-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Syndromic Surveillance: Adapting Innovations to Developing Settings
article has not abstract
Published in the journal: Syndromic Surveillance: Adapting Innovations to Developing Settings. PLoS Med 5(3): e72. doi:10.1371/journal.pmed.0050072
Category: Policy Forum
doi: https://doi.org/10.1371/journal.pmed.0050072Summary
article has not abstract
Surveillance, according to the World Health Organization (WHO), “is the cornerstone of public health security” [1]. In many developing countries, human, laboratory, and infrastructure limitations impede effective surveillance [2–5]. Such countries likely do not meet core surveillance and response capacities under the new International Health Regulations (IHR 2005) [6], which require detection of elevated disease and death rates, immediate implementation of control measures, and reporting to WHO of any event that may constitute a public health emergency of international concern [7]. (The previous IHR covered only cholera, plague, and yellow fever.)
In some high-income countries, “syndromic surveillance,” a novel approach, uses pre-diagnostic data and statistical algorithms to detect epidemics earlier than traditional surveillance, including unusual diseases with nonspecific presentations [8–10] (Box 1). Syndromic surveillance also supports public health “situational awareness” [11,12], which means monitoring the effectiveness of epidemic responses and characterizing affected populations. Despite obstacles to implementation in resource-limited settings, the tools and strategies of syndromic surveillance hold promise for improving public health security in developing countries. Successful applications show that the obstacles can be overcome.
Box 1. Overview of Syndromic Surveillance Systems
Purpose
Detect outbreaks earlier than possible with traditional surveillance
Situational awareness (e.g., monitoring outbreak distribution and spread, characterizing affected populations)
Features
“Indicator” (pre-diagnostic) data (e.g., syndromes, medication sales, absenteeism, patient chief complaints)
Automated or partially automated data acquisition and analysis
Statistical algorithms to detect unexpected elevations in indicator data
Near-real-time data acquisition and analysis
Computerized tools for visualizing data and analysis results
Synonymous terms (modified from [10])
Outbreak detection systems
Early warning systems
Health indicator surveillance
Prodromal surveillance
Potential Utility in Developing Countries
Syndromic surveillance offers a useful adjunct to diagnosis-based surveillance of emerging infections in developing countries. Where laboratory confirmation is not routinely used, syndromes associated with diseases of public health importance, such as influenza-like illness caused by multiple epidemic-prone tropical infections, could indicate outbreaks requiring laboratory-based investigation and control. Also, syndromic surveillance can identify outbreaks that do not fall into pre-established diagnostic categories, a capability essential for prompt control of new or changing diseases.
Another potential contribution of the syndromic surveillance field to developing countries is objective, automated approaches for detecting unusual morbidity trends, which could strengthen monitoring of syndromes, diagnoses, and other health-related data. Usually, these approaches involve entry of patient data into a computer, followed by (1) automatic, periodic application of statistical algorithms comparing the data to non-outbreak expectations (trends that depart from expectations by a predefined statistical threshold indicate possible outbreaks), and (2) visualization tools.
Objective criteria for identifying possible outbreaks complement subjective assessment, often the sole guide in developing settings, in two important ways. First, they can prevent unwitting bias, as in failing to account for readily explainable data behavior. For example, statistical algorithms can draw on historical data to remove effects of weekly clinic utilization cycles or seasonal disease cycles, uncovering unusual events that could reflect new or changing pathogens.
Second, objective procedures provide uniformity across health care facilities and personnel working separate departments or shifts within facilities. Without standardized approaches for identifying unusual health events, facility-level factors, such as the training, experience, and competing clinical responsibilities of personnel, influence the decision to notify higher authorities of potential outbreaks. Local notification protocols may vary markedly within decentralized Ministries of Health, which are common across developing countries.
Computer-based automation of routine data analysis is helpful because, with multiple reporting units and reportable events, the number of graphs or charts to inspect at public health offices likely exceeds the capacity of public health personnel (especially considering the competing responsibilities in short-staffed offices). The problem can be greatest during outbreaks—when thorough, rapid data assessment is critical for gauging outbreak extent and trajectory—as control activities take precedence.
Syndromic surveillance systems typically use computerized visualization tools to display algorithm results and morbidity trends [13–16]. Many software packages generate time-series graphs, maps, and data tables that are required routinely, and allow the user to produce other displays (e.g., focusing on specific age groups, surveillance sites, or syndromes) as needed. Tables and graphs summarizing key data and algorithm outputs, arranged to fit into a single computer screen view, can efficiently focus the user's attention on potential outbreaks.
Reason for Optimism
There is cause for optimism that syndromic surveillance approaches can feasibly be adapted to developing settings. First, they fit naturally with and could enhance existing strategies for outbreak detection and situational awareness in tropical areas. For example, with the goal of containing epidemics within two weeks of onset, WHO and African countries are implementing Malaria Early Warning Systems that use health data and climatology to forecast and detect epidemics [17]. Pre-diagnostic data have been evaluated as indicators for dengue outbreaks in French Polynesia [18], French Guiana [19], Puerto Rico [20], and elsewhere.
Second, while existing electronic health data are unavailable in some developing areas, many Ministries of Health already require reporting of data that have proven useful for syndromic surveillance in high-income countries, such as International Classification of Diseases codes. Adapting strategies for grouping International Classification of Diseases codes into syndromes representing priority diseases, as done in syndromic surveillance systems in the United States [21], could facilitate syndromic surveillance in resource-limited settings without requiring collection of new data.
Third, expanding access to communication networks and technology will facilitate rapid electronic data entry, reporting, and analysis in resource-limited areas. Between 2000 and 2005, Internet access improved more than 4-fold in developing countries, and more than one quarter of the developing world uses mobile phones (Figure 1) [22], making these especially promising tools for timely transmission of surveillance data. As costs decrease and network availability improves, laptop computers, personal digital assistants, and other technologies may increasingly find application in developing country surveillance systems (Table 1). Fourth, syndromic surveillance initiatives could dovetail with other efforts to improve health information systems. For example, the WHO-led Health Metrics Network, launched in 2005, aims to increase the availability and use of timely and accurate health information by catalyzing the joint funding and development of core country health information systems [23]. Though concerned with a range of health information systems (including vital registration, health surveys, disease surveillance, and others), its efforts to develop standards, as well as data management and analytic capacities, could lay essential groundwork for application of syndromic surveillance methods.
Fig. 1. Internet and Telephone Access in Developing Countries 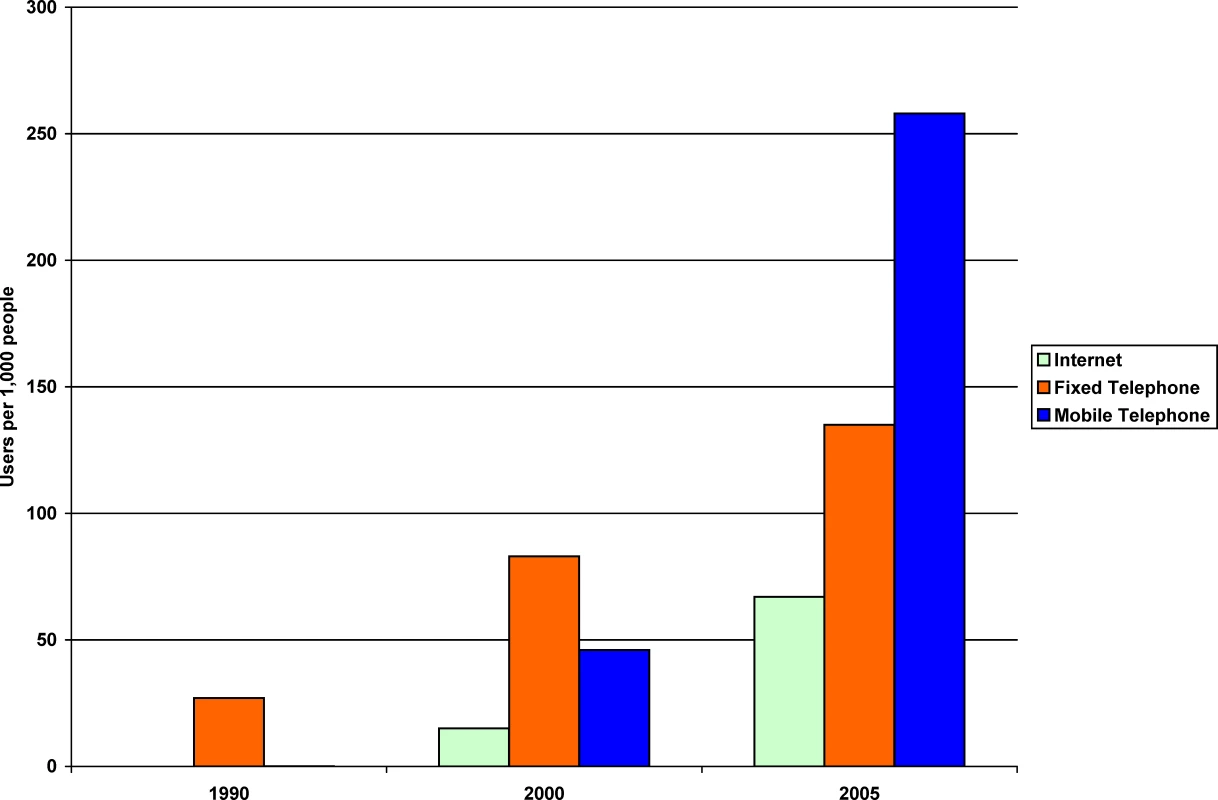
Adapted from [22]. Tab. 1. Technology for Health Data Capture and Transmission in Remote Areas 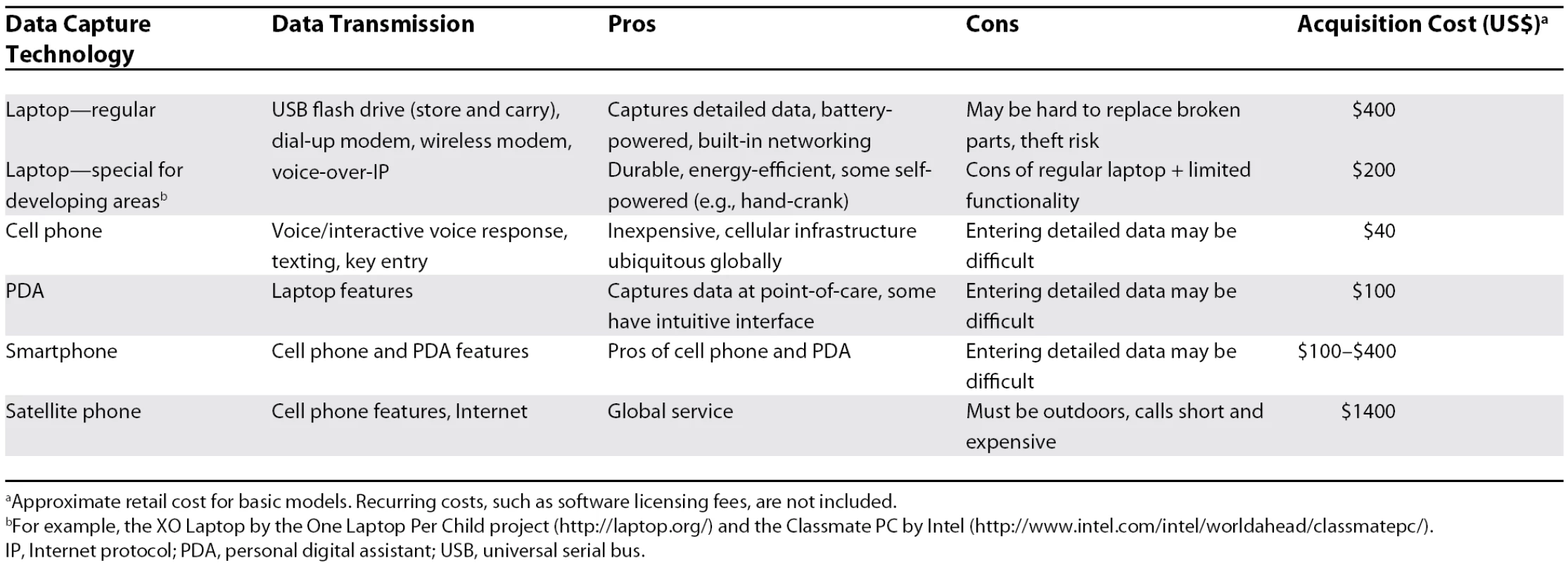
aApproximate retail cost for basic models. Recurring costs, such as software licensing fees, are not included. Results from Existing Systems in Developing Countries
Some developing countries have overcome resource constraints to establish effective electronic syndromic surveillance systems. The Indonesian Ministry of Health, together with a US laboratory it hosts in Jakarta, Naval Medical Research Unit-2, developed a simple but flexible syndromic surveillance system, Early Warning Outbreak Recognition System (EWORS), in 1998. For patients presenting to selected provincial hospitals, data on 29 signs and symptoms are collected and analyzed daily. Health authorities have used EWORS to detect outbreaks of dengue, diarrhea, influenza-like illness, and many other diseases.
For example, in 2002, EWORS facilitated detection and control of a diarrhea outbreak following a severe flood in Jakarta (Figure 2). A sentinel site in North Jakarta municipality reported above-average counts of watery diarrhea with other symptoms indicating moderate-to-severe disease in January, when heavy rains caused flooding with contamination of water sources. The first alert of a significant increase in cases, generated by an automated statistical detection algorithm, occurred during the second week of January. An outbreak investigation was initiated, including rectal swab sampling of patients with watery diarrhea. Culture tests identified Vibrio cholerae in 44 of 47 specimens collected, as well as Salmonella and Shigella. Health authorities implemented interventions immediately, including provision of clean water to flood-affected populations and rehydration for diarrhea patients; case counts returned to baseline levels by late February.
Fig. 2. Post-Flooding Diarrhea Outbreak in Jakarta, Indonesia, January–February 2002 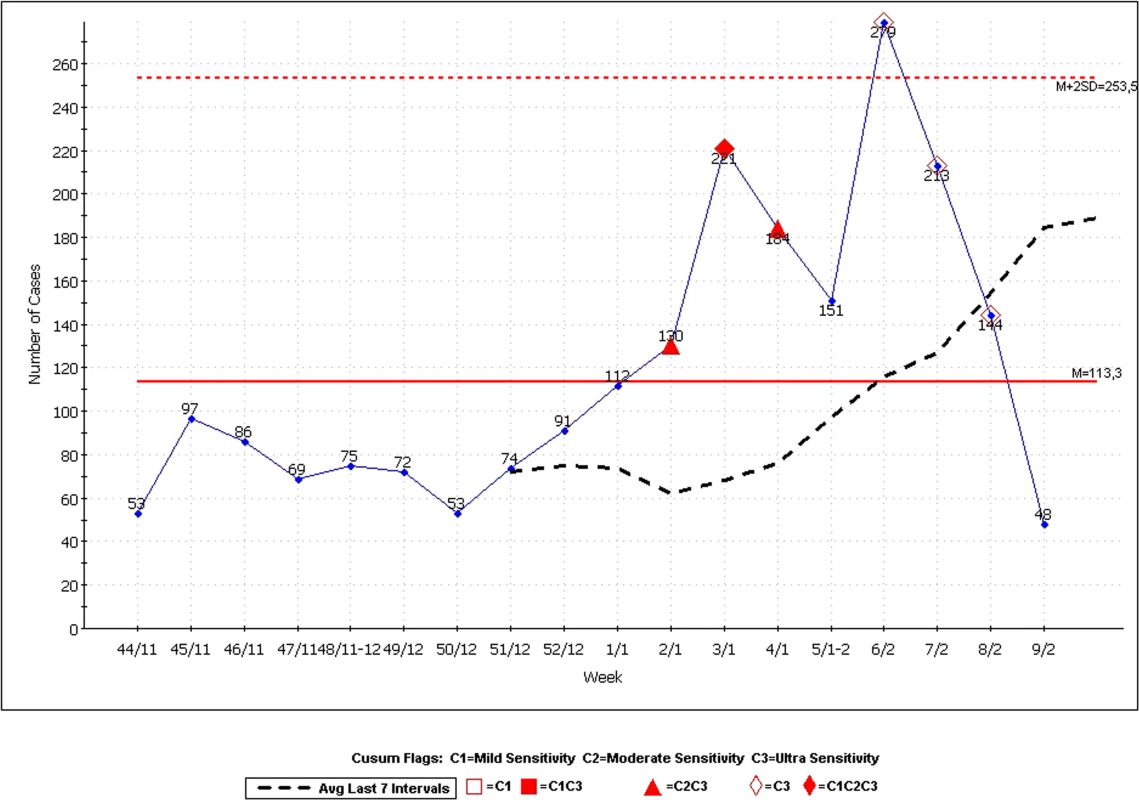
X-axis labels are week/month, from the 44th week of 2001 (in November) to the 9th week of 2002 (in February). The blue line shows the number of cases per week reporting to an EWORS site in Jakarta with watery diarrhea and dehydration, fever, or vomiting. The “Cusum” (cumulative sum) C1, C2, and C3 alerts identify, with increasing sensitivity, significant increases in case counts using the Early Aberration Reporting System [27]. The horizontal red solid and broken lines represent the long-term mean and mean plus two standard deviations (sometimes used as an outbreak detection threshold in other surveillance systems), respectively. In 2007, the Ministry of Health, through three of its subordinate organizations (National Institute of Health Research and Development, Directorate General of Disease Control and Environmental Health, and Directorate General of Medical Service), officially adopted EWORS as a national surveillance system. The Ministry of Health plans to expand EWORS to many more hospitals throughout Indonesia, and to include its implementation as a criterion for hospital accreditation. To enhance EWORS syndromic surveillance with laboratory validation, eight laboratories in Indonesia have been designated as regional reference centers that support outbreak investigations.
In Peru, the Directorate of Epidemiology (part of the Ministry of Health), supported by a US laboratory in Lima, the Naval Medical Research Center Detachment, implemented a system modeled on EWORS in 2005 at two public health centers on the country's northern border. Following a favorable evaluation in 2006, the system was expanded to several sites in Lima, where detection of dengue outbreaks is of high concern (autochthonous dengue fever transmission was reported in Lima in 2005 for the first time in more than 60 years, but has not been detected since).
The US laboratory in Lima also partnered with the Peruvian Navy and Voxiva to develop the Alerta surveillance system in 2002 to monitor reportable events in sailors and their families. Alerta allows real-time data transmission by mobile phone, text messaging, or Internet from units across the country, including remote Amazon bases and ships. Alerta has identified many outbreaks and facilitated rapid laboratory confirmation by response teams equipped with field-use diagnostic tests or by central laboratories.
For example, in 2005, Alerta identified two diarrhea outbreaks at a Peruvian Navy training base in Lima [24]. Prompt investigations identified Cyclospora cayetanensis as the cause of both outbreaks, leading to appropriate treatment (cotrimoxazole or empiric fluorquinolone), investigation of food and water sources and meal preparation, and an epidemiological study to test a hypothesis about the incidence of C. cayetanensis infection in the local population. There have been no further large outbreaks of diarrhea at this training base.
Implementation
Syndromic surveillance tools and approaches are not appropriate for all developing settings. Where no health data are routinely collected, developing basic surveillance capacities [25], including laboratory-based surveillance, should be a high priority for local and national health authorities. Where electronic syndromic surveillance systems may be feasible, a combination of technical, financial, political, ethical, cultural, and societal factors all may contribute to successful implementation and should be considered from the outset of planning (Box 2).
Box 2. Key Considerations in Planning Electronic Syndromic Surveillance Systems in Low-Resource Settings
Technical considerations
Harvesting data already required for existing systems may be more acceptable than adding new data collection requirements.
Even without Internet, automated decision support may facilitate timely transmission of key data through selective use of cell phones, radio, or Internet cafes.
Initial and refresher epidemiological and electronic system training is essential.
South–South, South–North, and multilateral technical partnerships can facilitate sharing of best practices and adoption of useful technologies.
Financial considerations
Relatively low-cost hardware, including laptop computers designed for developing settings and personal digital assistants, can be used.
Commercial software may involve license fees and recurring costs; open-source and custom software should be explored with technical partners.
Surveillance programs may partner with other programs to seek funding for shared technology needs from development banks or other potential sponsors.
Political considerations
New surveillance programs requiring significant initial investment may face strong competition for limited health resources from revenue-generating clinical programs.
Local political support is especially critical in decentralized Ministries of Health, where funding and administration are shared with local levels.
Engagement with key political stakeholders is needed to ensure that new systems do not conflict with existing priorities and that lines of authority are respected.
Systems must not be seen as driven by foreign sponsor or collaborator priorities.
Ethical, societal, and cultural considerations
Developing and explaining privacy safeguards may address patient concerns over electronic data capture and transmission.
Community education on the clinical and public health uses of surveillance data may improve patient acceptability.
Community education on local disease risks and presentations, and the importance of seeking care early, may enhance outbreak detection and patient care.
Patient preference for private health care and pharmaceutical providers over public facilities can limit the effectiveness of Ministry of Health systems.
(Framework adapted from a model for assessing the potential success of particular health-related biotechnologies in resource-poor regions, in [26].)
The role of technical partnerships focusing on software, hardware, and analytical methods is especially important. While the need for improved outbreak detection and situational awareness is greatest in developing settings, most syndromic surveillance applications have been used in high-income countries. Technical partnerships involving research laboratories, public health agencies, and other organizations could bridge this gap, and should aim to foster lasting capacity for system development, operation, and improvement.
An example of such a collaboration includes epidemiologists and information technology specialists from Indonesia, Peru, and the Johns Hopkins University Applied Physics Laboratory, who partnered to learn from experience with EWORS and Alerta and consult on further system improvement. In September 2007, they joined colleagues from other developing countries with experience or interest in syndromic surveillance to develop an informal professional network, and identify common surveillance needs and possible solutions (https://secwww.jhuapl.edu/dsw/index.htm). The International Society for Disease Surveillance (http://www.syndromic.org/), which has a strong syndromic surveillance focus, provides another forum for international syndromic surveillance partnerships.
Planning a new syndromic surveillance system requires special attention to some of the issues usually considered in surveillance system planning (Table 2). For example, procedures for developing, maintaining, and evaluating proficiency with new technologies, and for replacing or repairing failing hardware, must be established. As with any new surveillance effort, the system should, to the extent possible, be integrated into existing reporting pathways.
Tab. 2. Strategic and Operational Surveillance Planning: Key Activities for Syndromic Surveillance Systems 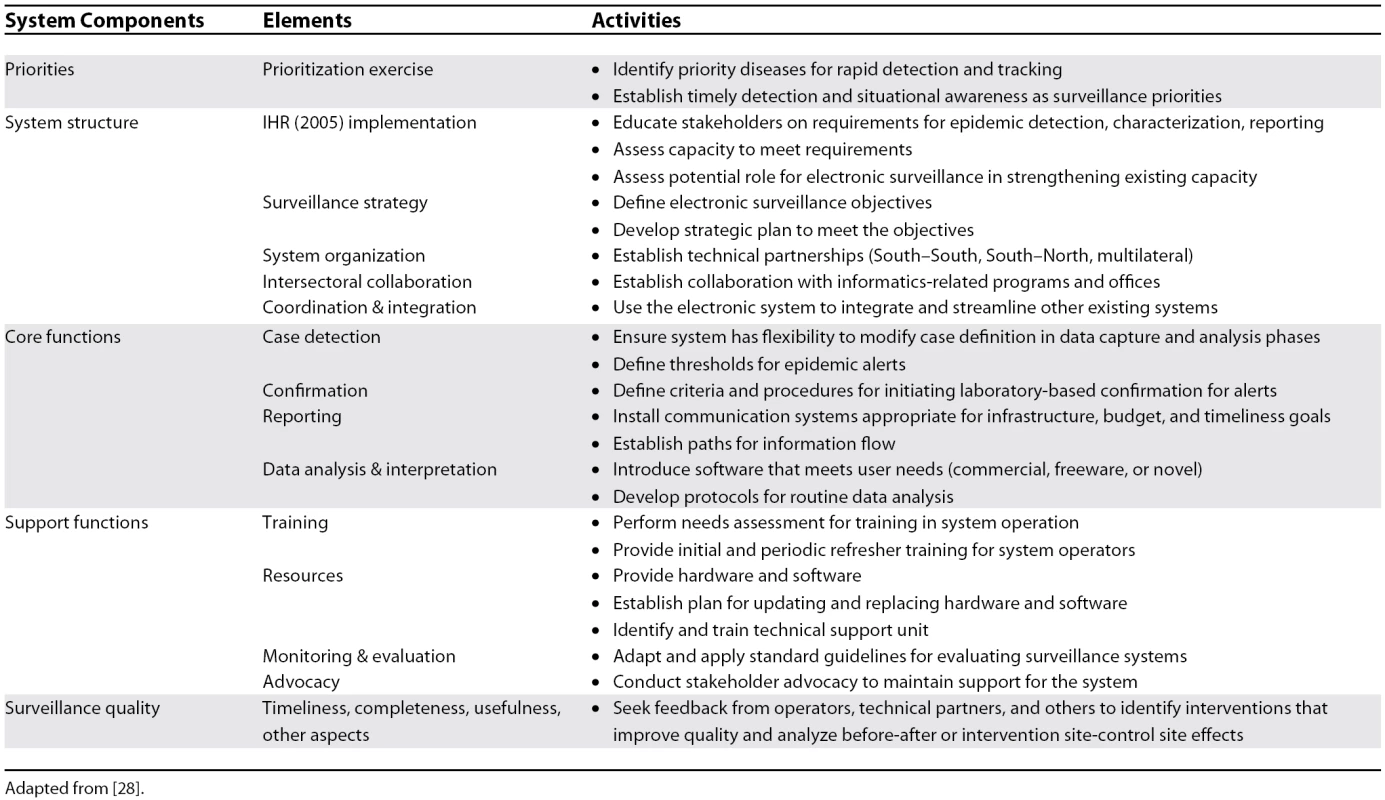
Adapted from [28]. Wider Benefits
By helping to rapidly detect and characterize unusual morbidity trends, syndromic surveillance holds promise as an early line of defense against new and emerging infections in developing settings. Considering the poor state of public health surveillance in those areas, syndromic surveillance tools and approaches may provide greater additional benefit than in high-income countries that already have other types of effective surveillance programs.
But implementation of syndromic surveillance tools and approaches may have wider public health benefits. Hardware, software, and communication infrastructure for timely outbreak detection and situational awareness could strengthen data collection, reporting, and interpretation for other public health programs (e.g., evaluating interventions and identifying resource needs). Perhaps most importantly, investing in human resources—through training in epidemiology, data management and analysis, use of computers, and other public health skills—would help address an important threat to public health security in developing countries.
Zdroje
1. World Health Organization
2007
The world health report 2007—A safer future: Global public health security in the 21st century.
Available: http://www.who.int/whr/2007/whr07_en.pdf. Accessed 13 February 2008
2. ChenLEvansTAnandSBouffordJIBrownH
2004
Human resources for health: Overcoming the crisis.
Lancet
364
1984
1990
3. United States General Accounting Office
2001
Global health. Challenges in improving infectious disease surveillance systems.
Available: http://www.gao.gov/new.items/d01722.pdf. Accessed 13 February 2008
4. NdiayeSMQuickLSandaONiandouS
2003
The value of community participation in disease surveillance: A case study from Niger.
Health Promot Int
18
89
98
5. PettiCAPolageCRQuinnTCRonaldARSandeMA
2006
Laboratory medicine in Africa: A barrier to effective health care.
Clin Infect Dis
42
377
382
6. The PLoS Medicine Editors
2007
How is WHO responding to global public health threats.
PLoS Med
4
e197
doi:10.1371/journal.pmed.0040197
7. Fifty-Eighth World Health Assembly
2005
Revision of the International Health Regulations.
Available: http://www.who.int/csr/ihr/IHRWHA58_3-en.pdf. Accessed 13 February 2008
8. BravataDMMcDonaldKMSmithWMRydzakCSzetoH
2004
Systematic review: surveillance systems for early detection of bioterrorism-related diseases.
Ann Intern Med
140
910
922
9. BuehlerJWHopkinsRSOverhageJMSosinDMTongV
2004
Framework for evaluating public health surveillance systems for early detection of outbreaks: Recommendations from the CDC Working Group.
MMWR Recomm Rep
53
1
11
10. HenningKJ
2004
Overview of syndromic surveillance. What is syndromic surveillance.
MMWR Morb Mortal Wkly Rep
53
Suppl
5
11
11. BradleyCARolkaHWalkerDLoonskJ
2005
BioSense: Implementation of a national early event detection and situational awareness system.
MMWR Morb Mortal Wkly Rep
54
Suppl
11
19
12. RolkaHBurkomHCooperGFKulldorffMMadiganD
2007
Issues in applied statistics for public health bioterrorism surveillance using multiple data streams: Research needs.
Stat Med
26
1834
1856
13. TsuiFCEspinoJUDatoVMGestelandPHHutmanJ
2003
Technical description of RODS: A real-time public health surveillance system.
J Am Med Inform Assoc
10
399
408
14. MandlKDOverhageJMWagnerMMLoberWBSebastianiP
2004
Implementing syndromic surveillance: A practical guide informed by the early experience.
J Am Med Inform Assoc
11
141
150
15. HeffernanRMostashariFDasDKarpatiAKulldorfM
2004
Syndromic surveillance in public health practice, New York City.
Emerg Infect Dis
10
858
864
16. ReisBYKirbyCHaddenLEOlsonKMcMurryAJ
2007
AEGIS: A robust and scalable real-time public health surveillance system.
J Am Med Inform Assoc
14
581
588
17. World Health Organization
2001
A framework for field research in Africa: Malaria Early Warning Systems: Concepts, indicators, and partners.
Available: http://www.who.int/malaria/cmc_upload/0/000/014/807/mews2.pdf. Accessed 13 February 2008
18. ChungueEBoutinJPRouxJ
1991
Dengue surveillance in French Polynesia: An attempt to use the excess number of laboratory requests for confirmation of dengue diagnosis as an indicator of dengue activity.
Eur J Epidemiol
7
616
620
19. CarmeBSobeskyMBiardMHCotellonPAznarC
2003
Non-specific alert system for dengue epidemic outbreaks in areas of endemic malaria. A hospital-based evaluation in Cayenne (French Guiana).
Epidemiol Infect
130
93
100
20. Rigau-PerezJGMillardPSWalkerDRDesedaCCCasta-VelezA
1999
A deviation bar chart for detecting dengue outbreaks in Puerto Rico.
Am J Public Health
89
374
378
21. Marsden-HaugNFosterVBGouldPLElbertEWangH
2007
Code-based syndromic surveillance for influenzalike illness by International Classification of Diseases, Ninth Revision.
Emerg Infect Dis
13
207
216
22. The World Bank
2006
Information & communications for development (IC4D): Global trends and policies.
Available: http://www.worldbank.org/ic4d. Accessed 13 February 2008
23. World Health Organization
2008
Health Metrics Network. What is HMN.
Available: http://www.who.int/healthmetrics/about/whatishmn/en/index.html. Accessed 13 February 2008
24. Torres-SlimmingPAMundacaCCMoranMQuispeJColinaO
2006
Outbreak of cyclosporiasis at a naval base in Lima, Peru.
Am J Trop Med Hyg
75
546
548
25. World Health Organization
2006
Information resources: National surveillance systems and integrated disease surveillance.
Available: http://www.who.int/csr/labepidemiology/surveillancesystems/en/index.html. Accessed 13 February 2008
26. SingerPABerndtsonKTracyCSCohenERMasumH
2007
A tough transition.
Nature
449
160
163
27. HutwagnerLCThompsonWSeemanGMTreadwellT
2003
The bioterrorism preparedness and response Early Aberration Reporting System (EARS).
J Urban Health
80
2 Suppl 1
i89
i96
28. World Health Organization
2006
Communicable disease surveillance and response systems. A guide to planning.
Available: http://www.who.int/csr/resources/publications/surveillance/WHO_CDS_EPR_LYO_2006_1.pdf. Accessed 13 February 2008
Štítky
Interné lekárstvo
Článok vyšiel v časopisePLOS Medicine
Najčítanejšie tento týždeň
2008 Číslo 3- Parazitičtí červi v terapii Crohnovy choroby a dalších zánětlivých autoimunitních onemocnění
- Intermitentní hladovění v prevenci a léčbě chorob
- Statinová intolerance
- Co dělat při intoleranci statinů?
- Monoklonální protilátky v léčbě hyperlipidemií
-
Všetky články tohto čísla
- Alcohol Intake and Blood Pressure: A Systematic Review Implementing a Mendelian Randomization Approach
- Could an Open-Source Clinical Trial Data-Management System Be What We Have All Been Looking For?
- Further Evidence that Exclusive Breast-Feeding Reduces Mother-to-Child HIV Transmission Compared With Mixed Feeding
- Determining Origins and Causes of Childhood Obesity via Mendelian Randomization Analysis
- Inferring HIV Transmission Dynamics from Phylogenetic Sequence Relationships
- Late-Life Cardiac Interventions and the Treatment Imperative
- It's the Network, Stupid: Why Everything in Medicine Is Connected
- Syndromic Surveillance: Adapting Innovations to Developing Settings
- The Potential Effect of Statins on Rituximab Immunotherapy
- PLOS Medicine
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Could an Open-Source Clinical Trial Data-Management System Be What We Have All Been Looking For?
- Syndromic Surveillance: Adapting Innovations to Developing Settings
- The Potential Effect of Statins on Rituximab Immunotherapy
- It's the Network, Stupid: Why Everything in Medicine Is Connected
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



