OCT Findings and Long-term Follow-up Results of Vitrectomy in Patients with Optic Disc Pit and Associated Maculopathy
Authors:
M. Kováčová; M. Meliška; B. Kalvodová
Authors‘ workplace:
Oční klinika, 1. lékařská fakulta, Univerzita Karlova a Všeobecná fakultní nemocnice, Praha, přednostka doc. MUDr. Jarmila Heissigerová, Ph. D., MBA
Published in:
Čes. a slov. Oftal., 73, 2017, No. 5-6, p. 171-177
Category:
Original Article
Overview
Purpose:
To evaluate OCT findings and long-term follow-up results in patient with optic disc pit (ODP) and associated maculopathy treated with pars plana vitrectomy (PPV).
Methods:
Six eyes of 6 patients (3 females, 3 males) were included in a retrospective study. We excluded patients with ODP without maculopathy. Patients were followed in years 2008-2017. Mean age at the first examination was 40,3 years (15-70 years). Duration of worsening of the best corrected visual acuity (BCVA) ranged from 2 days to few years. In all patients we performed BCVA test at Early Treatment of Diabetic Retinopathy Study (ETDRS) optotype, examination of anterior and posterior segment and photo documentation of fundus. Optic disc, parapapillary region and macula were examined by optic coherence tomography (OCT). Four patients underwent 23-Ga PPV with active detachment of posterior hyaloid membrane and tamponade with perfluoropropan (16% C3F8). In 2 patients a sample of tissue from ODP was taken during PPV to histological examination.
Results:
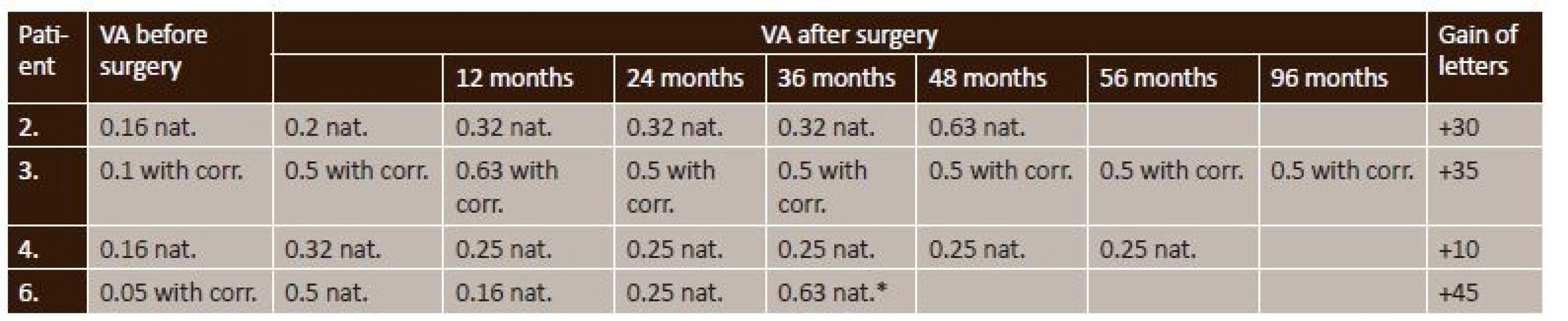
Mean BCVA at the first examination was 0,10 (ranging from 0,05 to 0,16). OCT findings proved macular schisis in outer retinal layers (RSE) in 2 eyes, in 1 of these eyes with additional presence of subretinal fluid. In 4 patients macular schisis in outer as well as inner retinal layers (RSI) was present, in 2 of them with additional subretinal fluid. In 5 eyes glial tissue and/or vitreous condensation was present in ODP. Four eyes with RSE and RSI improved both anatomically as well as functionally after vitrectomy. In 1 patient with previous communication between ODP and RSE this was closed after vitrectomy. Mean pre-operative BCVA was 0,11 (ranging from 0,05 to 0,16), mean final BVCA was 0,5 (ranging from 0,25 to 0,63), mean visual gain was +30 letters (ranging from +10 to +45). Mean follow-up after PPV was 59 months (36–96).
Conclusion:
Spectral OCT shows variability of morphological findings in patient with ODP associated with maculopathy. Traction of glial tissue and/or condensed vitreous in ODP together with adherent posterior vitreous membrane could be one of the factors causing macular retinoschisis and/or secondary serous macular detachment. Complete separation of vitreous from optic nerve head during the vitrectomy is an efficient treatment resulting in macular reattachment and improvement in visual functions.
Key words:
optic disc pit, intrapapillary proliferation, macular retinoschisis, optical coherence tomography, pars plana vitrectomy, posterior vitreous detachment
INTRODUCTION
Optic disc pit (ODP) is a rare congenital anomaly, the pathogenesis of which has not yet been entirely clarified. It is assumed that this concerns a developmental disorder of the primitive epithelial papilla of the optic nerve, and a disorder of the closure of the foetal ocular aperture. Histologically it concerns a herniation of the dysplastic retinal tissue by the focal peripapillary scleral ring (2). The prevalence of ODP is within the range of 0.02 to 0.19% (19). In the majority of cases it concerns a unilateral affliction. Both eyes are affected in only 10-15% of cases, and this frequently concerns an autosomally dominant hereditary disease. Biomicroscopically ODP is a rounded or vertically oval calicyform or crater-like indentation of yellowish-white, grey or black colour (fig. 6b). It is most often localised at the temporal edge of the disc, with adjacent peripapillary atrophy and pigment shifts, but may be localised in any part of the disc. During the course of life (most often in the 2nd to 3rd decade) a decrease of visual acuity (VA) occurs in approximately 25-75% of patients with ODP as a consequence of the inception of macular retinoschisis of the external (RSE) and/or internal layer of the retina (RSI), degenerative processes in the outer layers of the retina and retinal pigment epithelium, and secondary retinal detachment with and/or without the presence of subretinal fluid (SF) (21, 22). The etiopathogenesis of maculopathy, like the origin of intraretinal or SF, is not entirely known. A liquified vitreous body may infiltrate into the ODP upon partial detachment of the posterior vitreous membrane, or this may concern cerebrospinal fluid from the subarachnoid space (7). Fluid may also be produced by the Bruch's membrane or retinal pigment epithelium. In the majority of cases of maculopathy with ODP, posterior vitreous detachment (PVD) does not occur. It is expected that pars plana vitrectomy (PPV) with surgical PVD is an effective treatment of maculopathy upon ODP (1, 9, 6, 4, 15).
METHOD
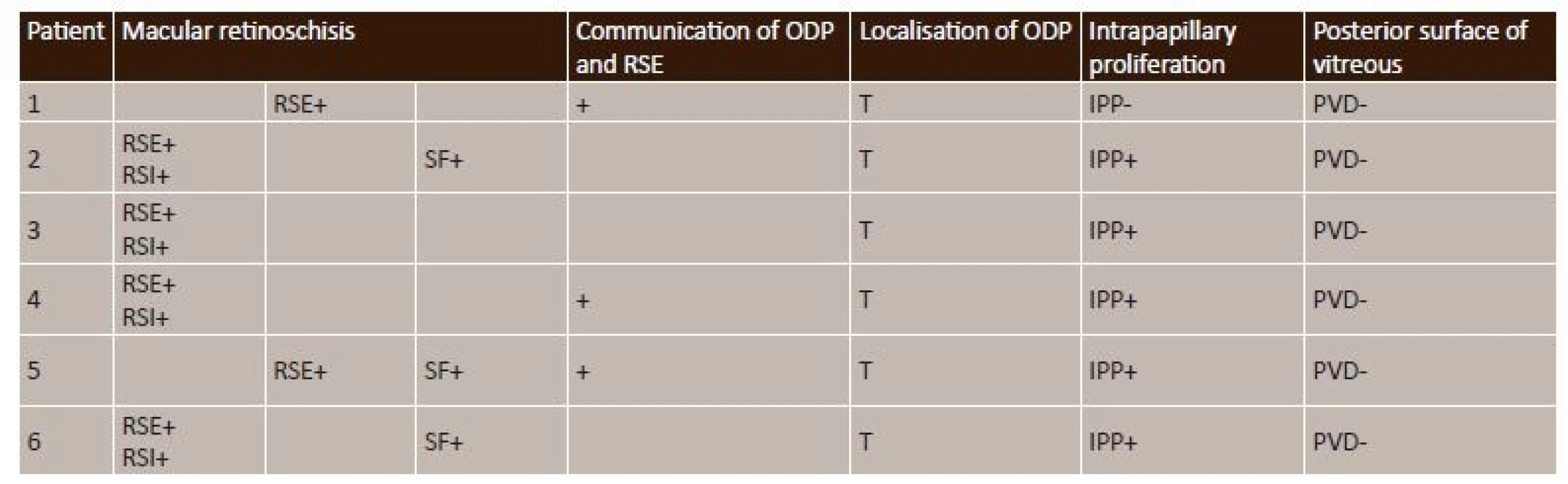
A retrospective study included 6 eyes of 6 patients (3 women and 3 men) with a unilateral finding of ODP with maculopathy. We excluded a patient with only ODP without maculopathy from the cohort. The patients were observed during the period of 2008-2017, the average age of the patients at the time of the first examination was 40.3 years (15-70 years). The period of duration of deterioration of VA was from two days to several years. In all patients we examined VA according to ETDRS optotypes, we performed a biomicroscopic examination on a slit lamp and examination of the fundus in artificial mydriasis with the aid of non-contact VOLK Super Field lenses 90D and 60D, and we documented the condition of the retina photographically (table 1). Upon an evaluation of the findings by optical coherence tomography (OCT/ SLO OTI, OCT Spectralis Heidelberg Engineering), we focused both on configuration of the papilla of the optic nerve and on the presence of glial tissue and/or condensation of the vitreous body in ODP, as well as on OCT of the characteristics of maculopathy. These covered communication of macular retinoschisis with ODP, the presence of macular RSE and/or RSI, a finding of SF and the condition of the vitreoretinal interface (table 2). In 4 eyes, 23-G three-port non-suture PPV was performed with active ablation of the posterior hyaloid membrane. For visualisation of the structures of the vitreous body we used 0.15% trypan blue (MembraneBlue, D.O.R.C. International, Rotterdam, the Netherlands) or a suspension of Triamcinolone acetonide (40 mg). We completed the operation with temporary internal gas tamponade of the retina by perfluoropropane (16% C3F8). In 2 operated eyes (patient no. 2, patient no. 4), a tissue sample was taken perioperatively from the region of the ODP and sent for a histopathological examination. After the operation the patients maintained a prone position for 2 days. We did not perform laser photocoagulation of the temporal edge of the papilla or peeling of the internal limiting membrane (ILM). We did not operate on two of the patients, namely a 54-year-old man with a deterioration of VA persisting for several years and a 70-year-old woman who came for an examination at the emergency outpatient Ophthalmology Clinic during the course of a temporary residence in the Czech Republic, and returned back abroad.
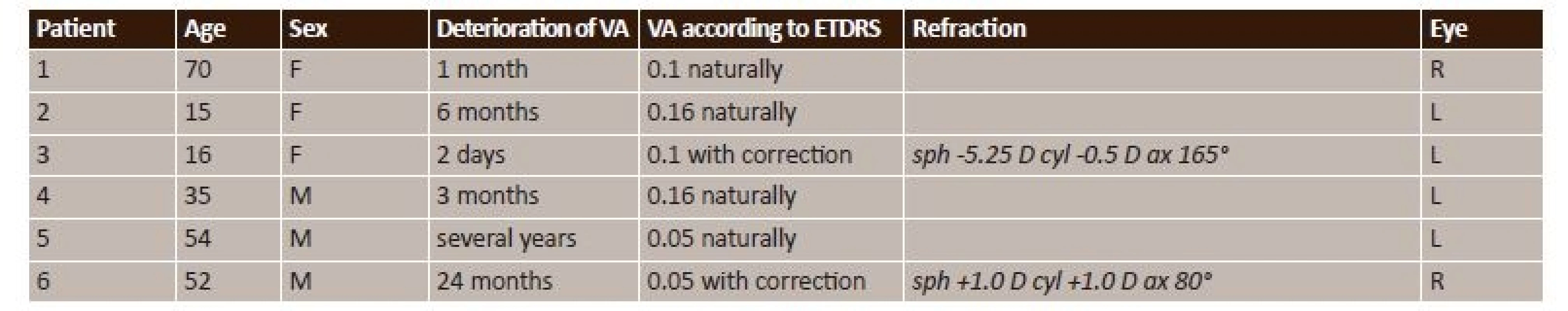
RESULTS
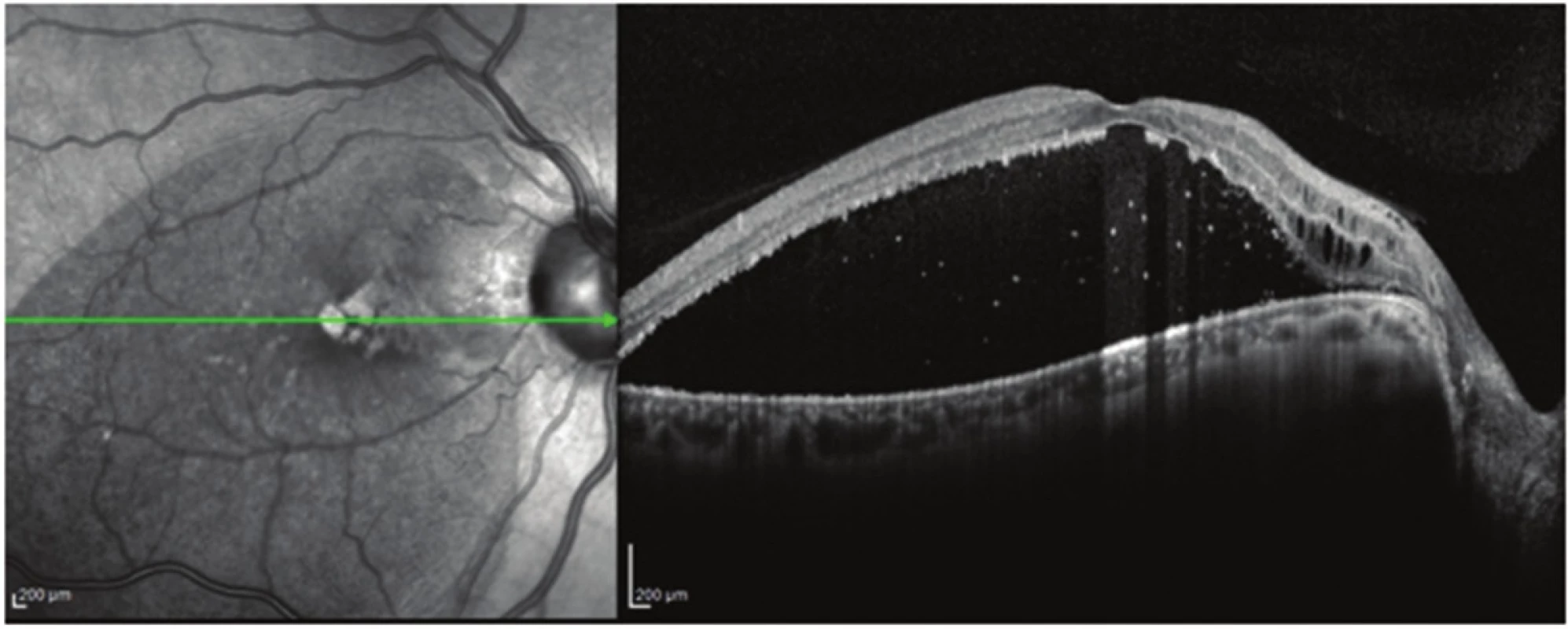
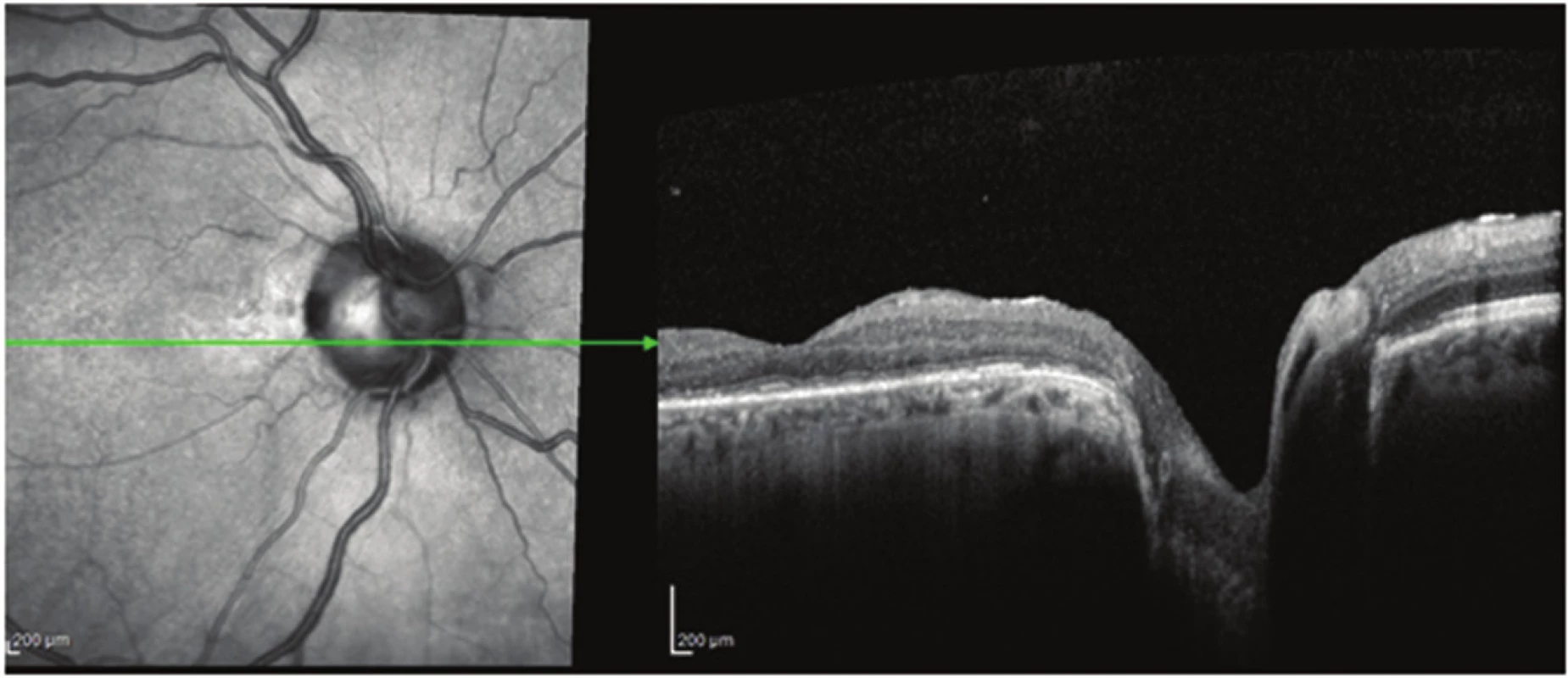
The clinical characteristics and findings of OCT in all patients in the observed study are presented in tables 1 and 2. The average age of the patients in the entire cohort was 40.3 years (15-70 years), the average age of the operated patients was 29.5 years (15-52 years). Average VA of the entire observed group upon the initial examination was 0.10 (range from 0.05 to 0.16). We operated on 4 out of the 6 observed eyes (67%). Average preoperative VA was 0.11 (range from 0.05 to 0.16). All victrectomated eyes were phakic, towards the end of the observation period one patient (no. 6) underwent cataract surgery with implantation of an intraocular lens due to the development of a postoperative nuclear cataract. The indication for cataract surgery was a symptomatic deterioration of VA. The OCT finding confirmed macular RSE in only 2 eyes, combined in one eye with the presence of SF. In all 4 eyes indicated for PPV we demonstrated macular RSE and RSI according to OCT, and in 2 eyes SF was also present (fig. 1). Macular detachment with the presence of SF occurred in 50% of eyes in our cohort. We determined communication of ODP with macular RSE in one operated eye and 2 non-operated eyes. Intrapapillary proliferation (IPP) was present in 5 out of 6 eyes in the observed cohort and in all vitrectomated eyes. Perioperatively removed proliferation from the ODP in 2 eyes was immediately fixed in 2.5% glutaraldehyde and sent for further processing by electron microscope. In patient no. 2 the histological examination of the taken sample in semi-thin slices confirmed a short streak with sparse composition, in ultra-thin slices composed partially of homogeneous, partially of hinted polygonal fine crystalline structures, probably of hyaluronate, and residues of collagen fibrils. In patient no. 4, the taken tissue was formed by sparse collagen ligament permeated by cells of a fibrohistiocytic nature.
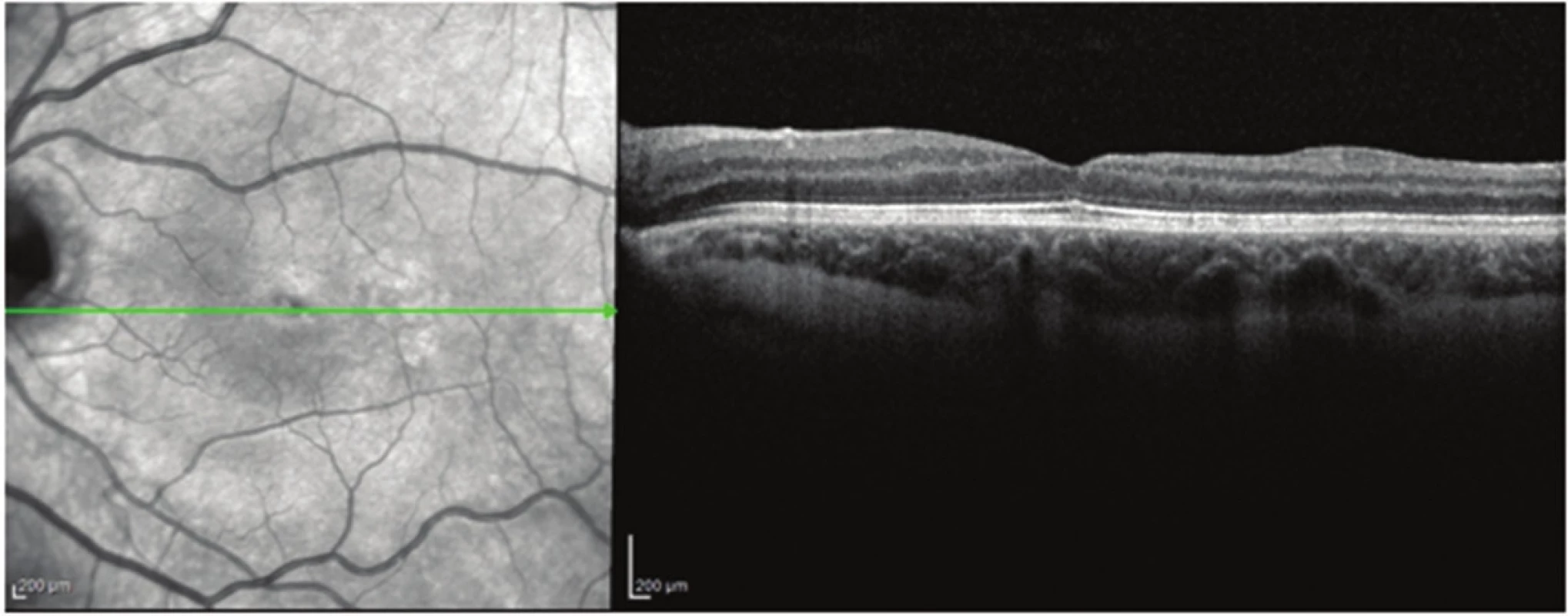
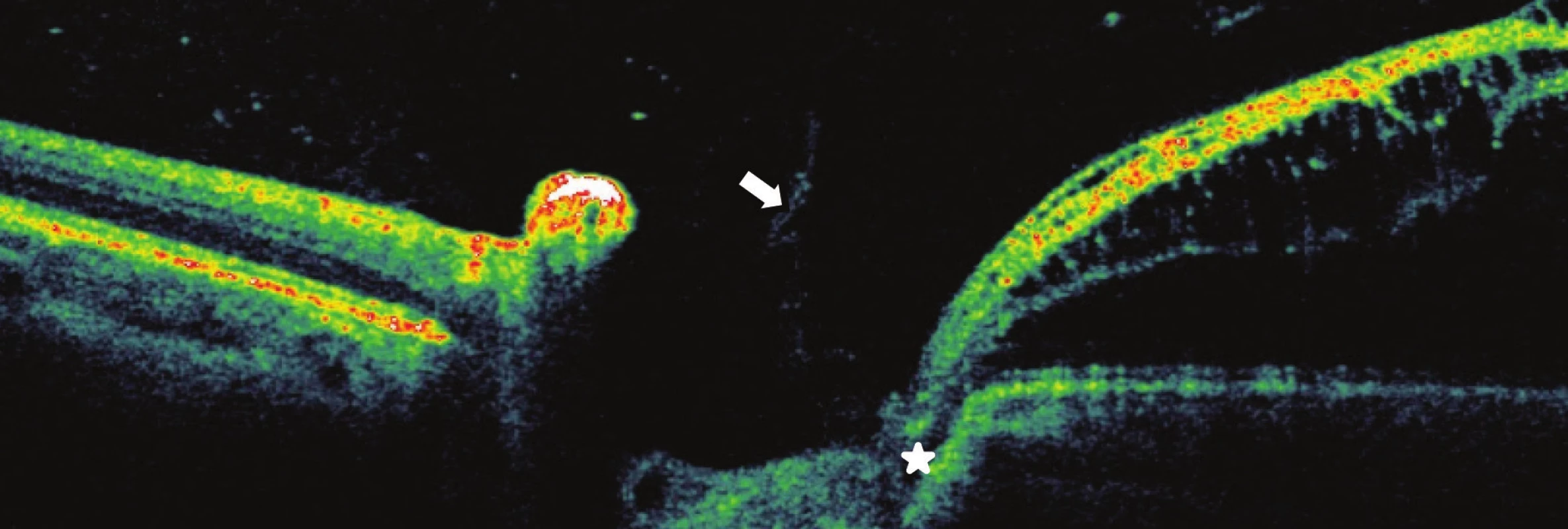
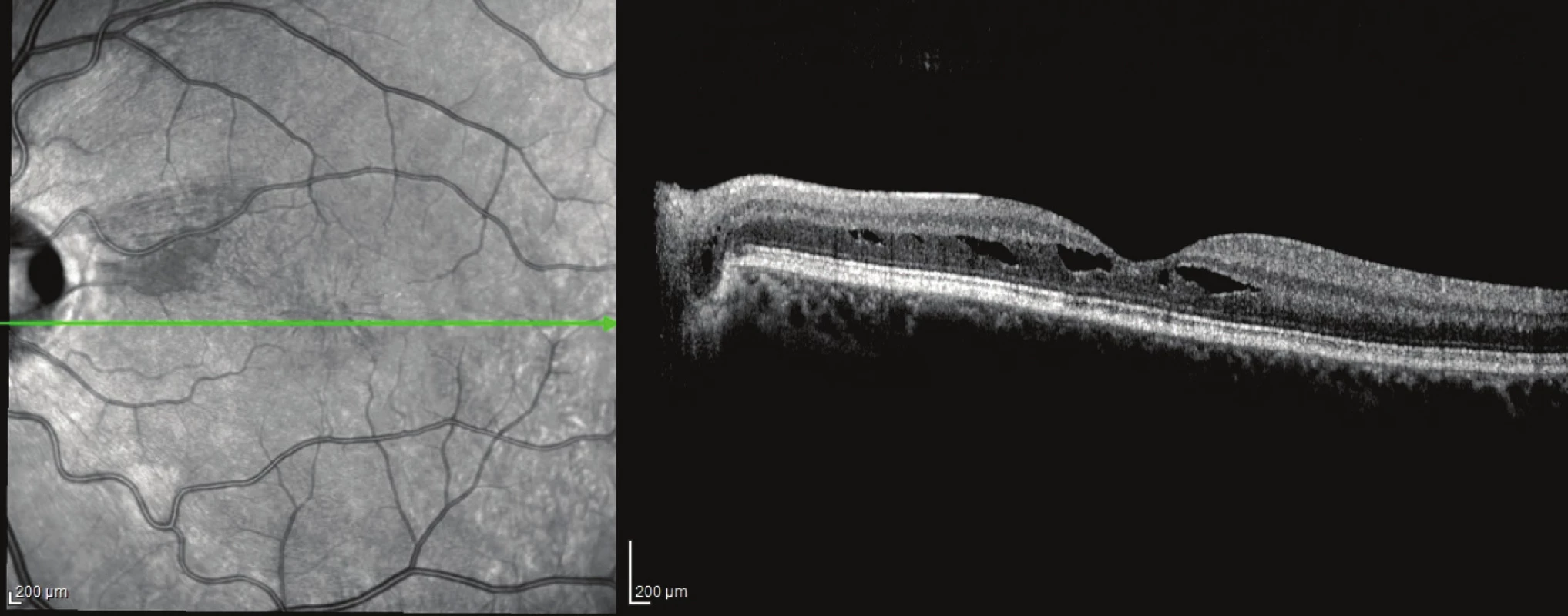
In 4 operated eyes with RSE and RSI we achieved an improvement of the anatomical finding in the macula in the postoperative period. After resorption of SF the subfoveolar detachment was reattached (fig. 2 and 3). In the case of one patient with communication of ODP with RSE, this connection was closed in the postoperative period (fig. 3 and 4). VA improved in all eyes from an average value of 0.11 to an average final value of VA 0.5 (range from 0.25 to 0.63), the average gain of letters was +30 (range from +10 to + 45), (table 3). The average observation period after surgery was 59 months (36-96 months), (table 3).
DISCUSSION
At present, despite significant advances in display methods, it is still not clear in which layer of the retina, external or internal, the initial schismatic changes occur. In 1988, Lincoff et al. presumed that macular detachment in ODP was of a bilaminar structure, exceptional in comparison with other retinal detachments. The authors were also of the opinion that fluid first of all accumulates in the layer of nerve fibres and subsequently gradually infiltrates to the retinal neuroepithelium via a preformed defect between the internal and external layers of the retina (12). In our cohort we diagnosed an external lamellar defect with macular detachment (fig. 6a) in one eye. Recent studies on ODP with the use of OCT have confirmed the presence of macular retinoschisis followed by macular detachment (18, 16, 11, 8).


Moon et al. (2006) recorded macular retinoschisis only in the external layers of the retina (14). We determined this finding in two of our patients, in one of whom RSE was complicated by the presence of SF with a manifest preformed defect between the external layer of the retina and the subretinal space (fig. 7a, b). The authors further pointed also to the possibility of penetration of fluid from ODP directly into the subretinal space. Maertz et al. (2017) also documented in four eyes out of a cohort of 16 eyes with SF and PP, observed with the aid of SD-EDI-OCT, a hyporeflexive space with a structure similar to meshwork, which was connected with the wall of the ODP (13). In our cohort of 6 patients we recorded communication of ODP with RSE in 2 eyes and with RSE and RSI in one eye.


In 5 out of 6 (83%) observed patients in our cohort, we demonstrated and in all operated eyes we confirmed the presence of glial tissue and/or condensation of the vitreous body in ODP, which correlates with the observation of Gregory-Roberts, which states an incidence of 89% (2). The fibrous tissue in the region of the optic nerve may be a residue of the Bergmeister's papilla (astrocytes which proliferated around the hyaloid artery during the course of the 12th week of gestation and which did not sufficiently regress), or may concern glial tissue independent of the vascular system of the hyaloid artery (2). Histology of samples of IPP taken in 2 eyes from our cohort during PPV demonstrated collagen fibrils and sparse collagen ligament with cells of a fibrohistiocytic nature. We expect that in future an analysis of this tissue will be conducted on a larger set of samples. Despite the fact that the pathogenesis of the origin of maculopathy in the case of ODP is not unequivocally clarified, it is presumed that the present glial tissue and/or condensation of the vitreous body in the optic disc pit (1, 2) contributes in a certain extent to the generation of serous retinal detachment and/or macular schisis. In our cohort, we removed IPP in all the operated eyes.
Haruta et al. (2012) are of the opinion that PPV is more effective in eyes with a non-detached posterior surface of the vitreous body than in those in which the posterior surface of the vitreous body is already detached (3). Active PVD, further assisted by intravitreally administered Triamcinolone, removes vitreomacular traction as one of the possible causes of macular retinoschisis. Hirakata et al., in two studies published in 2005, explain the origin of macular retinoschisis by means of a process in which the contraction of vitreous fibrils raises the fibroproliferative tissue from the ODP and fluid subsequently infiltrates from the ODP into the internal layers of the retina (5, 6). In the patients in our cohort who underwent PPV, we did not perform ILM peeling perioperatively. Opinions on ILM peeling in eyes with macular retinoschisis in the case of ODP are not entirely uniform. Shukla et al. (2012) attained very good surgical results in 7 patients with ODP, macular retinoschisis and central external retinal dihiscence following PPV with ILM peeling, despite the possible occurrence of macular hole throughout the full thickness, which occurred in 57,1% of eyes one month after PPV (17). Kim et al. (2012) recommend ILM peeling especially in eyes with posterior vitreous detachment, in which residues of the cortical vitreous body remain on the surface of the retina, together with vitreous cellular detritus (10). We agree with the opinion of Rayat et al. (2015), who do not consider ILM peeling to be essential in primary surgery, and are of the view that active PVD may be sufficient (15). In the view of the authors, ILM peeling is appropriate if repeated PPV is performed in the case of primary anatomic failure, in order to attain further limitation of macular traction. All the operated patients in our cohort had a temporary internal gas tamponade of the retina by perfluoropropane (16% C3F8). Intraocular gas tamponade together with positioning of the patient's head contributes to pneumatic relocation of the fluid extramacularly, and renewal of the function of the haematoretinal barrier, especially of the retinal pigment epithelium (20, 9).
CONCLUSION
Spectral OCT demonstrates the variability of the morphology of maculopathy. Vitreomacular traction of glial tissue and/or condensed vitreous body in ODP combined with a non-detached posterior hyaloid artery may be one of the factors influencing the origin of macular retinoschisis and/or secondary serous macular detachment. Complete detachment of the vitreous body from the papilla of the optic nerve and the macula is an effective surgical treatment, which leads to the successful reattachment of macular retinoschisis and improvement of the function of the eye.
Thanks:
The authors thank professor MUDr. (M.D.) Jaroslava Dušková, CSc., FIAC from the Institute of Pathology of the 1st Medical Faculty of the Charles University and the General University Hospital in Prague for processing and evaluating the histological examination of tissue samples.
MUDr. Magdalena Kováčová
Oční klinika 1. LF UK
U Nemocnice 2
128 08 Praha 2
magdalena.kovacova@lf1.cuni.cz
Sources
1. Barz-Schmidt, K.U., Heimann, K., Esser, P.: Vitrectomy for macular detachment associated with optic nerve pits. Int. Ophthalmology, 19; 1996 : 323–329.
2. Gregory-Roberts, E.M. , Mateo, C. ,Corcóstegui B. et al.: Optic dick pit morphology and Retinal detachment. Optical Coherence Tomography with Intraoperative Correlation. Retina, 33; 2013 : 363–370.
3. Haruta, M., Kamada, R., Umeno, Y.: Vitrectomy for optic disc pit-associated maculopathy with or without preoperative posterior vitreous detachment. Clin Ophthalmology, 6; 2012 : 1361–1364.
4. Hirakata, A., Inoue, M., Hiraoka, T. et al.: Vitrectomy without laser treatment or gas tamponade for macular detachmemnt associated with an optic disc pit. Ophthalmology, 119; 2012 : 810–818.
5. Hirakata, A., Hida, T., Ogasawara, A. et al.: Multilayered retinoschisis associated with optic disc pit, Jpn J Ophthalmol,49; 2005 : 414–416.
6. Hirakata, A., Okada, AA., Hida, T. et al.: Long-term results of vitrectomy without laser treatment for macular detachment associated with an optic disc pit. Ophthalmology, 112; 2005 : 1430–1435.
7. Christoforidis, J.B., Terrell, W. , Davidorf, F.H.: Histopathology of optic nerve pit - associated macolopathy. Clin Ophthalmol, 6; 2012 : 1169–1174.
8. Imamura, Y., Zweifel, S.A., Fujiwara, T. et al.: High-resolution optical coherence tomography findings in optic pit maculopathy. Retina, 30; 2010 : 1104–1112.
9. Kalvodová, B., Říčařová, R., Kuthan, P. et al.: Vitrektomie u jamky terče zrakového nervu s makulopatií. Čs. Oftal., 55; 1999 : 123–127.
10. Kim, KS, Lee, SB, Lee, WK.: Vitrectomy and internal limiting membrane peeling with and without gas tamponade for myopic foveoschisis. Am J Ophthalmol, 153; 2012 : 320–326.
11. Krivoy, D., Gentile, R., Liebmann, J.M. et al.: Imaging congenital optic disc pits and associated maculopathy using optical coherence tomography. Arch. Ophthalmol, 114; 1996 : 165–170.
12. Lincoff, H., Lopez, R., Kreissig, I. et al.: Retinoschisis associated with optic nerve pits. Arch Ophthalmol, 106; 1988 : 61–67.
13. Maertz, J., Mohler, K., Kolb, J.P. et al.: Intrapapillary proliferation in optic disk pits. Retina, 37; 2017 : 906–914.
14. Moon, S, Kim, J, Spaide, R: Optic pit maculopathy without inner retinal schisis cavity. Retina, 26; 2006 : 113–116.
15. Rayat, J.S., Rudnisky, CH. J., Waite, Ch. et al.: Long term outcomes for optic disk pit maculopathy after vitrectomy. Retina, 35; 2015 : 2011–2017.
16. Rupak, R.,Waanbah, A.D., Mathur, G. et al.: Optical Coherence Tomography characteristics in eyes with optic pit macolopathy. Retina, 33; 2013 : 771–774.
17. Shukla, D., Kalliath, J., Tandon, M. et al.: Vitrectomy for optic disk pit with macular schisis and outer retinal dehiscence. Retina, 32; 2012 : 1337–1342.
18. Sobol, W. M., Blodi, C.F., Weingeist, T.A. et al.: Long – term visual outcome in patients with optic nerve pit and serous retinal detachment of the macula. Ophthalmology, 97; 1990 : 1539–1542.
19. Tittler, E.H. , Khaderi, K.R., Sadun, A.A.: Optic Disc Pitting and Associated Serous Macular Detachment. http://www.retinalphysician.com/issues/2010/nov-dec/optic-disc-pitting-and-associated-serous-macular-detachment
20. Travassos, A.S., Regadas, I., Alfaiate, M. et al.: Optic pit: novel surgical management of complicated cases. Retina, 2013; 33 : 1708–1714.
21. Tzu, J.H., Flynn, H.W., Berrocal, A.M. et al.: Clinical manifestations of optic pit maculopathy as demonstrated by spectral domain optical coherence to mography. Clin Ophthalmol, 7; 2013 : 167–172.
22. Young R. C., Tzu, J.H., Flynn H.W.: Optic Pit Maculopathy: Where Is the Fluid? Retinal Physician, 10; 2013 : 52–55.
Labels
OphthalmologyArticle was published in
Czech and Slovak Ophthalmology

2017 Issue 5-6
-
All articles in this issue
- OCT Findings and Long-term Follow-up Results of Vitrectomy in Patients with Optic Disc Pit and Associated Maculopathy
- PERSISTENT HYALOID ARTERY – PERFORM A SURGERY OR NOT?
- Combination of Intravitreal Corticosteroid with Anti-vegf in Macular Edema Secondary to Retinal Vein Occlusion
- Sarkoidosis and its Eye Ocular Manifestation (an Analysis of Six Case Report)
- Results of Treatment of Diabetic Retinopathy by the Laser System PASCAL
- Ciliary body melanoma treatment by stereotactic radiosurgery
- The treatment results in patients with lmphoma disease in the orbit
- The Difference between Ganglion Cell Complex and Nerve Fiber Layer in the Same Altitudinal Halves of the Retina in Hyper-tension and Normal-tension Glaucomas
- Xerosis in Patient with Vitamin A Deficiency – a Case Report
- Recommended procedure for eye examination for infants and children of pre-school age in regular outpatient practice
- Czech and Slovak Ophthalmology
- Journal archive
- Current issue
- About the journal
Most read in this issue
- Sarkoidosis and its Eye Ocular Manifestation (an Analysis of Six Case Report)
- Recommended procedure for eye examination for infants and children of pre-school age in regular outpatient practice
- PERSISTENT HYALOID ARTERY – PERFORM A SURGERY OR NOT?
- The treatment results in patients with lmphoma disease in the orbit

