The reasons for reoperations after surgery for acute subdural hematoma and the implications of suspected injury mechanisms
Důvody reoperace po chirurgickém řešení akutních subdurálních hematomů a vztah k mechanismu poranění
Cíl studie: primárním cílem je analyzovat vztah mezi důvody reoperace po operaci akutního subdurálního hematomu a mechanizmem poranění a sekundárně vztah mezi akutním subdurálním hematomem primárně operovaným a oblastí reoperace.
Metody: u dospělých pacientů operovaných pro akutní subdurální hematom v období 2013 až 2017 byli pacienti reoperováni do 14 dnů. Byly studovány mechanizmy poranění, důvody opětovného otevření a lokalizace lézí.
Výsledky: z 86 pacientů operovaných pro akutní subdurální hematom bylo 24 pacientů reoperováno (27,9%). Hlavní indikací pro reoperaci po volných pádech jako příčiny zranění (12 pacientů) byl recidivující / významný reziduální subdurální hematom (7 pacientů) a kontralaterální subdurální hematom (3 případy). U komplikovaných (stupňovitých) pádů (dlouhé schodiště, 3 pacienti) byly důvody reoperace expanzivní intraparenchymální hematom nebo pohmoždění mozku. Při dopravních nehodách (4 pacienti, 3 chodci sražení auty) bylo důvodem reoperace pohmoždění mozku (dva případy), kontralaterální intracerebrální a subdurální hematom a pooperační epidurální hematom. Mechanizmus poranění nebyl znám u 5 pacientů. Ve 20,8% reoperací byla reoperovaná léze (hlavně subdurální hematom) kontralaterální k primárnímu subdurálnímu hematomu. Prognóza byla horší u reoperovaných pacientů.
Závěry: opakující se signifikantní reziduální subdurální hematomy jsou nejčastějšími důvody pro reoperaci po akutní operaci subdurálních hematomů. Důvody reoperace se vztahují k mechanizmu zranění. Prosté pády jsou spojovány hlavně s opakujícími se významnými zbytkovými nebo kontralaterálními subdurálními hematomy. Při komplikovaných pádech nebo dopravních nehodách (intenzivní poranění) převládají hemoragická poranění mozkového parenchymu.
Klíčová slova:
akutní subdurální hematom – reoperace – mechanizmus poranění mozku – zhmoždění mozku – kontralaterální subdurální hematom
Authors:
Krajsa Jan 1; Šilar Čeněk 2; Zeman Tomáš 2; Hrabovský Dušan 2; Chrastina Jan 2
Authors place of work:
Institute of Forensic Medicine, Faculty of Medicine, Masaryk University, Brno, Czech Republic
1; Department of Neurosurgery, St. Anne’s University Hospital, Faculty of Medicine, Masaryk University, Brno, Czech Republic
2
Published in the journal:
Soud Lék., 65, 2020, No. 4, p. 79-83
Category:
Original article
Summary
Study aim: The primary aim is to analyze the relationship between the reasons for reoperation after surgery for acute subdural hematoma and the injury mechanism and secondarily the relationship between the acute subdural hematoma primarily operated on and the area of reoperation.
Methods: Among adult patients operated on for acute subdural hematoma between 2013 and 2017, patients reoperated within 14 days were identified. Injury mechanisms, reasons for reoperation, and reoperated lesion location were studied.
Results: Of 86 patients operated on for acute subdural hematoma, 24 patients were reoperated (27.9%). The main indications for reoperation after uncomplicated falls as injury cause (12 patients) were recurrent/significant residual subdural hematoma (7 patients) and contralateral subdural hematoma (3 cases). In complicated falls (long staircase, 3 patients), the reasons for reoperation were expansive intraparenchymal hematoma or brain contusion. In traffic accidents (4 patients, 3 pedestrians hit by cars), the reason for reoperations was brain contusion (two cases), contralateral intracerebral and subdural hematoma and postoperative epidural hematoma. Injury mechanism was unknown in 5 patients. In 20.8% of reoperations, the reoperated lesion (mainly subdural hematoma) was contralateral to the primary subdural hematoma. Prognosis was worse in reoperated patients.
Conclusions: Recurrent/significant residual subdural hematomas are the most frequent reasons for reoperation after acute subdural hematoma surgery. The reasons for reoperations are related to the mechanism of injury. Simple falls are associated mainly with recurrent/significant residual or contralateral subdural hematomas. In complicated falls or traffic accidents (vigorous injuring force) hemorrhagic injuries of the brain parenchyma prevail.
Keywords:
Acute subdural hematoma – Reoperation – Brain injury mechanism – Brain contusion – Contralateral subdural hematoma
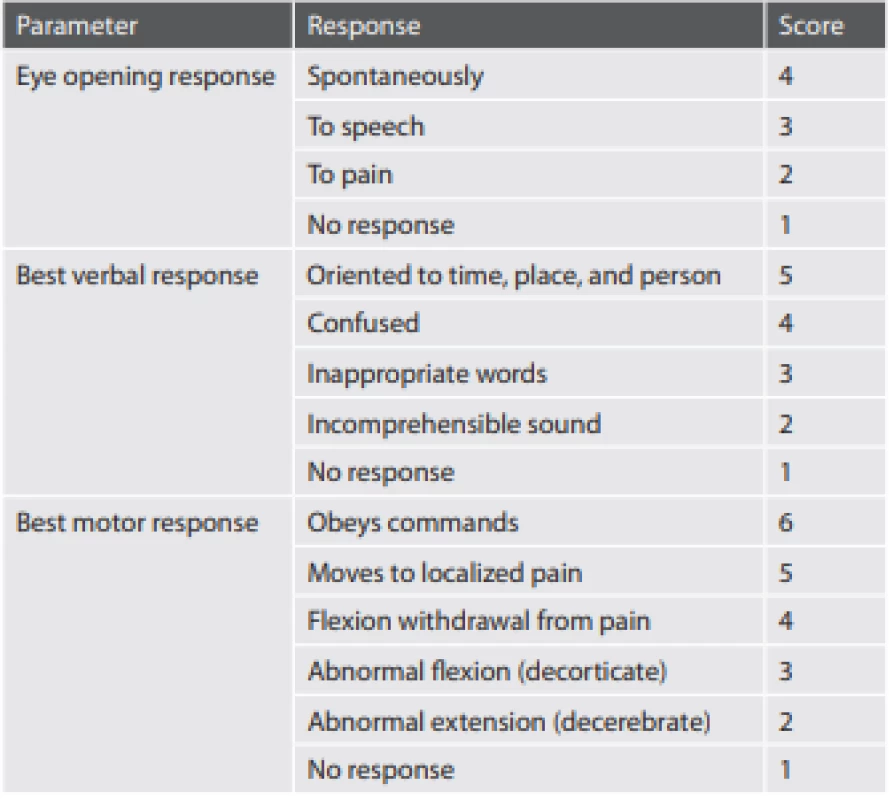
Acute subdural hematoma (aSDH) is found in approximately 11% of mild (Glasgow Coma Score 13–15) to moderate (Glasgow Coma Score 9–12) traumatic brain injuries (TBIs). In severe TBI (Glasgow Coma Score 3–8), the reported incidence is 20% to 33% of cases (1,2,3). Table 1 presents the parameters measured by the fundamental neurotraumatology Glasgow Coma Scale evaluating the injury severity.
The mortality of patients with aSDH is very high, reaching 67% of injured patients according to data published by Lenzi et al. (4). The factors responsible for the high mortality rate are the brain damage caused by cerebral compression from the aSDH and the injury to brain tissue caused by the primary trauma. The mechanism of the primary injury is important for the extent of brain tissue damage in patients with aSDH. aSDH as a dominant finding without significant brain tissue contusions is most frequently found in simple falls, impact injuries, or bikers trauma. According to autopsy findings described by Hartshorne et al. (5), aSDH was proven in 85% of fatal ground-level falls. In contrast, aSDH as well as diffuse axonal injury and multiple cerebral contusions with varying degrees of hemorrhagic transformation are present in fatalities after motor vehicle accidents and high-level falls (5,6). A delayed development or progression of hemorrhagic brain contusions after the primary trauma with an initially minimal or limited radiologically verified extent of brain parenchyma injury has also been described (7). Another significant cause of mortality in patients with aSDH is the fact that reoperation is needed in a high percentage of patients primarily operated on for aSDH. According to Desai et al. (8), reoperation was needed in 9.1% of patients after primary surgery for aSDH. The reasons for reoperation are recurrent or significant residual aSDH not removed during the primary surgery, but also the formation or progression of hemorrhagic cerebral contusions or intracerebral traumatic hematomas with expansive behavior. Lesions requiring reoperation may develop at the site of the primary aSDH operated on, but also distant from it and even contralateral to the site of the primary surgery (9,10,11).
The first aim of the study of patients primarily operated on for aSDH as the major finding is to analyze the relationship between the reoperated surgical lesion type and the mechanism of the primary injury. The second aim of the study is to analyze the traumatic changes affecting brain regions contralateral to or distant from the site of the primary aSDH operated on. Both problems are of utmost importance from a forensic point of view, both because of possible malpractice claims about the failure to recognize the real extent of brain injury during primary investigation and treatment and for the analysis of the location and direction of the injuring blunt force acting on the head provided by forensic medicine specialists. These data, presented by forensic medicine experts to prosecuting authorities or expert witnesses from the most diverse technical sciences (road traffic, biomechanics, etc.) are frequently of utmost importance for the correct evaluation of traffic accidents, work injuries, and violent crimes.
Materials and Methods
Patients with surgically treated aSDH were retrospectively identified from a group of adult patients (> 18 years) with craniocerebral injury who had been treated in the author’s department between 2013 and 2017. Patients were included in the study after the analysis of clinical data, postinjury, and follow-up CT scans and surgical reports proving that aSDH was the main surgical pathology. Patients who required reoperation within 14 days after the primary surgery were included in the study. In general, reoperation was undertaken in cases in which a radiological examination revealed a lesion (e.g. reaccumulation of aSDH, intracerebral hematoma, or expansive hemorrhagic contusion) with expansive behavior (e.g. focal brain compression, midline shift, or herniation signs) potentially treatable by surgery, and the neurological status was either failing to improve or deteriorating or the patient was unexaminable (e.g. due to sedation).
The following data were collected from the hospital information system
- injury mechanism
- time interval primary surgery – reoperation
- the type and location of the lesion indicated for reoperation.
For the purpose of the analysis of the relationship between injury mechanism and structural lesion requiring reoperation, the patients were divided into four groups according to injury mechanism:
- Simple, uncomplicated falls – not from heights, not down stairs; injury mechanism – head striking solid ground.
- Falls from heights, down longer staircases
- Traffic accidents (pedestrian or motor vehicle accidents)
- Unclear mechanisms of injury
The classification of the injury type was based on the available documentation of the emergency medical service, on data from the referring department, and, less frequently, on the report provided by the injured patient or trauma witnesses.
The time interval between primary surgery and reoperation was determined from the surgical reports available from the hospital information system.
The reason for reoperation and its relationship to the site of surgery for primary aSDH was defined after the analysis of CT scans performed before referral or during in-hospital stay (both available in the hospital PACS system) and surgical reports.
Regarding the type and location of the lesion indicated for reoperation: patients with a traumatic brain lesion requiring reoperation affecting the side contralateral to the primary aSDH or located in the distant intracranial compartment (e.g. primary surgery for supratentorial aSDH, reoperation for cerebellar hematoma) were identified.
The surgical outcomes at final follow-up visit in both reoperated and non-reoperated patients were evaluated using the standard Glasgow Outcome Scale (GOS: GOS 5 – Good outcome – resumption of normal life despite possible minor deficits; GOS 4 – Moderate disability – disabled but independent, can work in sheltered setting; GOS 3 – Severe disability – conscious, but disabled, dependent on others for daily support; GOS 2 – Persistent vegetative state – minimal responsiveness; GOS 1 – dead). Outcomes classified as GOS 4 or 5 were considered to be favorable (12).
Results
The studied group included 86 patients operated on for aSDH as the dominant surgical finding (males 60.5%). From this group, 24 patients had to be reoperated (27.9%), again with male predominance (62.5%). The average age of the reoperated patients was 66.7 years. The median of the interval between primary surgery and reoperation was 2 days (mean 4.13 days; SD 4.38 days). Fifteen reoperations were performed within the first 2 days after primary surgery, of which nine reoperations were performed during the first postsurgical day after the first postoperative CT either routinely planned (not later than 6 hours after primary surgery) or emergently performed in a deteriorating patient.
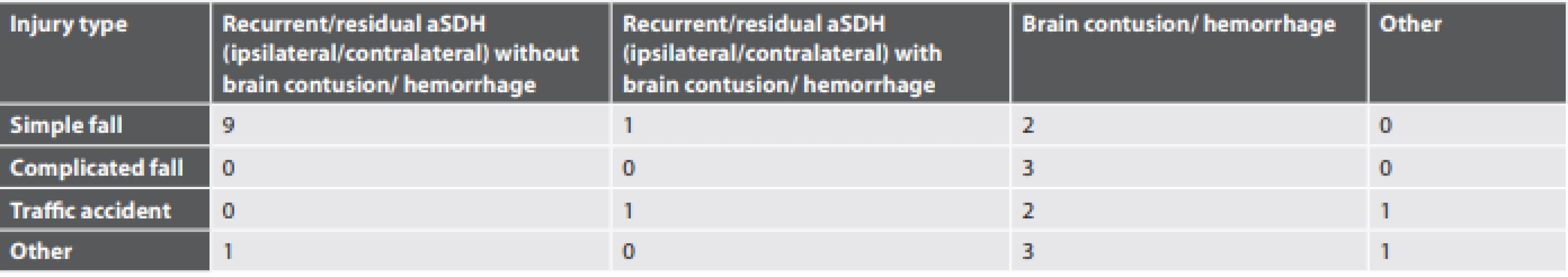
In 12 patients, the mechanism of injury was a simple, uncomplicated fall. In this group of patients, the prevailing reason for reoperation was recurrent or significant residual aSDH (7 patients – 58.3%). From this subgroup, in one patient significant contralateral aSDH had to be evacuated during the surgery for the recurrence of the aSDH primarily operated on; in another patient, progressing intracerebral hematoma in the primary surgical field had to be evacuated during the surgery for recurrent aSDH. From the remaining patients, the reason for reoperation was significant contralateral subdural hematoma in three, and reoperation was indicated because of progressive cerebral hemorrhagic contusion with expansive behavior and intracerebral hematoma without significant recurrent/significant residual aSDH in two patients.
Fall from a height (a longer staircase in all cases) was the cause of injury in three patients. In one patient, the reason for reoperation was a new intracerebral hematoma in the area of the aSDH primarily operated on; in two patients, the indications for reoperation were progressive foci of hemorrhagic contusions associated with massive brain edema and intracerebellar hematoma. Recurrent/ significant residual aSDH was not found in any of the patients.
Four patients were operated on for aSDH after traffic accidents (one motor vehicle driver, three pedestrians hit by a car). In two patients, the reason for reoperation was progressive hemorrhagic brain contusion with expansive behavior. One patient was reoperated for contralateral subdural and intracerebral hematoma. The last patient required reoperation due to postoperative epidural hematoma at the site of the primary craniotomy with less significant small hemorrhagic brain contusion. As in the previous group, there was no patient in whom the reason for reoperation was recurrent/ residual aSDH primarily operated on.
The group of five patients with unclear mechanism of injury requires further analysis. In three patients, the injury mechanism remains absolutely unclear even after retrospective detailed analysis of available data (found with left-sided hemiparesis, evaluated for multiple skin hematomas of different extent and age, found confused with superficial injury of the leg). In the remaining two cases, an uncomplicated fall could be considered as the potential cause of the injury, but the data were unclear. The indications for reoperations were expansive brain contusion with progressive edema, recurrence of the aSDH primarily operated on, progressive traumatic intracerebellar hematoma (the patients with completely unknown injury mechanism), epidural hematoma outside the primary craniotomy for aSDH (not contralateral), and progressive edema around brain contusion requiring decompressive craniectomy (falls suspected as the primary injury mechanism).
Simple uncomplicated falls were the most frequent cause of injury in reoperated patients primarily operated on for aSDH (63.2% of all patients with known injury mechanism and 50% of the entire group of patients), followed by traffic accidents (21.1% of all patients with known injury mechanism and 16.7% of the complete group) and complicated falls down long staircases (15.8% of all patients with known injury mechanism and 12.5% of the complete group).
The most frequent reasons for reoperation in patients after simple uncomplicated falls are recurrence or residuum of the primary aSDH operated on. In patients with complicated falls from heights (long staircases) or after traffic accidents (expected injuring force exceeding that of simple falls), expansive brain contusion or traumatic intracerebral hematomas largely prevails as the reason for reoperation. In contrast to the group of simple falls, there was no patient in whom the reason for reoperation was recurrent/ residual aSDH primarily operated on.
Table 2 provides the results summarizing the relationship between injury type and reason for reoperation, paying attention to the presence or absence of brain hemorrhagic contusion or traumatic intracerebral hematoma.
In the majority of reoperated patients, the lesion requiring surgery affected the area of the aSDH primarily operated on. Contralateral aSDH was observed in five patients (20.8%): isolated in three cases, in one case associated with significant intracerebral hematoma, and in one case with recurrent ipsilateral SDH. Regarding injury mechanisms, falls were expected in four cases, in the last case of contralateral aSDH with significant intracerebral hematoma fall was the most probable injury cause. Four of the five patients with contralateral subdural hematoma were older than 75 years. Evacuation of the primary aSDH was performed from osteoplastic craniotomy with bone flap replacement in three patients. Decompressive craniectomy (bone flap removal due to brain edema) was primarily performed in only one patient, and in one advanced age patient with high surgical risk the aSDH was reduced through smaller trephinations. In another two patients, follow-up CT scan after primary surgery for aSDH confirmed progressive cerebellar hemorrhagic contusion requiring surgical treatment (one after fall down a long staircase and one with unknown injury type).
The final treatment outcome was significantly worse in reoperated patients, as confirmed by the rates of favorable outcomes (GOS 4 or 5) in non-reoperated patients (41.2%) when compared with patients requiring reoperation (16.7%).
Discussion
Simple uncomplicated falls were the most frequent cause of injury in reoperated patients primarily operated on for aSDH (63.2% of all patients with known injury mechanism and 50% of the entire group of patients). This percentage of simple falls exceeds that reported by Hartshorne et al. (5), who studied a group of 75 fatal craniocerebral injuries. In contrast to our data, in this paper traffic accidents were the most frequent cause of the studied fatal craniocerebral injuries, with the incidence of accidental simple falls being 39%. In patients after uncomplicated falls, aSDH was the most frequently found type of intracranial bleeding (5). A simplified description of the situation during a simple fall adapted from the literature can be provided to explain the higher incidence of aSDH when compared with brain parenchyma injuries (hemorrhagic contusion or intracerebral hematoma) in this type of injury. Assuming a standard height of the head above ground level to be about 1.5 meters, from the mathematical formula v(head velocity) = (2gh)1/2 (g - gravity acceleration, h - height of the fall) the velocity of the head when it reaches the ground is between 5 and 6 m/sec. With the head weight about approximately 10 kg and the stiffness coefficient for the combination of the head and the impacting surface about 600 kN/m for a hard surface, the range of impact deceleration for the head striking surface is then between 1000 and 1800 m/s2. This deceleration is in the same range as the estimated threshold for the occurrence of observable brain parenchyma injury (1500 m/s2). Moreover the forces that produce aSDH are reported to have a high rate of deceleration onset and short duration, differing in these aspects from those that produce observable brain parenchyma injury. Other factors may contribute to the severity of the head injury, such as gait problems in elderly patients (stumbling or tripping with a slower response). These factors may add to the fall velocity and the rotational acceleration during the fall, therefore producing another component of the forces that act as the mechanism responsible for brain parenchyma injury. A similar situation may occur during falls down stairs (5,13,14).
This theoretical consideration was confirmed in our study by the type of lesions requiring reoperations in patient primarily operated on for aSDH as correlated with the injury mechanism. The most frequent reason for reoperation in patients after simple uncomplicated falls are recurrence or residuum of the primary aSDH operated on, followed by contralateral aSDH. Surgically significant hemorrhagic contusion or intraparenchymal hematoma requiring reoperation was found only in the minority of patients with simple falls. In patients with complicated falls (down long staircases in all our cases), the reason for reoperation was always traumatic injury of brain parenchyma (intracerebral hematoma or brain contusion). A similar situation was observed after traffic accidents (the patient reoperated for contralateral subdural hematoma also had a large intracerebral hematoma) with the exception of one patient in whom reoperation was indicated because of postoperative epidural hematoma with brain compression.
The dynamics of the extent of traumatic brain injury is studied by CT scans in the majority of cases. For the correlation between ante-mortem CT findings and autopsy data, there was a notable study by Panzer et al. (15). It is not surprising that the comparison between primary posttraumatic CT and the last follow-up CT before death proved extensive changes of the findings particularly in patients with severe traumatic brain injury requiring decompressive craniectomy. Based on high sensitivity (the rate of positive autopsy findings verified on CT), specificity (the rate of negative autopsy findings not verified on CT), and the resulting good correlation between radiological and autopsy findings, the authors suggest the inclusion of the clinically routine ante-mortem CT in the process of autopsy interpretation (15). On the other hand, it is important to underline the possible discrepancy between the extent of aSDH when comparing ante-mortem and postmortem CT (also on autopsy), as noted by Inokuchi et al. (16). The authors proved significant reduction of aSDH extent and midline shift regression when comparing ante-mortem and postmortem findings, stating that this discrepancy may elicit doubts about the cause of the death without knowing the details of the circumstances of the death (16). However the presence of brain parenchyma hemorrhagic lesions, particularly when reoperation is required, supports the possibility of high energy impact.
In the context of the problem of contralateral posttraumatic hematomas as reasons for reoperation, the data published by Nedugov (17) and Farkašová Iannaccone et al. (18) describing the possible redistribution of aSDH should be noted. According to these studies, aSDH can undergo any possible dislocation over the surface of large hemispheres of the brain as well as downward transtentorial and spinal migration. However their analysis gave no evidence of the possibility of the upward transtentorial redistribution of aSDH or subdural blood redistribution across the falx. This result reduces the validity of consideration of the simple contralateral redistribution of aSDH being the cause of contralateral aSDH requiring reoperation (17,18). In our group, contralateral aSDH were the reason for reoperation in 20.8% of all reoperated patients. Regarding the mechanism of formation of distant postoperative hematomas, probably the idea that they are caused by fast and sudden brain decompression leading to extensive shifts of brain tissue can be accepted. These shifts lead to the injury of the bridging veins entering the venous sinuses resulting in subdural hematomas. Moreover the extensive shifts of brain tissue caused by brain compression by the aSDH and also fast decompression after surgery may lead to the injury of blood vessels supplying brain parenchyma, with resulting intracerebral hematoma formation or the progression of hemorrhagic transformation of brain contusion. In our group, in one patient the contralateral aSDH was associated with extensive intracerebral hematoma. The possibility of sudden detamponade of already injured blood vessels after aSDH evacuation with subsequent bleeding should be considered. All these changes may also affect the contralateral brain hemisphere (11,19).
In the paper published by Flordelís Lasierre et al. (20), the development of contralateral aSDH or epidural hematoma was described in 9.2% in their group of 120 patients operated on for traumatic mass lesion. In contrast to our group, the reported predominance of contralateral acute epidural hematomas (63.6%) in their group is striking when compared to the zero rate of these findings in our group (20). This is probably because of the advanced age in our group. In general older people are more prone to developing aSDH rather than epidural hematoma, because of the stronger adherence of dura to the bone in elderly people. This assumption is also supported by the data reported by Su et al. (19) dealing with the clinical features and prognosis of contralateral epidural hematomas after aSDH evacuation. The average age of their patients was 39 years, with only one patient older than 60 years (19).
Conclusions
The paper proves the relationship between the reason for reoperation in patients operated on for aSDH and injury mechanism. In patients after simple uncomplicated ground level falls, the most frequent reason for reoperation was recurrent or residual aSDH primarily operated on. In patients after complicated falls or after traffic accidents, new or progressive traumatic intracerebral hematoma or hemorrhagic brain contusion were the most frequent reasons for reoperation. In 29.2% of reoperated patients, the offending lesion requiring reoperation was located contralaterally or in a different cranial compartment from the site of the aSDH primarily operated on.
Acknowledgements
Thanks to Anne Johnson for language correction and editorial assistance.
Funding source
None.
Conflict of Interest
The authors declare that they have no conflict of interest.
This article does not contain any studies with human participants or animals performed by any of the authors.
∗ Correspondence address:
Jan Chrastina, Associate Professor, M.D., Ph.D.
Department of Neurosurgery, Masaryk University Medical Faculty
St. Anne’s Hospital Brno
Pekařská 53, 656 91 Brno, Czech Republic
tel.: +420 543 182 697
e-mail: jan.chrastina@fnusa.cz
Received: January 21, 2020
Accepted: June 14, 2020.
Zdroje
- Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet 1974; 2: 81–84.
- Al-Mufti F, Mayer SA. Neurocritical Care of Acute Subdural Hemorrhage. Neurosurg Clin N Am 2017; 28: 267–278.
- Chen SH, Chen Y, Fang WK, Huang DW, Huang KC, Tseng SH. Comparison of craniotomy and decompressive craniectomy in severely head-injured patients with acute subdural hematoma. J Trauma 2011; 71: 1632–1636.
- Lenzi J, Caporlingua F, Caporlingua A, et al. Relevancy of positive trends in mortality and functional recovery after surgical treatment of acute subdural hematomas. Our 10-year experience. Br J Neurosurg 2017; 31: 78–83.
- Hartshorne NJ, Harruff RC, Alvord EC Jr. Fatal head injuries in ground-level falls. Am J Forensic Med Pathol 1997; 18 :258–264.
- Davceva N, Janevska V, Ilievski B, Petrushevska G, Popesca Z. The occurrence of acute subdural haematoma and diffuse axonal injury as two typical acceleration injuries. J Forensic Leg Med 2012; 19: 480–484.
- Servadei F, Nasi MT, Giuliani G, et al. CT prognostic factors in acute subdural haematomas: the value of the “worst” CT scan. Br J Neurosurg 2000; 14: 110–116.
- Desai VR, Grossman R, Sparrow H. Incidence of Intracranial Hemorrhage After a Cranial Operation. Cureus 2016; 8: e616.
- Fridley J, Thomas J, Kitagawa R, Chern J, Omeis I. Immediate development of a contralateral acute subdural hematoma following acute subdural hematoma evacuation. J Clin Neurosci 2011; 18: 422–423.
- Matsuno A, Katayama H, Wada H, et al. Significance of consecutive bilateral surgeries for patients with acute subdural haematoma who develop contralateral acute epi - or subdural haematoma. Surg Neurol 2003; 60: 23–30.
- Tomycz ND, Germanwala AV, Walter KA. Contralateral acute subdural haematoma after surgical evacuation of acute subdural hematoma. J Trauma 2010; 68: E11–E12.
- Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet 1975; 1: 480–484.
- Gennarelli TA, Thibault LE. Biomechanics of acute subdural hematoma. J Trauma 1982; 22: 680–686.
- Ryan GA, McLean AJ, Vilenius AT, et al. Brain injury patterns in fatally injured pedestrians. J Trauma 1994; 36: 469–476.
- Panzer S, Covaliov L, Augat P, Peschel O. Traumatic brain injury: Comparison between autopsy and ante-mortem CT. J Forensic Leg Med 2017; 52: 62–69.
- Inokuchi G, Yajima D, Hayakawa M, et al. Is acute subdural hematoma reduced during the agonal stage and postmortem? Int J Legal Med 2013; 127: 263–266.
- Nedugov GV. The possibility and mechanism of spontaneous redistribution of acute intracranial subdural hematomas. Sud Med Ekspert 2011; 54: 54–57.
- Farkašová Iannaccone S, Ginelliová A, Šantová I, et al. Redistribution of acute traumatic infratentorial subdural hematoma to the spinal subdural space. Soud Lek 2018; 63: 25–28.
- Su TM, Lee TH, Chen WF, Lee TC, Cheng CH. Contralateral acute epidural hematoma after decompressive surgery of acute subdural hematoma: clinical features and outcome. J Trauma 2008; 65: 1298–1302.
- Flordelís Lasierra JL, García Fuentes C, Toral Vázquez D, Chico Fernández M, Bermejo Aznáres S, Alted López E. Contralateral extraaxial hematomas after urgent neurosurgery of a mass lesion in patients with traumatic brain injury. Eur J Trauma Emerg Surg 2013; 39: 277–283.
Štítky
Patológia Súdne lekárstvo ToxikológiaČlánok vyšiel v časopise
Soudní lékařství

2020 Číslo 4
Najčítanejšie v tomto čísle
- Autoerotic deaths: report of two unusual cases
- Případ úpalu pod vlivem psychotropních látek
- The reasons for reoperations after surgery for acute subdural hematoma and the implications of suspected injury mechanisms
- MUDr. Jaromír Hrubecký osmdesátiletý
