-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Assessing Antimalarial Efficacy in a Time of Change to Artemisinin-Based
Combination Therapies: The Role of Médecins Sans Frontières
article has not abstract
Published in the journal: Assessing Antimalarial Efficacy in a Time of Change to Artemisinin-Based Combination Therapies: The Role of Médecins Sans Frontières. PLoS Med 5(8): e169. doi:10.1371/journal.pmed.0050169
Category: Policy Forum
doi: https://doi.org/10.1371/journal.pmed.0050169Summary
article has not abstract
During the 1990s, high levels of Plasmodium falciparum (Pf) resistance to common antimalarials were reported from malaria-endemic countries, raising questions about the efficacy of chloroquine (CQ), then the mainstay of antimalarial treatment. Drug resistance was considered a prime contributing factor to increased malaria mortality and morbidity across Africa [1,2]. The natural successor to CQ, sulfadoxine-pyrimethamine (SP), had a short therapeutic lifespan [3], and the choice of an effective first-line regimen emerged as a key issue in Pf malaria control. Artemisinin-based combination therapy (ACT), adopted in southeast Asia since the early 1990s, appeared to be the best available option [3].
Summary Points
-
More than 12,000 patients were enrolled in 43 efficacy studies in 18 countries of Asia and Africa between 1996 and 2004, accounting for one fourth of the overall research output in these countries.
-
This has provided extensive evidence on the efficacy of most drug regimens currently in use for uncomplicated malaria, which was often used for treatment policy changes by the concerned countries.
-
The greatest contribution was in conflict-affected countries of sub-Saharan Africa, where studies represent the vast majority of available data and where “traditional” academic research institutions were not or barely represented.
-
The vast majority of the studies were published in peer-reviewed journals, which shows that research performed in difficult settings can be of a high enough standard to ensure publication and to be useful in policy change.
-
This work demonstrates the potential role of non-governmental agencies in collecting the necessary evidence to stimulate and inform policy change in international health.
Médecins Sans Frontières (Doctors Without Borders, or MSF) is a humanitarian medical aid organisation, dedicated to providing assistance to populations who lack access to health care. In the 1990s, antimalarial resistance was emergent in most countries where MSF was operating, but scientific evidence of this resistance was often lacking, and CQ or SP were still recommended by national malaria control programmes. Faced with a lack of data and the reluctance of international technical advisors and donors to review treatment strategies, MSF initiated in vivo studies to document the situation in its programme locations. While the primary aim was optimising treatment strategies for MSF patients, results were often used to formulate national policy change. Studies followed World Health Organization (WHO) recommendations [4,5], were usually conducted in insecure or difficult-to-access sites where data were absent, and were generally supported by MSF's epidemiological unit, Epicentre, in collaboration with national Ministries of Health, WHO, and other partners.
Here, we describe the output of MSF's work in antimalarial efficacy assessment during the last decade, and place it within the broader context of studies leading to regimen change from monotherapies to mostly artemisinin-based combinations during a critical decade in malaria control. We also describe challenges and lessons learned whilst carrying out this research and discuss its role within antimalarial policy change.
Descriptive Analysis of Efficacy Studies
Review methods.
We identified all malaria in vivo drug efficacy studies for which MSF was the main sponsor during 1996–2004, whether published in peer-reviewed journals or existing as unpublished reports in MSF operational centres (Brussels, Paris, Amsterdam, Barcelona, and Geneva; unpublished reports are available upon request from epimail@epicentre.msf.org). Only Pf studies were considered. For every study, we compiled country and site, year of completion, treatment group(s) tested, drug allocation method, length of post-enrolment follow-up (14 days or less; more than 14 days, i.e., at least 28-day follow-up), and failure rate with 95% confidence intervals. A treatment group is defined as the regimen tested. Multi-centric studies simultaneously evaluating several treatment groups within the same country were treated as single studies.
We calculated the proportion of MSF study treatment groups among all treatment groups tested against Pf per country during 1996 to 2004 by consulting the Global Malaria Program database (http://www.who.int/malaria/resistance.html). We reviewed the WHO Global Antimalarial Drug Policy Database (http://www.who.int/malaria/treatmentpolicies.html) and reference document [6] to establish the occurrence and timing of changes in treatment policy for uncomplicated malaria. We did not consider the introduction of CQ and SP in combination, as this was not a recommended option to replace either monotherapy [7]. We compared the new drug policy to findings and recommendations of the relevant MSF malaria studies and calculated the proportion of countries where recommendations made by MSF were concordant with subsequent national decisions regarding policy change.
To calculate the proportion of MSF papers among all published papers published in peer-reviewed journals, we searched PubMed to identify antimalarial studies published since 1996 until up to April 2007, performed in the countries in which MSF's studies had taken place, and reporting original in vivo efficacy data for treatment of uncomplicated Pf malaria in non-pregnant populations. Keywords were “malaria” and country of intervention (e.g., “Angola”).
Study output.
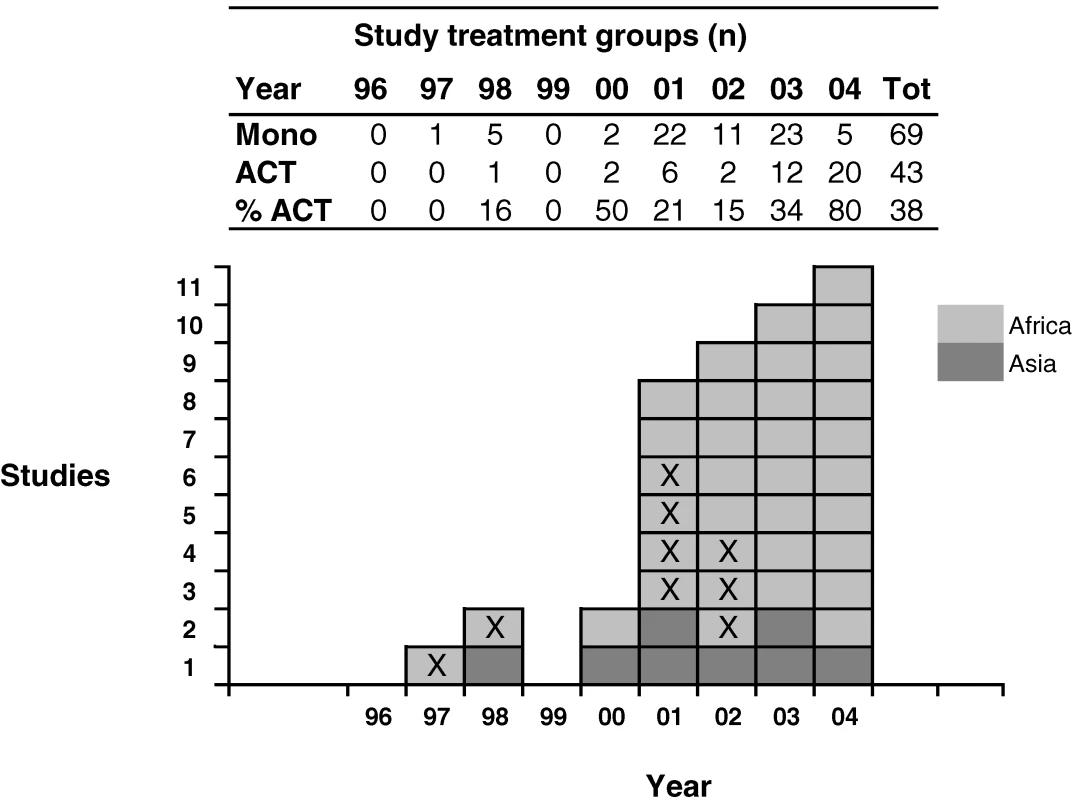
Between 1996 and 2004, MSF performed 43 efficacy studies or clinical trials in 18 countries, of which eight (17%) were in Asia (five countries) and 35 (83%) in Africa (13 countries) (Figure 1). Half of the studies took place in four African countries (21/43, 49%): Angola (n = 5), the Democratic Republic of the Congo (DRC, n = 6), Uganda (n = 5), and Sudan (n = 5). 12,145 patients were enrolled. Most studies (88%) were conducted between 2001 and 2004 and had a follow-up of 28 days or more (n = 34, 79%) with genotypic analysis of presumed failures/parasite recurrences to distinguish recrudescence from reinfection (Figure 2). Of studies with 28-day follow-up, 28/34 (82%) were published in peer-reviewed journals, and three out of 34 (9%) had been submitted to peer-reviewed journals at the time of writing; conversely, only three out of nine (33%) 14-day studies were published (Table 1).
Fig. 1. Flow Chart of Sites and Type of MSF Pf Efficacy Studies, 1996–2004 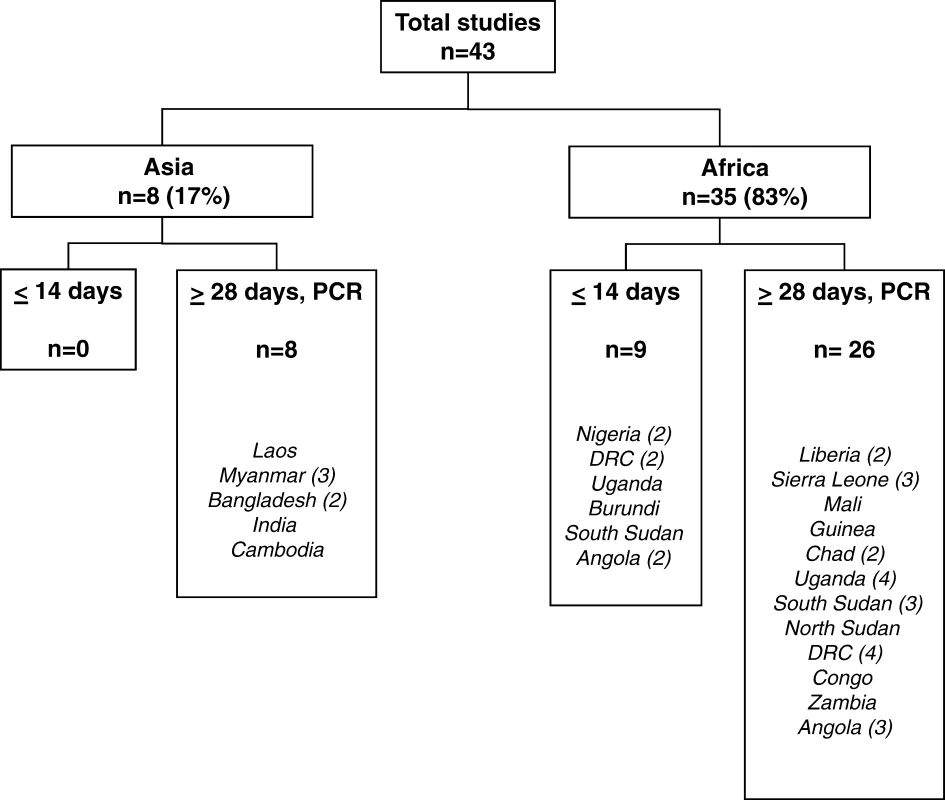
#tab:1#
Tab. 1. 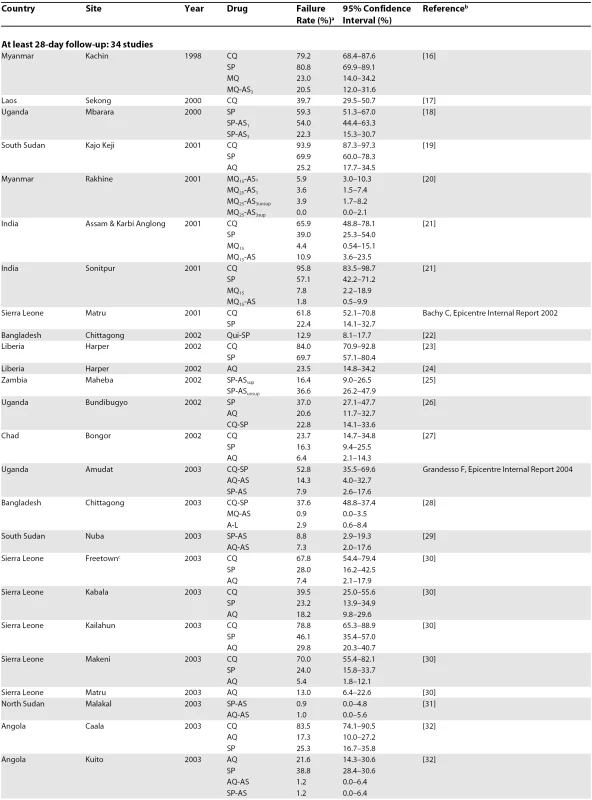
<sup>a</sup>These are usually 28-day PCR corrected failure rates, except in 6 studies: [<em class="ref">16</em>,<em class="ref">20</em>,<em class="ref">21</em>,<em class="ref">28</em>,<em class="ref">31</em>,<em class="ref">33</em>], where failure rates are given at day 42 or 63. Overall, nine (21%) studies were single arm, whereas 34 (79%) were comparative. Of the comparative studies, 22 (65%) were randomised. 117 treatment groups were investigated, of which 69 (59%) were monotherapies (SP, n = 27; CQ, n = 24; amodiaquine [AQ], n = 15; mefloquine [MQ], n = 3) and 48 (41%) were combinations. Most combinations (90%) were artemisinin-based (artesunate [AS]-SP, n = 14; AS-AQ, n = 12; AS-MQ, n = 10, artemether-lumefantrine, n = 5; dihydroartemisinin-piperaquine, n = 2); the remaining five were quinine-SP (n = 1) or CQ-SP (n = 4). The number of ACT studies increased over time, from one in 1998 to 20 (80% of total) in 2004 (Figure 2).
Contribution of MSF Studies to the Evidence for Policy Change
Within these 18 countries and during 1996–2004, 455 treatment groups were investigated, 112 (25%) by MSF (Table 2). The proportion of study groups investigated by MSF was higher for ACTs (46%) than monotherapies (19%), and higher in Africa than in Asia, both for monotherapies (23% versus 9%) and ACTs (57% versus 29%). Recommendations made by MSF were concordant with subsequent national decisions regarding policy change in 13/18 (72%) of the countries of intervention (Asia: two out of five [40%]; Africa: 11/13 [84%]).
Of the 43 MSF studies, 31 (72%) were published in peer-reviewed journals. MSF studies accounted for 23% (31/137) of all articles published during this period in the 18 countries of intervention (Table 3).
Tab. 2. 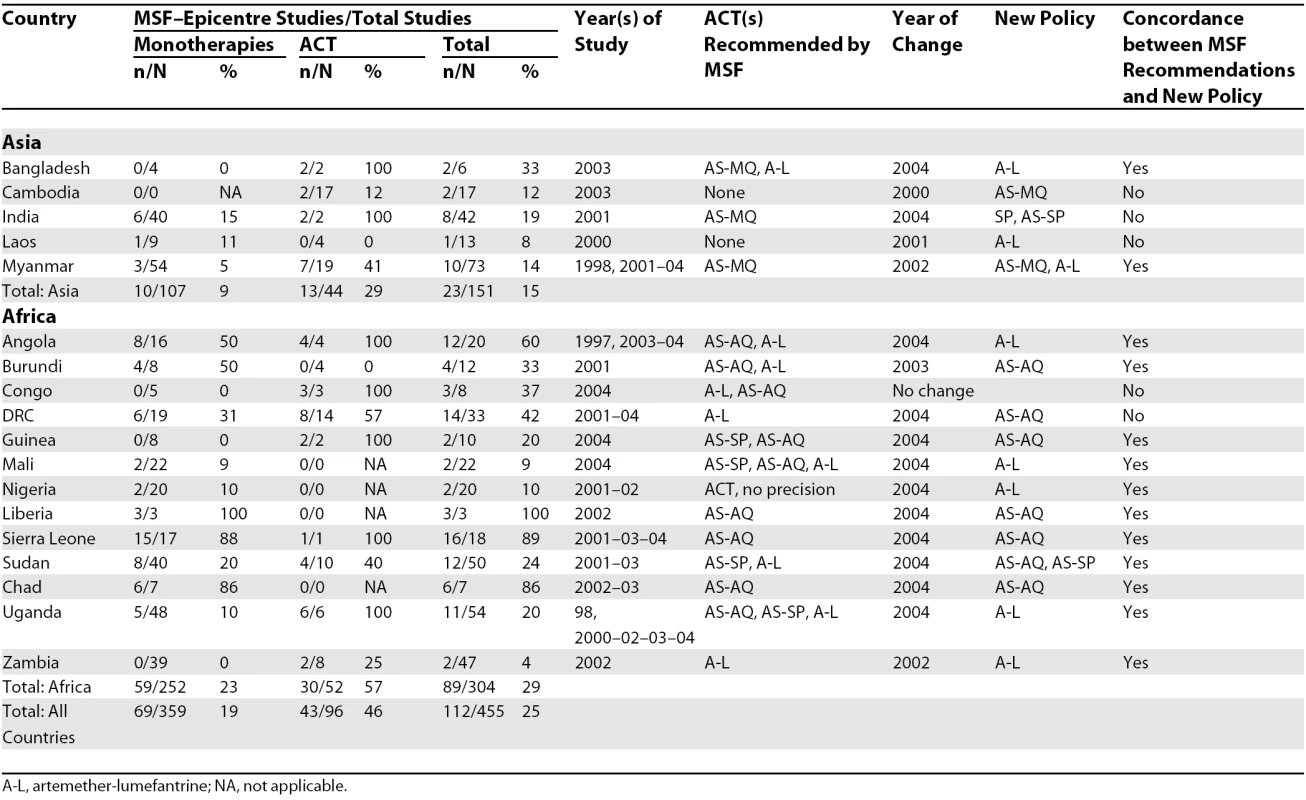
A-L, artemether-lumefantrine; NA, not applicable. MSF's largest output was in conflict-affected countries of sub-Saharan Africa, including Angola, Burundi, Chad, Liberia, Sierra Leone, and southern Sudan, where its studies represent the vast majority of available data, and where “traditional” academic research institutions were not or barely represented. Overall, MSF's study output accounted for one quarter of antimalarial drug efficacy research in 18 countries. Most studies were published in peer-reviewed journals.
Challenges and Lessons Learned
Generalisability of results obtained in crisis settings.
With the exception of Sierra Leone, where a national multi-centric study was carried out, the MSF studies were not necessarily representative of national trends. Armed conflict, forced displacement in Maheba, Zambia and Kailahun, Sierra Leone (potentially leading to the introduction of more or less resistant strains), and conflict-induced nutritional crises (leading to lower immuno-competence and thus impaired host response) that had recently affected many of the study populations (Angola; Burundi; DRC; Lankien, Mapel, and Nuba, southern Sudan; Sierra Leone; Amudat and Bundibugyo, Uganda) may have resulted in systematic differences in local antimalarial efficacy compared to other regions of the country. Evidence suggests that malnourished children have an increased risk of treatment failure [8–10]. Organisations conducting studies in crisis-affected settings need to consider the generalisability of their data carefully in addition to the more general problem of extrapolating findings from individual sites to wider populations.
Planning and organisational strategy.
MSF's contribution was not systematically planned but rather ad hoc, driven by its programmes. In retrospect, MSF's approach could have been more systematic, and more adherent to the standards of evidence-based medicine, in which randomised clinical trials are the primary tool by which inefficacious treatments are replaced once a more efficacious and equally safe alternative is identified. The approach shifted over time from measuring the efficacy of CQ and alternative potential partner drugs to combine with AS, to assuming that CQ was already inefficacious and focusing on head-on comparisons of different ACT combinations. MSF's strategy thus wavered between building an evidence base to argue against continued CQ use, trying to establish the baseline resistance of typical partner drugs, and a more pragmatic approach of directly investigating combinations.
Logistical and implementation challenges.
Carrying out field research in some of the remote settings proved extremely challenging. For example, Caala, Angola was under military siege and affected by a humanitarian emergency during the study period. In Bundibugyo, Uganda, security constraints due to rebel incursions necessitated innovative solutions to trace patients not attending follow-up, including field visits by clinicians and laboratory staff. Shabunda, DRC and most Sudanese sites were accessible only by plane or on foot. Laboratory facilities were usually established from scratch, without electricity and with the threat of possible sources of contamination and degradation of slides and blood samples. While most study personnel were from the country itself, it was necessary to either recruit qualified professionals from other areas of the country, or re-train local staff who had been unemployed for years because of health system collapse. The vast majority had no prior experience in research. Research procedures had to be adapted to programmes hitherto dedicated solely to emergency health care provision. The greatest evidence gaps may well be in remote locations featuring the most difficult research conditions. Organisations must be prepared to be flexible, innovative, and resourceful. Investment in basic infrastructure, training, and human resources is essential.
Follow-up and rescue treatment were also problematic. The WHO assessment protocol required investigators to withhold rescue treatment in case of asymptomatic parasite recurrence, which carries a high risk of avoidable morbidity [11]. Follow-up visits took place at one-week intervals, during which patients with known parasitaemia would remain without rescue treatment. On two occasions (two children treated respectively with AQ and CQ who were parasitaemic during follow-up and who did not come back for further visits), we believe this contributed to avoidable deaths from severe malaria. As a response, we instituted frequent home visits by field workers to detect any symptom progression.
Partly due to concerns about security-related interruptions to enrolment, a proportion of studies in the first half of the period were single arm or used sequential allocation procedures. Unplanned decisions to stop enrolment due to very high treatment failure were occasionally taken, thus exposing investigators to the criticism of having contravened the protocol; later, randomisation was introduced as the standard, along with systematic early stopping rules.
Quality versus timeliness.
Efforts were made to improve the quality of the studies, including establishment of routine laboratory quality control procedures (internal controls and review of slides by reference laboratories) and standard protocols and operating procedures for clinical and laboratory work. From 2003, follow-up was systematically extended to 28 days, and PCR genotyping analyses were always done to adjust failure rates for re-infections. This is broadly considered an appropriate method for assessing drug efficacy and therefore yielded realistic estimates for each site [12].
However, these analyses required the involvement of partner institutions (usually academic laboratories in Europe). Due to the heavy workload of these laboratories, PCR genotyping sometimes yielded considerable delays in releasing final results. In situations where treatment failure was severe, this raised an ethical dilemma of balancing the release of final results with the need for action. A common approach was to release preliminary, unadjusted failure rates based on 14-day follow-up, especially when these already warranted an urgent change of the current first-line therapy. This however often led to confusion, especially when subsequent 28-day results overturned the initial impression that other cheap non-ACT regimens were still efficacious (particularly SP, for which failures tend to occur late). Furthermore, MSF field officers mediating between study investigators and local stakeholders did not always have the technical expertise to discuss genotyping adjustment. With more complex methods, the extra time involved in ensuring that data are accurate must be weighed against the urgency of action in each setting. However, our experience shows that in order to avoid confusion it is preferable to await final results, as long as the delay is acceptable (to be determined on a case-by-case basis).
Ethical Issues
These studies presented ethical dilemmas common to research in crisis-affected populations [13]. Local clinicians had strong anecdotal evidence of poor drug efficacy, but lack of scientific evidence hindered advocacy to review treatment policies. Communities were particularly vulnerable to the effects of antimalarial drug resistance since they had poor access to health care, no recourse to efficacious second-line treatments, and limited civil rights and governance structures within which to voice their patient perspective. Furthermore, patients’ or caregivers’ ability to decide whether to participate in the study was severely constrained: the study venue was often their sole health care option, and their familiarity with biomedical concepts may have been insufficient to properly consider the risks and benefits of participation. Adhering to the strict follow-up schedule was also challenging, potentially entailing days of missed work.
In many countries there was no institutional review board (IRB), and protocols were approved by Ministry of Health directorates for research, as well as local health authorities. We considered that even in the absence of formal IRB review, generating evidence on antimalarial efficacy was essential to stimulate policy change. The assessment protocol was standardised and recommended by WHO; regimens were non-experimental; and patients’ risk of untoward outcomes was lower than in routine care due to the systematic follow-up and availability of second-line regimens in case of treatment failure. These considerations persuaded us that the harm–benefit ratio was favourable. This experience suggests that ethical risks of conducting research should always be weighed against the consequences of inaction. Measures to minimise risk include standardising protocols, ensuring locally appropriate, understandable consent procedures, developing alternative structures for ethics review, and involving the community.
Future Research Challenges
Recently, several players have become involved in antimalarial efficacy assessment, and there are global initiatives to co-ordinate studies [14]. Today's challenges are different: (1) to detect resistance to ACTs as early as possible, best done by combining molecular and in vivo studies, and defining strategic surveillance sites where resistance is more likely to arise de novo or be introduced from other regions; and (2) to demonstrate that new regimens (e.g., dihydroartemisinin-piperaquine) are at least as efficacious as current first-line ACTs and carry additional benefits in terms of safety, cost, or feasibility: this would require non-inferiority rather than comparative trial designs [15].
Conclusions
Our analysis shows that research can be performed in difficult settings to a high enough standard to ensure publication and to be useful in policy change.
MSF's work shows that nongovernmental organisations (NGOs) can provide extensive evidence on the efficacy of most antimalarial regimens. This evidence probably affected malaria treatment policy decisions, as suggested by the high number of countries where recommendations and decisions were the same. However, this conclusion has to be drawn with caution: factors leading to policy change are many and difficult to measure, as are reasons for adopting one regimen over another.
As part of their mandate, medical NGOs should be prepared to fill gaps in evidence, including evaluating current tools to control tropical diseases in hard-to-reach populations, and demonstrating the effectiveness of alternatives. Dissemination of findings in peer-reviewed journals is crucial to bolster the validity of such research and inform international policy and advocacy. While operational research can successfully be undertaken by NGOs, national malaria control programmes, WHO, and other major international disease control partnerships hold the primary responsibility for initiating such studies. Had such institutions stimulated a systematic process of monitoring antimalarial efficacy from the onset of reports of drug resistance, change might have occurred earlier. Finally, it is important that complacency does not set in. Artemisinin resistance may well arise, and countries, international bodies, and NGOs need to prospectively monitor the situation to avoid history repeating itself.
Zdroje
1. TrapeJF
2001
The public health impact of chloroquine resistance in Africa.
Am J Trop Med Hyg
64
1–2 Suppl
12
17
2. ZuckerJRRuebushTKIIObonyoCOtienoJCampbellC
2003
The mortality consequences of the continued use of chloroquine in Africa:
Experience in Siaya, Western Kenya.
Am J Trop Med Hyg
68
386
390
3. WhiteNJNostenFLooareesuwanSWatkinsWMMarshK
1999
Averting a malaria disaster.
Lancet
353
1965
1967
4. World Health Organization
1996
Assessment of therapeutic efficacy of antimalarial drugs for uncomplicated
falciparum malaria in areas with intense transmission.
Available: http://www.who.int/drugresistance/malaria/en/Assessment_malaria_96.pdf.
Accessed 7 July 2008
5. World Health Organization
2003
Assessment and monitoring of antimalarial drug efficacy for the treatment
of uncomplicated falciparum malaria.
Available: http://www.who.int/malaria/docs/ProtocolWHO.pdf. Accessed 7 July
2008
6. World Health Organization
2005
Susceptibility of Plasmodium
falciparum to antimalarial drugs.
Report on global monitoring, 1996–2004. Available: http://www.who.int/malaria/rbm/Attachment/20041108/SusceptibilityPlasmodium_report.pdf.
Accessed 7 July 2008
7. World Health Organization
2003
Position of WHO's Roll Back Malaria Department on malaria treatment policy.
Available: http://www.who.int/malaria/treatmentguidelines.html. Accessed 7 July
2008
8. HessFIIannuzziALeafasiaJCowdreyDNothdurftHD
1996
Risk factors of chloroquine resistance in Plasmodium falciparum malaria.
Acta Trop
61
293
306
9. HamelMJHoltzTMkandalaCKaimilaNChizaniN
2005
Efficacy of trimethoprim-sulfamethoxazole compared with
sulfadoxine-pyrimethamine plus erythromycin for the treatment of uncomplicated malaria
in children with integrated management of childhood illness dual classifications of
malaria and pneumonia.
Am J Trop Med Hyg
73
609
615
10. OlanrewajuWIJohnsonAW
2001
Chloroquine-resistant Plasmodium falciparum malaria in Ilorin, Nigeria: Prevalence and risk
factors for treatment failure.
Afr J Med Med Sci
30
165
169
11. OlliaroPPinogesLChecchiFVaillantMGuthmannJP
2008
Risk associated with asymptomatic parasitaemia occurring post-antimalarial
treatment.
Trop Med Int Health
13
83
90
12. GuthmannJPPinogesLChecchiFCousensSBalkanS
2006
Methodological issues in the assessment of antimalarial drug treatment:
Analysis of 13 studies in eight African countries from 2001 to 2004.
Antimicrob Agents Chemother
50
3734
3739
13. Committee on Population, National Research Council
2002
Research ethics in complex humanitarian emergencies: Summary of a workshop.
National Academy Press.
Available: http://books.nap.edu/catalog.php?record_id=10481. Accessed 7 July
2008
14. PriceRDorseyGAshleyEBarnesKBairdJK
2007
World Antimalarial Resistance Network I: Clinical efficacy of antimalarial
drugs.
Malar J
6
119
15. StepniewskaKWhiteNJ
2006
Some considerations in the design and interpretation of antimalarial drug
trials in uncomplicated falciparum malaria.
Malar J
5
127
16. SmithuisFShahmaneshMKyawMKSavranOLwinS
2004
Comparison of chloroquine, sulfadoxine/pyrimethamine, mefloquine and
mefloquine-artesunate for the treatment of falciparum malaria in Kachin State, North
Myanmar.
Trop Med Int Health
9
1184
1190
17. GuthmannJPKasparianSPhetsouvanhRNathanNGarciaM
2002
The efficacy of chloroquine for the treatment of acute, uncomplicated,
Plasmodium falciparum
malaria in Laos.
Ann Trop Med Parasitol
96
553
557
18. PriottoGKabakyengaJPinogesLRuizAErikssonT
2003
Artesunate and sulfadoxine-pyrimethamine combinations for the treatment of
uncomplicated Plasmodium
falciparum malaria in Uganda: A randomized, double-blind,
placebo-controlled trial.
Trans R Soc Trop Med Hyg
97
325
330
19. StivanelloECavaillerPCassanoFOmarSAKariukiD
2004
Efficacy of chloroquine, sulphadoxine-pyrimethamine and amodiaquine for
treatment of uncomplicated Plasmodium
falciparum malaria in Kajo Keji county, Sudan.
Trop Med Int Health
9
975
980
20. SmithuisFvan der BroekIKattermanNKyawMKBrockmanA
2004
Optimising operational use of artesunate-mefloquine: A randomised
comparison of four treatment regimens.
Trans R Soc Trop Med Hyg
98
182
192
21. CampbellPBaruahSNarainKRogersCC
2006
A randomized trial comparing the efficacy of four treatment regimens for
uncomplicated falciparum malaria in Assam state, India.
Trans R Soc Trop Med Hyg
100
108
118
22. van den BroekIVvan der WardtSTalukderLChakmaSBrockmanA
2004
Drug resistance in Plasmodium
falciparum from the Chittagong Hill Tracts, Bangladesh.
Trop Med Int Health
9
680
687
23. ChecchiFDurandRBalkanSVonhmBTKollieJZ
2002
High Plasmodium
falciparum resistance to chloroquine and sulfadoxine-pyrimethamine in
Harper, Liberia: Results in vivo and analysis of point mutations.
Trans R Soc Trop Med Hyg
96
664
669
24. ChecchiFBalkanSVonhmBTMassaquoiMBibersonP
2002
Efficacy of amodiaquine for uncomplicated Plasmodium falciparum malaria in Harper,
Liberia.
Trans R Soc Trop Med Hyg
96
670
673
25. DepoortereEGuthmannJPPresséJSipilanyambeNNkanduE
2005
Efficacy and effectiveness of the combination of sulfadoxine/pyrimethamine
and a 3-day course of artesunate for the treatment of uncomplicated falciparum malaria
in a refugee settlement in Zambia.
Trop Med Int Health
10
139
145
26. ChecchiFPiolaPKosackCArdizzoniEKlarkowskiD
2004
Antimalarial efficacy of sulfadoxine-pyrimethamine, amodiaquine and a
combination of chloroquine plus sulfadoxine-pyrimethamine in Bundi Bugyo, western Uganda.
Trop Med Int Health
9
445
450
27. GrandessoFBachyCDonamINtambiJHabimanaJ
2006
Efficacy of chloroquine, sulfadoxine-pyrimethamine and amodiaquine for
treatment of uncomplicated Plasmodium
falciparum malaria among children under five in Bongor and Koumra,
Chad.
Trans R Soc Trop Med Hyg
100
419
426
28. van den BroekIVMaungUAPetersALiemLKamalM
2005
Efficacy of chloroquine + sulfadoxine–pyrimethamine,
mefloquine + artesunate and artemether + lumefantrine combination
therapies to treat Plasmodium
falciparum malaria in the Chittagong Hill Tracts, Bangladesh.
Trans R Soc Trop Med Hyg
99
727
735
29. HamourSMelakuYKeusKWambuguJAtkinS
2005
Malaria in the Nuba Mountains of Sudan: Baseline genotypic resistance and
efficacy of the artesunate plus sulfadoxine-pyrimethamine and artesunate plus
amodiaquine combinations.
Trans R Soc Trop Med Hyg
99
548
554
30. ChecchiFRoddyPKamaraSWilliamsAMorineauG
2005
Evidence basis for antimalarial policy change in Sierra Leone: Five in vivo
efficacy studies of chloroquine, sulphadoxine-pyrimethamine and amodiaquine.
Trop Med Int Health
10
146
153
31. van den BroekIAmsaluRBalasegaramMHepplePAlemuE
2005
Efficacy of two artemisinin combination therapies for uncomplicated
falciparum malaria in children under 5 years, Malakal, Upper Nile, Sudan.
Malar J
4
14
32. GuthmannJPAmpueroJFortesFvan OvermeirCGaboulaudV
2005
Antimalarial efficacy of chloroquine, amodiaquine,
sulfadoxine-pyrimethamine, and the combinations of amodiaquine + artesunate and
sulfadoxine-pyrimethamine + artesunate in Huambo and Bie provinces, central
Angola.
Trans R Soc Trop Med Hyg
99
485
492
33. JanssensBvan HerpMGoubertLChanSUongS
2007
A randomized open study to assess the efficacy and tolerability of
dihydroartemisinin-piperaquine for the treatment of uncomplicated falciparum malaria in
Cambodia.
Trop Med Int Health
12
251
259
34. BonnetMRoperCFélixMCoulibalyLKankolongoGM
2007
Efficacy of antimalarial treatment in Guinea: In vivo study of two
artemisinin combination therapies in Dabola and molecular markers of resistance to
sulphadoxine-pyrimethamine in N’Zérékoré.
Malar J
6
54
35. SwarthoutTDvan den BroekIVKayembeGMontgomeryJPotaH
2006
Artesunate + amodiaquine and artesunate +
sulphadoxine-pyrimethamine for treatment of uncomplicated malaria in Democratic Republic
of Congo: A clinical trial with determination of sulphadoxine and
pyrimethamine-resistant haplotypes.
Trop Med Int Health
11
1503
1511
36. van den BroekIKitzCAl AttasSLibamaFBalasegaramM
2006
Efficacy of three artemisinin combination therapies for the treatment of
uncomplicated Plasmodium
falciparum malaria in the Republic of Congo.
Malar J
5
113
37. PiolaPFoggCBajunirweFBiraroSGrandessoF
2005
Supervised versus unsupervised intake of six-dose artemether-lumefantrine
for treatment of acute, uncomplicated Plasmodium falciparum malaria in Mbarara, Uganda: A randomised trial.
Lancet
365
1467
1473
38. GuthmannJPCohuetSRiguttoCFortesFSaraivaN
2006
High efficacy of two artemisinin-based combinations (artesunate +
amodiaquine and artemether + lumefantrine) in Caala, Central Angola.
Am J Trop Med Hyg
75
143
145
39. GrandessoFHagermanAKamaraSLamEChecchiF
2006
Low efficacy of the combination artesunate plus amodiaquine for
uncomplicated falciparum malaria among children under 5 years in Kailahun, Sierra Leone.
Trop Med Int Health
11
1017
1021
40. de RadiguèsXDialloKIDialloMNgwakumPAMaigaH
2006
Efficacy of chloroquine and sulfadoxine/ pyrimethamine for the treatment of
uncomplicated falciparum malaria in Koumantou, Mali.
Trans R Soc Trop Med Hyg
100
1013
1018
41. SmithuisFKyawMKPheOAyeKZHtetL
2006
Efficacy and effectiveness of dihydroartemisinin-piperaquine versus
artesunate-mefloquine in falciparum malaria: An open-label randomised comparison.
Lancet
367
2075
2085
42. LegrosDJohnsonKHoupikianPMakangaMKabakyengaJK
2002
Clinical efficacy of chloroquine or sulfadoxine-pyrimethamine in children
under five from south-western Uganda with uncomplicated falciparum malaria.
Trans R Soc Trop Med Hyg
96
199
201
43. KazadiWMVongSMakinaBNMantshumbaJCKabuyaW
2003
Assessing the efficacy of chloroquine and sulfadoxine-pyrimethamine for
treatment of uncomplicated Plasmodium
falciparum malaria in the Democratic Republic of Congo.
Trop Med Int Health
8
868
875
44. van den BroekIVGatkoiTLowokoBNzilaAOchongE
2003
Chloroquine, sulfadoxine-pyrimethamine and amodiaquine efficacy for the
treatment of uncomplicated Plasmodium
falciparum malaria in Upper Nile, south Sudan.
Trans R Soc Trop Med Hyg
97
229
235
Štítky
Interné lekárstvo
Článok vyšiel v časopisePLOS Medicine
Najčítanejšie tento týždeň
2008 Číslo 8- Parazitičtí červi v terapii Crohnovy choroby a dalších zánětlivých autoimunitních onemocnění
- Intermitentní hladovění v prevenci a léčbě chorob
- Statinová intolerance
- Co dělat při intoleranci statinů?
- Monoklonální protilátky v léčbě hyperlipidemií
-
Všetky články tohto čísla
- Predicting Outcome after Traumatic Brain Injury: Development and International Validation of Prognostic Scores Based on Admission Characteristics
- Greater Response to Placebo in Children Than in Adults: A Systematic Review and Meta-Analysis in Drug-Resistant Partial Epilepsy
- Can a Topical Microbicide Prevent Rectal HIV Transmission?
- Developing a Prognostic Model for Traumatic Brain Injury—A Missed Opportunity?
- Assessing Antimalarial Efficacy in a Time of Change to Artemisinin-Based Combination Therapies: The Role of Médecins Sans Frontières
- Children Are Not Just Small Adults: The Urgent Need for High-Quality Trial Evidence in Children
- The Use of Nonhuman Primate Models in HIV Vaccine Development
- More Evidence Against a Causal Association between C-Reactive Protein and Diabetes
- Strategies to Reduce Mortality from Bacterial Sepsis in Adults in Developing Countries
- Ensuring the Involvement of Children in the Evaluation of New Tuberculosis Treatment Regimens
- An Acute Evolving Flaccid Quadriparesis in an Elderly Woman
- PLOS Medicine
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Ensuring the Involvement of Children in the Evaluation of New Tuberculosis Treatment Regimens
- Predicting Outcome after Traumatic Brain Injury: Development and International Validation of Prognostic Scores Based on Admission Characteristics
- The Use of Nonhuman Primate Models in HIV Vaccine Development
- Strategies to Reduce Mortality from Bacterial Sepsis in Adults in Developing Countries
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy