification of the World Health Organization (WHO) as follows: neonates weighing <2000 g (low birth weight, LBW), neonates weighing 1000–1500 g (very low birth weight, VLBW), and neonates weighing 800–1000 g (extremely low birth weight, ELBW). In addition, according to the WHO parameters, the neonates were classified either as preterm, when their gestational age was <37 weeks, or as term, when their age was ≥37 weeks. The new Ballard method was used to calculate the gestational age. The outcomes of interest were neonatal death before discharge, neonatal respiratory distress syndrome, intraventricular hemorrhage, and necrotizing enterocolitis.
For the statistical comparisons between the delivery modes, neonatal weight groups, and gestational age, the outcomes of interest were divided into categorical variables and analyzed with the likelihood ratio test. The scale variables, the Apgar score at the 1st and 5th min of life, were analyzed using the Mann–Whitney and Kruskal–Wallis tests, with the significance level set at 5 %. The MS-Excel-2010 spreadsheet software (Microsoft Corp., Redmond, WA, USA) was used to organize the data and the IBM SPSS (Statistical Package for Social Sciences) software, version 21.0 (SPSS Inc., Chicago, IL< USA), was used for the statistics.
RESULTS
Of the 830 neonates included in the present study, 519 (62.5%) were born by CD and 311 (37.5%) by VD. Table 1 compares the variables of interest (respiratory distress syndrome, necrotizing enterocolitis, intraventricular hemorrhage, absence of any of these variables, and whether the neonate was alive or died upon discharge), according to the delivery mode and neonatal weight group. The results showed a significant difference (p < 0.05) in the incidence of these neonatal complications, with a better overall outcome for neonates born by VD, except for the group weighing <1500 g. In this group, there was a higher incidence of intracranial hemorrhage, and death before discharge. There was also a higher incidence of the joint occurrence of respiratory distress syndrome and intracranial hemorrhage among neonates born by VD, in all weight groups.
Table 2 shows that the sample was homogeneous regarding weight, with no significant differences regarding the Apgar scores at the 1st and 5th min of life between VD and CD.
Table 3, which compares the Apgar scores at the 1st and 5th min of life in relation to the delivery mode, shows a significant difference between groups, with better results for neonates born by VD, except for the group weighing <1000 g.
Table 4 shows that there was no significant difference between the modes of delivery and gestational age.
Tab. 1. Incidence of neonatal complications, according to the delivery mode and neonatal weight group 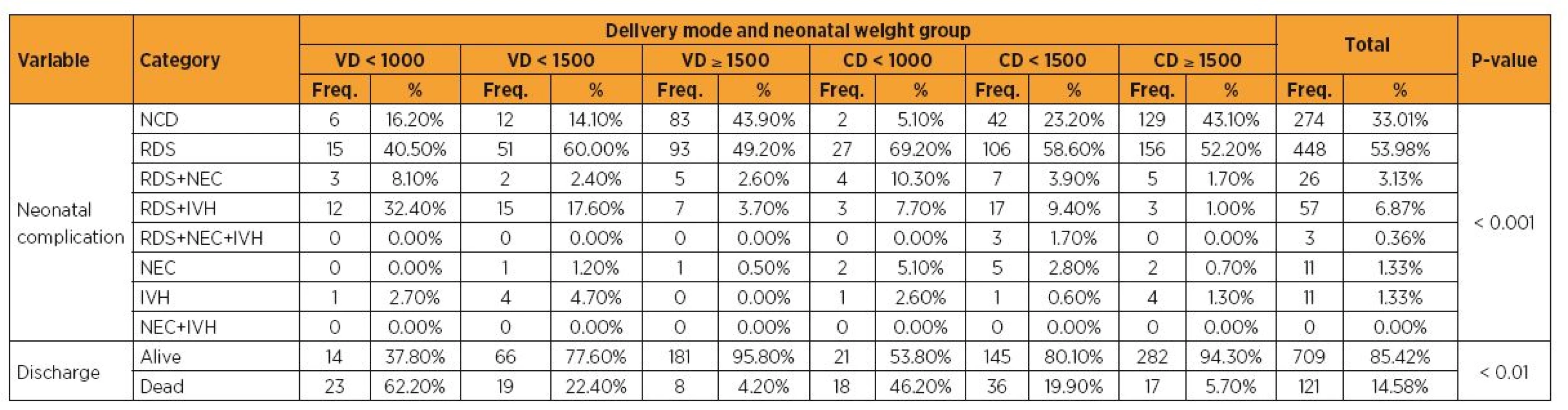
VD = vaginal delivery; CD = cesarean delivery; NCD = no complications detected; RDS = respiratory distress syndrome; NEC = necrotizing enterocolitis; IVH = intraventricular hemorrhage; <1000 = weight between 800 and 1000 g; <1500 = weight between 1000 and 1500 g; ≥ 1500 = weight between 1500 and 2000 g Tab. 2. Neonate weight and Apgar scores, according to the delivery mode 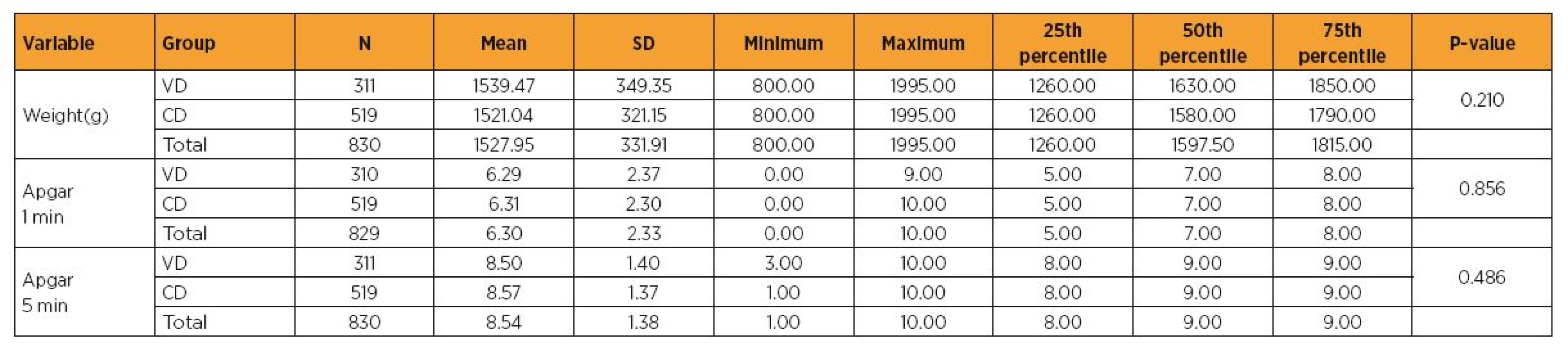
VD = vaginal delivery; CD = cesarean delivery; Apgar 1 min = Apgar score at the 1st min of life; Apgar 5 min = Apgar score at the 5th min of life. Tab. 3. Comparison of the Apgar scores at the 1st and 5th min of life, according to delivery mode and neonate weight group 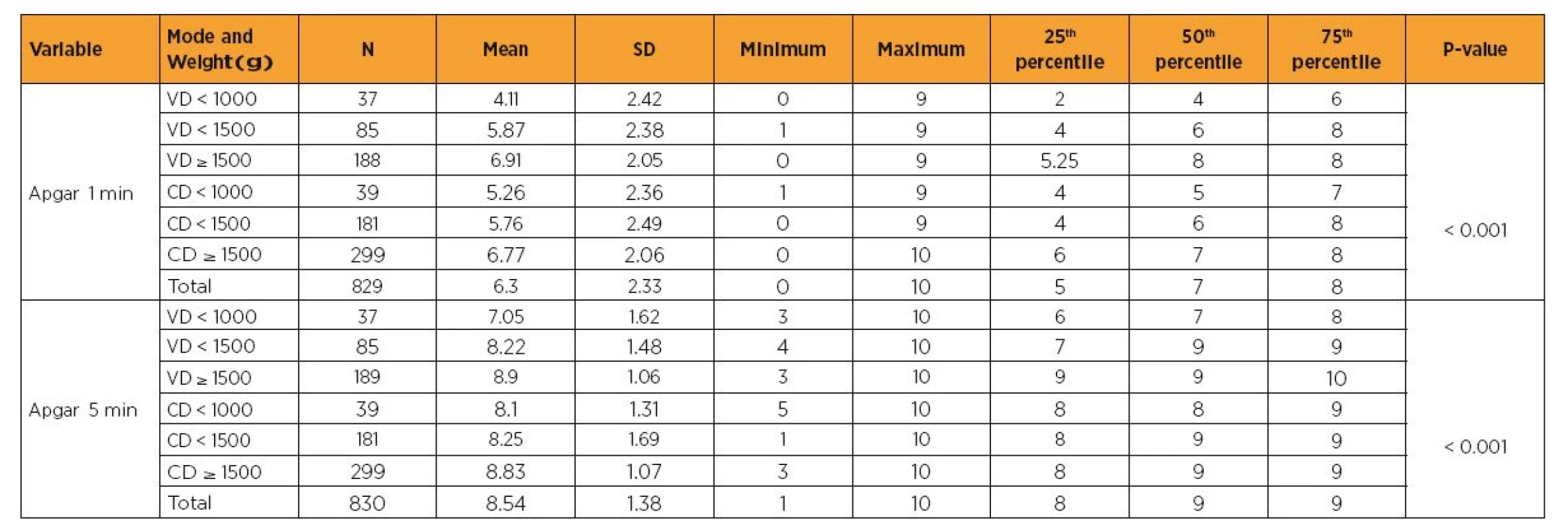
VD = vaginal delivery; CD = cesarean delivery; Apgar 1 min = Apgar score at the 1st min of life; Apgar 5 min = Apgar score at the 5th min of life. Tab. 4. Delivery modes (vaginal and cesarean) versus gestational age 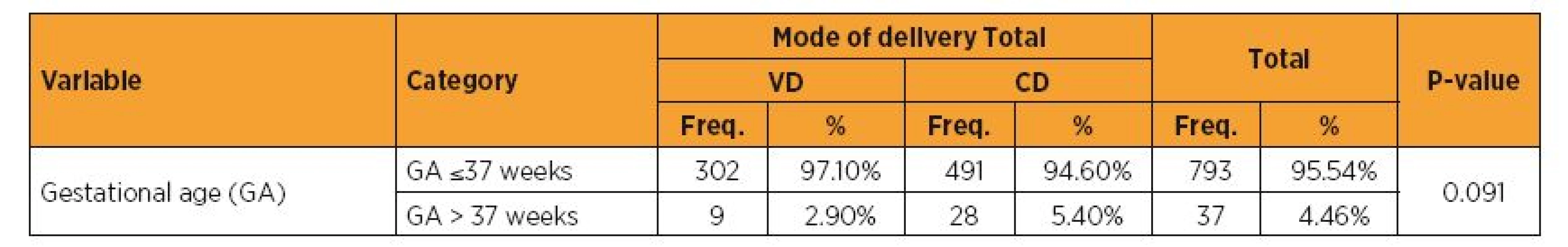
VD = vaginal delivery; CD = cesarean delivery; GA = gestational age; GA ≤ 37 = preterm; GA > 37 = term. DISCUSSION
Low birth-weight is an important risk factor of neonatal complications. The present results show that, in general, neonates born by VD had better results, as also reported in previous studies [4, 6, 17]. However, neonates weighing <1500 g had a higher incidence of intracranial hemorrhage and a lower survival rate, when born by VD. Accordingly, Deulofeut et al. [2] reported an association between VD and an increased risk of intracranial hemorrhage in VLBW neonates. The occurrence of intracranial hemorrhage seems to be related to the immaturity of cerebral flow self-regulation, and to the fragility of the vascular bed matrix [5, 13], although the role of trauma cannot be excluded [1].
Wylie et al. [17] reported, in a review study, that CD was not related to a higher survival of VLBW neonates, as compared to VD, as observed in the present study. These results, in turn, contrasted with those published by Lee and Gould [8], who detected a higher survival after CD in the same weight group.
In another study, the risks of respiratory distress syndrome and fetal hypoxia (Apgar score lower than 7 at the 5th min of life) did not differ significantly between VD and CD [15]. This differed in part from the present study, in which we detected a higher incidence of respiratory distress syndrome among neonates born by CD. This was an expected outcome, considering that hormonal and physiological changes associated with labor are necessary for pulmonary maturation. However, no significant difference was detected in the same group regarding their Apgar scores. However, Heinzmann et al. [7] who analyzed 2073 births with gestational age > 38 weeks found higher incidence of respiratory distress syndrome and admission in the NICU following CD.
The incidence of necrotizing enterocolitis was higher among neonates born by CD in all weight groups, reinforcing the better results seen in VD.
We performed an analysis to determine whether the gestational age was related to the occurrence of complications. Of the 830 neonates studied, 793 (95.54%) were preterm and the remaining ones were born at term, i.e., there was no significant incidence of neonates with fetal growth restriction, reducing this bias.
We observed lower mortality in neonates weighing <1000 g delivered vaginally. This result is in agreement with the study conducted by Minguez-Milio et al. [6] who analyzed 138 newborns <1000 g , 73 following CD and 65 VD, and the rate of mortality was higher in VD (49.3%) vs. CD (23.1%).
In summary, the above analyses indicate that CD is not beneficial for neonates weighing from 1000 to 2000 g, in contrast to what was observed in neonates weighing <1000 g.
Address for correspondence:
Prof. Edward ARAUJO JÚNIOR, PhD.
Department of Obstetrics, Paulista School of Medicine – Federal University of São Paulo (EPM-UNIFESP)
Rua Belchior de Azevedo, 156, apto. 111 Torre Vitoria
São Paulo–SP, Brazil
CEP 05089-030
e-mail: araujojred@terra.com.br
Zdroje
1. Antoniuk, S., da Silva, RV. Periventricular and intraventricular hemorrhage in the premature infants. Rev Neurol, 2000, 31, p. 238–243.
2. Deulofeut, R., Sola, A., Lee, B., et al. The impact of vaginal delivery in premature infants weighing less than 1,251 grams. Obstet Gynecol, 2005, 105, p. 525–531.
3. Durie, DE., Sciscione, AC., Hoffman, MK., et al. Mode of delivery and outcomes in very low-birth-weight infants in the vertex presentation. Am J Perinatol, 2011, 28, p. 195–200.
4. Ghi, T., Maroni, E., Arcangeli, T., et al. Mode of delivery in the preterm gestation and maternal and neonatal outcome. J Matern Fetal Neonatal Med, 2010, 23, p. 1424–1428.
5. Gould, SJ., Howard, S. An immunohistochemical study of the germinal matrix in the late gestation human fetal brain. Neuropathol Appl Neurobiol, 1987, 13, p. 421–437.
6. Haque, KN., Hayes, AM., Ahmed, Z., et al. Caesarean or vaginal delivery for preterm very low - birth weight (< or =1,250 g) infant: experience from a district general hospital in UK. Arch Gynecol Obstet, 2008, 277, p. 7–12.
7. Heinzmann, A., Brugger, M., Engels, C., et al. Risk factors of neonatal respiratory distress following vaginal delivery and caesarean section in the German population. Acta Paediatr, 2009, 98, p. 25–30.
8. Lee, HC., Gould, JB. Survival rates and mode of delivery for vertex preterm neonates according to small - or appropriate-for-gestational-age status. Pediatrics, 2006, 118, p. e1836–1844.
9. Ljustina, S., Berisavac, II., Berisavac, M., et al. Analysis of intracranial hemorrhage grade in preterm singleton pregnancies delivered vaginally or by cesarean section. Vojnosanit Pregl, 2013, 70, p. 255–258.
10. Menaker, F., Hamilton, BE. Recent trends in cesarean delivery in the United States. 2010. p. 1–8. Avaliable at: www.ncbi.nlm.nih.gov/pubmed/20334736. Retrieved April 9, 2012.
11. Ment, LR., Oh, W., Ehrenkranz, RA., et al. Antenatal steroids, delivery mode, and intraventricular hemorrhage in preterm infants. Am J Obstet Gynecol, 1995, 172, p. 795–800.
12. Minguez-Milio, JA., Alcázar, JL., Aubá, M., et al. Perinatal outcome and long-term follow-up of extremely low birth weight infants depending on the mode of delivery. J Matern Fetal Neonatal Med, 2011, 24, p. 1235–1238.
13. Perlman, JM., McMenamin, JB., Volpe, JJ. Fluctuating cerebral blood flow velocity in respiratory distress syndrome. Relation to the development of intraventricular hemorrhage. N Engl J Med, 1983, 309, p. 204–209.
14. Riskin, A., Riskin-Mashiah, S., Bader, D., et al. Delivery mode and severe intraventricular hemorrahge in single, very low birth weight, vertex infants. Obstet Gynecol, 2008, 112, p. 21–28.
15. Sangkimkamhang, U., Pattanittum, P., Laopaiboon, M., Lumbiganon, P. Mode of delivery and outcomes in preterm births. J Med Assoc Thai, 2011, 94, p. 415–419.
16. Werner, EF., Savitz, DA., Janevic, TM., et al. Mode of delivery and neonatal outcomes in preterm, small-for-gestational-age newborns. Obstet Gynecol, 2012, 120, p. 560–564.
17. Wylie, BJ., Davidson, LL., Batra, M., Reed, SD. Method of delivery and neonatal outcome in very low-birthweight vertex-presenting fetuses. Am J Obstet Gynecol, 2008, 198, p. 640.e1–7.
Štítky
Detská gynekológia Gynekológia a pôrodníctvo Reprodukčná medicína
Článok vyšiel v časopiseČeská gynekologie
Najčítanejšie tento týždeň
2015 Číslo 5- Ne každé mimoděložní těhotenství musí končit salpingektomií
- I „pouhé“ doporučení znamená velkou pomoc. Nasměrujte své pacienty pod křídla Dobrých andělů
- Mýty a fakta ohledně doporučení v těhotenství
- Gynekologické potíže pomáhá účinně zvládat benzydamin
-
Všetky články tohto čísla
- Robot assisted endometrial cancer staging – evaluation the first 100 operations and comparing the first andthe last 30 operations
- Diaphragmatic surgery in advanced ovarian cancer therapy
- Radical fertility preserving surgery of gynaecological malignancies – five-year-old file
- Efficacy of surgical treatment of stress urinary incontinence with mini-invasive single incision sling
- Correlation of subjective and objective assessment of vaginal prolapse surgery – secondary analysis of randomized controlled study in patients with pelvic floor injury treated with vaginal mesh or with sacrospinous ligament fixation
- Mental changes in women due to the use of hormonal contraception
- Histological types of uterine fibroids in reproductive age and postmenopausal women
- Delivery modes and the neonatal outcomes of low birth-weight neonates in a Brazilian reference health center
- Robotic sacrocolpopexy – two case reports and literature overview
- Heterotopic pregnancy after spontaneous conception
- Caesarean scar pregnancy – case report
-
GESTAČNÍ DIABETES MELLITUS
Doporučený postup - Zpráva o International Female Care Academy 2015 (IFCA) pořádané Sekcí gynekologické endokrinologie ČGPS
- Česká gynekologie
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Mental changes in women due to the use of hormonal contraception
- Histological types of uterine fibroids in reproductive age and postmenopausal women
- Heterotopic pregnancy after spontaneous conception
- Diaphragmatic surgery in advanced ovarian cancer therapy
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



