PERSISTENT HYALOID ARTERY – PERFORM A SURGERY OR NOT?
Authors:
T. Řeháková; A. Stepanov; N. Jirásková
Authors‘ workplace:
Oční klinika Fakultní nemocnice Hradec Králové, přednostka prof. MUDr. Naďa Jirásková Ph. D., FEBO
Published in:
Čes. a slov. Oftal., 73, 2017, No. 5-6, p. 178-182
Category:
Original Article
Overview
The review points to the issues of persistent hyaloid artery, more precisely to possible clinical features, the influence on visual functions and potential complications during intraocular surgeries. In professional journals we can find just few reviews regarding this rare deviation of the eye development, therefore we want to present our experience.
The persistent hyaloid artery causes chronical local changes of eye background at both of our patients, retinal detachment and retinoschisis. The findings weren’t accompanied by significant decrease of visual functions or subjective patient’s complaints. Considering the potential complications published in journals such as hemoftalmus or retinal vessel occlusion we decided to be more conservative. That’s why we just checked-up the condition of the eye background and we were prepared to perform a surgery if necessary.
Key words:
persistent hyaloid artery, tractional retinal detachment, retinoschisis
INTRODUCTION
The hyaloid artery (HA), a branch of the primitive arteria ophthalmica, represents a transitional vascular system of the eye which ensures nutrition of the developing lens and posterior segment of the eye during its early embryonic development. It enters the eyeball in the place of the disc of the optic nerve (DON) between the 3rd (3, 5) and 4th (1, 6, 8) week of gestation and grows distally until it reaches the lens between the 4th and 5th week (3, 5), forming the tunica vasculosa lentis in the 9th to 11th week of intrauterine development (1, 6, 8). The natural development of the hyaloid vascular system also includes the complete regression of the distal part of the HA. This process commences in the 3rd month (8) of intrauterine development, and in the majority of individuals is completed before birth or shortly afterwards (1, 3, 5). The proximal part persists and changes into the central retinal artery (CRA) and central retinal vein (CRV) (3, 6).
The term “persistent hyaloid artery” (PHA) describes an anatomical residue of the impaired regression of the embryonic hyaloid system, in which its scope is very variable (6). It is most frequently manifested as a persistent trace of glial tissue by the DON, indicated as Bergmeister's papilla, more rarely we find fibrous residues on the posterior pole of the lens capsule, the Mittendorf dot. In rare cases it is possible to identify PHA in the form of a fibrotic strip throughout the entire range from the DON to the posterior lens capsule, and in entirely exceptional cases active blood flow is retained in the vessel even postnatally (1, 3, 5, 7, 8, 9, 11).
The severity of the condition fluctuates within a broad range from a random, asymptomatic finding, through intralenticular or vitreous haemorrhage and vitreoretinal traction of the posterior pole, to severe complications upon cataract surgery or upon simultaneous persistent hyperplastic primary vitreous body (PHPV), which is linked with a more pronounced developmental affliction of the visual system, including microphthalmos, nystagmus and severe damage to visual functions (9, 11).
Very few publications dealing with the issue of PHA appear in the literature, usually only individual case reports. The majority of authors concur that this concerns a rare developmental deviation of the eye, nevertheless within the framework of ocular anomalies it is relatively frequent (1, 2, 3, 9). It occurs in up to 3% of individuals born within the planned date (6, 8) and as many as 99% of prematurely born infants (8).
The aim of the article is to indicate the individual potential clinical manifestations of PHA, its influence on visual functions and above all the possible complications upon its surgical removal or during cataract surgery.
CASE REPORTS
In 2016, two female patients were referred by the district health centre to the Department of Ophthalmology at the University Hospital of Hradec Králové (UHHK) for consideration of the further procedure. Both patients complained of long-term progressive deterioration of vision and a feeling of pressure in their eyes. An examination of the ocular fundus in mydriasis detected preretinal fibrosis, in one case causing local tractional retinal detachment (TRD), and in the second case local retinoschisis.
First case report: A 15-year-old girl was referred to our centre by a district ophthalmologist for evaluation of the ocular finding following an attack by inmates of a children's home, in which she was repeatedly kicked in the head, primarily in the region of the right temple and forehead. The patient had already previously stated blurred vision bilaterally, nevertheless following the attack her vision deteriorated further. Intraocular pressure (IOP) measured by non-contact method was within the norm, in the right eye 17 torr and in the left eye 13 torr. Visual acuity (VA) evaluated with the aid of Snellen's optotypes was as follows: uncorrected visual acuity (UVA) in right eye 0.4, with correction -0.5cyl on an axis of 40° 0.8, in left eye UVA 0.8, not improved by correction. Upon examination on a slit lamp, the finding on the anterior segment was bilaterally physiological.
A biomicroscopic examination of the ocular fundus of the right eye (RE) in mydriasis demonstrated thinning of the retina in the upper quadrants and residues of PHA with fibrotic tissue binding to the upper temporal arcade (fig. 1), where local retinoschisis of an older date was present, and in the surrounding area there were evident holes in the internal layer of the neuroretina. The remaining part of the retina was lying. In the left eye (LE) the finding on the posterior segment was entirely physiological (fig. 2).


With regard to the good VA and the age of the patient, a surgical solution to the finding on the retina of the RE was not indicated. This also took into consideration the fact that it did not concern an acute finding in connection with the trauma that had occurred, but that the changes were congenital. Regular annual follow-up examinations with the district ophthalmologist were recommended in order to monitor the dynamic of the condition, including examination of the ocular fundus in mydriasis.
Second case report: The patient, a 35-year-old woman, reported to our clinic for a consultation concerning a surgical solution to a condition of the retina in the LE, which was recommended at another centre. Upon arrival she stated deterioration of vision in the LE persisting for approximately one year, in which she complained most of fatigue during work and a feeling of pressure in the LE. Anamnestically the patient is not being treated for any condition in the long term, and does not use pharmaceuticals regularly. She last underwent a complete eye examination approximately ten years ago, she does not wear glasses correction, but states the performance of laser treatment of the retina of the LE 15 years ago. UVA in the RE was 0.8, not improved by correction and UVA in the LE was 0.12, with correction +2.0sf / -1.0cyl / 100° 0.6 paracentrally, IOP measured by non-contact within the norm, in RE 19 torr and in LE 16 torr.
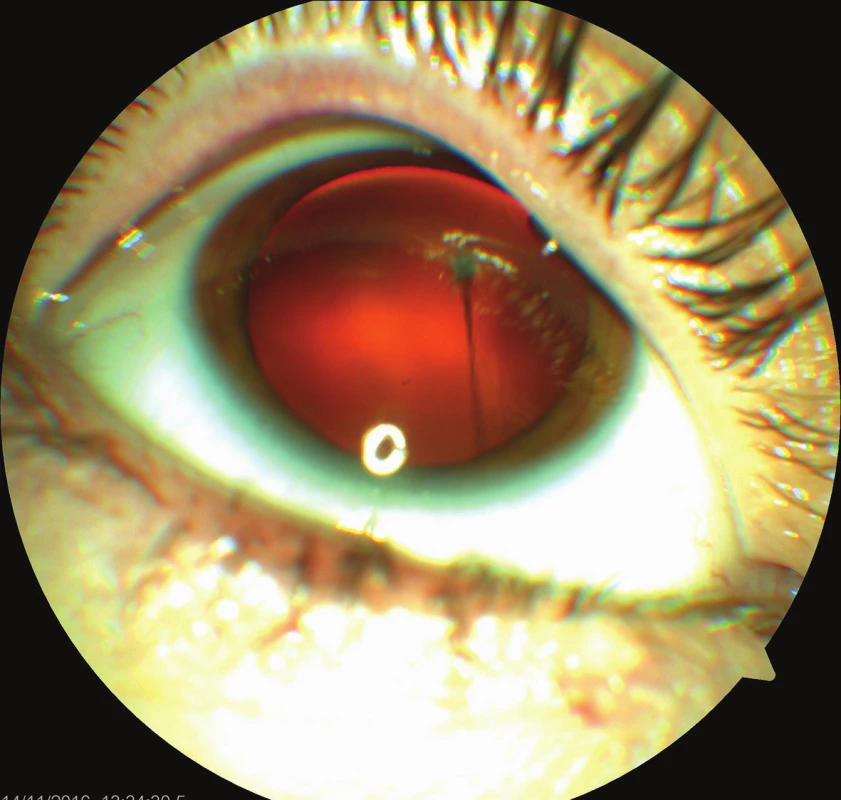
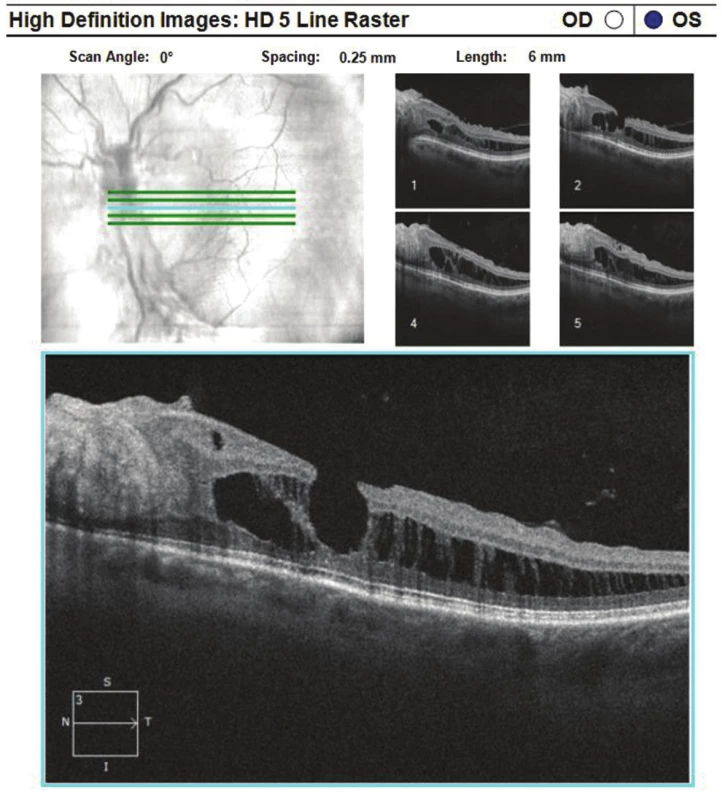
Examination of the anterior segment on a slit lamp revealed PHA of the RE with an attachment of the distal segment to the posterior capsule of the lens (fig. 3), also physiological finding on the RE as well as LE. Fundoscopy in mydriasis of the RE demonstrated a proximal part of the PHA adhering to the upper temporal arcade, where it conditioned the origin of local TRD of an older date (fig. 4), in the surrounding area there were evident laser traces, otherwise the retina was without deposit changes, attached. On the ocular fundus of the LE there was manifest preretinal fibrosis, causing draping of the retina in the central landscape (CL), where a lamellar defect of the neuroretina was also evident, otherwise the finding on the retina was within the norm (fig. 5). In the LE an examination was concurrently performed with the aid of optical coherence tomography, which confirmed a separation of the retinal layers in the lower temporal arcade with epiretinal fibrosis, including a defect of the lamellar layers of the retina (fig. 6).


With regard to the fact that this concerned the first examination at our centre, monitoring within the district and at the vitreoretinal clinic of UHHK was recommended, for the purpose of observing the finding on the retina of the LE over time, with consideration of a surgical solution if required according to the development of the condition. The finding on the retina of the RE was not indicated for a surgical solution due to good vision and the absence of subjective complaints on the part of the patient.
DISCUSSION
The presence of PHA postnatally is the result of a disorder of regression of the transitional embryonic hyaloid system of the eye. To date, the mechanism triggering atrophisation of the now obsolete HA has not been entirely clarified. It is assumed that cells related to macrophages are responsible for this process, but direct evidence of their active role is not yet available. Taniguchi et al. (10) attempted to answer this question in their study of longitudinal cross-sections in the optical axis of the eye in 1, 5, 10 and 20 day old rats, which they subsequently subjected to both immuno-histochemical examination techniques and observation under an optical and electron microscope. Their results suggest that macrophages clear away apoptotic cells and furthermore have an important role in the early phase of regression of the HA. And in this phase they have the capacity to induce apoptosis in capillary cells, the result of which is a disordered structure of the vessel, with its constriction and the restriction of blood flow, including the supply of growth factors, which in its final result leads to atrophisation of the HA. Douglas et al. (4) stated in their study that persistent foetal vasculature may have a causal relationship also with congenital defect of coagulation, specifically with a deficit of protein C or S, which leads to pro-thrombotic states already during the intrauterine development of the foetus. Prenatal intraocular ischaemia originating in this manner may be the basis of up-regulation of angiogenic stimuli and the subsequent persistence of foetal vascular structures or the development of other ocular pathologies such as microphthalmos and vitreoretinal dysplasia.
The clinical picture and scope of functional affliction of the visual system depends on the degree of disorder of regression of the HA, complete or partial. PHA may be entirely asymptomatic, a chance finding upon a standard eye examination for another reason, or may be connected with amblyopia, nystagmus or strabismus (1). At the first examination, above all if this concerns identification in childhood age, it is important to differentiate PHA as a separate clinical unit or assess whether it is a part of a more complex ocular pathology in the case of PHPV. This may be manifested by leukocoria and thus imitate retinoblastoma, congenital cataract, retinopathy of prematurity or retinal dysplasia (1, 4).
Nevertheless, it is possible to expect that the fibrotic component of PHA, due to its rigidity, will later constitute an obstacle to posterior vitreous detachment (PVD) in the region of the vitreopapillary interface. This condition may even develop into a cleavage of the vitreous body, in which a part of the vitreous body without a relationship to PHA retracts physiologically with age and collapses as in the case of PVD, whereas the layer of the cortical vitreous body in the place of PHA adheres firmly to the retina (9). Local TRD or local retinoschisis may originate by means of a similar mechanism of vitreoretinal traction of the contracting ligament of the PHA, even without more pronounced subjective symptomatology, as we observed in our two patients. Gandorfer et al. (5) described a cohort of 20 patients with PHA, in which vitreomacular traction syndrome (VMTS) occurred in 2 patients only. At the same time, in one of the patients they also found TRD in addition to the DON, also incorporating the CL, in the second patient they found only tractional maculopathy without retinal detachment (RD).
Simple uncomplicated PHA does not require surgical intervention (8, 9). Surgical solution by means of pars plana vitrectomy (PPV) can be considered in the case of the development of complications leading to the damage of visual functions such as pronounced VMTS, rhegmatogenous RD, non-resorbing or recurring haemophthalmos. Upon indication for PPV, however, it is necessary to keep in mind the specific complications of the operation with regard to the presence of PHA.
Thumann et al. (11) published a case report of a young woman with a finding of highly elevated TRD, also incorporating the CL, which was the consequence of retraction of the ligament part of the PHA leading from the DON to the posterior surface of the lens capsule. Relaxation of traction was performed by means of PPV, in which the blood-filled PHA was coagulated by diathermy. The perioperative course was without complications, but on the first postoperative day the patient began to observe a paracentral scotoma in the visual field of the operated eye. A subsequent examination of the ocular fundus detected occlusion of the inferotemporal branch of the CRA, probably caused by diathermy of the PHA. This complication of PPV in the presence of PHA appears in isolated cases in the literature, and for this reason there is not a precise determination of the safe distance between the place of coagulation and the retina, in which there would be no risk of damage to the surrounding vascular structures. As a result, maximum caution is recommended in the indication of diathermy in the case of a finding of an atypical branch of the CRA (5, 11).
Doménech-Aracil et al. (3) described a case of a 72-year-old woman who underwent cataract surgery. Within the framework of the preoperative examination, a fibrotic stem adhering to the DON was detected, active blood flow was not demonstrated. Perioperatively, in the phase of hydrodissection, its re-channelling occurred, with renewal of blood flow and also breach of the posterior part of the lens capsule. Cataract surgery was completed by means of PPV with an examination of the posterior pole, where the finding was entirely within the norm. At the end of the procedure an artificial intraocular lens was implanted into the capsule. On the first postoperative day a pronounced deterioration of VA in the operated eye occurred, from an initial 20/80 to <20/200. The finding on the retina, the paleness of the posterior pole with a clearly red stain in the CL, tortuosity of veins, pronounced haemorrhage in all 4 quadrants and papillary edema indicated that the deterioration of VA was conditioned by the occurrence of both occlusion of the CRA and of the CRV, which was confirmed by fluorescence angiography. The authors explained the development of this condition by means of a common embryonic origin of the PHA and CRA, in which dissection of the lens wall passing also to the CRA occurred upon renewal of the blood flow of the PHA in the phase of hydrodissection of the lens. The newly generated 3rd space caused a collapse of the CRA and limited its blood flow, with the subsequent development of CRAO.
Another published complication in connection with the presence of PHA which raises the question of whether or not to embark upon a surgical solution is haemophthalmos. Various mechanisms of the origin of vitreous haemorrhage are described in the literature, nevertheless this again concerns only individual case reports. The most commonly stated cause was spontaneous occurrence, frequently explained by rapid eye movements during sleep, thus in its rapid (REM) phase, above all if the symptoms appeared in the morning after waking. The development of haemophthalmos was also observed following an external blunt trauma of the bulb (1, 8, 9). This complication of PHA usually did not require surgical solution, because vitreous haemorrhage was resorbed (within 20 months) or it was possible to differentiate structures of the posterior pole (9) even in the case of its persistence. PPV was performed only in cases of long-term non-resorbing haemophthalmos or in children, where the influence of non-transparency of ocular media caused a risk of occurrence of amblyopia. In the case of repeated vitreous haemorrhage, some authors chose photocoagulation of the haemorrhaging artery as prevention of further recurrence (8, 9).
CONCLUSION
In our two case reports we wished to demonstrate that a finding of PHA adhering to the retinal blood vessels, where local changes occur in the sense of TRD or retinoschisis, need not immediately be indicated for a surgical solution. Both of our patients were no longer at risk of the development of amblyopia, the finding on the ocular fundus did not manifest signs of acute changes, and no more pronounced subjective complaints or deterioration of VA were present. Also with regard to the possible risks in connection with PPV for the relaxation of vitreretinal traction, even though these are stated only in rare cases in the literature in the form of individual case reports, we decided in favour of a conservative procedure, specifically observation of the finding on the retina over time, if applicable with re-evaluation of our procedure in the case of progression of the condition.
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company.
MUDr. Tereza Řeháková
Oční klinika
Fakultní nemocnice Hradec Králové
Sokolská 581 500 05 Hradec Králové
Sources
1. Azrak, C., Campos-Mollo, E., Lledó-Riquelme, M. et al.: Vitreous haemorrhage associated with persistent hyaloid artery. Arch Soc Esp Oftalmol. 2011; 86 : 331-334.
2. Borbolla-Pertierra, A.M., Martínez - Hernández, C.K., Juárez-Echenique, J.C.: Bilateral persistent hyaloid artery. A case report. Arch Soc Esp Oftalmol. 2014; 89 : 235-238.
3. Doménech-Aracil, N., Montero-Hernández, J., Gracia-García, A. et al.: Combined central retinal artery and vein occlusion secondary to cataract surgery in a patient with persistent hyaloid artery. Arch Soc Esp Oftalmol. 2014; 89 : 161-164.
4. Douglas, A.G.L., Rafferty, H., Hodgkins, P. et al.: Persistent Fetal Vasculature and Severe Protein C Deficiency. Mol Syndromol. 2010; 1 : 82-86.
5. Gandorfer, A., Rohleder, M., Charteris, D. et al.: Ultrastructure of vitreomacular traction syndrome associated with persistent hyaloid artery. Eye. 2005; 19 : 333-336.
6. Gerinec A.: Detská oftalmólogia, Osveta, Martin, 2005, s. 25-26, 371-372.
7. Lai, A., Novel, A., Hung, S. et al.: Atypical Persistent hyloid Artery Remnant. Journal of the American Optometric Association. 2004; 75 : 377.
8. Önder, F., Coşar, C.B., Gültan, E. et al.: Vitreous Hemorrhage From the Persistent Hyaloid Artery. Journal of AAPOS. 2000; 4 : 190-191.
9. Štěpánková, J., Dotřelová, D.: Pars plana vitrektomie pro hemoftalmus na podkladě arteria hyaloidea persistens u tří dětí. Čes. a slov. Oftal. 2013; 69 : 243-247.
10. Taniguchi, H., Kitaoka, T., Gong, H. et al.: Apoptosis of the hyaloid artery in the rat eye. Ann Anat. 1999; 181 : 555-560.
11. Thumann, G., Bartz-Schmidt, K.U., Kirchhof, B. et al.: Branch Retinal Artery Occlusion by Diathermy. American Journal of Ophathalmology. 1997; 124, 3 : 415-416.
Labels
OphthalmologyArticle was published in
Czech and Slovak Ophthalmology

2017 Issue 5-6
-
All articles in this issue
- OCT Findings and Long-term Follow-up Results of Vitrectomy in Patients with Optic Disc Pit and Associated Maculopathy
- PERSISTENT HYALOID ARTERY – PERFORM A SURGERY OR NOT?
- Combination of Intravitreal Corticosteroid with Anti-vegf in Macular Edema Secondary to Retinal Vein Occlusion
- Sarkoidosis and its Eye Ocular Manifestation (an Analysis of Six Case Report)
- Results of Treatment of Diabetic Retinopathy by the Laser System PASCAL
- Ciliary body melanoma treatment by stereotactic radiosurgery
- The treatment results in patients with lmphoma disease in the orbit
- The Difference between Ganglion Cell Complex and Nerve Fiber Layer in the Same Altitudinal Halves of the Retina in Hyper-tension and Normal-tension Glaucomas
- Xerosis in Patient with Vitamin A Deficiency – a Case Report
- Recommended procedure for eye examination for infants and children of pre-school age in regular outpatient practice
- Czech and Slovak Ophthalmology
- Journal archive
- Current issue
- About the journal
Most read in this issue
- Sarkoidosis and its Eye Ocular Manifestation (an Analysis of Six Case Report)
- Recommended procedure for eye examination for infants and children of pre-school age in regular outpatient practice
- PERSISTENT HYALOID ARTERY – PERFORM A SURGERY OR NOT?
- The treatment results in patients with lmphoma disease in the orbit

