-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Successful Associating Liver Partition and Portal Vein Ligation after Unsuccessful Double TACE Procedure Complicated with Sepsis and Pancreatitis
Úspěšná spojená resekce jater a podvaz portální žíly po neúspěšné dvojité TACE proceduře komplikované sepsí a pankreatitidou
Spojená resekce jater a podvaz portální žíly (associated liver partition and portal vein ligation for staged hepatectomy – ALPPS) je nový postup s rostoucí řadou vědeckých a klinických studií, a jak se ukazuje, je to účinná a bezpečná metoda pro vybranou skupinu pacientů. Představujeme první případ ALPPS provedené po dvojité TACE proceduře u 64leté pacientky s rozsáhlým hepatocelulárním karcinomem pravého jaterního laloku. Postup byl úspěšný a zbytek jater vykázal značnou 90% hypertrofii, což dokazuje, že ALPPS někdy může být provedena po paliativních postupech u jaterních malignit.
Klíčová slova:
hepatocelulární karcinom – spojená resekce jater a podvaz portální žíly (ALPPS) – transhepatální arteriální chemoembolizace (TACE) – játra – resekce – hypertrofie
Autoři deklarují, že v souvislosti s předmětem studie nemají žádné komerční zájmy.
Redakční rada potvrzuje, že rukopis práce splnil ICMJE kritéria pro publikace zasílané do biomedicínských časopisů.Obdrženo:
17. 10. 2015Přijato:
10. 11. 2015
Authors: B. Romic; I. Romic; M. Mance; G. Pavlek; M. Skegro
Authors place of work: Department of Surgery, University Hospital Centre Zagreb, Croatia
Published in the journal: Klin Onkol 2016; 29(1): 59-62
Category: Kazuistika
doi: https://doi.org/10.14735/amko201659Summary
The associating liver partition and portal vein ligation (ALPPS) is a novel procedure with increasing number of scientific and clinical studies, and by now, it showed to be efficient and safe procedure in selected group of patients. Here we present the first case of ALPPS done after double TACE procedure in a 64-years-old female patient with extensive hepatocellular carcinoma of the right liver lobe. The procedure was successful and liver remnant showed significant 90% hypertrophy which proves that ALPPS sometimes can be performed after palliative procedures in liver malignancies.
Key words:
hepatocellular carcinoma – associating liver partition and portal vein ligation (ALPPS) – trans-hepatic arterial chemoembolization (TACE) – liver – resection – hypertrophyIntroduction
The associating liver partition and portal vein ligation in staged hepatectomy (ALPPS) is still a novel procedure, and scientific data are limited due to a small number of reported cases and low number of indications for this type of procedure. This surgical strategy is indicated in a selected group of patients with an inadequate future liver volume in whom other conventional methods are not feasible due to a too small future live remnant (FLR) that would lead to postoperative liver failure [1]. It is an extensive, complex and physiologically demanding surgical procedure; there are concerns about performing additional preoperative, intraoperative or postoperative procedures which may have a more or less significant impact on complication and mortality rates.
Case presentation
A 64-year-old female patient was referred to our hospital due to a large primary hepatocellular carcinoma (HCC) located in the right liver lobe and with a suspicious intrahepatic metastasis in the third Couinaud’s segment. In another institution, the tumor was pronounced inoperable and therefore palliative transhepatic arterial chemoembolization (TACE) was performed. The first TACE was performed two months after initial diagnosis, and the second was performed one month later. The patients postprocedural course was further complicated with pancreatitis and gram negative sepsis while CT scan showed a partial right liver lobe necrosis and progression of tumor size two weeks after the last TACE procedure. The patient was transferred to our institution where pancreatitis and sepsis were treated; following stabilization, we performed ALPPS with the transection line between the left anterior and left posterior liver sections. Also, the liver lesion in segment 3 was removed and sent to pathohistologic analysis. The interval between the two stages was 13 days. Prior to the 2nd stage, CT volumetry showed a 90% increase in volume in segments 2, in the remnant part of segment 3, atrophic right lobe with progression in size of areas of necrosis. There was no significant elevation of liver enzymes between the two periods and there was no indication of liver failure.
The 2nd stage was performed, and the atrophic and necrotic right liver lobe was removed. Intraoperatively, there was no sign of tumor remnants seen in the liver. Pathological examination of the resected specimen and lesions in segment 3 confirmed the diagnosis of hepatocellular carcinoma. Our patient’s postoperative course was uneventful. At 12 months of follow‑up the patient is alive with no signs of recurrence.
Fig. 1. CT image prior to first TACE procedure (A) and after second TACE procedure showing partial right lobe necrosis (B). 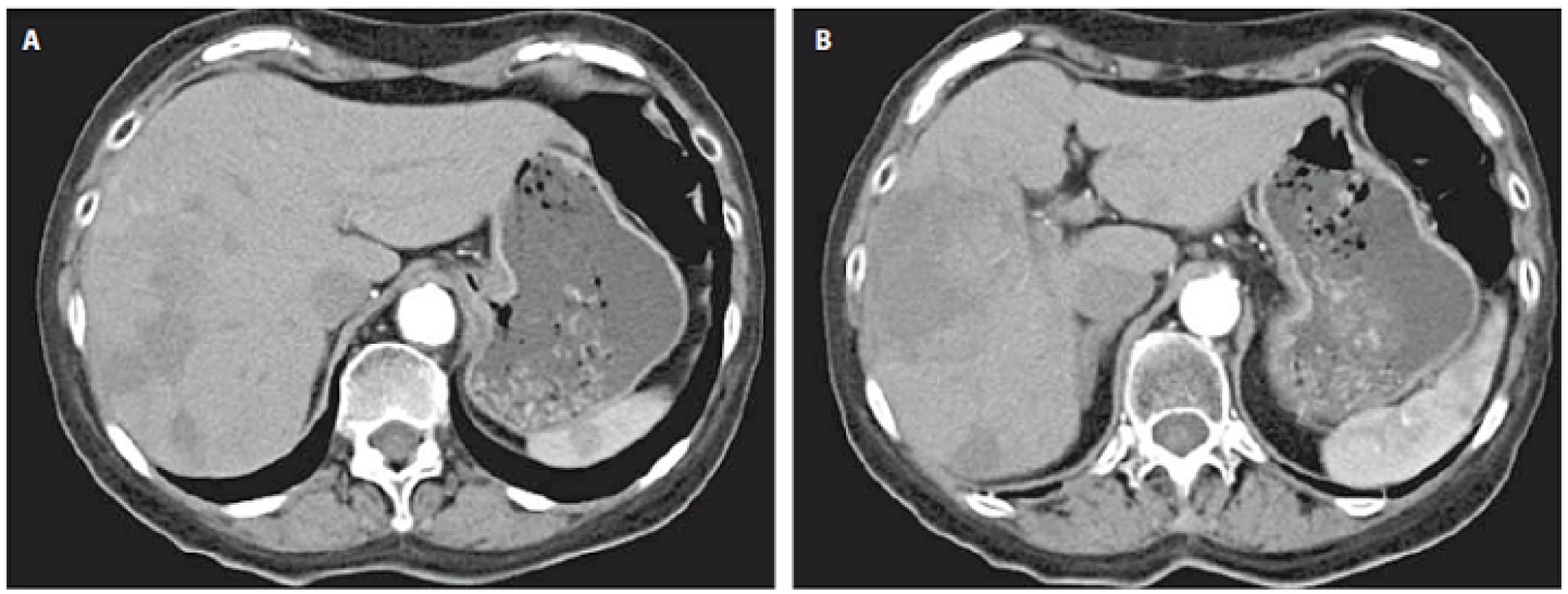
Fig. 2. CT image showing the liver four days after ALPPS where further right lobe atrophy and necrosis is seen with no significant contralateral hypertrophy (A) after 14 days where signifi cant left lobe hypertrophy is noticed (B). 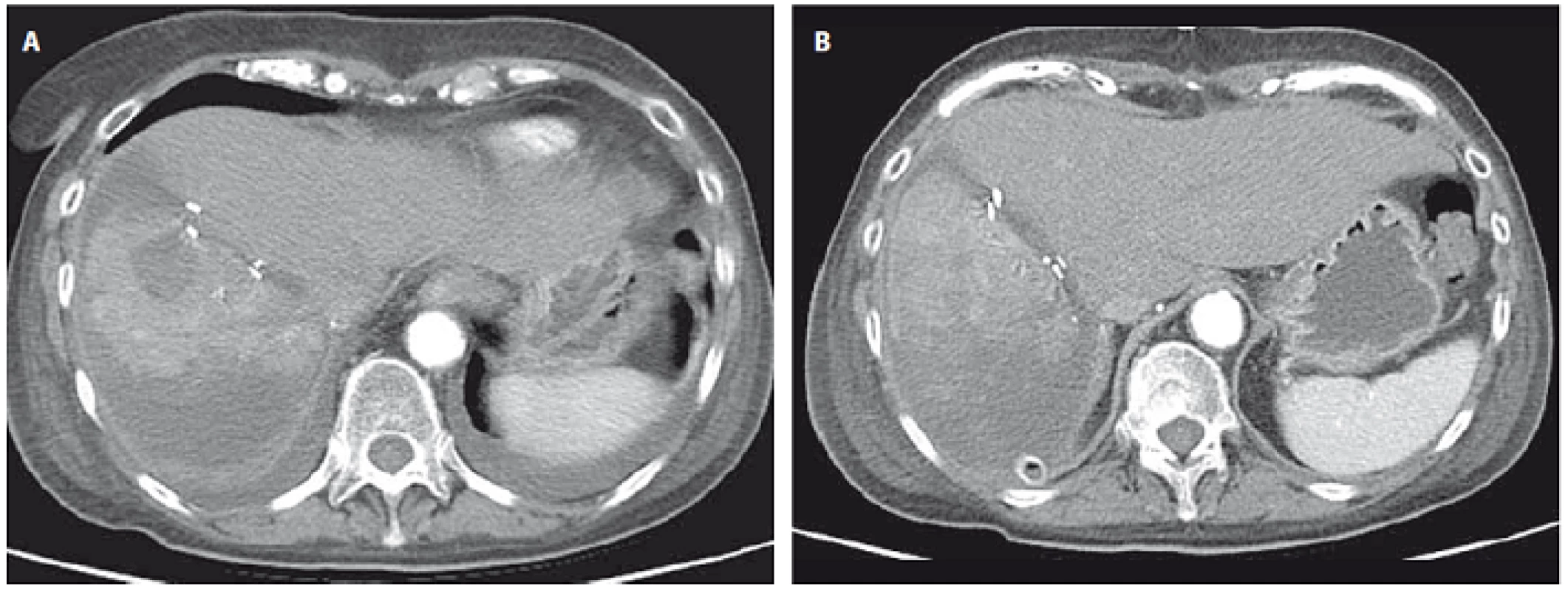
Fig. 3. Intraoperative photograph of the hypertrophied left liver lobe (A) and specimen of necrotic right liver lobe after removal (B). 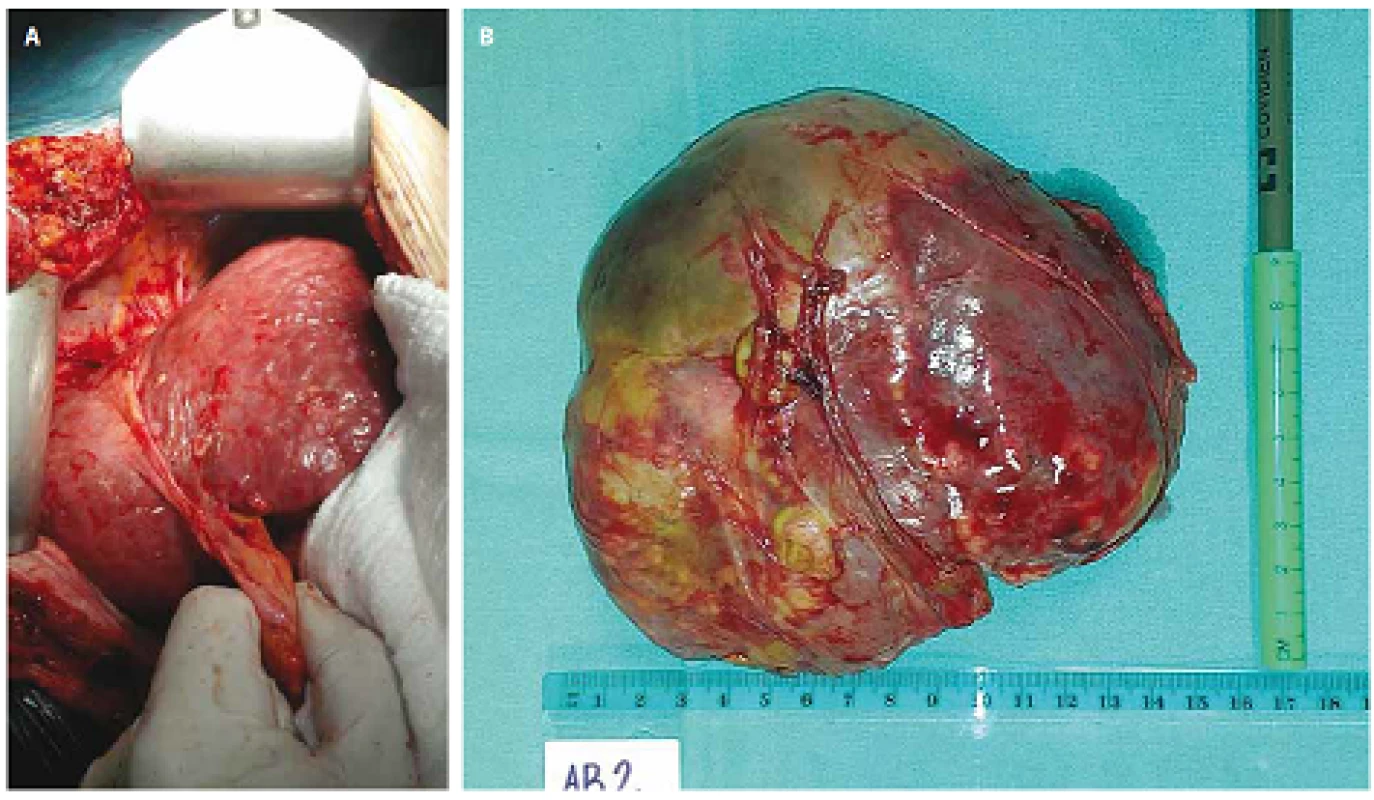
Discussion
In scientific literature, we did not find any reports regarding the ALPPS procedure performed after TACE. In all similar reported cases, ALPPS was performed either as a primary procedure or after unsuccessful portal vein embolization/ ligation. Palliative procedures, such as TACE, RFA or ethanol injection, were not performed prior to ALPPS since the intention of ALPPS is curative resection and surgeons do not want to risk possible complications caused by these procedures. Also the impact of palliative procedures on liver hypertrophy rate between two stages of ALPPS is not known [2,3].
ALPPS was developed mostly through clinical investigations, and we expect more experimental basic studies regarding the mechanisms of liver hypertrophy.
TACE causes atrophy and necrosis of the tumor but also, damages the surrounding liver tissue. It is performed in cases of unresectable malignant disease as part of palliative treatment. Criteria for unresectability in malignant tumors are: tumor infiltration of major vessels, extrahepatic disease and inadequate FLR. Inadequate liver remnant criteria changed after development of ALPPS procedure since it is possible to achieve curative liver resection in patients who were considered inoperable, in those with less than 25% of FLR in normal liver and 35% in cirrhotic liver [4]. The exact physiologic mechanisms that promote faster and more intensive liver hypertrophy are still not known, but changes in portal blood flow and molecular signals from deportalized liver lobes are now identified as possible factors [5]. In ourcase, we were concerned that liver atrophy and necrosis after TACE could lead to failure of the ALPPS procedure due to a lack of these molecular signals, but results showed a more than average liver hypertrophy and a quick recovery of patient [6].
Conclusion
Considering our case, we can highlight the importance of raised portal flow in the healthy liver compared to humoral signals of a deportalized liver. This indicates that additional palliative or regional procedures can be performed prior to ALPPS, and preoperative planning may include these procedures as well. The comparison between ALPPS alone and ALPPS after palliation will show us indications for surgical strategies in different types and stages of disease. In the future, more studies will show if additional procedures can be safely performed in ALPPS and possible positive or negative effects on ALPPS success.
The authors declare they have no potential conflicts of interest concerning drugs, products, or services used in the study.
The Editorial Board declares that the manuscript met the ICMJE recommendation for biomedical papers.
Ivan Romic, M.D.
Department of Surgery
University Hospital Centre Zagreb
Kispaticeva 12
10 000 Zagreb
Croatia
e-mail: i.romic@gmail.com
Submitted: 17. 10. 2015
Accepted: 10. 11. 2015
Zdroje
1. Schnitzbauer AA, Lang SA, Goessmann H et al. Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling 2-staged extended right hepatic resection in small‑for ‑ size settings. Ann Surg 2012; 255(3): 405 – 414. doi: 10.1097/ SLA.0b013e31824856f5.
2. Hasselgren K, Sandström P, Björnsson B. Role of associating liver partition and portal vein ligation for staged hepatectomy in colorectal liver metastases: a review. World J Gastroenterol 2015; 21(15): 4491 – 4498. doi: 10.3748/ wjg.v21.i15.4491.
3. Ome Y, Kawamoto K, Park TB et al. Two‑stage hepatectomy and associated liver partition and portal vein ligation for staged hepatectomy (ALPPS) in treating liver metastases of rectal cancer: a case report. Springerplus 2015; 4 : 194. doi: 10.1186/ s40064-015-0965-z.
4. El ‑ Serag HB, Marrero JA, Rudolph L et al. Diagnosis and treatment of hepatocellular carcinoma. Gastroenterology 2008; 134(6): 1752–1763. doi: 10.1053/ j.gastro.2008.02.090.
5. Miraglia R, Pietrosi G, Maruzzelli L et al. Efficacy of transcatheter embolization/ chemoembolization (TAE/ TACE) for the treatment of single hepatocellular carcinoma. World J Gastroenterol 2007; 13(21): 2952 – 2955.
6. Rammohan A, Sathyanesan J, Ramaswami S et al. Embolization of liver tumors: past, present and future. World J Radiol 2012; 4(9): 405 – 412. doi: 10.4329/ wjr.v4.i9.405.
Štítky
Detská onkológia Chirurgia všeobecná Onkológia
Článok vyšiel v časopiseKlinická onkologie
Najčítanejšie tento týždeň
2016 Číslo 1- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Nejasný stín na plicích – kazuistika
- Kombinace metamizol/paracetamol v léčbě pooperační bolesti u zákroků v rámci jednodenní chirurgie
- Antidepresivní efekt kombinovaného analgetika tramadolu s paracetamolem
- Fixní kombinace paracetamol/kodein nabízí synergické analgetické účinky
-
Všetky články tohto čísla
- Genomic Tests as Predictors of Breast Cancer Patients’ Prognosis
- Potential of Long Non- coding RNA Molecules in Diagnosis of Tumors
- The Role of Heat Shock Proteins in Leukemia
- Survival Analysis Three-year Follow-up of Pacients with Head and Neck Cancer
- Editorial
- Predicting Vitality Change in Older Breast Cancer Survivors after Primary Treatment – an Approach Based on Using Time-related Difference of Pro-inflammatory Marker C-reactive Protein
- Successful Associating Liver Partition and Portal Vein Ligation after Unsuccessful Double TACE Procedure Complicated with Sepsis and Pancreatitis
- SOUTĚŽ NA PODPORU AUTORSKÝCH TÝMŮ PUBLIKUJÍCÍCH V ZAHRANIČNÍCH ODBORNÝCH TITULECH
- Successful Therapy of Czech Patients with ROS1 Translocation by Crizotinib
-
Průvodce mladého onkologa infuzní terapií a výživou
Díl 1 – Hypokalemie. Bílkoviny. Kazuistika 1 -
Zpráva z European Cancer Congress 2015
Cílená biologická kombinační léčba prodloužila celkové přežití u metastatického melanomu - Informace z České onkologické společnosti
- Aktuality z odborného tisku
- Docentce MUDr. Janě Prausové, Ph.D., v přátelství a s obdivem
-
Vyhlášení výsledků
SOUTĚŽE NA PODPORU AUTORSKÝCH TÝMŮ PUBLIKUJÍCÍCH V ZAHRANIČNÍCH ODBORNÝCH TITULECH - Angiosarkom prsu po radioterapii před 11 lety
- SOUTĚŽ O NEJLEPŠÍ PRÁCI
- Klinická onkologie
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Survival Analysis Three-year Follow-up of Pacients with Head and Neck Cancer
-
Průvodce mladého onkologa infuzní terapií a výživou
Díl 1 – Hypokalemie. Bílkoviny. Kazuistika 1 - Genomic Tests as Predictors of Breast Cancer Patients’ Prognosis
- The Role of Heat Shock Proteins in Leukemia
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



