Xerosis in Patient with Vitamin A Deficiency – a Case Report
Authors:
A. Kopecký 1,2,3
; F. Benda 1,2; J. Němčanský 1,2
Authors‘ workplace:
Oční klinika, FN Ostrava, Ostrava
1; Lékařská fakulta OU, Ostrava
2; 1. LF Univerzity Karlovy v Praze, Praha
3
Published in:
Čes. a slov. Oftal., 73, 2017, No. 5-6, p. 222-224
Category:
Case Report
Overview
Xerosis is a corneal and ocular surface disease caused by vitamin A deficiency. It is a rare disease in developed countries, but in third world countries it is a common cause of blindness. We describe a typical xerosis in patient with vitamin A deficiency and long-term malnutrition and alcoholism in our case. In spite of initially serious presentation of the disease, the patient’s response to treatment was prompt and there was complete regression of the disease.
Key words:
xerosis, vitamin A deficiency
INTRODUCTION
Vitamin A ranks among the vitamins soluble in fat. Its function is of key importance in the visual cycle of the retinal pigment epithelium. On the surface of the eye it has a key function in the growth of the epithelium and differentiation of the limbal cells (4). Natural sources of vitamin A are e.g. fish oil, leafy vegetables, carrots or apricots, while the foods richest in vitamin A include cod liver oil and beef or turkey liver (12).
Xerosis upon a background of vitamin A deficiency is a rare phenomenon in economically developed countries, since it is mostly linked with malnutrition of the patient. Another possibility is the occurrence of a deficiency upon a malfunction of fat absorption, for example in cystic fibrosis (3). The first ophthalmological symptom is “nyctalopia”, a disorder of vision in twilight, followed by xerophthalmia – a pronounced “drying” of the anterior segment. If the patient's diet is not improved, however, the pathology may progress as far as to severe keratomalacia with perforation (8). A specific and rare finding is then “xerophthalmic fundus”, with yellowish stains on the periphery of the ocular fundus (7). General manifestations may be pruritus, anaemia or follicular hyperkeratosis (5).
Pathophysiologically, disorders of vision in twilight originate due to a progressive inhibition of the synthesis of rhodopsin. A deficiency of vitamin A also afflicts the cup cells of the conjunctiva and the holocrine glands producing mucin, a deficiency of which leads to the development of severe dry eye syndrome and its subsequent complications (3).
In addition to dry eye syndrome, the patient is also at risk of local infectious inflammations. Subjective complaints are frequently masked by reduced sensitivity of the damaged cornea.
EPIDEMIOLOGY
Summary data on this issue does not exist for the Czech Republic, we consider the pathology to be rare in our region. By contrast, in Third World countries malnutrition and connected vitamin A deficiency is one of the prominent factors in the origin of blindness, above all in childhood. Various sources state the deficiency of vitamin A, either in clinical or subclinical form, is a problem in approximately 75 countries of the world, in which approximately 250 million children worldwide are endangered due to complications resulting from an insufficiency of the entire spectrum of vitamins (9). Every year an estimated 20-100 thousand persons go blind as a result of complications due to vitamin A deficiency. The most affected are the regions of sub-Saharan Africa and South Asia (11). With regard to the fact that in the regions in question this mostly does not concern isolated deficiencies of only one vitamin, the insufficiency is also linked with a high rate of morbidity and mortality (6).
CASE REPORT
A 55-year-old female patient reported to our outpatient department in an acute condition, stating deterioration of vision in the right eye. From her personal anamnesis we determined that the patient was a socially deprived person, dependent on alcohol and living in a shelter for the homeless. She had been treated within the framework of institutional emergency care approximately one month before reporting to us, when suspicion of severe dry eye syndrome was stated, incipient white dot syndrome was determined in the left eye, and in addition to therapy with artificial tears, intensive observation at our centre was recommended. The patient did not report for any of the originally recommended follow-up examinations.
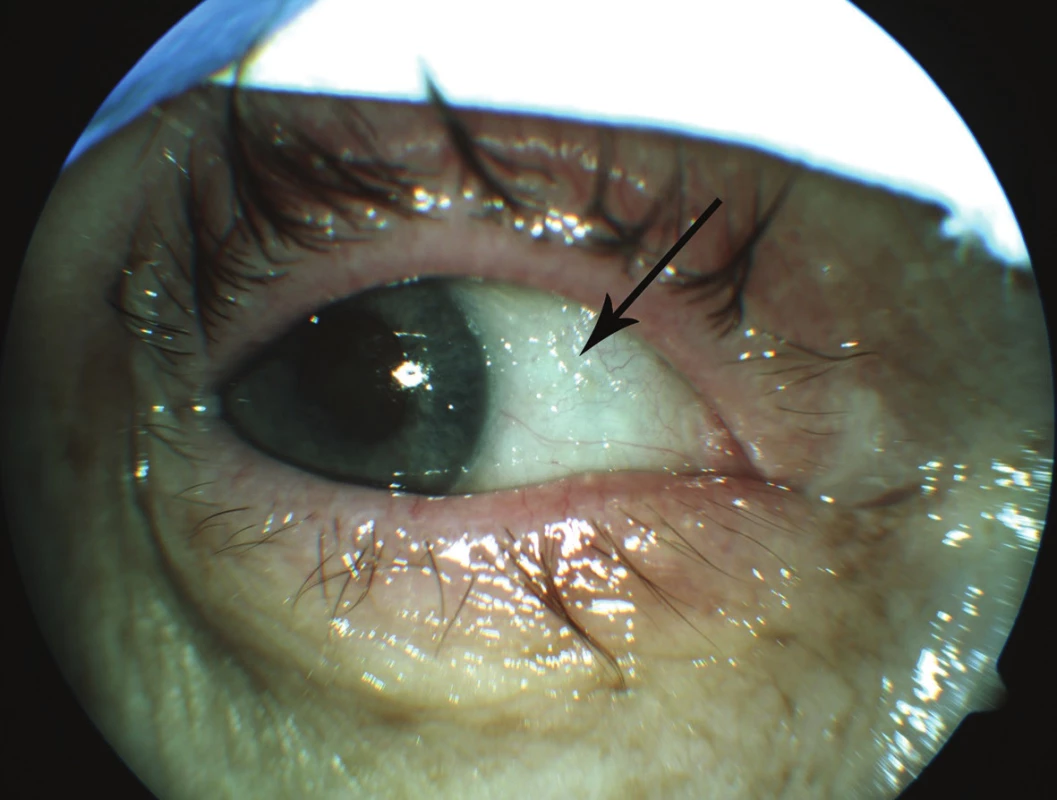
Other than deterioration of vision in the right eye, the patient did not state any complaints. Best corrected visual acuity in the right eye was 1.5 metres, in the left eye questionably without light perception. In the right eye there was a typical finding of xerophthalmia, including Bitot's spots (fig. 1), keratinisation and severe dry eye syndrome, in the left eye we found extensive perforation of the cornea by the tamponaded iris, anterior chamber with hyphaema (fig. 2).
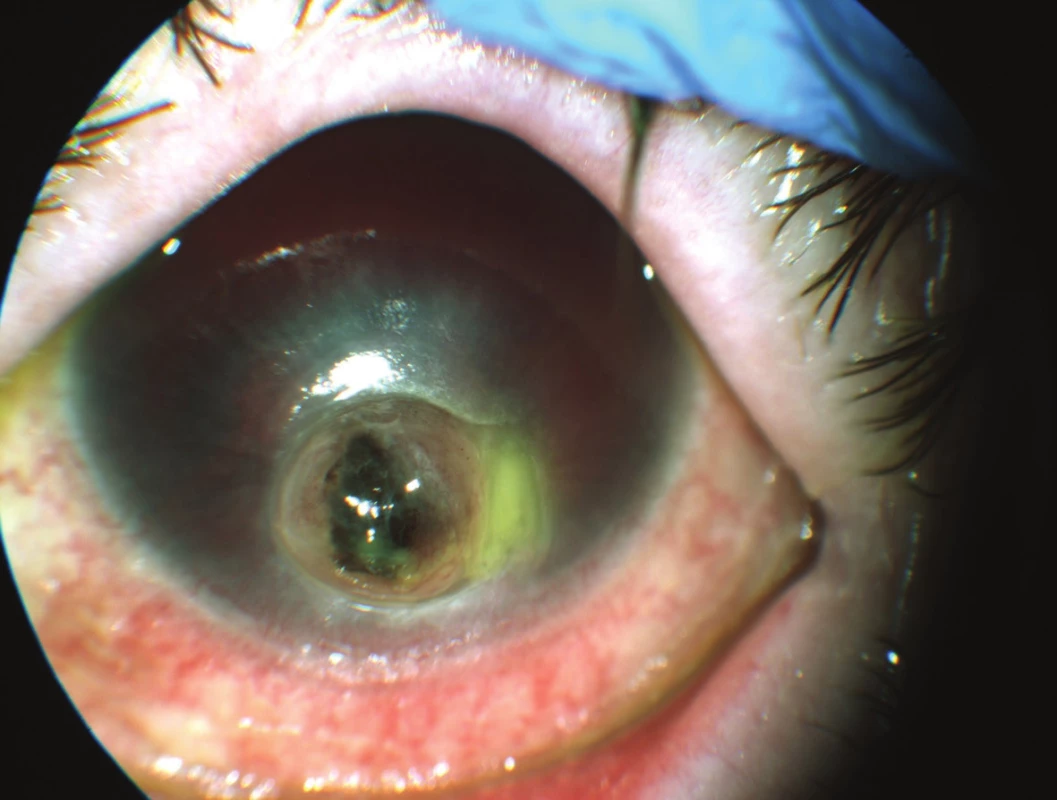
Due to the severity of the finding, the patient was admitted for therapy in hospitalisation, and for a general full examination at our inpatient department – internal specialist examination and blood tests. The blood samples confirmed general malnutrition and vitamin A deficiency (the resulting level was beneath 0.10 µmol/l, the norm value according to the laboratory is 1.05-2.80 µmol/l), and the patient herself stated that for more than a year she had “been on a diet of only rice, bread rolls and occasional alcohol”. Artificial tears were intensively applied to the patient locally, generally she was administered vitamin A – according to the recommended dosage (vitamin A in the form of drops per os – daily dose 100 000 IU). Due to the ominous finding in the left eye, evisceration of the eyeball was first of all considered. On the second day of hospitalisation, following a slight improvement of the local finding, we eventually decided to proceed with a conserving operation. Due to the very poor quality corneal stroma in the left eye, the affected surroundings of the perforation and its unclear edges, as well as the contraindication of general anaesthesia on the part of the internal specialist, we acceded to suturing of an autologous scleral graft ipsilaterally, for the purpose of closing the extensive corneal defect and restoring the integrity of the eyeball, with a potential view to further surgical reconstruction.
The patient was progressively given a thorough general examination, including internal specialist examination, in which thrombophlebitis of the lower limbs, of which there was suspicion shortly after her admittance, was excluded. Following consultation with a haematologist, the patient was administered two transfusions of erythrocytes for anaemia.
During hospitalisation the patient's general condition improved, and there was also a marked improvement in the local finding in the right eye. In the left eye the postoperative course was without complications, the graft was without signs of rejection or infection, with good toning of the left eyeball.
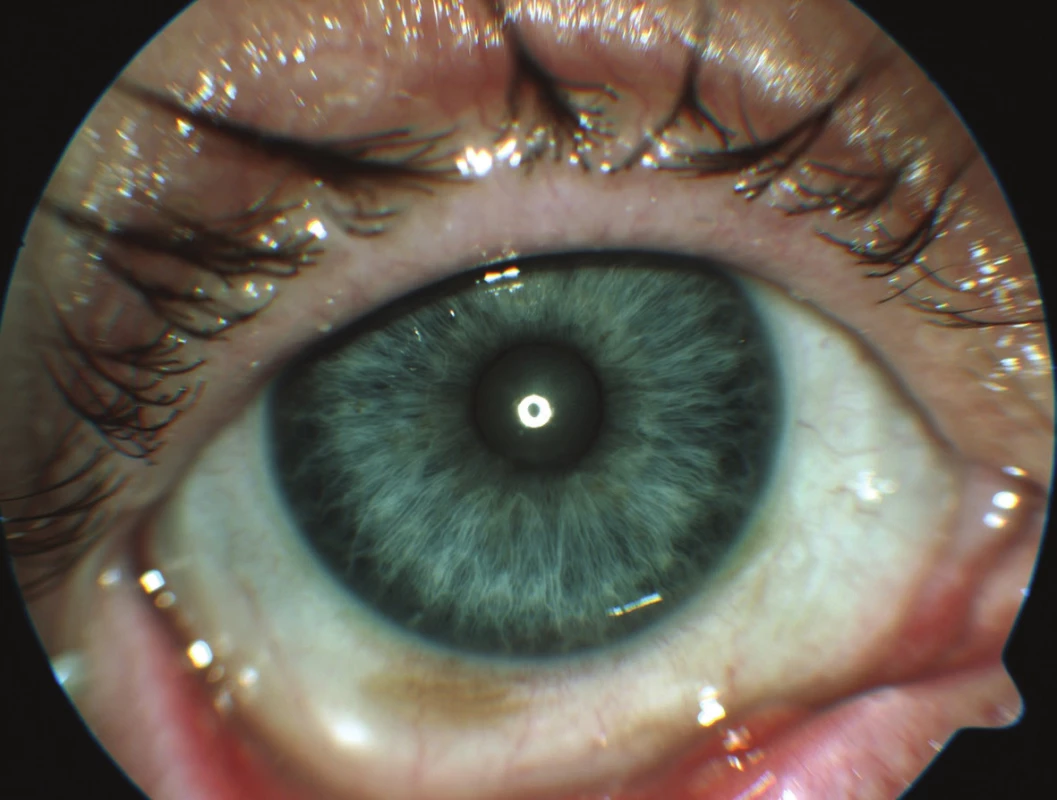
After one week the patient was transferred to a sanatorium for the long-term sick, with a plan for further regular follow-up examinations at our centre. At a follow-up after two weeks, vision in the right eye naturally was 6/18, best corrected visual acuity 6/9, the local finding was markedly improved (fig. 3), in the left eye the postoperative finding was stable, vision 30 cm movement, light perception with unclear projection.
DISCUSSION
In developing countries, xerophthalmia is one of the most common causes of childhood blindness, which can be prevented by nutritional measures (1). Correspondingly, the largest number of studies on this theme relate to the regions of sub-Saharan Africa and South Asia. In developing countries, supplements with vitamin A are one of the main strategies of prevention of this disease (1). By contrast, in developed countries this is a relatively rare pathology, linked for example with cystic fibrosis (10). However, cases of disorder of twilight vision are described as a consequence of vitamin A deficiency in patients following a colon bypass (2). In general, it is possible to find many cases in the literature from developed countries describing xerosis in patients with malnutrition of various origin, even if cases occurring in connection with alcoholism are described more rarely. Nevertheless, long-term alcoholism is an unequivocally demonstrated risk of vitamin A deficiency, with subsequent development of xerosis (13).
CONCLUSION
In our geographical conditions, xerosis is a rare disease. The diagnosis is determined not only on the basis of the anamnesis and a typical finding on the anterior segment, but primarily must be confirmed by laboratory. It is important to be aware that local therapy (artificial tears, antibiotics prophylaxis) is only supportive, similarly as local therapy by retinoids, stated in some of the literature (7). The fundamental pillar of therapy is general treatment with vitamin A (recommended dose 100 000 IU/day in the case of keratomalacia), accompanied by full examination of the general condition and ideally change of dietary habits and lifestyle (7).
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company.
MUDr. Adam Kopecký
Oční klinika FN
708 52 Ostrava-Poruba
E-mail: adam.kopecky@fno.cz
Sources
1. Akhtar, S., Ahmed, A., Randhawa, M. A., et al.: Prevalence of Vitamin A Deficiency in South Asia: Causes, Outcomes, and Possible Remedies. J Health Popul Nutr. 31(4); 2013 : 413–423.
2. AlHassany, A. A.: Night blindness due to vitamin A deficiency associated with copper deficiency myelopathy secondary to bowel bypass surgery. BMJ Case Rep. Březen 2014. Dostupné na WWW: < https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4009832/pdf/bcr-2013-202478.pdf >.
3. Cantor, L. B., Rapuano, C. J., Cioffi, G. A., et al.: Systemic Disorders with Corneal and Other Anterior Segment Manifestation. In Cantor, L. B., Rapuano, C. J., Cioffi, G. A., et al.: Basic and Clinical Science Course: External Disease and Cornea, San Francisco, American Academy of Ophthalmology, 2017, s. 196–197.
4. Chelala, E., Durani, A., Fadlallah, A., et al.: The role of topical vitamin A in promoting healing in surface refractive procedures: a prospective randomized controlled study. Clin Ophthalmol, 7; 2013 : 1913–1918.
5. Ganong, W. F.: Energetická bilance, metabolismus a výživa. In Ganong, W. F.: Přehled lékařské fyziologie. Praha, Galén, 2005, s. 320–322.
6. Humphrey, J. H., West, K P., Sommer, A.: Vitamin A deficiency and attributable mortality among under-5-year-olds. Bull World Health Organ. 70(2); 1992 : 225–232.
7. Kanski, J. J., Bowling, B.: Cornea. In Kanski, J. J., Bowling B.: Clinical Ophthalmology: A Systematic Approach, 7th Edition, Elsevier Sanders, 2011, s. 209–210
8. Kuchynka, P., et al.: Spojivka. In Kuchynka, P., et al.: Oční lékařství, 2. přepracované a doplněné vydání, Grada, 2016, s. 275.
9. Lee, V., Ahmed, F., Wada, S., et al.: Extent of vitamin A deficiency among rural pregnant women in Bangladesh. Public Health Nutr. 11(12); 2008 : 1326–31.
10. Rayner, R. J., Tyrrell, J. C., Hiller, E. J., et al.: Night blindness and conjunctival xerosis caused by vitamin A deficiency in patients with cystic fibrosis. Arch Dis Child. 64(8); 1989 : 1151–1156.
11. Reddy, V.: History of the International Vitamin A Consultative Group 1975-200. J Nutr. 132 (9Suppl.); 2002 : 2852–6.
12. Vitamin A. Fact Sheet for Healthcare Professional. National Institutes of Health. Dostupné na WWW: <https://ods.od.nih.gov/factsheets/VitaminA-HealthProfessional>.
13. You, Y. S., Qu, N. B., Yu, X. N.: Alcohol consumption and dry eye syndrome: a Meta-analysis. Int J Ophthalmology, 9(10); 2016 : 1487–1492.
Labels
OphthalmologyArticle was published in
Czech and Slovak Ophthalmology

2017 Issue 5-6
-
All articles in this issue
- OCT Findings and Long-term Follow-up Results of Vitrectomy in Patients with Optic Disc Pit and Associated Maculopathy
- PERSISTENT HYALOID ARTERY – PERFORM A SURGERY OR NOT?
- Combination of Intravitreal Corticosteroid with Anti-vegf in Macular Edema Secondary to Retinal Vein Occlusion
- Sarkoidosis and its Eye Ocular Manifestation (an Analysis of Six Case Report)
- Results of Treatment of Diabetic Retinopathy by the Laser System PASCAL
- Ciliary body melanoma treatment by stereotactic radiosurgery
- The treatment results in patients with lmphoma disease in the orbit
- The Difference between Ganglion Cell Complex and Nerve Fiber Layer in the Same Altitudinal Halves of the Retina in Hyper-tension and Normal-tension Glaucomas
- Xerosis in Patient with Vitamin A Deficiency – a Case Report
- Recommended procedure for eye examination for infants and children of pre-school age in regular outpatient practice
- Czech and Slovak Ophthalmology
- Journal archive
- Current issue
- About the journal
Most read in this issue
- Sarkoidosis and its Eye Ocular Manifestation (an Analysis of Six Case Report)
- Recommended procedure for eye examination for infants and children of pre-school age in regular outpatient practice
- PERSISTENT HYALOID ARTERY – PERFORM A SURGERY OR NOT?
- The treatment results in patients with lmphoma disease in the orbit

