-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Primary signet ring cell adenocarcinoma as a rare cause of colonic stenosis in a young patient with Crohn’s disease – the case report
Kolorektální adenokarcinom z prstenčitých buněk jako vzácná příčina stenózy tlustého střeva u mladých pacientů s Crohnovou chorobou – kazuistika
Karcinom z prstenčitých buněk (signet ring cell carcinoma – SRCC) je vzácný typ vysoce maligního adenokarcinomu, který produkuje mucin a postihuje převážně žaludek, vaječníky a tenké střevo. Primární lokalizace SRCC v tračníku je raritní a prognóza tohoto typu nádoru je vysoce nepříznivá. Prezentujeme kazuistiku 44leté ženy léčené pro Crohnovou chorobou od roku 2000 a poslední tři roky na biologické terapii ustekinumabem s rozvojem klinické, laboratorní a endoskopické remise. Pacientka byla v počátkem roku 2021 došetřována pro nově vzniklé pasážové obtíže, koloskopicky bylo zjištěno stenotické postižení tračníku (sigmatu) a z histologického vzorku verifikován primární kolorektální karcinom z prstenčitých buněk, který v tomto případě klinicky imitoval aktivitu Crohnovy choroby. Vzhledem k metastatickému charakteru postižení již v době diagnózy (játra, pobřišnice) a k přetrvávajícím symptomům poruchy střevní pasáže bylo přistoupeno k ileostomii jako definitivnímu chirurgickému řešení a byla zahájena paliativní chemoterapie. Prognóza pacientky byla infaustní a nemocná zemřela do 5 měsíců od stanovení diagnózy v hospicové péči.
Klíčová slova:
Crohnova choroba – kolorektální karcinom z prstenčitých buněk – nádor tlustého střeva – stenotické postižení tlustého střeva
Authors: B. Pipek- 1 3; K. Prokešová 4; R. Kotásek 5; Martin Štěpán 1
; P. Fojtík 1,3
Authors place of work: Digestive Diseases Centre, Hospital AGEL Ostrava-Vítkovice 1; 2nd Department of Internal Medicine – Gastroenterology and Geriatrics, Faculty of Medicine and Dentistry, Palacky University and University Hospital Olomouc 2; Department of Internal Medicine, Faculty of Medicine, University of Ostrava, Ostrava 3; Department of Pathology, Hospital AGEL Prostějov 4; Department of Radiotherapy and Oncology, Hospital AGEL Nový Jičín 5
Published in the journal: Gastroent Hepatol 2023; 77(1): 21-25
Category: IBD: kazuistika
doi: https://doi.org/10.4895/ccgh202321Summary
Signet ring cell carcinoma (SRCC) is a rare type of highly malignant adenocarcinoma that produces mucin and predominantly affects the stomach, ovaries, and the small intestine. Primary localisation in the colon is rare, and the prognosis of this type of adenocarcinoma is very poor. We present a case report of a 44-year-old woman who suffered from Crohn‘s disease beginning in the year 2000. During the last three years of her treatment, she was treated using biological therapy with ustekinumab. The treatment led to clinical, laboratory, and endoscopic remission. In February 2021, she had widely metastatic primary signet ring cell carcinoma of the colon, which mimicked the IBD activity in the case of her colon obstruction. Because of the extensive infiltration of her liver and peritoneum at the time of the diagnosis, in addition to the symptoms of the passage disorders she was experiencing, she proceeded with an end ileostomy and palliative treatment was started. The patient‘s prognosis was unfavourable, and she died within 5 months of the diagnosis in hospice care.
Keywords:
Crohn‘s disease – primary signet ring cell carcinoma – colon cancer – colonic stenosis
Introduction
Primary signet ring cell adenocarcinoma (PSRCC) of the colon is a rare type of colorectal carcinoma that has a relatively higher incidence in younger patients and is characterised by poor prognosis. Primary localisation in the colon is uncommon, and the diagnosis is often delayed and is associated with an advanced tumour stage. The treatment is usually only palliative with poor response. Histologically speaking, PSRCC is an epithelial malignancy with cells resembling signet rings and a large amount of mucin, which pushes the nucleus to the cell periphery. The association with Crohn‘s disease is described only in rare case reports.
Herein we report a patient with Crohn‘s disease who was diagnosed with signet ring cell carcinoma that was mimicking sigmoid colonic stenosis.
Case presentation
We present the case report of a 44-year--old woman who was treated for corticosteroid-dependent Crohn‘s disease of the terminal ileum and the left colon beginning in 2000. She developed severe acute pancreatitis after azathioprine treatment, and therefore she soon after underwent biologic therapy with infliximab in 2004–2006. This was followed by adalimumab with secondary failure. She was treated using biological treatment with ustekinumab beginning in 2017 with the induction of clinical, laboratory, and endoscopic remission. The last total colonoscopy was performed in February 2020 with complete endoscopic healing (Fig. 1). During a follow-up examination in December 2020, the patient was clinically completely healthy. She had one formed stool a day, stable weight, and even laboratory samples did not show any pathology (CRP 3 mg/l and fecal calprotectin was below 100 µg/g).
Fig. 1. The last total colonoscopy was performed in February 2020 with complete endoscopic healing.
Obr. 1. Poslední úplná koloskopie byla provedena v únoru 2020 s nálezem kompletní ho endoskopického zhojení.
The patient started feeling worse at the beginning of January 2021. She experienced an overall deterioration of her condition, abdominal pain, diarrhoea, and an increase in flatulence. According to her, she was, at the time, taking care of her sick and long-immobile mother, who had been repeatedly hospitalized at an internal medicine ward for Clostridium difficile colitis. The patient’s leukocyte count and CRP (29 mg/l) were increased in laboratory samples. Her stool cultures were negative, but a sample of her stool was positive for clostridium toxin and antigen. The diagnosis was a colonic Clostridium difficile infection, and our patient was treated with orally administered vancomycin with a slight improvement of her condition and regression of diarrhoea. However, abdominal pain and a feeling of abdominal discomfort still persisted. For this reason, we examined fecal calprotectin, which was significantly increased to 2,340 µg/g. Significant bulging of the sigmoid to 10 mm, slightly blurred stratification for a length of 45 mm, and an accumulation of mesenteric fat around the affected section of the sigma was evident from bowel sonography. Soon after, a colonoscopy was ordered, and the patient was treated with systemic corticosteroids (methylprednisone) at a dose of 1 mg/kg due to the alleged relapse of Crohn‘s disease. After 4 days of corticosteroid treatment, the patient came to the hospital showing symptoms of an acute bowel obstruction. An X-ray of her abdomen was performed on the day of her admission (Fig. 2). Pneumatosis was found in the left part of her colon with signs of ileus and empty content in the right part of the colon. At the same time, her COVID-19 PCR saline gargle test performed at the beginning of her admission to the hospital came back positive. The patient was asymptomatic, but she had to be quarantined in a COVID ward. The patient was monitored by the surgical department, and she was treated conservatively with infusions and prokinetics with general improvement. An early colonoscopy was performed, which showed tight filiform stenosis of the sigmoid that was not permeable to the endoscope; nor was it possible to introduce a dilation balloon (Fig. 3). The stenosis was biopsied, followed by a computer tomography scan of the abdomen. Additional laboratory tests included carcinoembryonic antigen (CEA) and CA 19-9. The CT scan surprisingly showed massive ascites in the abdominal cavity with highly suspected tumour lesions of the peritoneum, thickening of the left colon wall with increased dilation of the colon proximal to the area of sigmoid, and still the same persistent ileus status (Fig. 4). No abscess was detected. Additional tumour markers were present, consisting of significant positivity of CEA above 100 g/l, and malignant cells with a level of CEA above 1,000 g/l found in cytological examinations from ascites liquid. The early result of the biopsy histological examination from the sigmoid stenosis showed poorly differentiated adenocarcinoma with areas of mucin production and signet ring cells infiltrating the lamina propria of the colon. The immunohistochemical analysis of the tumour had a positive staining pattern for cytokeratin 20 and a negative pattern for cytokeratin 7 (Fig. 5a, b). According to the TNM stag-ing classification, the neoplasm of the sigmoid was classified as stage IV cT3, cN1, M1 (PER), grade 3, RAS wild-type, BRAF mutation negative. Our patient was presented to the oncological-surgical-gastroenterological board with a proposal for further treatment. An axial ileostomy was performed due to extensive peritoneal dissemination. Palliative chemotherapy with the FOLFOX regimen (folinic acid, fluorouracil, and oxaliplatin) was initiated in April 2021. However, the patient could not eat or drink due to the chronic ileus despite the stoma. She repeatedly vomited and lost weight leading to a deterioration of her physical condition. A home parenteral infusion was agreed on, and the patient and her husband were educated accordingly so they could start this type of parenteral nutrition as soon as possible.
Fig. 2. X-ray image of abdomen with ileus sign.
Obr. 2. Prostý rentgenový snímek břicha s nálezem ileózního stavu.
Fig. 3. An early colonoscopy, which showed tight fi liform stenosis of the sigmoid that was not permeable to the endoscope.
Obr. 3. Časná koloskopie, která prokázala těsnou filiformní stenózu sigmatu neprostupnou pro endoskop.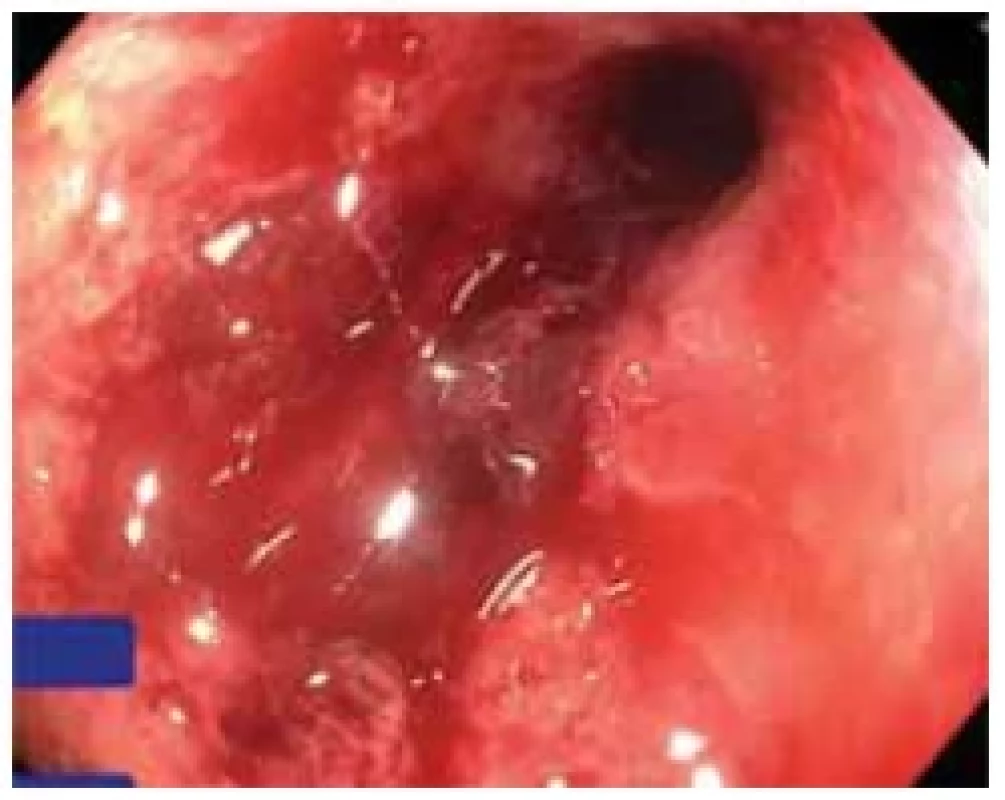
Fig. 4. The CT scan surprisingly showed massive ascites in the abdominal cavity with highly suspected tumour lesions of the peritoneum and hepar and confirmed wall thickening of colon sigmoideum.
Obr. 4. CT sken překvapivě ukázal masivní ascites v dutině břišní s vysoce suspektním metastatickým postižením pobřišnice a jater a potvrdil známé postižení stěny sigmatu.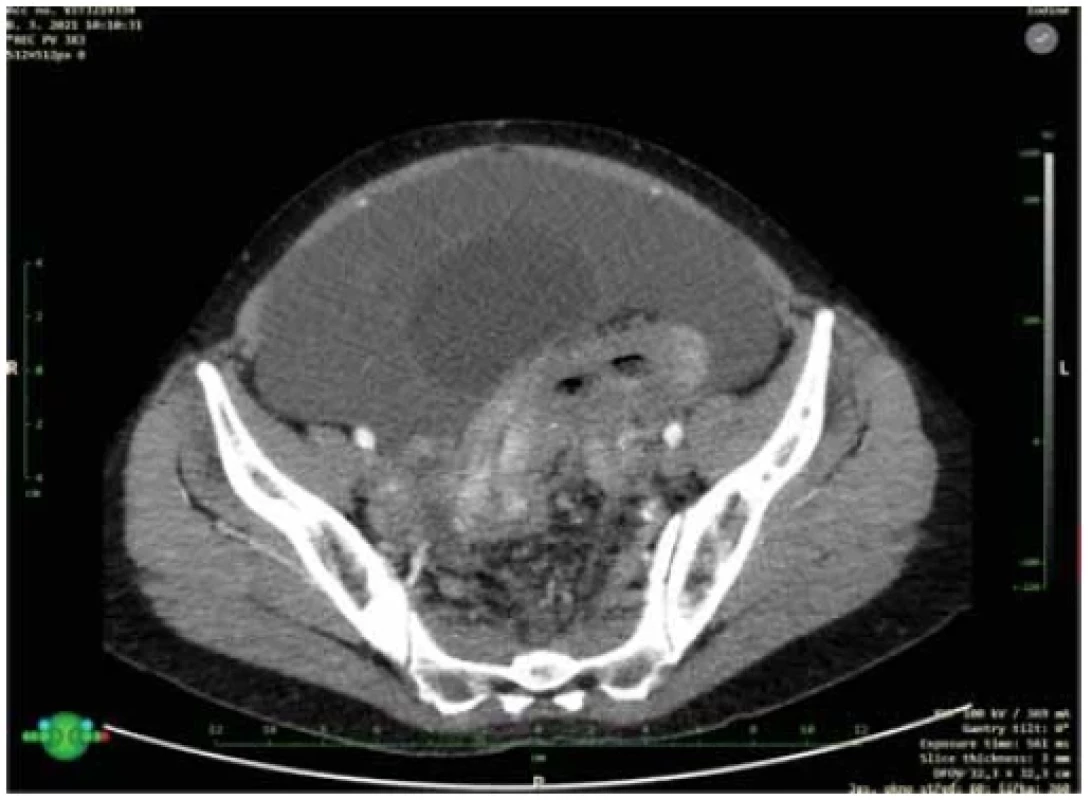
Fig. 5. a) Histopathologic examination of colonic biopsy. Haematoxylin and eosin staining of the tissue with mucin producing poorly diff erentiated adenocarcinoma in muscularis propria with signet ring cell features. Enlargement 40×.
Fig. 5b) Histopathologic examination of colonic biopsy. Alcian blue staining of the mucin producing poorly diff erentiated adenocarcinoma in muscularis propria with signet ring cell features. Enlargement 40×.
Obr. 5a) Histopatologické zhodnocení střevní biopsie. Barvení hematoxylinem a eosinem. Záchyt nízce diferencovaného mucin produkujícího adenokarcinomu v lamina muscularis propria s buňkami tvaru „pečetního prstene“. Zvětšení 40×.
Obr. 5b) Histopatologické zhodnocení střevní biopsie. Barvení alciánová modř. Záchyt nízce diferencovaného mucin produkujícího adenokarcinomu v lamina muscularis propria s buňkami tvaru „pečetního prstene“. Zvětšení 40×.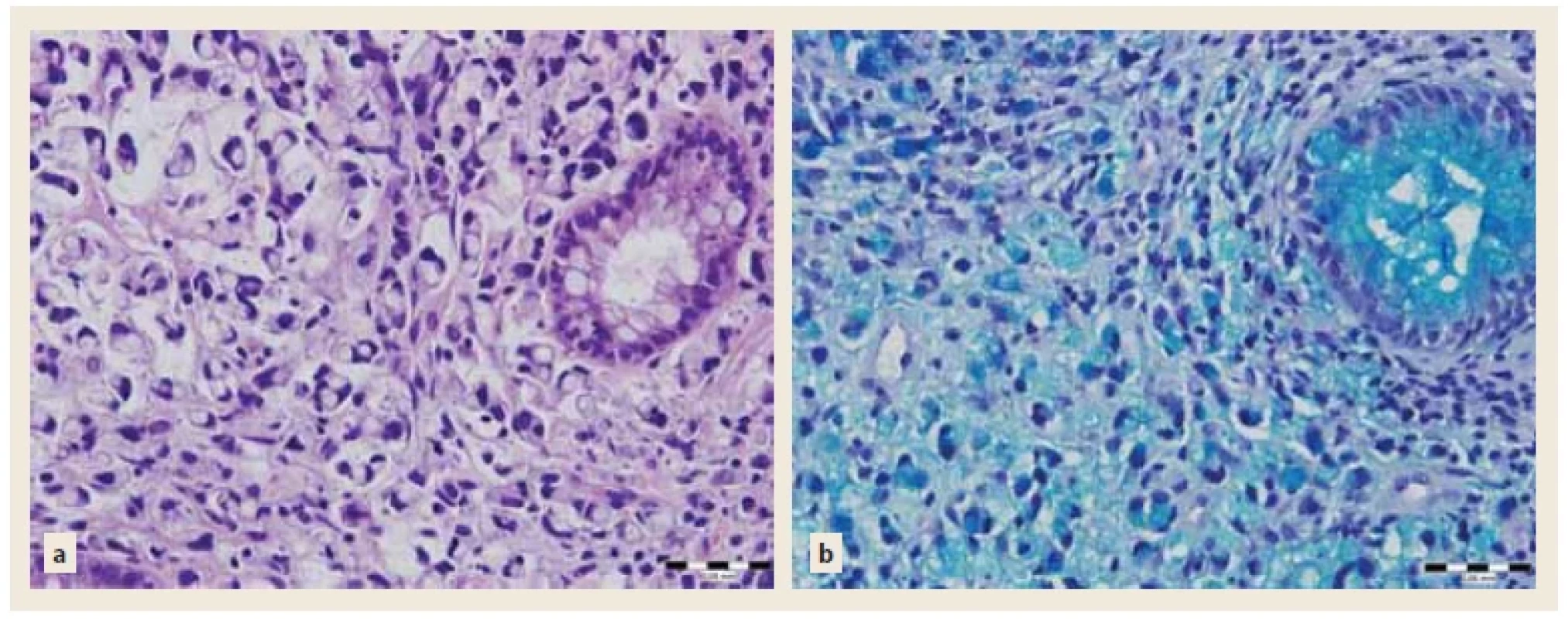
Unfortunately, her tolerance of chemotherapy was very poor, and the progression of the disease was rapid. Therefore, the chemotherapy was discontinued after three cycles. The patient‘s general condition progressed very quickly, and despite supportive treatment, the oncological therapy was terminated due to the above-mentioned facts. Hospice care was indicated due to the progression of pain and dyspnoea. The patient died within 5 months of the diagnosis.
Discussion
Crohn‘s disease is a chronic inflammatory disease of the digestive tract that mainly affects young patients. With the diagnosis of Crohn‘s disease comes an increased risk of colorectal cancer, but based on current data, the disease is associated only with a slightly increased incidence of colorectal cancer, which, moreover, has shown a clear tendency of reduced incidence in recent de - cades [1,2]. An association between IBD (inflammatory bowel disease) and the development of PSRCC has been proposed, but no surveillance guidelines have been established. Only isolated case reports around the world have been described. Tumours localised at the site of previous disease activity in the colon have not yet been described in the literature.
In our case report, we presented the negative course of the illness of a young woman suffering from Crohn‘s disease with an acute ileus state caused by sigmoid stenosis due to this type of tumour. The diagnosis was made using endoscopy, a computer tomography scan, and a histopathological examination of a colonic biopsy, which revealed the mucin-producing poorly differentiated adenocarcinoma with signet ring cell features. Because of the extensive infiltration of her liver and peritoneum at the time of the diagnosis and the symptoms of passage disorders, the patient proceeded with an end ileostomy and palliative treatment was started. Her prognosis was unfavourable, and she died within 5 months of the diagnosis in hospice care.
We only found case reports on the detection of PSRCC in IBD patients in the available literature [3–10], and from those cases, only two described PSRCC in the colon [3,4]. Feng et al mentioned a case report of a 44-year-old female with IBD that was treated with rivaroxaban. She had an obstructing process in the wall of the cecum that was biopsied as SRCC [3]. Aschneck et al presented a case of a young woman with IBD where the colonoscopy demonstrated a tight stricture 30 cm from the anal verge, which was biopsied as SRCC. The segment of the stricture was resected. Upon exploration, there was no evidence of metastatic disease in the abdominal cavity, and a left colectomy with primary anastomosis was performed. The common marks of all the case reports we introduced are the diagnoses at a young age and the poor prognosis of this malignancy. Because of the rarity of SRCC, it is difficult to estimate the incidence of this malignancy in the IBD population as no relevant data is available. Median survival of a patient with primary signet ring cell carcinoma without any association with IBD, which is mentioned in older information sources, is less than 12 months [4,11]. SRCC grows faster than non-ring cell carcinoma, and a possible delay in diagnosis is associated with an advanced tumour stage and a bad life prognosis [4,12].
In conclusion, primary signet ring cell adenocarcinoma of the colon is a rare disease with an aggressive course and poor prognosis mainly due to a common delay in diagnoses. PSRCC is more prevalent in young adults, and the association with Crohn‘s disease is uncommon and only described in a few case reports worldwide.
Statement of ethics
The patient was contacted after her hospital stay, and she was told that all her information would be anonymized. She agreed to have her medical case published, and written informed consent was obtained from the patient. All the authors listed were involved in the patient‘s care. The authors have no ethical conflicts to disclose.
Submitted/Doručeno: 17. 9. 2022
Accepted/Přijato: 26. 9. 2022
Barbora Pipek, MD
Digestive Diseases Centre
Hospital AGEL Ostrava-Vítkovice, a. s.
Zalužanského 1192/15
703 84 Ostrava-Vítkovice
Conflict of interest: The authors declare that the article/ manuscript complies with ethical standards, patient anonymity has been respected, and they state that they have no
financial, advisory or other commercial interests in relation to the subject matter.Publication ethics: This article/ manuscript has not been published or is currently being submitted for another review. The authors agree to publish their names and e-mails
in the published article/ manuscript.Dedication: The article/ manuscript is not supported by a grant nor has it been created with the support of any company. The Editorial Board declares that the manuscript met the ICMJE “uniform requirements” for bio medical papers.
Konflikt zájmů: Autoři deklarují, že text článku odpovídá etickým standardům, byla dodržena anonymita pacientů a prohlašuji, že v souvislosti s předmětem článku nemají
finanční, poradenské ani jiné komerční zájmy.Publikační etika: Příspěvek nebyl dosud publikován ani není v současnosti zaslán do jiného časopisu pro posouzení. Autoři souhlasí s uveřejněním svého jména a e-mailového kontaktu v publikovaném textu.
Dedikace: Článek není podpořen grantem ani nevznikl za podpory žádné společnosti. Redakční rada potvrzuje, že rukopis práce splnil ICMJE kritéria pro publikace zasílané do bio medicínských časopisů.
Gastroent Hepatol 2023; 77(1): 21 – 25
Zdroje
1. Castano-Milla C, Chaparro M, Gisbert JP. Systematic review with meta-analysis: the declining risk of colorectal cancer in ulcerative colitis. Aliment Pharmacol Ther 2014; 39 (7): 645–659. doi: 10.1111/apt.12651. PMID: 24612141.
2. Clarke WT, Feuerstein JD. Updates in colorectal cancer screening in inflammatory bowel diseases. Curr Opin Gastroenterol 2018; 34 (4): 208–216. doi: 10.1097/MOG.0000000000000448.
3. Feng JH, Navas CM, Olofson AM et al. Signet-Ring Cell Carcinoma Presenting as Hematochezia in a Patient with Crohn’s Disease. Case Rep Gastroenterol 2019; 13 (1): 85–88. doi: 10.1159/000493920.
4. Achnek HE, Pradhan SK, Kavic SM et al. Primary signet-ring cell carcinoma mimicking segmental Crohn’s colitis. Dig Liver Dis 2005; 27 (7): 537–542. doi: 10.1016/j.dld.2004.12.015.
5. Farraj FA, Sabbagh H, Aridi T et al. Signet Ring Cell Carcinoma of the Colon in Young Adults: A Case Report and Literature Review. Case Rep Oncol Med 2019; 2019 : 3092674. doi: 10.1155/2019/3092674.
6. Matkovcik Z, Hlad J. Kolorektalni karcinom z prstencitych bunek – kazuistika. Rozhledy v chirurgii 2015; 94 (8): 333–336.
7. Carvalho JR, Tavares J, Goulart I et al. Signet ring cell carcinoma, ileal Crohn disease or both? A case of diagnostic challenge. GE Port J Gastroenterol 2018; 25 (1): 47–51. doi: 10.1159/ 000479590.
8. Kim JS, Cheung DY, Park SH. A case of small intestinal signet ring cell carcinoma in Crohn’s disease [in Korean]. Korean J Gastroenterol 2007; 50 (1): 51–55.
9. Paparo F, Piccardo A, Clavarezza M et al. Computed tomography enterography and 18F - -FDG PET/CT features of primary signet ring cell carcinoma of the small bowel in a patient with Crohn’s disease. Clin Imaging 2013; 37 (4): 794–797. doi: 10.1016/j.clinimag.2013.02.010.
10. Hammani MB, Aboushaar R, Musmar A et al. Ileal signet ring cell carcinoma masked by Crohn disease. Ochsner J 2020; 20 (3): 323–325. doi: 10.31486/toj.19.0066.
11. Almagro UA. Primary signet-ring carcinoma of the colon. Cancer 1983; 52 (8): 1453–1457.
12. Sasaki S, Masaki T, Umetani N et al. Characteristics in primary signet-ring cell carcinoma of the colorectum, from clinicopathological observations. Jpn J Clin Oncol 1998; 28 (3): 202–206. doi: 10.1093/jjco/28.3.202.
Štítky
Detská gastroenterológia Gastroenterológia a hepatológia Chirurgia všeobecná
Článok vyšiel v časopiseGastroenterologie a hepatologie
Najčítanejšie tento týždeň
2023 Číslo 1- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Kombinace metamizol/paracetamol v léčbě pooperační bolesti u zákroků v rámci jednodenní chirurgie
- Antidepresivní efekt kombinovaného analgetika tramadolu s paracetamolem
- Parazitičtí červi v terapii Crohnovy choroby a dalších zánětlivých autoimunitních onemocnění
- Fixní kombinace paracetamol/kodein nabízí synergické analgetické účinky
-
Všetky články tohto čísla
- Editorial
- Editorial
- Fatální průběh zánětlivého onemocnění
- Dva roky pandemie covidu-19 v populaci českých pacientů s idiopatickými střevními záněty léčenými biologickou léčbou – zkušenosti terciárního IBD centra
- Primary signet ring cell adenocarcinoma as a rare cause of colonic stenosis in a young patient with Crohn’s disease – the case report
- Biologická terapie ulcerózní kolitidy v graviditě
- Komplikovaný průběh IBD v graviditě
- K otázce zaměnitelnosti monoklonálních biosimilárních protilátek v léčbě imunitně zprostředkovaných zánětlivých chorob
- Gastrointestinální obtíže a jejich vliv na kvalitu života stárnoucích osob s míšní lézí
- Epidemiological and demographic characteristics of individuals with irritable bowel syndrome based on the Rome III vs. Rome IV criteria in the Northern part of Serbia
- Autoimunní hepatitida po očkování proti covidu-19
- Výběry z mezinárodních časopisů
- Terapeutické monitorování biologických léčiv: na cestě k personalizované medicíně
- 17. vzdělávací a diskuzní gastroenterologické dny
- Profesor Ryska zemřel, jeho odkaz zůstává
- Doc. MUDr. Igor Kajaba, CSc.
- Kreditovaný autodidaktický test
- Přehled nejčastějších kožních nežádoucích účinků bio logické léčby u pacientů s idiopatickými střevními záněty – část 1
- Tofacitinib – je čas na změnu léčebného postupu u ulcerózní kolitidy?
- Gastroenterologie a hepatologie
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Autoimunní hepatitida po očkování proti covidu-19
- Primary signet ring cell adenocarcinoma as a rare cause of colonic stenosis in a young patient with Crohn’s disease – the case report
- Gastrointestinální obtíže a jejich vliv na kvalitu života stárnoucích osob s míšní lézí
- Fatální průběh zánětlivého onemocnění
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



