Breast implant-associated anaplastic large-cell lymphoma – an evolution through the decades: citation analysis of the top fifty most cited articles
Authors:
Paul Austin Kallarackal 1; Igor Slaninka 2; Nancy Mrozková 3
Authors‘ workplace:
Faculty of Medicine in Hradec Králové, Charles University, Prague
1; Department of Plastic Surgery, Faculty Hospital Hradec Králové
2; Faculty of Pharmacy in Hradec Králové, Charles University, Prague
3
Published in:
ACTA CHIRURGIAE PLASTICAE, 63, 3, 2021, pp. 127-138
doi:
https://doi.org/10.48095/ccachp2021127
Introduction
Breast implant-associated anaplastic large cell lymphoma (BIA-ALCL) is a newly recognized neoplastic disease entity. As suggested by the nomenclature, this malignancy of T-cell type is strongly linked to the use of breast implants. Though first described in 1997 by Keech and Creech [1], it was only recently that BIA-ALCL has received wider recognition in the medical field. In 2011, it was recognized by FDA [2] and in 2016, it was included in the WHO classification of lymphoid malignancies [3]. The latest studies on etiopathogenesis theorize that textured implants promote the growth of bacteria on them and a subsequent formation of a biofilm, leading to chronic inflammation and malignant transformation.
Over the last decade, there has been increased awareness and improved diagnostics [4] with peri-implant fluid collection and classification of implant shell textures [5] leading to the detection and treatment of an increasing number of cases. As of today, there exists a large array of studies on BIA-ALCL focused on the topics as pathophysiology, diagnostics, oncologic management and reconstruction. Thus, there arises a need to identify the most important articles with a greater impact. In this study, we chose citation analysis as a tool to achieve the same. As observed in similar studies [6–8], this would allow us to appreciate the evolution of our knowledge and understanding of this disease.
Citation is the acknowledgment received by an article from another, later one. The number of times an article is cited can be a representation of its overall impact [9]. Citation analysis is a tool to study such relations between articles and may be used to identify the most cited studies, which would have the most impact. In this study, we sought to create a compilation of landmark, peer reviewed articles and to classify them according to the topics they focus on. We hope this article proves to be a useful resource for future plastic surgeons and to the industry involved in the manufacture of breast prostheses. Here we report on the 50 most cited articles pertaining to the field of BIA-ALCL.
Methods
Article selection
For the purpose of identifying the high impact articles, we searched the Web of Science Citation Index in November 2019. The search included all years until 2019 and all the databases available through Web of Science. Various combinations of key words such as: BIA-ALCL, breast implant-associated anaplastic large cell lymphoma, breast implant non-Hodgkin’s lymphoma, breast implant illness, anaplastic lymphoma and breast implant, were used to obtain several search results. All results were compared among each other by individually reviewing the resultant articles and “breast implant-associated anaplastic large cell lymphoma” was selected as the main search term. This initial search returned 325 articles. Following this, articles from the other reports which were focused on the field of BIA-ALCL were included in this study according to the number of citations they received. Subsequently the top 50 articles [1,10–58] (with the highest number of citations) were extracted from this compiled list of articles. Since literature reviews are not original articles, but still have a high citation rate, including them would have skewed the results and so they were excluded.
Data extraction
The articles sourced were subsequently analyzed based on their publishing journal, authorship, publication year, institution and country of origin, type of study (basic science or clinical research), level of evidence (LoE), and study topic. The articles were then classified and categorized according to the same.
Results
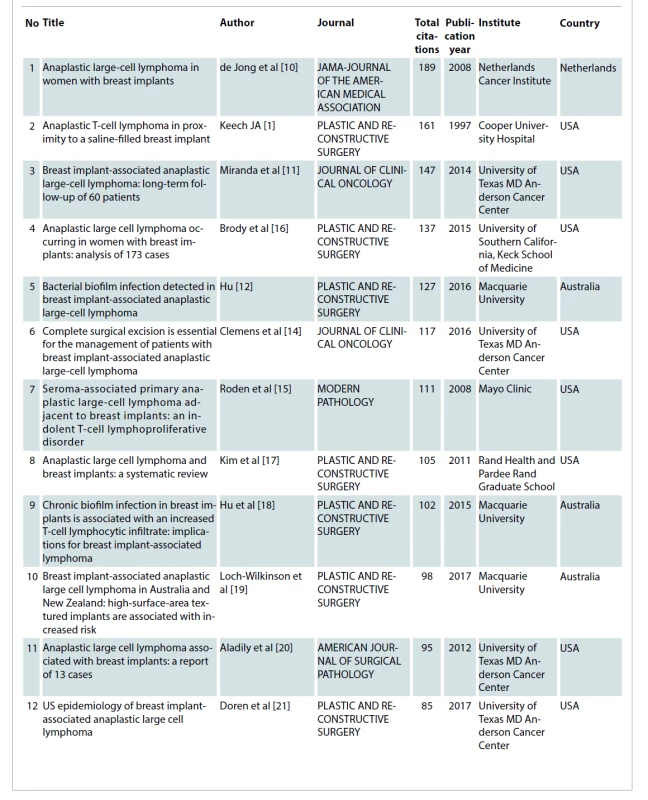
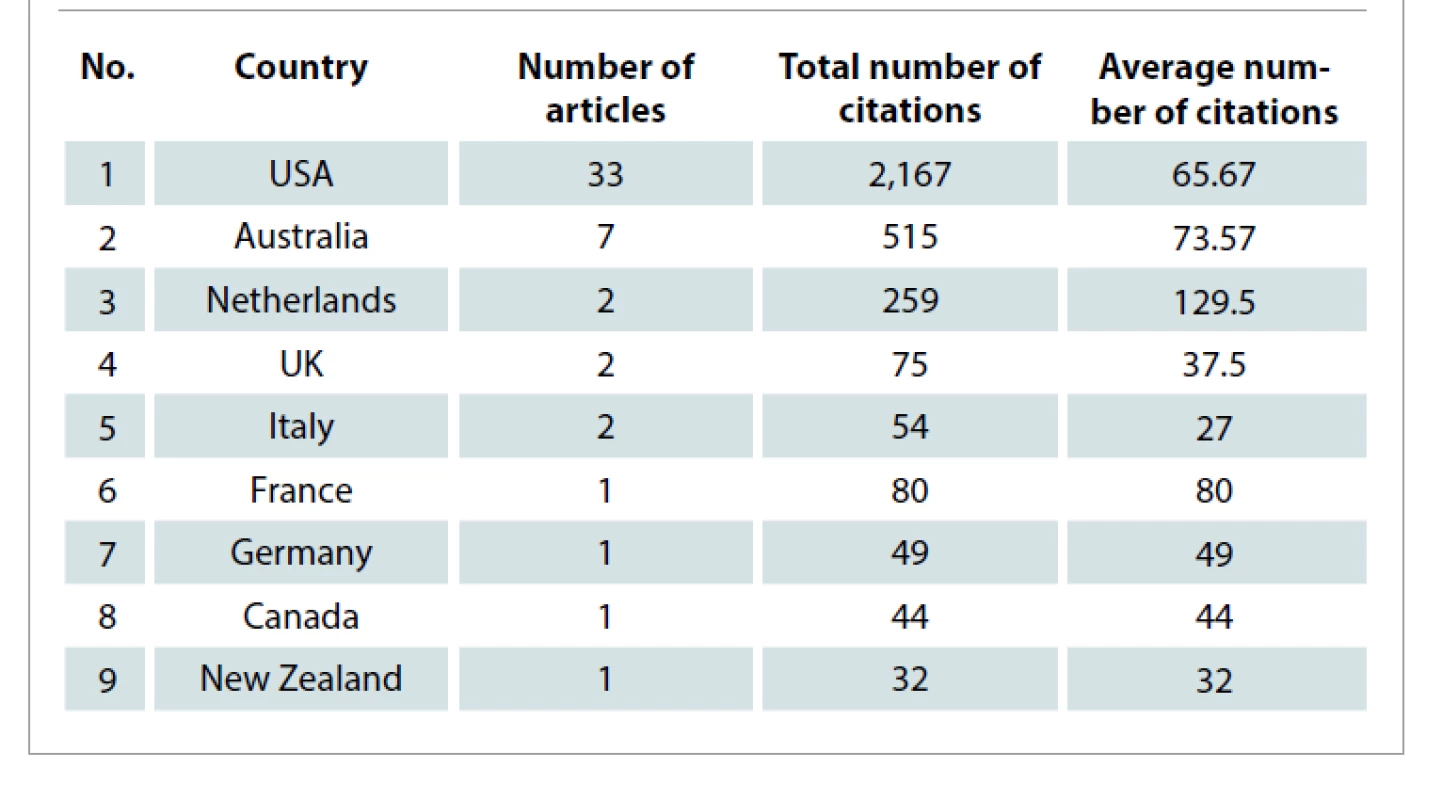
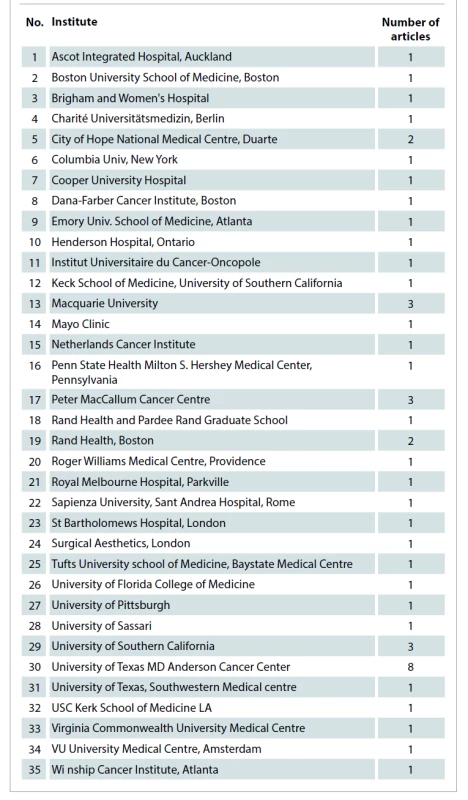
Following collection, the 50 most cited articles were included in this study. Tab. 1 illustrates these publications in the descending order of their number of citations. The earliest article considered for this study was from August 1997 and the latest was from January 2018. The highest number of publications were in 2016 and 2017 with seven articles each. This is highlighted in Graph 1 which shows the distribution of published articles across the years. The United States of America was found to have a significantly higher number of publications (N = 33) compared to the 8 other nations (Tab. 2). On the other hand, in terms of the average number of citations per article, the Netherlands leads by a wide margin. Among the institutes of the origin of these articles, University of Texas, MD Anderson Cancer Center had the highest number of publications (N = 8) followed by Peter MacCallum Cancer Centre and Macquarie University with 3 articles each (Tab. 3).

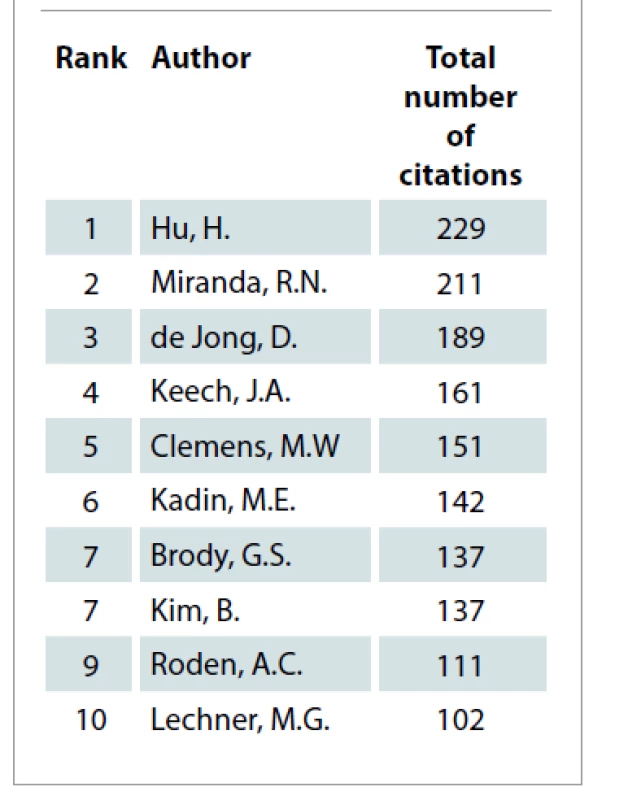
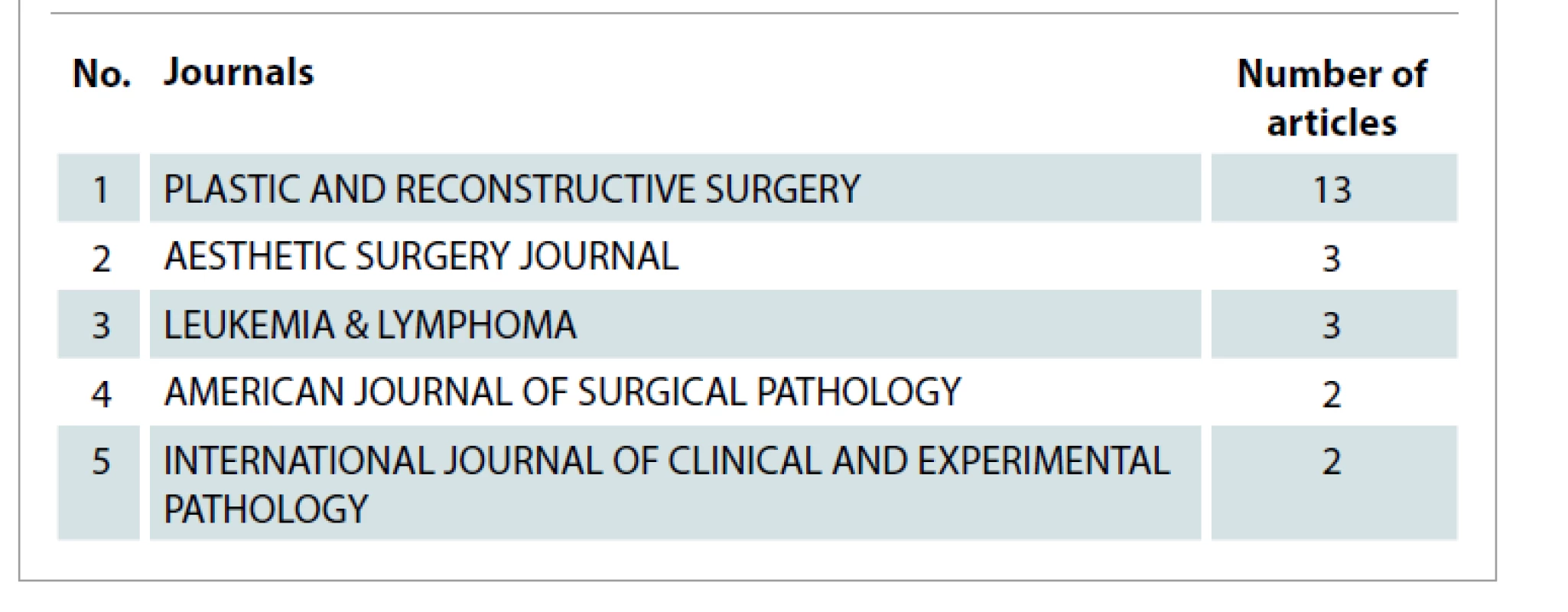
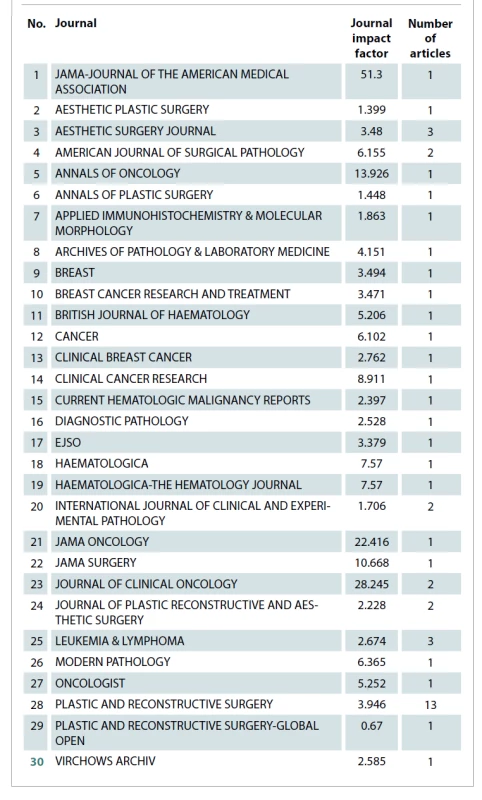
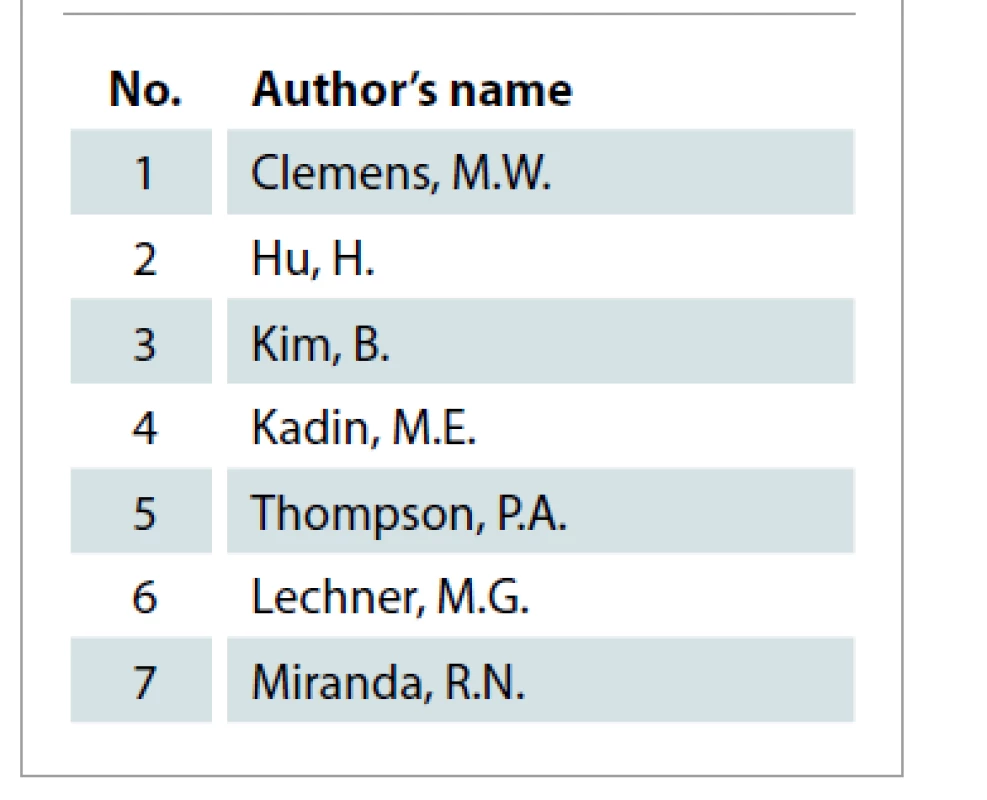
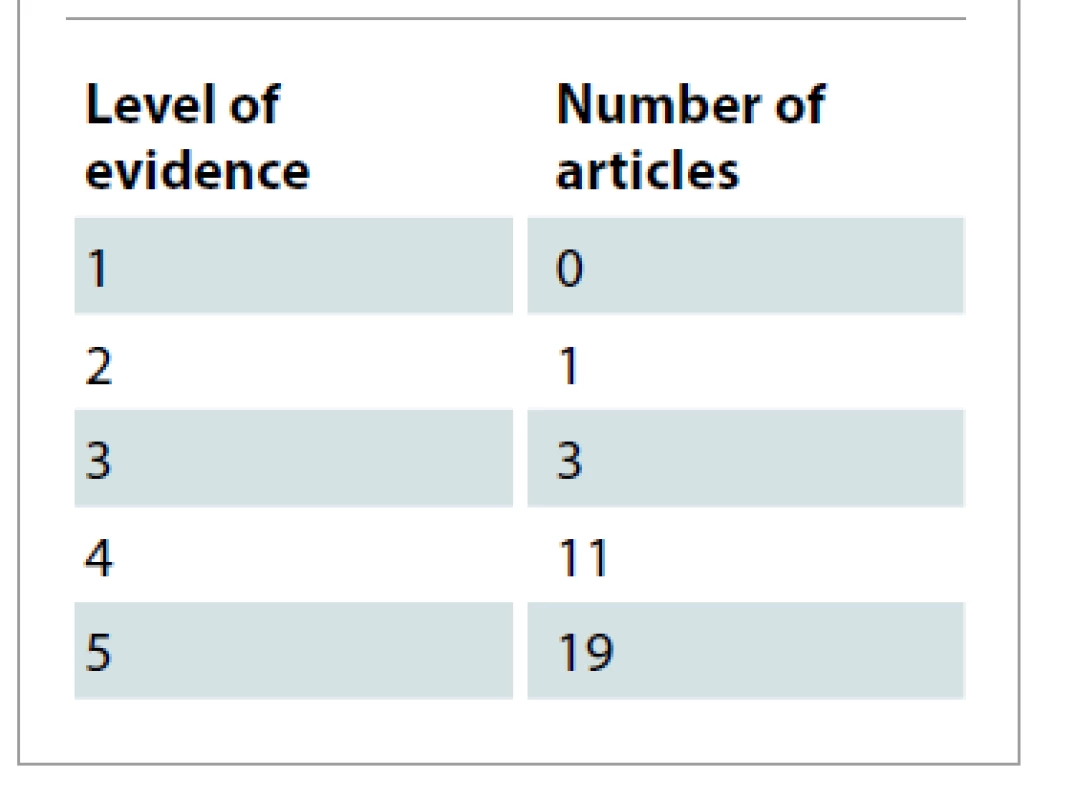
The collected articles were published across 30 journals. Tab. 4 displays these journals. Plastic and Reconstructive Surgery was a journal with the majority of publications (N = 13). Tab. 5 lists the authors with 2 articles among the 50 most cited. Tab. 6 show cases of the top 10 authors according to their total number of citations and among them H. Hu tops the list with 229 citations, followed by R. N. Miranda with 211 citations and D. de Jong with 189 citations. Among the included publications, 8 were basic science studies and the rest were clinical research studies. The articles were further classified based on their level of evidence in Tab. 7 according to the protocols developed by Oxford Centre for Evidence-Based Medicine [59,60]. Most of the articles in this study had LoE 5 (N = 19) and none were found to have LoE 1.
Discussion
Citation analysis has been performed on the literature of the various subspecialties of plastic surgery such as microsurgery [61,62], hand surgery [63], craniofacial surgery [64–67], breast surgery [7,68], cleft lip surgery [69,70] and lower extremity reconstruction [71], among others. However, to the best of our knowledge, this is the first time it has been carried out on the field of BIA-ALCL. Through this study, we hoped to create a compilation of important publications that have contributed to the evolution and development of this field. Although each article is worthy of discussion, here we briefly comment on the most cited articles and the high impact publications focused on the different areas of interest (pathophysiology, diagnostics, oncologic management, databases, case series and reports).
The article with the highest number of citations (189 citations) authored by D. de Jong in 2008 describes a study to determine the risk of ALCL associated with breast implants. Following the identification of 2 patients with ALK-negative ALCL close to implanted breast prostheses, the authors investigated the national database of Netherlands to identify 11 patients with similar findings. This study postulates three mechanisms of causation for this pathology, and concludes that though the risk is low, there is an association between silicone breast implants and ALCL [10].
Second on our list of highest impact articles is the pioneer report on BIA-ALCL by J. A. Keech a B. Creech, authored in 1997. This article details the follow-up care of a singular patient from November 1991 to 1996, who presented with a peri-implant lesion in late 1995. Prior to this report, there is no literature discussing this disease entity and there was only speculation regarding an association between breast implants and cutaneous lymphoma [1].
With 147 citations, the third article on the list was published in 2014 and was authored by R. N. Miranda from University of Texas MD Anderson Cancer Centre. The authors performed clinical follow up on 60 published cases of breast implant associated ALCL from 1997 to December 2012. They observed the overall survival as well as the oncological management of these patients. In conclusion, this study states that with capsulectomy and implant removal, most patients achieved complete remission [11].
Moving on to the specific fields of interest, we observed that among the articles describing the pathophysiology of this disease, the study by H. Hu published in 2016 in Plastic and Reconstructive Surgery journal has the highest number of citations (127 citations). This article describes the discovery of a distinct microbiome and bacterial biofilm in histological samples from BIA-ALCL patients suggesting a possible role of infection as a causative agent. This article also suggests that strategies to reduce implant contamination must be adopted as well as improved [12].
In the field of diagnostics, the publication with the most citations was received by M. E. Kadin from Boston University School of Medicine. Published in Aesthetic Surgery Journal in 2016, this article received 71 citations. In this study the authors suggest certain biomarkers like JunB and SATB1 as possible indicators to identify the risk of developing BIA-ALCL [13].
Among the studies focused on the oncological management of BIA-ALCL, the aforementioned article by Miranda et al tops the list. This is followed by “Complete surgical excision is essential for the management of patients with breast implant-associated anaplastic large cell lymphoma” , an article authored by M. W. Clemens in 2016 which received 117 citations. The authors performed a clinical follow up of 87 patients, and reported on their overall survival. Also they compared the outcomes of different management strategies such as partial and total capsulectomy, systemic chemotherapy, radiation therapy and concluded that complete surgical excision achieves the best outcomes [14].
Excluding the pioneering report by Keech et al, the case report with the highest number of citations was by A. C. Roden from Mayo Clinic, Rochester, Minnesota (111 citations). In this study from 2008, the authors followed the progress of therapy of 4 patients diagnosed with primary ALCL adjacent to breast prostheses and was able to showcase the indolent nature of this disease entity [15]. Among systemic reviews, the most influential one received 137 citations and was authored by G. S. Brody in 2015. In this article, the authors performed a review of the existing literature at the time and also reported on a number of new cases [16].
The mean number of citations of these 50 most cited articles was calculated to be 65.5 citations. The authors observed (Graph 2) that the majority of the high impact literature on BIA-ALCL are case reports (36%; N = 18) followed by case series (18%; N = 9) and articles on its pathophysiology (16%; N = 8). There were 3 articles focusing on the topic of oncologic management, 2 on diagnostics and 1 on informed consent. The rest of the publications were systemic reviews (12%; N = 6) and database studies (6%; N = 3). This showcases that the lion’s share of the existing literature on BIA-ALCL is focused on the monitoring of this disease entity. Therefore, there may be a need for future studies to investigate the fields of diagnosis and oncological management.

Regarding their origin, the nation with the highest number of articles was the USA (66%; N = 33); whereas among the institutes, University of Texas MD Anderson Cancer Center tops the list (Tab. 8). The high volume of research originating in the USA may be attributed partly to the large number of breast reconstruction procedures being performed there [72,73]. Most of the articles were published in Plastic and Surgery Journal (26%; N = 13). The second place was shared by Aesthetic Surgery Journal and Leukemia and Lymphoma with 3 articles each (Tab. 9). The majority of the included studies had LoE 5 (38%; N = 19), while only one article achieved LoE 2. The lack of articles with LoE 1, i.e. randomized controlled trials, may be partly attributed to the unique challenges faced in generating such evidence [74–76].
The Web of Science Citation Index was the only tool used for our data collection and therefore this study is limited by its accuracy. Another limitation is that though citation analysis was used here to stratify the articles, it is not necessarily a measure of the scientific quality or influence of the individual manuscripts. A further shortcoming of this study was that only articles in the English language were taken into consideration. Though the number of citations may represent the impact of an article on the literature, it can be influenced by many external factors and bias [77].
Conclusion
To the best of our knowledge this is the first time citation analysis has been performed on publications pertaining to BIA-ALCL. Through this study we see that the majority of existing literature is focused on the monitoring of this disease entity. Thus, there may be a need to further investigate the pathophysiology and to develop strategies for diagnosis, and protocols for oncological management.
Roles of authors: The first author, Austin Paul Kallarackal was involved in writing the manuscript and the collection of articles via Web of Science citation index, and also partly worked on the extraction and compilation of the data. Igor Slaninka provided the guidance and support to come up with the research question, decide on the correct search terms and finalize the articles to be included. Nancy Mrozková was involved in working on the collected articles, compiling them into the final list of articles and also in extracting the required data.
Disclosure: The authors declared no potential conflicts of interest with respect to the research, authorship and publication of this article.
Funding: The authors received no financial support for the research, authorship and publication of this article.
Austin Paul Kallarackal, MD
Faculty of Medicine in Hradec Kralove, Charles University in Prague
Šimkova 870
500 03 Hradec Králové
Czech Republic
e-mail: austinpaul@gmail.com
Submitted: 27.3.2021
Accepted: 28.7.2021
Sources
1. Keech JA. Jr, Creech BJ. Anaplastic T-cell lymphoma in proximity to a saline-filled breast implant. Plast Reconstr Surg. 1997, 100(2): 554–555.
2. Rastogi P., Riordan E., Moon D., et al. Theories of etiopathogenesis of breast implant-associated anaplastic large cell lymphoma. Plast Reconstr Surg. 2019, 143 (3S): 23S–29S.
3. Swerdlow SH., Campo E., Pileri SA., et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood 2016, 127(20): 2375–2390.
4. Di Napoli A. Achieving Reliable Diagnosis in Late Breast Implant Seromas: From Reactive to Anaplastic Large Cell Lymphoma. Plast Reconstr Surg. 2019, 143(3S): 15S–22S.
5. Collett DJ., Rakhorst H., Lennox P., et al. Current risk estimate of breast implant-associated anaplastic large cell lymphoma in textured breast implants. Plast Reconstr Surg. 2019, 143 (3S): 30S–40S.
6. Kreutz-Rodrigues L., Shapiro D., Mardini S., et al. Landmarks in facial rejuvenation surgery: the top 50 most cited articles. Aesthet Surg J. 2020, 40(1): NP1–NP7.
7. Uysal E. Top 100 cited classic articles in breast cancer research. Eur J Breast Health. 2017, 13(3): 129–137.
8. Joyce KM., Joyce CW., Kelly JC., et al. Levels of evidence in the plastic surgery literature: a citation analysis of the top 50 ”classic” papers. Arch Plast Surg. 2015, 42(4): 411–418.
9. Paladugu R., Schein M., Gardezi S., et al. One hundred citation classics in general surgical journals. World J Surg. 2002, 26(9): 1099–1105.
10. de Jong D., Vasmel WLE., de Boer JP., et al. Anaplastic large-cell lymphoma in women with breast implants. JAMA. 2008, 300(17): 2030–2035.
11. Miranda RN., Aladily TN., Prince HM., et al. Breast implant-associated anaplastic large-cell lymphoma: long-term follow-up of 60 patients. J Clin Oncol. 2014, 32(2): 114–120.
12. Hu H., Johani K., Almatroudi A., et al. Bacterial biofilm infection detected in breast implant-associated anaplastic large-cell lymphoma. Plast Reconstr Surg. 2016, 137(6): 1659–1669.
13. Kadin ME., Deva A., Xu H., et al. Biomarkers provide clues to early events in the pathogenesis of breast implant-associated anaplastic large cell lymphoma. Aesthet Surg J. 2016, 36(7): 773–781.
14. Clemens MW., Medeiros LJ., Butler CE., et al. Complete surgical excision is essential for the management of patients with breast implant-associated anaplastic large-cell lymphoma. J Clin Oncol. 2016, 34(2): 160–168.
15. Roden AC., Macon WR., Keeney GL., et al. Seroma-associated primary anaplastic large-cell lymphoma adjacent to breast implants: an indolent T-cell lymphoproliferative disorder. Mod Pathol. 2008, 21(4): 455–463.
16. Brody GS., Deapen D., Taylor CR., et al. Anaplastic large cell lymphoma occurring in women with breast implants: analysis of 173 cases. Plast Reconstr Surg. 2015, 135(3): 695–705.
17. Kim B., Roth C., Chung KC., et al. Anaplastic large cell lymphoma and breast implants: a systematic review. Plast Reconstr Surg. 2011, 127(6): 2141–2150.
18. Hu H., Jacombs A., Vickery K., et al. Chronic biofilm infection in breast implants is associated with an increased T-cell lymphocytic infiltrate: implications for breast implant-associated lymphoma. Plast Reconstr Surg. 2015, 135(2): 319–329.
19. Loch-Wilkinson A., Beath KJ., Knight RJW., et al. breast implant-associated anaplastic large cell lymphoma in Australia and New Zealand: high-surface-area textured implants are associated with increased risk. Plast Reconstr Surg. 2017, 140(4): 645–654.
20. Aladily TN., Medeiros LJ., Amin MB., et al. Anaplastic large cell lymphoma associated with breast implants: a report of 13 cases. Am J Surg Pathol. 2012, 36(7): 1000–1008.
21. Doren EL., Miranda RN., Selber JC., et al. U.S. epidemiology of breast implant-associated anaplastic large cell lymphoma. Plast Reconstr Surg. 2017, 139(5): 1042–1050.
22. Laurent C., Delas A., Gaulard P., et al. Breast implant-associated anaplastic large cell lymphoma: two distinct clinicopathological variants with different outcomes. Ann Oncol. 2016, 27(2): 306–314.
23. Kadin ME., Morgan J., Xu H., et al. CD30+ T cells in late seroma may not be diagnostic of breast implant-associated anaplastic large cell lymphoma. Aesthet Surg J. 2017, 37(7): 771–775.
24. de Boer M., van Leeuwen FE., Hauptmann M., et al. Breast implants and the risk of anaplastic large-cell lymphoma in the breast. JAMA Oncol. 2018, 4(3): 335–341.
25. Gaudet G., Friedberg JW., Weng A., et al. Breast lymphoma associated with breast implants: two case-reports and a review of the literature. Leuk Lymphoma. 2002, 43(1): 115–119.
26. Miranda RN., Lin L., Talwalkar SS., et al. Anaplastic large cell lymphoma involving the breast: a clinicopathologic study of 6 cases and review of the literature. Arch Pathol Lab Med. 2009, 133(9): 1383–1390.
27. Carty MJ., Pribaz JJ., Antin JH., et al. A patient death attributable to implant-related primary anaplastic large cell lymphoma of the breast. Plast Reconstr Surg. 2011, 128(3):112e–118e.
28. Newman MK., Zemmel NJ., Bandak AZ., et al. Primary breast lymphoma in a patient with silicone breast implants: a case report and review of the literature. J Plast Reconstr Aesthet Surg. 2008, 61(7): 822–825.
29. Thompson PA., Lade S., Webster H., et al. Effusion-associated anaplastic large cell lymphoma of the breast: time for it to be defined as a distinct clinico-pathological entity. Haematologica. 2010, 95(11): 1977–1979.
30. Wong AK., Lopategui J., Clancy S., et al. Anaplastic large cell lymphoma associated with a breast implant capsule: a case report and review of the literature. Am J Surg Pathol. 2008, 32(8): 1265–1268.
31. Lechner MG., Megiel C., Church CH., et al. Survival signals and targets for therapy in breast implant-associated ALK – anaplastic large cell lymphoma. Clin Cancer Res. 2012, 18(17): 4549–4559.
32. Berry MG., Stanek JJ. The PIP mammary prosthesis: a product recall study. J Plast Reconstr Aesthet Surg. 2012, 65(6): 697–704.
33. Fritzsche FR., Pahl S., Petersen I., et al. Anaplastic large-cell non-Hodgkin’s lymphoma of the breast in periprosthetic localisation 32 years after treatment for primary breast cancer – a case report. Virchows Arch. 2006, 449(5): 561–564.
34. Lechner MG., Lade S., Liebertz DJ., et al. Breast implant-associated, alk-negative, t-cell, anaplastic, large-cell lymphoma: establishment and characterization of a model cell line (TLBR-1) for this newly emerging clinical entity. Cancer. 2011, 117(7): 1478–1489.
35. Li S., Lee AK. Silicone implant and primary breast ALK1-negative anaplastic large cell lymphoma, fact or fiction? Int J Clin Exp Pathol. 2010, 3(1): 117–127.
36. Srinivasa DR., Miranda RN., Kaura A., et al. Global adverse event reports of breast implant-associated alcl: an international review of 40 government authority databases. Plast Reconstr Surg. 2017, 139(5): 1029–1039.
37. Gidengil CA., Predmore Z., Mattke S., et al. Breast implant-associated anaplastic large cell lymphoma: a systematic review. Plast Reconstr Surg. 2015, 135(3): 713–720.
38. Taylor CR., Siddiqi IN., Brody GS., et al. Anaplastic large cell lymphoma occurring in association with breast implants: review of pathologic and immunohistochemical features in 103 cases. Appl Immunohistochem Mol Morphol. 2013, 21(1): 13–20.
39. Popplewell L., Thomas SH., Huang Q., et al. Primary anaplastic large-cell lymphoma associated with breast implants. Leuk Lymphoma. 2011, 52(8): 1481–1487.
40. Olack B., Gupta R., Brooks GS. Anaplastic large cell lymphoma arising in a saline breast implant capsule after tissue expander breast reconstruction. Ann Plast Surg. 2007, 59(1): 56–57.
41. Alobeid B., Sevilla DW., El-Tamer MB., et al. Aggressive presentation of breast implant-associated ALK-1 negative anaplastic large cell lymphoma with bilateral axillary lymph node involvement. Leuk Lymphoma. 2009, 50(5): 831–833.
42. Blombery P., Thompson ER., Jones K., et al. Whole exome sequencing reveals activating JAK1 and STAT3 mutations in breast implant-associated anaplastic large cell lymphoma anaplastic large cell lymphoma. Haematologica. 2016, 101(9): e387–e390.
43. Taylor KO., Webster HR., Prince HM. Anaplastic large cell lymphoma and breast implants: five Australian cases. Plast Reconstr Surg. 2012, 129(4): 610e–617e.
44. Adrada BA., Miranda RN., Rauch GM., et al. Breast implant-associated anaplastic large cell lymphoma: sensitivity, specificity, and findings of imaging studies in 44 patients. Breast Cancer Res Treat. 2014, 147(1): 1–14.
45. Bishara MRY., Ross C., Sur M.. Primary anaplastic large cell lymphoma of the breast arising in reconstruction mammoplasty capsule of saline filled breast implant after radical mastectomy for breast cancer: an unusual case presentation. Diagn Pathol. 2009, 4 : 11.
46. George EV., Pharm J., Houston C., et al. Breast implant-associated ALK-negative anaplastic large cell lymphoma: a case report and discussion of possible pathogenesis. Int J Clin Exp Pathol. 2013, 6(8): 1631–1642.
47. Adams WP. Jr, Culbertson EJ., Deva AK., et al. Macrotextured breast implants with defined steps to minimize bacterial contamination around the device: experience in 42,000 implants. Plast Reconstr Surg. 2017, 140(3): 427–431.
48. Thompson PA., Prince HM. Breast implant-associated anaplastic large cell lymphoma: a systematic review of the literature and mini-meta analysis. Curr Hematol Malig Rep. 2013, 8(3): 196–210.
49. Story SK., Schowalter MK., Geskin LJ. Breast implant-associated ALCL: a unique entity in the spectrum of CD30+ lymphoproliferative disorders. Oncologist. 2013, 18(3): 301–307.
50. Di Napoli A., Jain P., Duranti E., et al. Targeted next generation sequencing of breast implant-associated anaplastic large cell lymphoma reveals mutations in JAK/STAT signalling pathway genes, TP53 and DNMT3A. Br J Haematol. 2018, 180(5): 741–744.
51. Roden MW., Miranda RN., Butler CE. Breast implant informed consent should include the risk of anaplastic large cell lymphoma. Plast Reconstr Surg. 2016, 137(4): 1117–1122.
52. Kim B., Predmore ZS., Mattke S., et al. Breast implant-associated anaplastic large cell lymphoma: updated results from a structured expert consultation process. Plast Reconstr Surg Glob Open. 2015, 3(1): e296.
53. Smith TJ., Ramsaroop R. Breast implant related anaplastic large cell lymphoma presenting as late onset peri-implant effusion. Breast. 2012, 21(1): 102–104.
54. Leberfinger AN., Behar BJ., Williams NC., et al. Breast implant-associated anaplastic large cell lymphoma: a systematic review. JAMA Surg. 2017, 152(12): 1161–1168.
55. Hart AM., Lechowicz MJ., Peters KK., et al. Breast implant-associated anaplastic large cell lymphoma: report of 2 cases and review of the literature. Aesthet Surg J. 2014, 34(6): 884–894.
56. Bautista-Quach MA., Nademanee A., Weisenburger DD., et al. Implant-associated primary anaplastic large-cell lymphoma with simultaneous involvement of bilateral breast capsules. Clin Breast Cancer. 2013, 13(6): 492–495.
57. Johnson L., O’Donoghue JM., McLean N., et al. Breast implant associated anaplastic large cell lymphoma: The UK experience. Recommendations on its management and implications for informed consent. Eur J Surg Oncol. 2017, 43(8): 1393–1401.
58. Farace F., Bulla A., Marongiu F., et al. Anaplastic large cell lymphoma of the breast arising around mammary implant capsule: an Italian report. Aesthetic Plast Surg. 2013, 37(3): 567–571.
59. Oxford Centre for Evidence-Based Medicine Levels of Evidence. [online]. Available from: https://www.cebm.net/2016/05/ocebm-levels-of-evidence/.
60. Sinha Y., Iqbal FM., Spence JN., et al. A bibliometric analysis of the 100 most-cited articles in rhinoplasty. Plast Reconstr Surg Glob Open. 2016, 4(7): e820.
61. Kim K., Ibrahim AM., Koolen PG., et al. Highest impact articles in microsurgery: a citation analysis. J Reconstr Microsurg. 2015, 31(7): 527–540.
62. Joyce CW., Carroll SM. Microsurgery: the top 50 classic papers in plastic surgery: a citation analysis. Arch Plast Surg. 2014, 41(2): 153–157.
63. Joyce CW., Kelly JC., Carroll SM. The 100 top-cited classic papers in hand surgery. J Plast Surg Hand Surg. 2014, 48(4): 227–233.
64. Mahon NA., Joyce CW., Thomas S., et al. The 50 most cited papers in craniofacial anomalies and craniofacial surgery. Arch Plast Surg. 2015, 42(5): 559–566.
65. Whitney E., Mahato D., Odell T., et al. The 100-most cited articles about craniectomy and hemicraniectomy: a bibliometric analysis. Cureus. 2019, 11(8): e5524.
66. Tahiri Y., Fleming TM., Greathouse T., et al. Analysis of the 50 most cited papers in craniofacial surgery. J Craniomaxillofac Surg. 2015, 43(10): 2152–2157.
67. Chang MT., Schwam ZG., Schutt CA., et al. The 50 most cited articles in facial plastic surgery. Aesthetic Plast Surg. 2017, 41(5): 1202–1207.
68. Muslu Ü. The evolution of breast reduction publications: a bibliometric analysis. Aesthetic Plast Surg. 2018, 42(3): 679–691.
69. Christou P., Antonarakis GS. The 100 most-cited human cleft lip and palate-related articles published in dentistry, oral surgery, and medicine journals. Cleft Palate Craniofac J. 2015, 52(4): 437–446.
70. Mahon NA., Joyce CW. A bibliometric analysis of the 50 most cited papers in cleft lip and palate. J Plast Surg Hand Surg. 2015, 49(1): 52–58.
71. Mbaidjol Z., Rothenberger J., Chetany R. A scientometric analysis of the 50 most cited articles for reconstruction of the lower extremity. Surg Res Pract. 2019, 2019 : 3068028.
72. Wilkins EG., Alderman AK. Breast reconstruction practices in North America: current trends and future priorities. Semin Plast Surg. 2004, 18(2): 149–155.
73. Moghimi M., Fathi M., Marashi A., et al. A scientometric analysis of 20 years of research on breast reconstruction surgery: a guide for research design and journal selection. Arch Plast Surg. 2013, 40(2): 109–115.
74. Joyce CW., Joyce KM., Sugrue CM., et al. Plastic surgery and the breast: a citation analysis of the literature. Plast Reconstr Surg Glob Open. 2(11): e251.
75. Solomon MJ., Laxamana A., Devore L., et al. Randomized controlled trials in surgery. Surgery. 1994, 115(6): 707–712.
76. van der Linden W. Pitfalls in randomized surgical trials. Surgery. 1980, 87(3): 258–262.
77. Asaad M., Kallarackal AP., Meaike J., et al. Citation skew in plastic surgery journals: does the journal impact factor predict individual article citation rate? Aesthet Surg J. 2020, 40(10): 1136–1142.
Labels
Plastic surgery Orthopaedics Burns medicine TraumatologyArticle was published in
Acta chirurgiae plasticae

2021 Issue 3
- Possibilities of Using Metamizole in the Treatment of Acute Primary Headaches
- Metamizole at a Glance and in Practice – Effective Non-Opioid Analgesic for All Ages
- Metamizole vs. Tramadol in Postoperative Analgesia
- Spasmolytic Effect of Metamizole
- Metamizole in perioperative treatment in children under 14 years – results of a questionnaire survey from practice
-
All articles in this issue
- Reconstructive and esthetic breast surgery after solid organ transplantation – a systematic review, proposal of a novel protocol and case presentations
- Characteristics of fingertip injuries and proposal of a treatment algorithm from a hand surgery referral center in Mexico City
- Platelet-rich plasma improves esthetic postoperative outcomes of maxillofacial surgical procedures
- Breast implant-associated anaplastic large-cell lymphoma – an evolution through the decades: citation analysis of the top fifty most cited articles
- Bone invasion by oral squamous cell carcinoma
- Three-dimensional navigation in maxillofacial surgery – the way to minimize surgical stress and improve accuracy in fibula free flap and Eagle’s syndrome surgical procedures
- Is it a second scrotum?
- Professor Radana Königová Prize awards
- Editorial
- Fournier’s gangrene secondary to male’s circumcision – a case report and review of the literature
- Acta chirurgiae plasticae
- Journal archive
- Current issue
- About the journal
Most read in this issue
- Bone invasion by oral squamous cell carcinoma
- Platelet-rich plasma improves esthetic postoperative outcomes of maxillofacial surgical procedures
- Breast implant-associated anaplastic large-cell lymphoma – an evolution through the decades: citation analysis of the top fifty most cited articles
- Characteristics of fingertip injuries and proposal of a treatment algorithm from a hand surgery referral center in Mexico City