-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Intimate Partner Violence and Depression Symptom Severity among South African Women during Pregnancy and Postpartum: Population-Based Prospective Cohort Study
In a population-based prospective cohort study, Alexander C. Tsai and colleagues examine bidirectional associations between intimate partner violence and depressed mood among pregnant and postpartum women living near Cape Town, South Africa.
Published in the journal: Intimate Partner Violence and Depression Symptom Severity among South African Women during Pregnancy and Postpartum: Population-Based Prospective Cohort Study. PLoS Med 13(1): e32767. doi:10.1371/journal.pmed.1001943
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1001943Summary
In a population-based prospective cohort study, Alexander C. Tsai and colleagues examine bidirectional associations between intimate partner violence and depressed mood among pregnant and postpartum women living near Cape Town, South Africa.
Introduction
Violence against women by intimate partners remains unacceptably common worldwide [1–5], particularly in South Africa, where violence against women occurs at rates that are among the highest in the world [6–9]. The cross-sectional association between intimate partner violence (IPV) and adverse mental health-related outcomes among women is well known [10–12]. These studies are consistent with a broader body of literature linking stressful life events with incident major depressive episodes [13–15], as well as literature linking traumatic stressors to post-traumatic stress disorder and suicide [16–18]. Moreover, acts of violence against women perpetuate gender-unequal norms about the acceptability of violence, which itself compromises women’s reproductive health and decision-making irrespective of any direct exposure to violence [2,19–22].
In a recently published systematic review, Devries and colleagues [23] identified 13 longitudinal studies linking IPV to incident depression, none of which were conducted in sub-Saharan Africa. This is an important gap in the literature because rates of partner and non-partner violence in sub-Saharan Africa are among the highest in the world [4,5]. Methodologically, the importance of conducting longitudinal studies in this field was highlighted by Foa and colleagues [24], whose conceptual model suggests that psychological difficulties may be a risk factor for subsequent victimization. For example, women with poor mental health may selectively partner with men who also have poor mental health (which is a risk factor for perpetration [25]) or have greater difficulty extracting themselves from abusive relationships [26]. Also consistent with this line of inquiry are intervention studies showing that effective depression treatment can reduce the probability of re-victimization [27]. Short of experimental study designs like these, longitudinal studies offer a design superior to cross-sectional studies in their ability to adjust for unobserved confounding and ensure temporal ordering of the exposures and outcomes of interest. Since the publication of the review by Devries and colleagues [23], one recent study showed that sexual violence was associated with depression among HIV-positive women in rural Uganda [28], but interpretation of those findings was limited by the study’s small sample size, relatively unique population, and the observation of relatively few exposure events.
To address these gaps in the literature, we analyzed longitudinal data collected during the course of a 3-y cluster-randomized trial conducted in 2009–2014 with more than 1,200 pregnant women living in 24 neighborhoods near Cape Town, South Africa. The primary aim of the randomized trial was to determine whether a community-based home visiting intervention could improve maternal and child health over 3 y post-birth. With repeated measures of both IPV and depression symptom severity, these data offered us the opportunity to estimate the association between IPV and depression while adjusting for both observed and unobserved confounding.
Materials and Methods
Ethics Statement
All interviews were conducted in accordance with ethical and safety recommendations promulgated by the World Health Organization [29]. Namely, research assistants were trained on how to administer surveys for gathering sensitive information and provided assurances of confidentiality. The survey was framed generally as being part of a study of family health and well-being, not a study about violence against women. In consultation with on-site supervisors, research assistants provided referrals to local counseling resources and/or child social services as needed, with standardized protocols in place to refer women to emergency services in the case of acutely elevated risk of harm to self or harm from others. All study procedures were approved by the South General Institutional Review Board of the University of California at Los Angeles and the Health Research Ethics Committee of the Stellenbosch University Faculty of Health Sciences. A four-person Data Safety Monitoring Board populated by local and international experts monitored implementation of the study. The secondary analysis described in this manuscript was based on a de-identified dataset and did not require additional approval or consent.
Study Population
Details of the study design, field training, and primary outcome analyses at 6, 18, and 36 mo have already been published [30–35] (ClinicalTrials.gov registration NCT00972699). The study was conducted during 2009–2014 in three townships surrounding Cape Town, South Africa. All pregnant women living in 24 neighborhoods (matched on population density, number of bars, distance to health care, and access to public works infrastructure) were identified and recruited into the study, with a 98% participation rate. These matched neighborhoods were randomized in blocks of four to either a home visiting intervention or standard clinic care groups. Standard clinic care was available (within 5 kilometers) to all women living in the study catchment area and generally consisted of tuberculosis and HIV testing, partner HIV testing, antiretroviral therapy, antenatal and postnatal care, well-child clinics, and primary health care [30].
The home visiting intervention was implemented by the Philani Maternal, Child Health, and Nutrition Project, a non-governmental organization that has been operating in the Western Cape of South Africa since 1979 [36] and which has since expanded to the Eastern Cape of South Africa as well as Ethiopia and Swaziland. Philani implements a “mentor mother” program, recruiting women from the community who have successfully raised thriving children despite concentrated adversity and then training these women to serve as paraprofessional community health workers for home visiting among pregnant women and their families [37,38]. For the purposes of the randomized trial, the Philani intervention was standardized and augmented with training in a pragmatic model of problem-solving and cognitive-behavioral techniques to address major community health challenges, including HIV/tuberculosis, malnutrition, and alcohol use [39,40,41]. An independent team of Xhosa-speaking research assistants obtained written informed consent from all study participants and collected survey data through face-to-face interviews conducted at baseline, 6 mo, 18 mo, and 36 mo. Analyses of these data revealed that the “Philani Plus” intervention improved overall maternal and child health across a number of different outcomes, notably those related to HIV-prevention behaviors, breastfeeding, and child growth over 18 mo; and maternal emotional well-being, child language development, and child growth over 36 mo [31–35].
Measures
The primary outcome of interest in this secondary analysis was depression symptom severity, which was measured at all time points with the Xhosa version of the ten-item Edinburgh Postnatal Depression Scale (EPDS) [42]. Scale items inquire about depressive symptoms within a 7-d recall period, with responses scored on a four-point Likert-type scale ranging from 0 (“not at all”) to 3 (“all the time”). Among Xhosa-speaking women, the EPDS has been shown to have a coherent internal structure [43], high sensitivity and specificity for detecting major depressive disorder [44–46], and good construct validity [39,47]. In the baseline sample, the EPDS had good internal consistency (Cronbach’s alpha = 0.89), and, using 500 bootstrap replications to compute the standard error, the 95% confidence interval (CI) was 0.88–0.90.
The primary explanatory variable of interest in this secondary analysis was experience of IPV, measured with a four-item scale. Following Straus’ [48] approach of asking behaviorally specific questions, the IPV scale included items inquiring about the frequency with which a woman’s current or previous intimate partner had, during the past 12 mo, slapped or thrown anything at her; pushed or shoved her; hit her with a fist or another object; or threatened or attacked her with a gun, knife, or other weapon. Responses were scored on a four-point Likert-type scale ranging from 1 (“never”) to 4 (“many”). Together, these four items had acceptable internal consistency, with a Cronbach’s alpha of 0.75 (95% CI, 0.71–0.80) in the baseline sample. To generate an omnibus measure of the intensity of IPV across all four items, following Kling and colleagues [49] we defined a summary IPV index as the equally weighted average of the four z-scores (i.e., each item was standardized to a mean of 0 and standard deviation of 1, and then the summary index was defined as their average value). While the absolute values of the index carry no meaning, higher values denote greater intensity of IPV.
We adjusted our estimates of the association between IPV intensity and depression symptom severity for a number of potentially confounding time-invariant and time-varying covariates. Time-invariant covariates were elicited at the baseline interview and included binary indicators denoting whether the participant had been assigned to the intervention or standard clinic care arm, age at baseline, and whether the participant had completed high school. Household asset wealth was elicited by asking participants a series of 13 questions about household assets and housing characteristics (e.g., whether there is a flush toilet in the home, whether a household member owns a radio, etc.). Then, following the method of Filmer and Pritchett [50], we applied principal components analysis to these variables. The first principal component was retained and used to define the asset wealth index, and participants were sorted into quintiles of relative asset wealth.
Time-varying covariates were elicited at each interview. Time elapsed since the baseline interview was measured in months. We included binary indicators denoting whether the participant was employed (either full - or part-time), whether the father of the child was staying with the participant, HIV serostatus (classified as HIV-positive, HIV-negative, or unknown/refused testing), and whether the participant had been diagnosed with high blood pressure or diabetes. Household monthly income was measured in South African Rand. Alcohol abuse was measured with the three-item consumption subset of the Alcohol Use Disorders Identification Test (AUDIT-C) [51–53].
Statistical Analysis
We did not publish or pre-register a plan for this secondary analysis. The analysis plan is described below, with any deviations noted in S1 Text. Given the repeated-measures design, we sought to estimate the association between IPV intensity and depression symptom severity, adjusted for the time-invariant and time-varying covariates described above. We fitted a linear regression model to the pooled cross-sectional data, specifying the EPDS score as the continuous dependent variable, using cluster-correlated robust estimates of variance [54–56] to correct standard errors for clustering within participants over time. To ensure the correct temporal sequence of the exposure and outcome, IPV measurements were lagged by one time point (an average of 12 mo). The estimated regression coefficients therefore provided information about the association between IPV intensity at one time point and depression symptom severity at the subsequent time point. We sought to determine whether the adverse impacts of IPV were experienced to a greater extent by women at the upper end of the conditional depression distribution. To do this, we fitted quantile regression models [57] to estimate the association between IPV intensity and the 20th, 40th, 60th, and 80th percentiles of the conditional depression distribution, using a covariance matrix of the asymptotic distribution of the quantile regression estimator that permits within-participant correlation over time [58].
Although the regression models included adjustment for a number of potentially important confounding variables, it is possible that some important variables were not observed. For example, in the specific setting of this randomized trial, no data on participants’ histories of child sexual abuse were obtained. Child sexual abuse could potentially confound our estimates of the association between IPV intensity and depression symptom severity [23]; even in the lagged-covariate models where the exposure precedes the outcome, the confounding influence of child sexual abuse would precede both the exposure and the outcome. Estimates could be similarly biased by omitting other types of childhood adversities, such as paternal incarceration or orphanhood [59,60]. We therefore fitted a fixed effects regression model to the data, using within-participant variation over time to identify the estimated associations [61]. The estimated regression coefficients are interpreted as providing information about the association between changes in IPV intensity and changes in depression symptom severity. A substantial advantage of the fixed effects regression model is that the procedure adjusts for confounding, whether observed or unobserved, that is time-invariant over the period of study (such as history of child abuse). The principal disadvantage of the fixed effects regression model is that, because the fixed effects sweep out all time-invariant confounding, only associations between changes in the outcome and changes in time-varying covariates can be examined. Because time-invariant covariates, by definition, do not change over time, they are eliminated from the model. To determine whether changes in IPV intensity were differentially associated with changes in depression symptom severity at different points in the conditional depression distribution, we used Canay’s [62] fixed effects quantile regression model.
Sensitivity Analyses
We conducted a number of ancillary analyses to assess the robustness of our main findings. First, to confirm that our findings were robust to the specification of the IPV variable, we generated dichotomous exposure variables indicating the presence or absence of any exposure to each of the four types of IPV. These four dichotomous exposure variables were included in the multivariable regression models both independently and jointly as lagged covariates. Second, because caseness for (probable) depression is frequently of clinical interest, we defined probable depression as EPDS ≥13 [45,46,63–65]. We fitted logistic regression models as above, instead specifying probable depression as the binary dependent variable. We also report marginal effects [66] so that the logistic regression coefficients can be interpreted as the percentage-point probability difference in the outcome associated with the covariates. Third, to determine the extent to which the association was potentially bidirectional [23,67], we re-fitted the regression model with IPV intensity as the dependent variable and depression symptom severity as a lagged covariate, thereby estimating the association between depression symptom severity at one time point and IPV intensity at the subsequent time point.
Results
Characteristics of the Sample
Summary statistics for the sample are displayed in Table 1. Of 1,238 women initially randomized, there were 117 mother-child dyads in which either the mother or the child died, and these were removed from the study (and, therefore, this analysis) [68]. Of these, 958 (85%) remained at 36-mo follow-up. Women lost to follow-up had a lower median EPDS (7 versus 10; p = 0.87 on the non-parametric equality-of-medians test) and were similar on the four types of IPV exposures (p-values on χ2 tests ranged from 0.16–0.99). Women lost to follow-up had lower household asset wealth (p = 0.06) and were less likely to be employed at baseline (p = 0.051) but were otherwise similar on other covariates (p-values ranged from 0.16–0.97).
Tab. 1. Baseline characteristics of the sample. 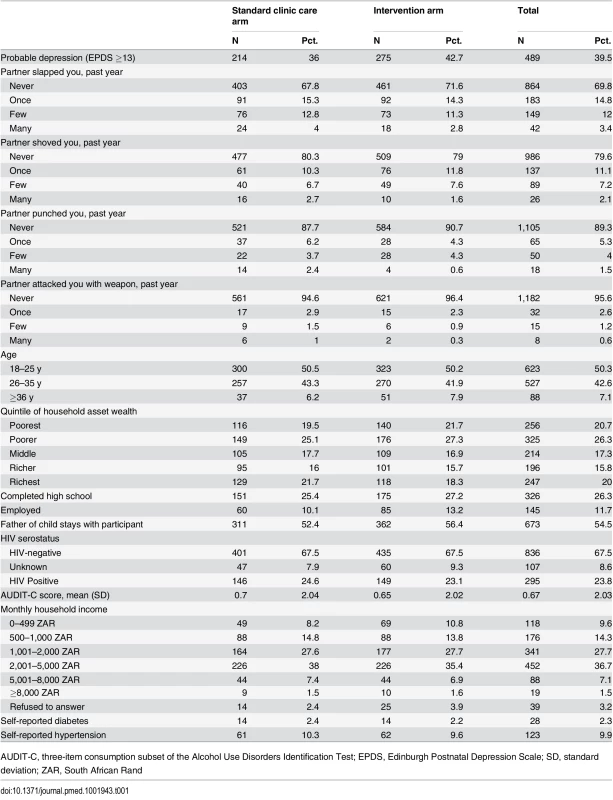
AUDIT-C, three-item consumption subset of the Alcohol Use Disorders Identification Test; EPDS, Edinburgh Postnatal Depression Scale; SD, standard deviation; ZAR, South African Rand For most variables there was a sufficient degree of variation within participants over time. The EPDS had an intra-class correlation (ICC) of 0.19, and the IPV index had an ICC of 0.32, suggesting that most of the total variance was “within group” (over time) rather than “between group.” Intra-class correlation values ranged from 0.12–0.66 for the time-varying covariates, with HIV serostatus (plausibly) featuring the highest intra-class correlation at 0.84.
IPV Intensity and Depression Symptom Severity
At baseline, the prevalence of any IPV varied from 4.4–30.2%, and 39.5% of women screened positive for depression. Kernel density plots suggested that greater frequency of IPV, regardless of type, was associated with greater depression symptom severity (Fig 1). As is apparent in the figure, both the location and shape of the plots suggest the need to investigate changes in the mean and the distribution of the outcome. After multivariable adjustment, IPV intensity had a strong and statistically significant association with depression symptom severity, regardless of the specification. In the pooled cross-sectional analysis, the estimated association between lagged IPV intensity and depression symptom severity was statistically significant (regression coefficient b = 1.04; 95% CI, 0.61–1.47) (Table 2). The quantile regression results, also shown in Table 2, indicate that IPV had an approximately 4 - to 5-fold greater impact on depression symptom severity in the upper quintiles of the conditional depression distribution.
Fig. 1. Kernel density plots of depression symptom severity, by type and frequency of intimate partner violence. 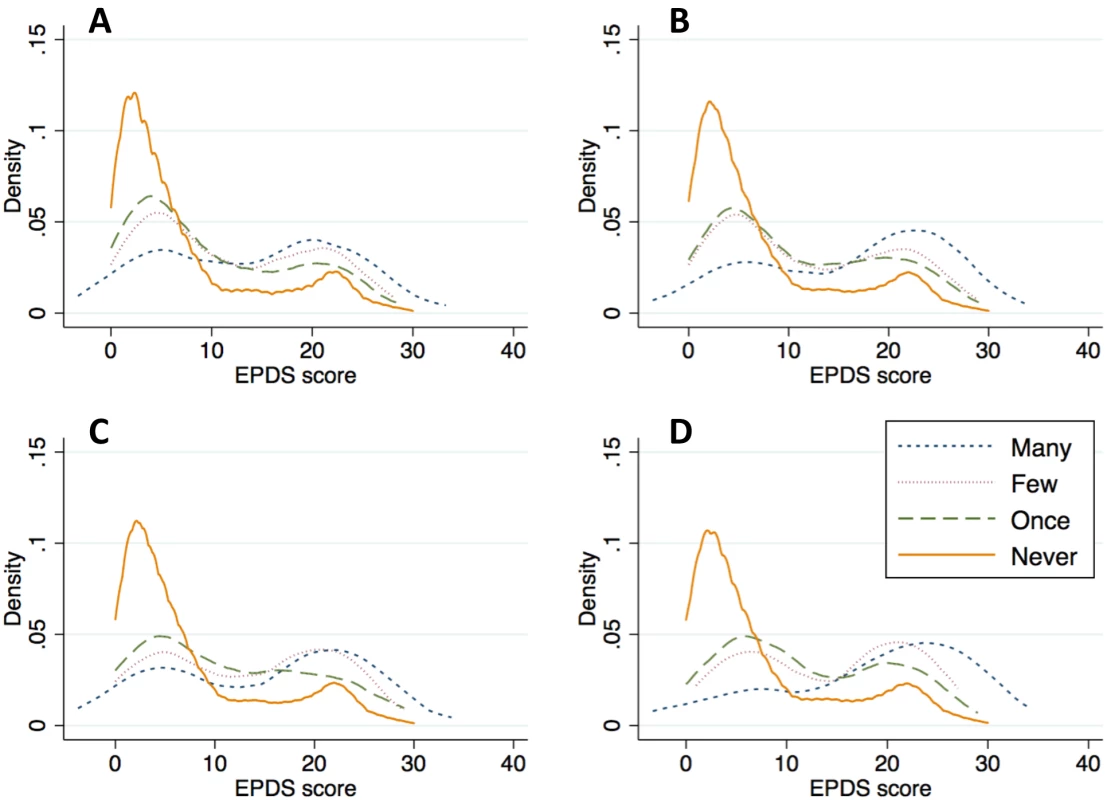
The scale includes items inquiring about the frequency with which a women’s current or previous intimate partner had, during the past 12 mo, (A) slapped or thrown anything at her; (B) pushed or shoved her; (C) hit her with a fist or another object; or (D) threatened or attacked her with a gun, knife, or other weapon. Tab. 2. Association between depression symptom severity and lagged intensity of intimate partner violence. 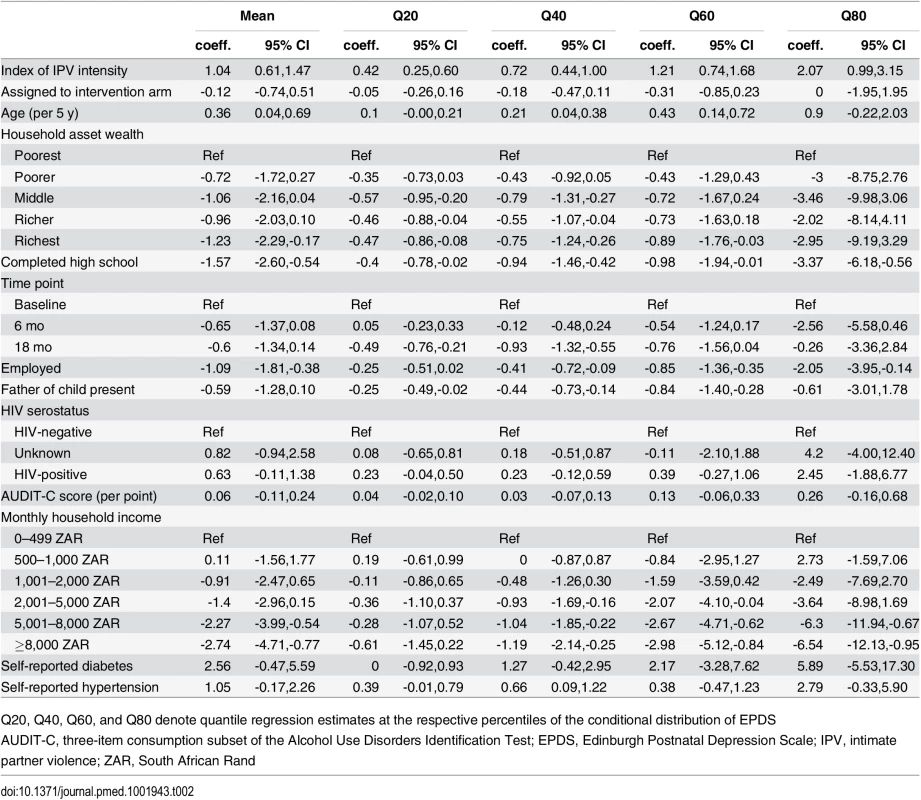
Q20, Q40, Q60, and Q80 denote quantile regression estimates at the respective percentiles of the conditional distribution of EPDS In terms of the magnitude of the association, when evaluated at the mean of the covariates, a one-standard deviation increase in IPV intensity was associated with a subsequent 13% relative increase in depressed mood. In multivariable logistic regression, lagged IPV intensity had a statistically significant association with probable depression (adjusted odds ratio [AOR], 1.26; 95% CI, 1.13–1.40). Evaluated at the mean of the covariates, a one–standard-deviation increase in IPV intensity was associated with a 4.0 percentage-point increase in probable depression (a 4.0/39.5 = 10.1% difference relative to the baseline prevalence). When the omnibus IPV exposure variable was replaced with the four IPV exposures as separate covariates, three of the four variables (having been slapped, shoved, or punched) had statistically significant associations with depression symptom severity (all p < 0.001, with regression coefficients ranging from 1.85–2.66) (S1 Table). When all four IPV exposures were entered jointly into a multivariable regression model, only being shoved was statistically significant (b = 1.66; 95% CI, 0.61–2.72).
In the fixed effects specification adjusting for all time-invariant confounding, the estimated association between IPV and depression symptom severity remained statistically significant (b = 1.54; 95% CI, 1.13–1.96) (Table 3). In terms of the interpretation of the estimate, a one-standard deviation increase in the intensity of IPV from one time point to the next was associated with a 1.33 point increase in the EPDS over the same time period. Compared to the baseline mean, this value represents a 1.33/10.8 = 12.3% relative increase; compared to the baseline standard deviation, this value represents 1.33/7 = 0.19 standard deviation units. The fixed effects quantile regression estimates, also shown in Table 3, indicate that increases in IPV intensity were associated with the greatest increases in depression symptom severity at the upper end of the conditional depression distribution.
Tab. 3. Association between changes in depression symptom severity and changes in intensity of intimate partner violence. 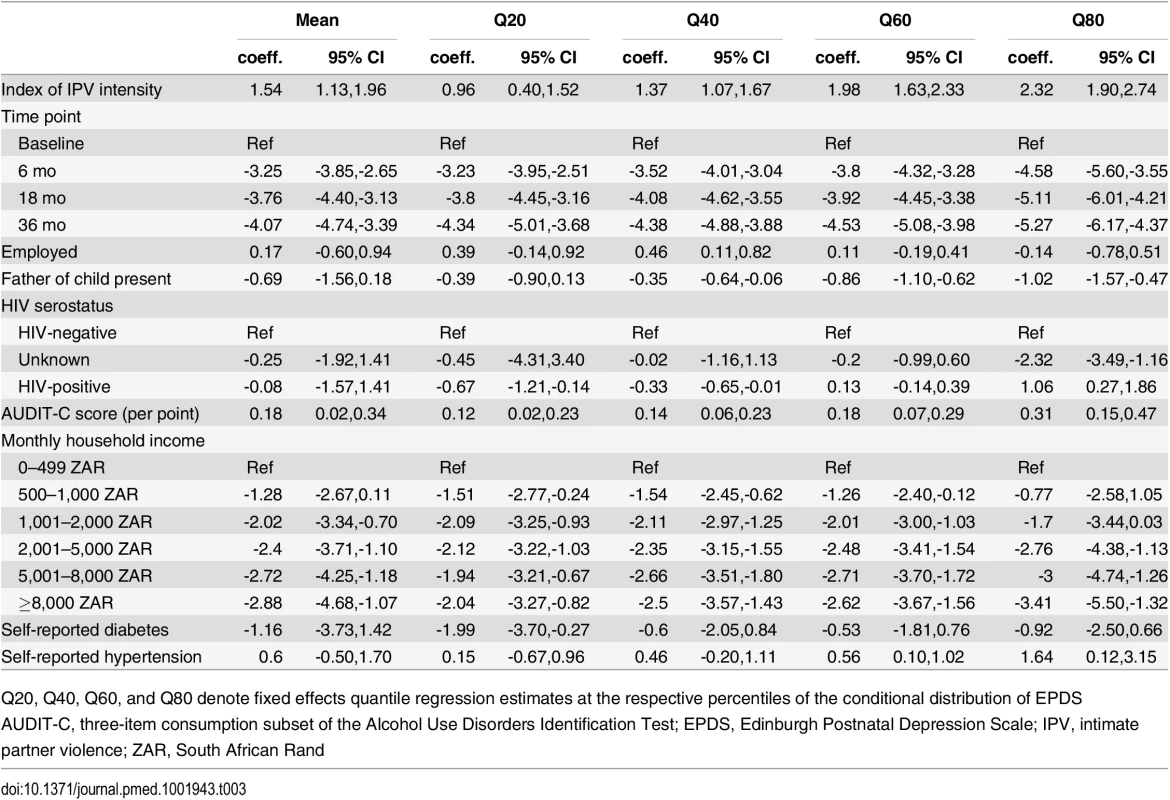
Q20, Q40, Q60, and Q80 denote fixed effects quantile regression estimates at the respective percentiles of the conditional distribution of EPDS When the ordering of the exposure and outcome were reversed, lagged depression symptom severity had a statistically significant association with IPV intensity. Each five-point difference in the EPDS score was associated with a 0.9–2.3 percentage point difference in subsequent IPV risk, depending on the specific outcome, with smaller marginal effects observed for more severe forms of IPV (Table 4). The pattern of smaller marginal effects observed for more severe forms of IPV is due to the lower baseline prevalences of the more severe forms of IPV. When expressed as relative odds, each five-point difference in the EPDS score was associated with AORs for the outcome ranging from 1.17–1.18 (being slapped or punched) to 1.29 (being attacked with a weapon). While the magnitudes of the coefficients cannot be directly compared, the magnitudes of the test statistics suggest that the strength of the association between IPV and subsequent depression is stronger than the strength of the association between depression and subsequent IPV.
Tab. 4. Association between lagged depression symptom severity and intimate partner violence. 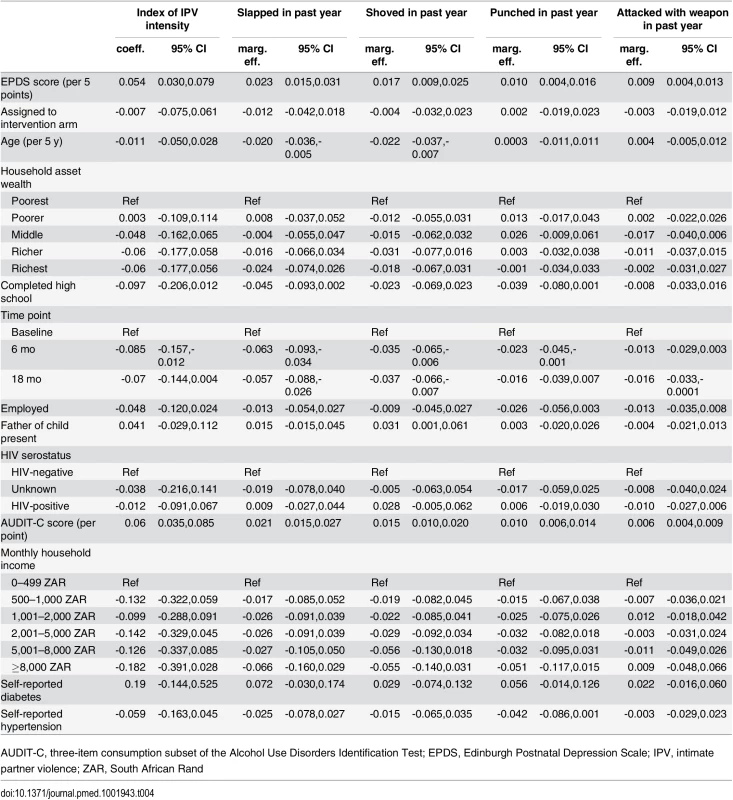
AUDIT-C, three-item consumption subset of the Alcohol Use Disorders Identification Test; EPDS, Edinburgh Postnatal Depression Scale; IPV, intimate partner violence; ZAR, South African Rand Discussion
In this secondary analysis of data from a population-based, 3-y cluster-randomized controlled trial of more than 1,200 women in peri-urban South Africa, we found that both IPV and depression were highly prevalent and that IPV intensity had a statistically significant association with depression symptom severity. The estimated association was relatively large in magnitude: the experience of IPV was associated with a difference in depression symptom severity that was comparable to the treatment effects observed in short-term randomized-controlled trials of psychotherapy interventions for peripartum depression [69,70]. Our findings are consistent with what has been shown in longitudinal studies conducted among women in high-income countries [23,67,71], plausible in light of what is generally known about the adverse psychological impacts of stressful life events and traumatic stressors [13–17], and robust to alternative specifications and potential confounding by time-invariant factors. Taken together, our findings have important policy and programmatic implications for women’s health in sub-Saharan Africa.
The association between IPV and poor mental health outcomes is generally accepted in the field [20,72], but most of the evidence is based on data from high-income countries. The evidence base from sub-Saharan Africa has lagged. The study in the literature most similar to ours is a study of 1,045 women in northeastern Brazil who were interviewed one time during pregnancy and one time postpartum [73]. In that study, Ludermir and colleagues [73] showed that IPV during pregnancy was associated with increased incidence of postpartum depression. Since the publication of the systematic review by Devries and colleagues [23], in which they identified no longitudinal studies of IPV and incident depression from sub-Saharan Africa, there has been one new study examining the relationship between sexual violence and mental-health–related outcomes among HIV-positive women in rural Uganda [28]. Several factors limit the generalizability of that study. Estimation was limited to HIV-positive women enrolled in a long-term HIV cohort. Given the myriad ways in which HIV stigma undermines treatment uptake [74–76], it is likely that theirs was a fairly unique population that had overcome substantial barriers to remain engaged in care [77,78]. (In contrast, in our sample, less than two-thirds of the HIV-positive women had re-engaged in HIV care following childbirth [68].) Furthermore, the findings of Tsai and colleagues [28] were based on a relatively small sample size and a relatively small number of exposure events. The analysis described in this manuscript is based on data collected from a large, population-based sample of women recruited from the community, thereby overcoming some of the limitations of their work.
Notably, we found that the association between IPV and depression was bi-directional: not only was IPV associated with greater subsequent depression symptom severity but also depression symptom severity was associated with a greater risk of subsequent IPV. Concerns about victim-blaming have hampered empirical research into understanding how individual characteristics of IPV survivors may be predictive of subsequent revictimization [79]. Our findings are consistent with prior conceptual and empirical work describing the role of psychological difficulties in maintaining abusive relationships [26,80,81]. Our findings are also consistent with longitudinal studies conducted with survivors of IPV showing that symptoms of post-traumatic stress are predictive of subsequent revictimization [82–84]. The data do not permit us to understand the mechanisms linking symptoms of depression to increased victimization risk. It is possible, for example, that depression may influence partner selection, reduce self-efficacy for leaving abusive relationships, or lead to distorted cognitions about risk, or some combination of the above. If IPV and depression are intertwined in a vicious cycle, with IPV increasing the risk of future depression and depression increasing the risk of future revictimization, these mutually reinforcing effects could potentially undermine the effectiveness of single-component interventions. It is possible that combined interventions, such as a broad-based package of services (e.g., case management, crisis services, legal aid, transitional housing, and childcare support) [85] plus cognitive-behavioral therapy [27] may be effective in interrupting the cycle of IPV and depression, but the effectiveness of such a multi-component approach is as of yet unknown.
In addition to bringing longitudinal, population-based data to bear on this issue, our analysis makes several unique contributions to this literature. First, the analysis is based on data from a highly vulnerable population: pregnant women living in one of the poorest communities in South Africa, where both the experience of violence and depression are extremely common. Second, our outcome measure has strong evidence of reliability, criterion-related validity, and construct validity in the local setting [39,43–47]. Third, given the richness of the data, our analysis permitted adjustment for potentially confounding factors (that could influence risks for both IPV and depressed mood) noted by Devries and colleagues [23] to have received less attention in the literature, including alcohol abuse [86,87]. Fourth, the fixed effects design accounts for potential confounding by time-invariant factors (that could also influence risks for both IPV and depression), such as personality structure [88] and childhood adversity [60,89,90]. And finally, our quantile regression and fixed effects quantile regression estimates indicate that the adverse impacts of IPV are greatest for women in the upper end of the conditional depression distribution.
Interpretation of our findings is subject to a number of assumptions and limitations. First, the fixed effects regression model relies on within-participant variation over time to estimate the quantities of interest and therefore could not estimate associations between time-invariant factors (e.g., educational attainment) and depression symptom severity. However, this is a small price to pay for the ability to gain greater traction on estimating the primary association of interest, i.e., between IPV and depression. Second, while Hill’s [91] criteria for causation require temporality, the exposure and outcome must be consistent with the known latency period. Most studies in the field have used a latency period of 3–6 mo for observing adverse changes in mental health in response to a stressor [92–94]. In our study, interviews were conducted at baseline, 6 mo, 18 mo, and 36 mo, suggesting an average latency period of 12 mo in the lagged-covariate and fixed-effects specifications. The extended latency period could have caused us to underestimate the strength of the association. However, in many studies in the literature on medical and psychosocial risk factors for depression, extended latency periods are not uncommon and may extend from 12 mo [95] to 2 y or even more [71,96]. Third, exposure assessment in this study was limited to different types of physical violence and, to a lesser extent, emotional violence. The home visiting intervention studied in the parent randomized controlled trial was designed to promote maternal and child health in a broad sense, and violence against women was one of many different aspects of wellness examined [30–35]. To minimize respondent burden, this study did not assess sexual violence or a more comprehensive range of emotional violence. However, these other aspects of IPV tend to co-occur as part of an overall phenotype of controlling behavior [1,67,90,97,98], suggesting a certain degree of collinearity. Therefore, while assessment of these violent behaviors should be incorporated into future studies of IPV (particularly because the adverse impacts of emotional violence on depression may be at least as severe as those resulting from physical and sexual violence [67,73,98,99]), we do not believe that failure to measure these other aspects of IPV would have biased our estimates away from the null. Fourth, outcomes were assessed using a screening instrument rather than structured diagnostic interviews. The EPDS is a reliable, sensitive, and valid instrument for assessing depression symptom severity [44], and its use in studies of partner violence and psychological distress is standard in the field [73]. The limitations of using screening instruments in this context are well known [100]. However, even sub-syndromal symptoms of depression that do not rise to the occasion of a formal diagnosis of major depressive disorder may entail significant psychosocial impairment and should therefore be pertinent to public health interest [101].
These limitations notwithstanding, our findings provide novel, population-based, longitudinal evidence from sub-Saharan Africa corroborating the link between IPV and negative mental health outcomes. The medical and psychological treatment of victimized women can likely be improved by attending to the underlying causes of their symptoms. Universal screening interventions (that seek to identify asymptomatic victimized women) have not proved successful in improving mental-health–or quality-of-life–related outcomes [102–104], but more intensive health sector responses should be explored. For example, screening combined with individually tailored psychosocial intervention has been shown to be effective in reducing health risks among pregnant and postpartum women [105,106]. Because the association between IPV and depression is likely reciprocal, psychosocial interventions may have important collateral impacts on reducing women’s susceptibility to violence [27]. Further research elucidating the conditions under which depression increases women’s susceptibility to IPV may yield additional targets for intervention. Because IPV is frequently embedded within an overall pattern of controlling behavior (“patriarchal terrorism” [107]) that can give rise to these bi-directional relationships, clinicians may need to modify their treatment plans if IPV is part of the complex network of causal influences on their patients’ depression. For women at risk of further victimization, judicious selection of an antidepressant medication without adverse cognitive effects should be considered to minimize the possibility of iatrogenically compromising their ability to respond to or avoid threatening situations or leave abusive relationships [12]. And post-discharge safety plans for women who have attempted suicide will need to involve collaboration with extended social ties (rather than return to family) if partner abuse is suspected as a causative factor. Outside of the health sector, structural interventions [108] that seek to modify the context of gender-unequal norms in which violence against women is overlooked, sustained, or encouraged [20] should also be explored as means of reducing IPV and improving women’s mental health [109–111].
Supporting Information
Zdroje
1. Garcia-Moreno C, Jansen HA, Ellsberg M, Heise L, Watts CH (2006) Prevalence of intimate partner violence: findings from the WHO multi-country study on women's health and domestic violence. Lancet 368 : 1260–1269. 17027732
2. Hung KJ, Scott J, Ricciotti HA, Johnson TR, Tsai AC (2012) Community-level and individual-level influences of intimate partner violence on birth spacing in sub-Saharan Africa. Obstet Gynecol 119 : 975–982. doi: 10.1097/AOG.0b013e31824fc9a0 22525908
3. Stockl H, Devries K, Rotstein A, Abrahams N, Campbell J, Watts C, et al. (2013) The global prevalence of intimate partner homicide: a systematic review. Lancet 382 : 859–865. doi: 10.1016/S0140-6736(13)61030-2 23791474
4. Devries KM, Mak JY, Garcia-Moreno C, Petzold M, Child JC, Falder G, et al. (2013) Global health. The global prevalence of intimate partner violence against women. Science 340 : 1527–1528. doi: 10.1126/science.1240937 23788730
5. Abrahams N, Devries K, Watts C, Pallitto C, Petzold M, Shamu S, et al. (2014) Worldwide prevalence of non-partner sexual violence: a systematic review. Lancet 383 : 1648–1654. doi: 10.1016/S0140-6736(13)62243-6 24529867
6. Jewkes R, Abrahams N (2002) The epidemiology of rape and sexual coercion in South Africa: an overview. Soc Sci Med 55 : 1231–1244. 12365533
7. Dunkle KL, Jewkes RK, Brown HC, Gray GE, McIntryre JA, Harlow SD (2004) Gender-based violence, relationship power, and risk of HIV infection in women attending antenatal clinics in South Africa. Lancet 363 : 1415–1421. 15121402
8. Jewkes RK, Dunkle K, Nduna M, Shai N (2010) Intimate partner violence, relationship power inequity, and incidence of HIV infection in young women in South Africa: a cohort study. Lancet 376 : 41–48. doi: 10.1016/S0140-6736(10)60548-X 20557928
9. Groves AK, Kagee A, Maman S, Moodley D, Rouse P (2012) Associations between intimate partner violence and emotional distress among pregnant women in Durban, South Africa. J Interpers Violence 27 : 1341–1356. doi: 10.1177/0886260511425247 22203635
10. Weaver TL, Clum GA (1995) Psychological distress associated with interpersonal violence: a meta-analysis. Clin Psychol Rev 15 : 115–140.
11. Golding JM (1999) Intimate partner violence as a risk factor for mental disorders: a meta-analysis. J Fam Viol 14 : 99–132.
12. Fischbach RL, Herbert B (1997) Domestic violence and mental health: correlates and conundrums within and across cultures. Soc Sci Med 45 : 1161–1176. 9381230
13. Kendler KS, Kessler RC, Walters EE, MacLean C, Neale MC, Heath AC, et al. (1995) Stressful life events, genetic liability, and onset of an episode of major depression in women. Am J Psychiatry 152 : 833–842. 7755111
14. Kendler KS, Karkowski LM, Prescott CA (1999) Causal relationship between stressful life events and the onset of major depression. Am J Psychiatry 156 : 837–841. 10360120
15. Kendler KS, Thornton LM, Prescott CA (2001) Gender differences in the rates of exposure to stressful life events and sensitivity to their depressogenic effects. Am J Psychiatry 158 : 587–593. 11282693
16. Hearst N, Newman TB, Hulley SB (1986) Delayed effects of the military draft on mortality. A randomized natural experiment. N Engl J Med 314 : 620–624. 3945247
17. Cesur R, Sabia JJ, Tekin E (2013) The psychological costs of war: military combat and mental health. J Health Econ 32 : 51–65. doi: 10.1016/j.jhealeco.2012.09.001 23220456
18. Steel Z, Chey T, Silove D, Marnane C, Bryant RA, van Ommeren M (2009) Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: a systematic review and meta-analysis. JAMA 302 : 537–549. doi: 10.1001/jama.2009.1132 19654388
19. Tsai AC, Subramanian SV (2012) Proximate context of gender-unequal norms and women's HIV risk in sub-Saharan Africa. AIDS 26 : 381–386. doi: 10.1097/QAD.0b013e32834e1ccb 22045344
20. Tsai AC (2013) Intimate partner violence and population mental health: why poverty and gender inequities matter. PLoS Med 10: e1001440. doi: 10.1371/journal.pmed.1001440 23667344
21. Jewkes R, Sikweyiya Y, Morrell R, Dunkle K (2011) Gender inequitable masculinity and sexual entitlement in rape perpetration South Africa: findings of a cross-sectional study. PLoS ONE 6: e29590. doi: 10.1371/journal.pone.0029590 22216324
22. Shannon K, Leiter K, Phaladze N, Hlanze Z, Tsai AC, Heisler M, et al. (2012) Gender inequity norms are associated with increased male-perpetrated rape and sexual risks for HIV infection in Botswana and Swaziland. PLoS ONE 7: e28739. doi: 10.1371/journal.pone.0028739 22247761
23. Devries K, Mak J, Bacchus LJ, Child JC, Falder G, Petzold M, et al. (2013) Intimate partner violence and incident depressive symptoms and suicide attempts: a systematic review of longitudinal studies. PLoS Med 10: e1001439. doi: 10.1371/journal.pmed.1001439 23671407
24. Foa EB, Cascardi M, Zoellner LA, Feeny NC (2000) Psychological and environmental factors associated with partner violence. Trauma Violence Abuse 1 : 67–91.
25. Stith SM, Smith DB, Penn CE, Ward DB, Tritt D (2004) Intimate partner physical abuse perpetration and victimization risk factors: a meta-analytic review. Aggr Viol Behav 10 : 65–98.
26. Barnett OW (2001) Why battered women do not leave, part 2: external inhibiting factors—social support and internal inhibiting factors. Trauma Violence Abuse 2 : 3–35.
27. Iverson KM, Gradus JL, Resick PA, Suvak MK, Smith KF, Monson CM (2011) Cognitive-behavioral therapy for PTSD and depression symptoms reduces risk for future intimate partner violence among interpersonal trauma survivors. J Consult Clin Psychol 79 : 193–202. doi: 10.1037/a0022512 21341889
28. Tsai AC, Wolfe WR, Kumbakumba E, Kawuma A, Hunt PW, Martin JN, et al. (in press) Prospective study of the mental health consequences of sexual violence among women living with HIV in rural Uganda. J Interpers Violence. Epub 13 Jan 2015. doi: 10.1177/0886260514567966
29. World Health Organization (2001) Putting women first: ethical and safety recommendations for research on domestic violence against women. Geneva: World Health Organization.
30. Rotheram-Borus MJ, le Roux IM, Tomlinson M, Mbewu N, Comulada WS, le Roux K, et al. (2011) Philani Plus (+): a Mentor Mother community health worker home visiting program to improve maternal and infants' outcomes. Prev Sci 12 : 372–388. doi: 10.1007/s11121-011-0238-1 21850488
31. le Roux IM, Tomlinson M, Harwood JM, O'Connor MJ, Worthman CM, Mbewu N, et al. (2013) Outcomes of home visits for pregnant township mothers and their infants in South Africa: a cluster randomised controlled trial. AIDS 27 : 1461–1471. doi: 10.1097/QAD.0b013e3283601b53 23435303
32. le Roux IM, Rotheram-Borus MJ, Stein J, Tomlinson M (2014) The impact of paraprofessional home visitors on infants' growth and health at 18 months. Vulnerable Child Youth Stud 9 : 291–304. 25342956
33. Rotheram-Borus MJ, Tomlinson M, Roux IL, Stein JA (2015) Alcohol use, partner violence, and depression: a cluster randomized controlled trial among urban South African mothers over 3 years. Am J Prev Med 49 : 715–725. doi: 10.1016/j.amepre.2015.05.004 26231855
34. Rotheram-Borus MJ, Tomlinson M, le Roux IM, Harwood JM, Comulada S, O'Connor MJ, et al. (2014) A cluster randomised controlled effectiveness trial evaluating perinatal home visiting among South African mothers/infants. PLoS ONE 9: e105934. doi: 10.1371/journal.pone.0105934 25340337
35. Tomlinson M, Rotheram-Borus MJ, Harwood J, le Roux IM, O'Connor M, Worthman C (2015) Community health workers can improve child growth of antenatally-depressed, South African mothers: a cluster randomized controlled trial. BMC Psychiatry 15 : 225. doi: 10.1186/s12888-015-0606-7 26400691
36. Austin SA, Mbewu N (2009) Philani program: a case study of an integrative approach of empowerment and social and economic development. Soc Work Public Health 24 : 148–160. doi: 10.1080/19371910802569724 19229780
37. le Roux IM, le Roux K, Comulada WS, Greco EM, Desmond KA, Mbewu N, et al. (2010) Home visits by neighborhood Mentor Mothers provide timely recovery from childhood malnutrition in South Africa: results from a randomized controlled trial. Nutr J 9 : 56. doi: 10.1186/1475-2891-9-56 21092178
38. le Roux IM, le Roux K, Mbeutu K, Comulada WS, Desmond KA, Rotheram-Borus MJ (2011) A randomized controlled trial of home visits by neighborhood mentor mothers to improve children's nutrition in South Africa. Vulnerable Child Youth Stud 6 : 91–102. 22299019
39. Hartley M, Tomlinson M, Greco E, Comulada WS, Stewart J, le Roux I, et al. (2011) Depressed mood in pregnancy: prevalence and correlates in two Cape Town peri-urban settlements. Reprod Health 8 : 9. doi: 10.1186/1742-4755-8-9 21535876
40. O'Connor MJ, Tomlinson M, Leroux IM, Stewart J, Greco E, Rotheram-Borus MJ (2011) Predictors of alcohol use prior to pregnancy recognition among township women in Cape Town, South Africa. Soc Sci Med 72 : 83–90. doi: 10.1016/j.socscimed.2010.09.049 21084142
41. Tomlinson M, O'Connor MJ, le Roux IM, Stewart J, Mbewu N, Harwood J, et al. (2014) Multiple risk factors during pregnancy in South Africa: the need for a horizontal approach to perinatal care. Prev Sci 15 : 277–282. doi: 10.1007/s11121-013-0376-8 23475562
42. Cox JL, Holden JM, Sagovsky R (1987) Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry 150 : 782–786. 3651732
43. De Bruin GP, Swartz L, Tomlinson M, Cooper PJ, Molteno C (2004) The factor structure of the Edinburgh Postnatal Depression scale in a South African peri-urban settlement. S Afr J Psychol 34 : 113–121.
44. Tsai AC, Scott JA, Hung KJ, Zhu JQ, Matthews LT, Psaros C, et al. (2013) Reliability and validity of instruments for assessing perinatal depression in African settings: systematic review and meta-analysis. PLoS ONE 8: e82521. doi: 10.1371/journal.pone.0082521 24340036
45. Tsai AC, Tomlinson M, Dewing S, le Roux IM, Harwood JM, Chopra M, et al. (2014) Antenatal depression case-finding by community health workers in South Africa: feasibility of a mobile phone application. Arch Womens Ment Health 17 : 423–431. doi: 10.1007/s00737-014-0426-7 24682529
46. Hung KJ, Tomlinson M, le Roux IM, Dewing S, Chopra M, Tsai AC (2014) Community-based prenatal screening for postpartum depression in a South African township. Int J Gynaecol Obstet 126 : 74–77. doi: 10.1016/j.ijgo.2014.01.011 24786139
47. Dewing S, Tomlinson M, le Roux IM, Chopra M, Tsai AC (2013) Food insecurity and its association with co-occurring postnatal depression, hazardous drinking, and suicidality among women in peri-urban South Africa. J Affect Disord 150 : 460–465. doi: 10.1016/j.jad.2013.04.040 23707034
48. Straus MA (1979) Measuring intrafamily conflict and violence: the conflict tactics (CT) scales. J Marriage Fam 41 : 75–88.
49. Kling JR, Liebman JB, Katz LF (2007) Experimental analysis of neighborhood effects. Econometrica 75 : 83–119.
50. Filmer D, Pritchett LH (2001) Estimating wealth effects without expenditure data—or tears: an application to educational enrollments in states of India. Demography 38 : 115–132. 11227840
51. Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M (1993) Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption—II. Addiction 88 : 791–804. 8329970
52. Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA (1998) The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med 158 : 1789–1795. 9738608
53. Bradley KA, Bush KR, Epler AJ, Dobie DJ, Davis TM, Sporleder JL, et al. (2003) Two brief alcohol-screening tests From the Alcohol Use Disorders Identification Test (AUDIT): validation in a female Veterans Affairs patient population. Arch Intern Med 163 : 821–829. 12695273
54. Froot KA (1989) Consistent covariance matrix estimation with cross-sectional dependence and heteroskedasticity in financial data. J Fin Quant Analysis 24 : 333–355.
55. Rogers WH (1993) Regression standard errors in clustered samples. Stata Tech Bull 13 : 19–23.
56. Williams RL (2000) A note on robust variance estimation for cluster-correlated data. Biometrics 56 : 645–646. 10877330
57. Koenker R, Hallock KF (2001) Quantile regression. J Econ Perspect 15 : 143–156.
58. Parente PMDC, Santos Silva JMC (in press) Quantile regression with clustered data. J Econometric Meth. Epub 27 Feb 2015. doi: 10.1515/jem-2014-0011
59. Rutter M, Quinton D (1977) Psychiatric disorder: ecological factors and concepts of causation. In: McGurk H, editor. Ecological factors in human development. Amsterdam: North-Holland Publishing Co. pp. 173–187.
60. Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. (1998) Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med 14 : 245–258. 9635069
61. Mundlak Y (1961) Empirical production function free of management bias. J Farm Econ 43 : 44–56.
62. Canay IA (2011) A simple approach to quantile regression for panel data. Economet J 14 : 368–386.
63. Rochat TJ, Richter LM, Doll HA, Buthelezi NP, Tomkins A, Stein A (2006) Depression among pregnant rural South African women undergoing HIV testing. JAMA 295 : 1376–1378. 16551708
64. Honikman S, van Heyningen T, Field S, Baron E, Tomlinson M (2012) Stepped care for maternal mental health: a case study of the Perinatal Mental Health Project in South Africa. PLoS Med 9: e1001222. doi: 10.1371/journal.pmed.1001222 22666181
65. Rochat TJ, Tomlinson M, Newell ML, Stein A (2013) Detection of antenatal depression in rural HIV-affected populations with short and ultrashort versions of the Edinburgh Postnatal Depression Scale (EPDS). Arch Womens Ment Health 16 : 401–410. doi: 10.1007/s00737-013-0353-z 23615932
66. Bartus T (2005) Estimation of marginal effects using margeff. Stata J 5 : 309–329.
67. Tsai AC, Weiser SD, Dilworth SE, Shumway M, Riley ED (2015) Violent victimization, mental health, and service utilization outcomes in a cohort of homeless and unstably housed women living with or at risk of becoming infected with HIV. Am J Epidemiol 181 : 817–826. doi: 10.1093/aje/kwu350 25834138
68. Rotheram-Borus MJ, Tomlinson M, Scheffler A, le Roux IM (2015) Re-engagement in HIV care among mothers living with HIV in South Africa over 36 months postbirth. AIDS 29 : 2361–2362. doi: 10.1097/QAD.0000000000000837 26258526
69. Spinelli MG, Endicott J (2003) Controlled clinical trial of interpersonal psychotherapy versus parenting education program for depressed pregnant women. Am J Psychiatry 160 : 555–562. 12611838
70. Mulcahy R, Reay RE, Wilkinson RB, Owen C (2010) A randomised control trial for the effectiveness of group Interpersonal Psychotherapy for postnatal depression. Arch Womens Ment Health 13 : 125–139. doi: 10.1007/s00737-009-0101-6 19697094
71. Rees S, Steel Z, Creamer M, Teesson M, Bryant R, McFarlane AC, et al. (2014) Onset of common mental disorders and suicidal behavior following women's first exposure to gender based violence: a retrospective, population-based study. BMC Psychiatry 14 : 312. doi: 10.1186/s12888-014-0312-x 25403750
72. Ellsberg M, Jansen HA, Heise L, Watts CH, Garcia-Moreno C (2008) Intimate partner violence and women's physical and mental health in the WHO multi-country study on women's health and domestic violence: an observational study. Lancet 371 : 1165–1172. doi: 10.1016/S0140-6736(08)60522-X 18395577
73. Ludermir AB, Lewis G, Valongueiro SA, Barreto de Araújo TV, Araya R (2010) Violence against women by their intimate partner during pregnancy and postnatal depression: a prospective cohort study. Lancet 376 : 903–910. doi: 10.1016/S0140-6736(10)60887-2 20822809
74. Sayles JN, Wong MD, Kinsler JJ, Martins D, Cunningham WE (2009) The association of stigma with self-reported access to medical care and antiretroviral therapy adherence in persons living with HIV/AIDS. J Gen Intern Med 24 : 1101–1108. doi: 10.1007/s11606-009-1068-8 19653047
75. Govindasamy D, Ford N, Kranzer K (2012) Risk factors, barriers and facilitators for linkage to antiretroviral therapy care: a systematic review. AIDS 26 : 2059–2067. doi: 10.1097/QAD.0b013e3283578b9b 22781227
76. Katz IT, Ryu AE, Onuegbu AG, Psaros C, Weiser SD, Bangsberg DR, et al. (2013) Impact of HIV-related stigma on treatment adherence: systematic review and meta-synthesis. J Int AIDS Soc 16 : 18640. doi: 10.7448/IAS.16.3.18640 24242258
77. Ware NC, Idoko J, Kaaya S, Biraro IA, Wyatt MA, Agbaji O, et al. (2009) Explaining adherence success in sub-Saharan Africa: an ethnographic study. PLoS Med 6: e11. doi: 10.1371/journal.pmed.1000011 19175285
78. Lankowski AJ, Siedner MJ, Bangsberg DR, Tsai AC (2014) Impact of geographic and transportation-related barriers on HIV outcomes in sub-Saharan Africa: a systematic review. AIDS Behav 18 : 1199–1223. doi: 10.1007/s10461-014-0729-8 24563115
79. Cattaneo LB, Goodman LA (2005) Risk factors for reabuse in intimate partner violence: a cross-disciplinary critical review. Trauma Violence Abuse 6 : 141–175. 15753198
80. Rusbult CE, Martz JM (1995) Remaining in an abusive relationship: an investment model analysis of non-voluntary dependence. Pers Soc Psychol B 21 : 558–571.
81. Strube MJ (1988) The decision to leave an abusive relationship: empirical evidence and theoretical issues. Psychol Bull 104 : 236–250. 3054996
82. Bell ME, Cattaneo LB, Goodman LA, Dutton MA (2008) Assessing the risk of future psychological abuse: predicting accuracy of battered women's predictions. J Fam Viol 23 : 69–80.
83. Perez S, Johnson DM (2008) PTSD compromises battered women's future safety. J Interpers Violence 23 : 635–651. doi: 10.1177/0886260507313528 18272729
84. Krause ED, Kaltman S, Goodman L, Dutton MA (2006) Role of distinct PTSD symptoms in intimate partner reabuse: a prospective study. J Trauma Stress 19 : 507–516. 16929505
85. Spangaro J, Zwi AB, Poulos R (2009) The elusive search for definitive evidence on routine screening for intimate partner violence. Trauma Violence Abuse 10 : 55–68. doi: 10.1177/1524838008327261 19056688
86. Klostermann KC, Fals-Stewart W (2006) Intimate partner violence and alcohol use: exploring the role of drinking in partner violence and its implications for intervention. Aggress Violent Behav 11 : 587–597.
87. Fergusson DM, Boden JM, Horwood LJ (2009) Tests of causal links between alcohol abuse or dependence and major depression. Arch Gen Psychiatry 66 : 260–266. doi: 10.1001/archgenpsychiatry.2008.543 19255375
88. Krueger RF, Caspi A, Moffitt TE (2000) Epidemiological personology: the unifying role of personality in population-based research on problem behaviors. J Pers 68 : 967–998. 11130741
89. Heyman RE, Slep AMS (2002) Do child abuse and interparental violence lead to adulthood family violence? J Marriage Fam 64 : 864–870.
90. Dunkle KL, Jewkes RK, Brown HC, Yoshihama M, Gray GE, McIntyre JA, et al. (2004) Prevalence and patterns of gender-based violence and revictimization among women attending antenatal clinics in Soweto, South Africa. Am J Epidemiol 160 : 230–239. 15257996
91. Hill AB (1965) The environment and disease: association or causation? Proc R Soc Med 58 : 295–300. 14283879
92. Hammen C (2005) Stress and depression. Annu Rev Clin Psychol 1 : 293–319. 17716090
93. Tsai AC, Bangsberg DR, Frongillo EA, Hunt PW, Muzoora C, Martin JN, et al. (2012) Food insecurity, depression and the modifying role of social support among people living with HIV/AIDS in rural Uganda. Soc Sci Med 74 : 2012–2019. doi: 10.1016/j.socscimed.2012.02.033 22513248
94. Palar K, Kushel M, Frongillo EA, Riley ED, Grede N, Bangsberg D, et al. (2015) Food insecurity is longitudinally associated with depressive symptoms among homeless and marginally-housed individuals living with HIV. AIDS Behav 19 : 1527–1534. doi: 10.1007/s10461-014-0922-9 25351185
95. Heflin CM, Siefert K, Williams DR (2005) Food insufficiency and women's mental health: findings from a 3-year panel of welfare recipients. Soc Sci Med 61 : 1971–1982. 15927331
96. Polsky D, Doshi JA, Marcus S, Oslin D, Rothbard A, Thomas N, et al. (2005) Long-term risk for depressive symptoms after a medical diagnosis. Arch Intern Med 165 : 1260–1266. 15956005
97. Stets JE (1990) Verbal and physical aggression in marriage. J Marriage Fam 52 : 501–514.
98. Coker AL, Davis KE, Arias I, Desai S, Sanderson M, Brandt HM, et al. (2002) Physical and mental health effects of intimate partner violence for men and women. Am J Prev Med 23 : 260–268. 12406480
99. Crowell NA, Burgess AW (1996) Understanding violence against women. Washington, D.C.: National Academy Press.
100. Kagee A, Tsai AC, Lund C, Tomlinson M (2013) Screening for common mental disorders: reasons for caution and a way forward. Int Health 5 : 11–14. doi: 10.1093/inthealth/ihs004 23580905
101. Judd LL, Akiskal HS, Maser JD, Zeller PJ, Endicott J, Coryell W, et al. (1998) A prospective 12-year study of subsyndromal and syndromal depressive symptoms in unipolar major depressive disorders. Arch Gen Psychiatry 55 : 694–700. 9707379
102. MacMillan HL, Wathen CN, Jamieson E, Boyle MH, Shannon HS, Ford-Gilboe M, et al. (2009) Screening for intimate partner violence in health care settings: a randomized trial. JAMA 302 : 493–501. doi: 10.1001/jama.2009.1089 19654384
103. Klevens J, Kee R, Trick W, Garcia D, Angulo FR, Jones R, et al. (2012) Effect of screening for partner violence on women's quality of life: a randomized controlled trial. JAMA 308 : 681–689. doi: 10.1001/jama.2012.6434 22893165
104. Hegarty K, O'Doherty L, Taft A, Chondros P, Brown S, Valpied J, et al. (2013) Screening and counselling in the primary care setting for women who have experienced intimate partner violence (WEAVE): a cluster randomised controlled trial. Lancet 382 : 249–258. doi: 10.1016/S0140-6736(13)60052-5 23598181
105. El-Mohandes AA, Kiely M, Joseph JG, Subramanian S, Johnson AA, Blake SM, et al. (2008) An intervention to improve postpartum outcomes in African-American mothers: a randomized controlled trial. Obstet Gynecol 112 : 611–620. doi: 10.1097/AOG.0b013e3181834b10 18757660
106. Kiely M, El-Mohandes AA, El-Khorazaty MN, Blake SM, Gantz MG (2010) An integrated intervention to reduce intimate partner violence in pregnancy: a randomized controlled trial. Obstet Gynecol 115 : 273–283. doi: 10.1097/AOG.0b013e3181cbd482 20093899
107. Johnson MP (1995) Patriarchal terrorism and common couple violence: two forms of violence against women. J Marriage Fam 57 : 283–294.
108. Tsai AC (2012) A typology of structural approaches to HIV prevention: a commentary on Roberts and Matthews. Soc Sci Med 75 : 1562–1567; discussion 1568–1571. doi: 10.1016/j.socscimed.2012.06.033 22877933
109. Pronyk PM, Hargreaves JR, Kim JC, Morison LA, Phetla G, Watts C, et al. (2006) Effect of a structural intervention for the prevention of intimate-partner violence and HIV in rural South Africa: a cluster randomised trial. Lancet 368 : 1973–1983. 17141704
110. Aizer A (2010) The gender wage gap and domestic violence. Am Econ Rev 100 : 1847–1859. 25110354
111. Green EP, Blattman C, Jamison J, Annan J (2015) Women's entrepreneurship and intimate partner violence: A cluster randomized trial of microenterprise assistance and partner participation in post-conflict Uganda. Soc Sci Med 133 : 177–188. doi: 10.1016/j.socscimed.2015.03.042 25875324
Štítky
Interné lekárstvo
Článek Sharing Clinical Trial Data: A Proposal from the International Committee of Medical Journal EditorsČlánek Data Sharing as Part of the Normal Scientific Process: A View from the Pharmaceutical Industry
Článok vyšiel v časopisePLOS Medicine
Najčítanejšie tento týždeň
2016 Číslo 1- Parazitičtí červi v terapii Crohnovy choroby a dalších zánětlivých autoimunitních onemocnění
- Intermitentní hladovění v prevenci a léčbě chorob
- Statinová intolerance
- Co dělat při intoleranci statinů?
- Monoklonální protilátky v léčbě hyperlipidemií
-
Všetky články tohto čísla
- Sharing Clinical Trial Data: A Proposal from the International Committee of Medical Journal Editors
- Pharmaceutical Industry Off-label Promotion and Self-regulation: A Document Analysis of Off-label Promotion Rulings by the United Kingdom Prescription Medicines Code of Practice Authority 2003–2012
- Can Data Sharing Become the Path of Least Resistance?
- Between Openness and Privacy in Genomics
- Developing Global Norms for Sharing Data and Results during Public Health Emergencies
- Advancing Medical Professionalism in US Military Detainee Treatment
- Resuscitating the Dying Autopsy
- Data Sharing as Part of the Normal Scientific Process: A View from the Pharmaceutical Industry
- Evidence for Community Transmission of Community-Associated but Not Health-Care-Associated Methicillin-Resistant Strains Linked to Social and Material Deprivation: Spatial Analysis of Cross-sectional Data
- Intimate Partner Violence and Depression Symptom Severity among South African Women during Pregnancy and Postpartum: Population-Based Prospective Cohort Study
- Intramuscular Artesunate for Severe Malaria in African Children: A Multicenter Randomized Controlled Trial
- Strategies to Prevent Cholera Introduction during International Personnel Deployments: A Computational Modeling Analysis Based on the 2010 Haiti Outbreak
- Preventing Weight Gain in Women in Rural Communities: A Cluster Randomised Controlled Trial
- Cotrimoxazole Prophylaxis Discontinuation among Antiretroviral-Treated HIV-1-Infected Adults in Kenya: A Randomized Non-inferiority Trial
- Sharing Individual Participant Data (IPD) within the Context of the Trial Reporting System (TRS)
- “Asymptomatic” Malaria: A Chronic and Debilitating Infection That Should Be Treated
- “Real-Time” Monitoring of Under-Five Mortality: A Vision Tempered by Reality
- “Real-Time” Monitoring of Under-Five Mortality: Lessons for Strengthened Vital Statistics Systems
- PLOS Medicine
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Cotrimoxazole Prophylaxis Discontinuation among Antiretroviral-Treated HIV-1-Infected Adults in Kenya: A Randomized Non-inferiority Trial
- Sharing Individual Participant Data (IPD) within the Context of the Trial Reporting System (TRS)
- Pharmaceutical Industry Off-label Promotion and Self-regulation: A Document Analysis of Off-label Promotion Rulings by the United Kingdom Prescription Medicines Code of Practice Authority 2003–2012
- Between Openness and Privacy in Genomics
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



