The Effect of Different Occupational Therapy Techniques on Post-stroke Patients
Vliv různých technik pracovních terapií na pacienty po mozkové mrtvici
Cíl:
Zhodnotit účinnost terapie vynuceného používání (constraint-induced movement therapy) a zrcadlové terapie (mirror therapy) prováděné v průběhu ergoterapie z hlediska funkce horních končetin, soběstačnosti a kognitivních funkcí u pacientů po cévní mozkové příhodě.
Materiál a metody:
Do studie bylo zařazeno 36 pacientů po cévní mozkové příhodě, kteří byli náhodně rozděleni do dvou skupin: ve skupině 1 bylo 18 pacientů, kteří podstoupili terapii vynuceného používání, a ve skupině 2 bylo 18 pacientů, kteří absolvovali zrcadlovou terapii. Funkčnost postižené paže byla u pacientů hodnocena pomocí Frenchayského testu paže (Frenchay Arm Test) a pro hodnocení soběstačnosti pacientů byl použit test funkční soběstačnosti – Functional Independence Measure (FIM). Pro vyhodnocení změn kognitivních funkcí sledovaných subjektů byl použit krátký test kognitivních funkcí (Mini-Mental State Examination).
Výsledky:
V obou skupinách pacientů bylo pozorováno signifikantní zlepšení funkčnosti postižené končetiny, soběstačnosti a kognitivních funkcí. Porovnání výsledků v obou skupinách ukázalo, že pacienti ve skupině 2 dosahovali statisticky signifikantně lepších výsledků při plnění úkolů v rámci Frenchayského testu paže.
Závěr:
Použití zrcadlové terapie při rehabilitaci pacientů po cévní mozkové příhodě se z hlediska obnovení funkčnosti postižené paže (při hodnocení rychlosti plnění úkolů) ukázalo jako účinnější než terapie vynuceného používání.
Klíčová slova:
cévní mozková příhoda – terapie vynuceného používání – zrcadlová terapie
Autoři deklarují, že v souvislosti s předmětem studie nemají žádné komerční zájmy.
Redakční rada potvrzuje, že rukopis práce splnil ICMJE kritéria pro publikace zasílané do biomedicínských časopisů.
Authors:
D. Petruševičienė 1; D. Virviciūtė 1; R. Savickas 1,2; E. Lendraitienė 1; S. Mingaila 1,2; P. Vasilavicius 3
Authors‘ workplace:
Department of Rehabilitation, Medical
Academy of Lithuanian University
of Health Sciences, Kaunas, Lithuania
1; Department of Neurorehabilitation
Hospital of Lithuanian University
of Health Sciences Kauno klinikos
Kaunas, Lithuania
2; Department of Environmental and
Occupational Medicine, Lithuanian
University of Health Sciences, Kaunas
Lithuania
3
Published in:
Cesk Slov Neurol N 2017; 80/113(4): 464-468
Category:
Short Communication
doi:
https://doi.org/10.14735/amcsnn2017464
Overview
Aim:
To evaluate the effect of constraint-induced movement and mirror therapy on stroke patients’ arm function, independence, and cognitive functions during occupational therapy.
Materials and methods:
The study included 36 ischaemic stroke patients. The subjects were randomly distributed into two groups: group 1 consisted of 18 patients who underwent constraint-induced movement therapy, and group 2 consisted of 18 patients who underwent mirror therapy. The function of the affected arm in the subjects was evaluated by applying the Frenchay Arm Test, and the patients’ independence level was evaluated by using the Functional Independence Measure. The Mini-Mental State Examination was applied for the evaluation of changes in the subjects’ cognitive functions.
Results:
A significant improvement in the function of the affected arm, independence, and cognitive functions was observed in both patient groups. The comparison of the results between the groups showed that group 2 patients demonstrated statistically significantly better results of the changes in the arm function when performing Frenchay Arm Test tasks.
Conclusion:
The application of mirror therapy in stroke patients during inpatient rehabilitation proved to be more effective in restoring the function of the affected arm (when evaluating the task performance speed), compared to the application of constraint-induced movement therapy.
Key words:
stroke – constraint-induced movement therapy – mirror therapy
Chinese summary - 摘要
不同职业疗法技术对卒中后遗症患者的影响目标:
评估强制性诱导运动和镜像疗法对卒中患者的手臂功能、独立性和职业疗法期间认知功能的影响。
材料和方法:
该研究包括36名缺血性卒中患者。受试者被随机分为两组:第一组由18名接受强制性诱导运动疗法的患者组成,第二组由18名接受镜像疗法的患者组成。采用Frenchay手臂测试评估患者受影响手臂的功能,并使用功能独立性评定评估患者的独立性水平。 应用简易精神状态检查表评估患者认知功能的变化程度。
结果:
在两组患者里,受影响手臂功能、独立性以及认知功能都有明显改善。通过比较两组患者的结果发现:第2组患者在进行Frenchay手臂测试任务时,手臂功能变化统计力度更显著,取得的结果更好。
结论:
在恢复受影响手臂功能(评估任务表现速度时)方面,与应用强制性诱导运动疗法相比,在脑卒中患者住院康复期间应用镜像疗法被证明更有效。
关键词:
卒中 - 强制性诱导运动疗法 - 镜像疗法
Introduction
A stroke is an acute focal disruption of cerebral blood flow. It is recognised as one of the main causes of morbidity, mortality, and long-term disability worldwide – both in developed and developing countries. As the cause of death, it ranks second (11.13%) to cardiovascular diseases [1,2]. In the European Union, about one million strokes occur annually [3]. Lithuania has the 5th highest rate of death from stroke in Europe – 202 women and 247 men per 100,000 population [4]. Approximately 87% of strokes are ischaemic [2].
The manifestations of a stroke may differ from patient to patient [5]. Arm dysfunction is among the most common neurological sequela of a stroke [6]. As much as 60% of stroke patients have residual arm dysfunction 6 months after completion of the rehabilitation programme, and this dysfunction negatively affects independence in daily activities [7]. Cognitive dysfunction has been proven to have an indirect effect on functional recovery, limiting the patients’ participation in rehabilitation due to their poor compliance [8]. An occupational therapist helps the patients to recover physical and mental abilities and to strive for maximal independence in daily activities.
There are numerous techniques – both well-established and novel ones – that, when used in combination with the conventional occupational therapy procedures, help the patients recover their functional status, cognitive functions, and independence. In Lithuania, both constraint-induced movement therapy and mirror therapy are used with increasing frequency during the occupational therapy procedures for stroke patients. The effectiveness of these techniques in restoring stroke patients’ arm function and independence has been proven by scientific research, but so far it has remained unclear which of the two techniques is superior in this respect. In addition, evaluations of the effect of these therapies on the patients’ cognitive functions and independence have been controversial. Only small-scale studies have analysed the effect of these therapies, focusing separately on their effect on the arm function, independence, and/ or cognitive functions. The aim of our study was to evaluate the effect of constraint-induced movement therapy and mirror therapy on stroke patients’ arm function, independence, and cognitive functions during occupational therapy.
Materials and methods
Study design
A randomized pre-test and post-test group design. The study was approved by the Bioethics Centre (No. BEC-ER(B)-180). All of the participants provided their written informed consent prior to their inclusion in the study, in accordance with the ethical principles of the Declaration of Helsinki.
Participants
This study was conducted in 2015 – 2016. The subjects were selected according to the following criteria: muscle force evaluation score on manual muscle testing (MMT) – 2–3 points out of 5; mental state evaluation score on the Mini-Mental State Examination (MMSE) scale – not less than 20 points; muscle spasticity according to the Ashworth scale – 0–1 point; and evaluation on the Barthel index (BI) – from 25 to 60 points.
Exclusion criteria: refusing to participate in a study, muscle force evaluation score on manual muscle testing (MMT) < 2 or > 3; mental state evaluation score on the Mini-Mental State Examination (MMSE) scale < 20; muscle spasticity according to the Ashworth scale > 1 and evaluation on the Barthel index (BI) – < 25 or > 60.
After the analysis of literature data, we developed the data collection protocol – a questionnaire for stroke patients. In total, 36 ischaemic stroke patients participated in the study. The patients’ age ranged from 50 to 81 years, the mean age being 67.7 ± 9.4 years. Both subject groups were homogeneous with respect to the dominant arm, the affected side, and the attributes evaluated according to the selection criteria (Tab. 1).
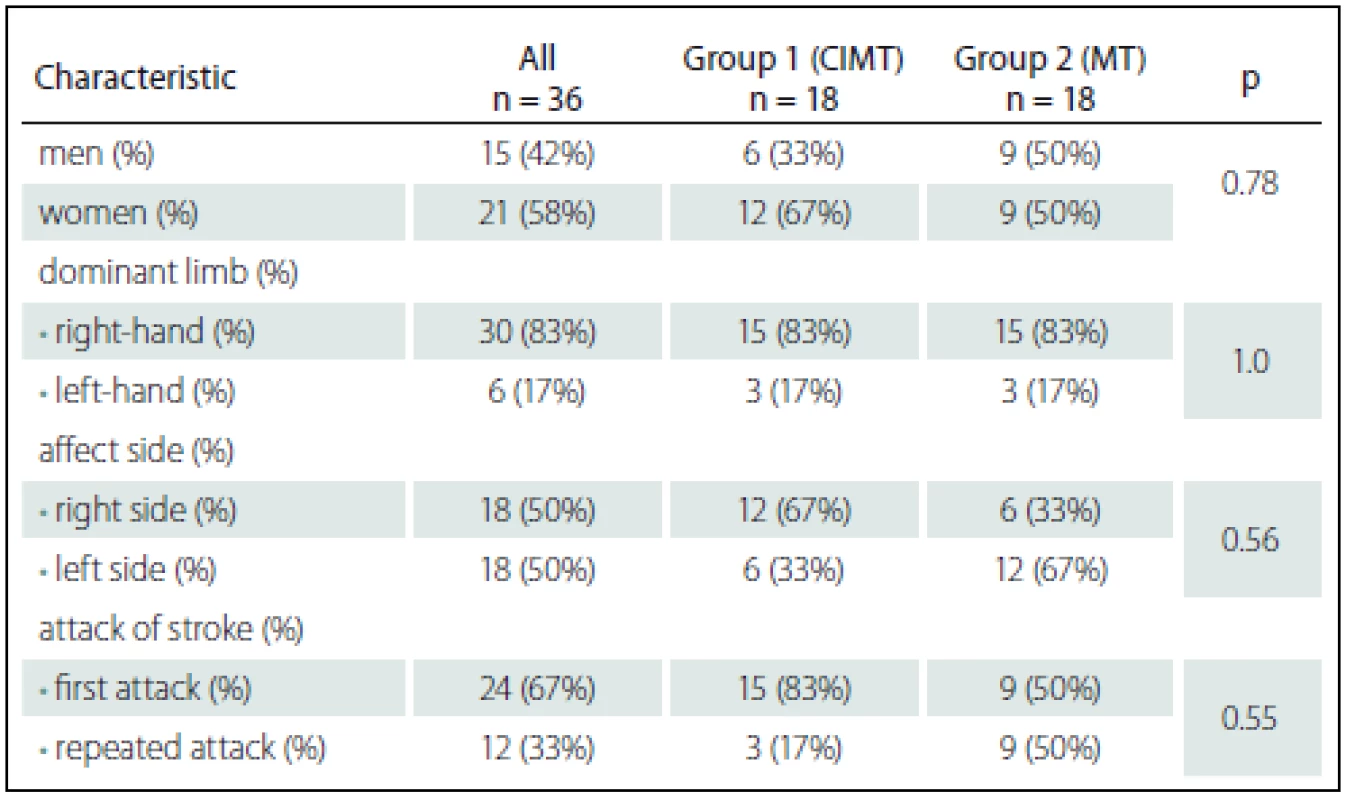
The subjects were randomly distributed into two groups: the first group (group 1)consisted of 18 patients who underwent conventional occupational therapy and constraint-induced movement therapy (CIMT), and the second group (group 2) consisted of 18 patients who underwent conventional occupational therapy and mirror therapy (MT).
Interventions
In subjects from group 1 (CIMT), the movements of the healthy arm were restrained using a special glove. The subjects had to wear this glove for 4 hours a day during their waking hours. Every hour, the subjects had 10 min breaks. The patients were informed in which situations they could remove the glove (e. g. during bathing). When wearing the glove, the patients had to perform various tasks with the affected arm only – e. g. physical exercises, inserting pegs, collecting small objects, performing daily activity tasks, etc.
During the mirror therapy, a mirror screen was used. During the tasks, subjects from group 2 (MT) had to sit at the table with a mirror in front of them. The affected arm was placed behind the mirror at a distance of 10 – 15 cm, and the healthy arm was positioned in front of the mirror at the same distance – i.e. 10 – 15 cm. The total number of tasks the subjects had to perform was 12. During the last three tasks, an additional object – hand therapy exercise putty – was required. The tasks varied in complexity and were performed successively – from the simplest to the most complex. Prior to performing the tasks, the subjects received verbal instructions. During the tasks, the subjects had to watch the reflection of the unaffected arm in the mirror because this is the only way to activate mirror neurons in the brain, to create feedback, and to stimulate movement recovery.
The occupational therapy programme was designed when taking into consideration the patients’ complaints and predominant dysfunctions. The assignments were performed once daily, and the programme consisted of exercises and instruments for strengthening arm muscles, increasing the range of motion, improving fine motor functions and movement coordination, and developing cognitive functions.
During the rehabilitation programme, in addition to occupational therapy, the patients also underwent physical therapy and physiotherapy, were consulted by a social worker and a psychologist, and received pharmacological treatment. The physiotherapy was identical in both groups: functional electrical stimulation of muscles, intermittent pneumatic compression therapy and paraffin wax treatment.
During the rehabilitation period, we evaluated the subjects’ arm function, independence level, and cognitive functions. The testing was performed twice – at the beginning of the rehabilitation and after 2 weeks of therapy. To evaluate arm function, we used the Frenchay Arm Test (FAT) [9], to evaluate the subjects’ independence level, the Functional Independence Measure (FIM) [9] was used, and the MMSE [9] was applied for the evaluation of the subjects’ cognitive functions.
Statistical analysis
Statistical data analysis was performed using software packages “Microsoft Office Excel 2007” and “IBM SPSS Statistics Base 22.0”. The findings of the study were described by using conventional numeral characteristics (percentage, minimal and maximal values, mean value, standard error of the mean, standard deviation, median, mean rank, and quartile range). To compare the distributions before and after the therapy, we applied the marginal homogeneity test and the Wilcoxon criterion. Distributions between the groups were compared by applying the Mann-Whitney U test and the χ2 criterion. To compare the time changes between the groups, we applied dispersion analysis of repeated measurements. The difference between the results was considered to be statistically significant when p < 0.05.
Results
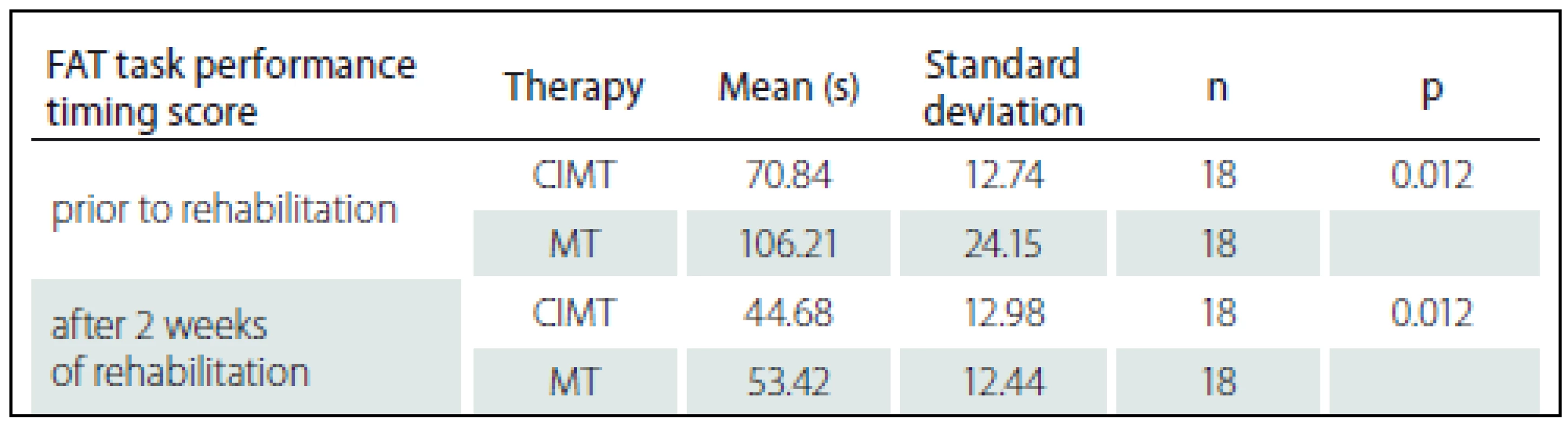
The function of the subjects’ affected arm was evaluated by applying the Frenchay Arm Test (FAT), where the function was assessed by applying the performance score (the range of the score was 0 – 5 points) and the performance time (in seconds). Both at baseline and at the end of the study, the function of the affected arm in group 1(CIMT) subjects was better than that observed in subjects of group 2 (MT). However, at the end of the study, a significant improvement in the function of the affected arm was observed in subjects from both groups (p < 0.05) (Graph 1, 2).


The subjects’ independence level during inpatient rehabilitation was evaluated using the FIM test, and the results were calculated as a sum score, which ranged from 18 to 126 points. The evaluation of the subjects’ independence level revealed that both at baseline and at the end of the study, group 1 (CIMT) subjects demonstrated slightly better results than those subjects from group 2 (MT), but the difference was not statistically significant (p > 0.05). The subjects from both groups demonstrated an improvement in the independence level at the end of the study (p < 0.05). The subjects’ cognitive functions were evaluated using the MMSE test (based on the selection criteria, the score interval was limited to 20 – 30 points). The obtained results showed that subjects in both groups demonstrated similar cognitive skills at the begining of the study (p > 0.05). At the end of the study, a statistically significant improvement in cognitive skills was observed in both subject groups (p < 0.05) (Tab. 2).
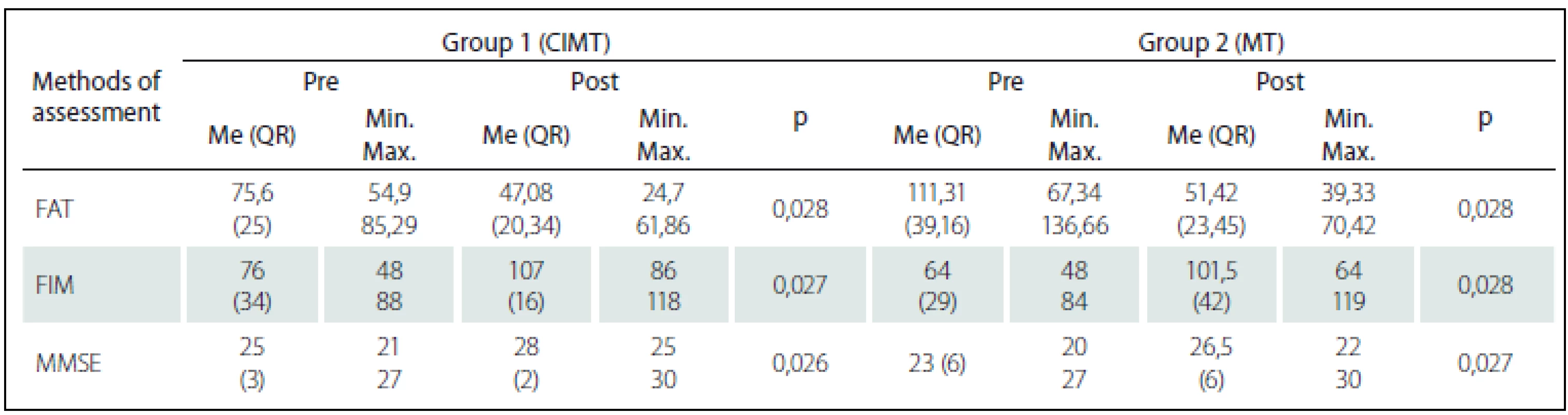
The evaluation of the arm function (in points, using the FAT), the independence level, and cognitive skills in subjects from group 1 (CIMT) and group 2 (MT) yielded no statistically significant difference between the groups (p > 0.05). At the beginning of the study, during the evaluation of the function of the affected arm (task performance time) via the Frenchay Arm Test, subjects from group 1 (CIMT) demonstrated better results (p < 0.05) than from the subjects in group 2: the mean FAT task performance time (± standard deviation) in group 1 was 70.84 s (± 12.74), compared to 106.21 s (± 24.15) in group 2 (MT) subjects (Tab. 3). At the end of the study, the mean FAT task performance time (± standard deviation) after conventional occupational therapy plus constraint-induced movement therapy statistically significantly decreased to 44.68 s (± 12.98) (p = 0.012), and after conventional occupational therapy and mirror therapy, it statistically significantly decreased to 53.42 ± 12.44 s (p = 0.012). However, as seen from the results, the decrease in FAT task performance time in subjects from group 2 (MT) was double that of group 1 (CIMT) subjects. The comparison of FAT task performance time between group 1 (CIMT) and group 2 (MT) subjects revealed a statistically significant difference (p = 0.025).
Discussion
In this study, we presented constraint-induced movement therapy and mirror therapy applied in combination with occupational therapy in stroke patients during the subacute rehabilitation period. In total, we evaluated the arm function, independence level, and cognitive functions in 36 ischaemic stroke patients. The mean age of the participants of the study was 67.7 ± 9.4 years. There was no statistically significant difference (p > 0.05) between group 1 (CIMT) and group 2 (MT) subjects concerning their age, the dominant side, or the affected side. The assessment of the two subject groups with respect to the characteristics evaluated according to the selection criteria (manual muscle testing – MMT, Ashworth, MMSE and BI) showed that both groups were homogeneous (p > 0.05).
The time average after the stroke in patients included in this study was 11 days. The duration of the applied course of therapy was 10 working days. CIMT was applied for 4 hours per day, and MT – for 30 min per day, performing 12 tasks during each session. The core of the constraint-induced movement therapy was first described in 1909 by a German researcher Munk, who described primates’ behaviour. Later on, Ogden and Franz (1917) performed studies with monkeys. Researchers T. P. Pons (1991) and E. Taub (1994) are considered to be pioneers of constraint-induced movement therapy, and R. Ramachandran (1996) – the pioneer of mirror therapy. Original (also known as classical) constraint-induced movement therapy is applied for 6 hours daily, and lasts 2 weeks [10]. Researchers state that classical CIMT should be applied for as much as 90% of the day. Other researchers apply modified constraint-induced movement therapy (mCIMT), whose application varies in duration from 30 min to 6 hours per day, from 2 to 7 sessions per week, and from 2 to 12 weeks [11]. Most researchers apply mirror therapy for 30 min per day for 4 weeks [6,11,12]. Mirror therapy is believed to be effective for the recovery of motor functions and independence in stroke patients [13 – 16].
All the selected patients willingly participated in the study and successfully completed it. Prior to the study, we were careful to make sure the patients did not have the neglect syndrome or severe balance or coordination disorders because this would impede the study. According to literature data, in the presence of the aforementioned disorders, the application of constraint-induced movement therapy is dangerous, and the application of mirror therapy – pointless.During CIMT, the patients were taught appropriate techniques for correct performance of the tasks, whereas during MT, the patients repeatedly performed tasks during which they had to focus on the observation of the reflection of hand movement in the mirror. During the study, we made every effort to commend the patients and motivate them during task performance in order to increase their self-confidence and to stimulate them to use the affected arm. Some patients needed task adjustment, i.e. for some, the task complexity had to be increased, and for some, reduced. This depended on the patients’ physical and mental condition.
During the study, the functional status of the patients’ affected arm was evaluated by applying the Frenchay Arm Test (FAT), their independence – by using the Functional Independence Measure (FIM), and changes in their cognitive functions – by using the MMSE. We found only one study where both therapies – constraint-induced movement therapy and mirror therapy – were applied. In this study, researchers Yoon et al. (2014) evaluated the arm function by using the Box and Block test, the 9-hole Pegboard test, the Wolf Motor Function Test, and Fugl-Meyer Assessment of Motor Recovery after Stroke. Changes in the independence level were evaluated by applying the modified Barthel index (Korean version). In addition to the aforementioned evaluation techniques, other researchers also used the Manual Function Test (MFT) for the evaluation of the arm function, while MMSE was used only as a selection criterion for evaluating the patients’ cognitive functions [4,6].
A search of literature yielded no similar studies in Lithuania or abroad, and thus we cannot compare the obtained results. Yoon et al. (2014) also used both techniques in their study, but they did not compare them.
Post-stroke motor dysfunction – particularly arm dysfunction – is one of the most important factors limiting patients’ occupation and participation. The results of the study showed that the function of the affected arm, the independence level, and cognitive functions significantly (p < 0.05) improved in both studied groups – i.e. both after conventional occupational therapy combined with constraint-induced movement therapy and after conventional occupational therapy combined with mirror therapy. The comparison between mirror therapy and constraint-induced movement therapy showed that mirror therapy was more effective in restoring the function of the affected arm, evaluating it as task performance time in the Frenchay Arm Test (p < 0.05). The application of mirror therapy in stroke patients during inpatient rehabilitation also proved to be superior to constraint-induced movement therapy in restoring the function of the affected arm when evaluating task performance speed. A faster restoration of the arm function increases the patients’ independence and brings them closer to resuming the usual daily routine and occupation.
The authors declare they have no potential conflicts of interest concerning drugs, products, or services used in the study.
The Editorial Board declares that the manuscript met the ICMJE “uniform requirements” for biomedical papers.
assoc. prof. Raimondas Savickas, MD, PhD
Department of Neurorehabilitation
Hospital of Lithuanian
University of Health Sciences Kauno klinikos
Eivenių 2
LT-50161 Kaunas
Lithuania
e-mail: raimondas.savickas@kaunoklinikos.lt
Accepted for review: 7. 12. 2016
Accepted for print: 12. 4. 2017
Sources
1. Sąlyga J, Žiliukas G, Kazlauskas H, Kasiliauskaitė M. Patients after stroke functional status changes in the process of rehabilitation. Sveikatos Mokslai 2014;4 : 95 – 9.
2. Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics – 2015 update: a report from the American Heart Association. Circulation 2015;131(4):29 – 322. doi: 10.1161/ CIR.0000000000000152.
3. Baltaduonienė D, Karsokaitė N. Changes in hand motoric function when applying mirror therapy for patients after stroke. Sveikatos Mokslai 2014;6 : 144 – 7.
4. OECD/ European Union. Health at a Glance: Europe 2014. Paris: OECD Publishing 2014.
5. Hankey GJ. Stroke. Vilnius: Vaistų žinios 2007.
6. Kim H, Shim J. Investigation of the effects of mirror therapy on the upper extremity functions of stroke patients using the manual function test. J Phys Ther Sci 2015;27(1):227 – 9. doi: 10.1589/ jpts.27.227.
7. Claflin ES, Krishnan C, Khot SP. Emerging treatments for motor rehabilitation after stroke. Neurohospitalist 2015;5(2):77 – 88. doi: 10.1177/ 1941874414561023.
8. Cumming TB, Marshall RS, Lazar RM. Stroke, cognitive deficits, and rehabilitation: still an incomplete picture. Stroke 2013;8(1):38 – 45. doi: 10.1111/ j.1747-4949.2012.00972.x.
9. Kolar P, Calta J, Lewit K, et al. Clinical rehabilitation. 1st ed. Praha: Rehabilitation Prague school 2013.
10. Kwakkel G, Veerbeek MJ, van Wegen EE, et al. Constraint-induced movement therapy after stroke. Lancet Neurol 2015;14(2):224 – 34. doi: 10.1016/ S1474-4422(14)70160-7.
11. Kim H, Lee G, Song C. Effect of functional electrical stimulation with mirror therapy on upper extremity motor function in poststroke patients. J Stroke Cerebrovasc Dis 2014;4 : 655 – 61.
12. Yavuzer G, Selles R, Sezer N, et al. Mirror therapy improves hand function in subacute stroke: a randomized controlled trial. Arch Phys Med Rehabil 2008;89(3):393 – 8. doi: 10.1016/ j.apmr.2007.08.162.
13. Bae SH, Jeong WS, Kim KY. Effects of mirror therapy on subacute stroke patients’ brain waves and upper extremity functions. J Phys Ther Sci 2012;11 : 1119 – 22.
14. Park JY, Chang M, Kim KM, et al. The effects of mirror therapy with tasks on upper extremity function and self-care in stroke patients. J Phys Ther Sci 2015;6 : 1499 – 501.
15. Park JY, Chang M, Kim KM, et al. The effect of mirror therapy on upper-extremity function and activities of daily living in stroke patients. J Phys Ther Sci 2015;6 : 1681 – 3.
16. Kim K, Lee S, Kim D, et al. Effects of mirror therapy combined with motor tasks on upper extremity function and activities daily living of stroke patients. J Phys Ther Sci 2016;2 : 483 – 7.
Labels
Paediatric neurology Neurosurgery NeurologyArticle was published in
Czech and Slovak Neurology and Neurosurgery

2017 Issue 4
- Advances in the Treatment of Myasthenia Gravis on the Horizon
- Hope Awakens with Early Diagnosis of Parkinson's Disease Based on Skin Odor
- Memantine in Dementia Therapy – Current Findings and Possible Future Applications
-
All articles in this issue
- Ataxia
- Patient with Hemiplegia Should be Transported Right to the Cerebrovascular Center
- Patient with Hemiplegia Should not be Transported Right to the Cerebrovascular Center
- Should be Patient with Hemiplegia Transported Right to the Cerebrovascular Center?
- Cognitive Functions in Low-grade Glioma Patients – a Systematic Review
- Clinical Importance of Radiological Parameters in Lumbar Spinal Stenosis
- Neurosonological Markers Predict ing Cognitive Deterioration
- Czech National Guillain-Barré Syndrome Registry
- The Role of Drug-induced Sleep Endoscopy in Treatment (Surgical and Non-surgical) in Patients with Obstructive Sleep Apnea
- Nerve Injuries in Supracondylar Humeral Fractures in Children
- A Comprehensive Nationwide Evaluation of Stroke Centres in the Czech Republic Performing Mechanical Thrombectomy in Acute Stroke in 2016
- Clinical View of the Otorhinolaryngologist and Radiologist on the Classification of Fractures of the Temporal Bone
- Experience with using the RevoLix Jr thulium laser – Case Reports
- Dissection of All Four Cervical Arteries in a Patient with Fibromuscular Dysplasia – a Case Report
- Intravenous Thrombolysis after Dabigatran Reversal with a Specific Antidote Idarucizumab
- The Czech Pneumological and Physiological Society and the Czech Society for Paediatric Pulmonology Guidelines for Long-term Home Treatment Using the CoughAssist Machine in Patients with Serious Cough Disorders
- Prevalence of Martin-Gruber Anastomosis – an Electrophysiological Study
- Mortality Prediction in a Neurosurgical Intensive Care Unit
- The Effect of Different Occupational Therapy Techniques on Post-stroke Patients
- Comment of Article The Effect of Different Occupational Therapy Techniques on Post-stroke Patients
- Czech and Slovak Neurology and Neurosurgery
- Journal archive
- Current issue
- About the journal
Most read in this issue
- Czech National Guillain-Barré Syndrome Registry
- Clinical View of the Otorhinolaryngologist and Radiologist on the Classification of Fractures of the Temporal Bone
- The Czech Pneumological and Physiological Society and the Czech Society for Paediatric Pulmonology Guidelines for Long-term Home Treatment Using the CoughAssist Machine in Patients with Serious Cough Disorders
- Nerve Injuries in Supracondylar Humeral Fractures in Children
