EFFECT OF MULTIPLE VARIABLES ON THE REFRACTIVE ERROR AFTER CATARACT SURGERY
Authors:
I. Popov 1; J. Valašková 1; V. Krásnik 1; D. Tomčíková 2
Authors‘ workplace:
Klinika oftalmológie LFUK a UNB Ružinov, Bratislava, Slovensko
1; Klinika detskej oftalmológie LF UK a NÚDCH, Bratislava, Slovensko
2
Published in:
Čes. a slov. Oftal., 74, 2018, No. 4, p. 158-161
Category:
Original Article
doi:
https://doi.org/10.31348/2018/1/4-6-2018
Overview
Purpose:
To analyze refractive results after cataract surgery in relation to used type of monofocal intraocular lens, calculation formula, to age, gender and laterality.
Settings:
Department of Ophthalmology, Comenius University and University hospital in Bratislava, Slovakia
Methods:
We analyzed 173 eyes (118 patients) after uneventful cataract surgery. We calculated prediction error (PE) and mean absolute error (MAE) of postoperative refraction.
Results and conclusion:
We found no statistically significant differences in PE and MAE in relation to types of used IOL, calculation formulas, gender, age or laterality.
Key words:
Optical biometry, monofocal IOL, IOL calculation, refractive error
INTRODUCTION
Cataract surgery has made dramatic advances since 29 November 1949, when Sir Harold Ridley implanted the first artificial intraocular lens (IOL) produced from polymethylmethacrylate (1). The first patient was a woman whose postoperative refraction was high myopia to the degree of -14 D. Today cataract surgery is not only a procedure for restoring the transparency of optic media, but also for adjusting refractive errors. With an improvement in the surgical techniques and biometric methods, we have made substantial progress since Ridley's first lens. More than 90% of operated eyes attain postoperative refraction (stated in spherical equivalent) within a range of +/ - 1 D (2). Multiple factors play a role in the overall result of cataract surgery. The most important are precise biometry and a correctly chosen model for calculation of the dioptric strength of the IOL. In addition to these factors, also of fundamental importance are the material, shape and other parameters such as individual healing of the wounds, contraction of the capsule and many others. For this reason we decided to compare certain input and output parameters upon cataract surgery, and to evaluate our results.
COHORT AND METHOD
Our study was conducted in the premises of the Department of Ophthalmology at the Faculty of Medicine, Comenius University and University Hospital in Bratislava. We retrospectively analysed data from examinations of patients before and after cataract surgery. In total we included 173 eyes (of 118 patients) in our cohort. Of the total number of 118 patients, 48 were men and 70 women. The patients were aged from 27 to 90 years. The average age was 70.7 ± 9.84 years. All the patients who took part in the study were operated on at the department for cataract, with implantation of an IOL. All the preoperative and postoperative examinations, including the operation itself, were conducted in the period from September 2014 to March 2017. The operation itself was conducted by a number of different surgeons, but with the same location of corneal incisions. Before cataract surgery the patients underwent a measurement of the biometric parameters of the eye with the aid of an optic biometer Lenstar LS900 (Haag-Streit, USA), using the principle of OLCR (Optical Low-Coherence Reflectometry). A model was used for calculation of the required IOL according to the recommendations and experiences of the centre as follows: for axial length (AL) of the eyeball less than 22 mm a Hoffer Q model was used, for AL from 22 mm to 24.5 mm an SRK-II model was used, for AL longer than 24.5 mm and less than 26 mm a Holladay 2 model was used, and for AL equal to or longer than 26 mm an SRK-T model was used. Eyes which had undergone uncomplicated cataract surgery with implantation of an IOL into the capsule were chosen for analysis. The eyes were not selected on the basis of axial length of the eye. All the patients in the cohort had refraction of the operated eye measured at least 5 days after surgery with the aid of an automatic keratorefractometer (Nidek Medical ARK-500A, NIDEK CO., LTD., Japan). Patients who manifested any kind of anomaly upon measurement in connection with cataract surgery (e.g. edema of the corneal epithelium, striae of the Descemet's membrane, anomaly of shape and localisation of pupil among others) were excluded from the observation. All the refractions were stated as spherical equivalent of refraction (SE). The estimated postoperative refraction was determined from tables automatically calculated by a Lenstar LS900 instrument on the basis of the selected IOL. Upon the calculation the Lenstar LS900 worked with selected surgically induced astigmatism of the size of 0.5 D. The difference between the estimated and actually measured refraction after the surgery served for determination of the average prediction error (PE) of postoperative refraction, its absolute error (AE) and its mean absolute error (MAE). The data was analysed and interpreted with the aid of descriptive statistics. For an evaluation of the relationship between the individual variables we used the Pearson correlation coefficient. For a comparison of the averages we used a t-test. In all the statistical analyses, the chosen level of significance was 5%. The data was statistically processed with the aid of the software IBM® SPSS® Statistics.
RESULTS
The descriptive statistics of the cohort are shown in table 1. From the table we can see that the dimensions of the eyes did not diverge markedly from the average in our population (3).
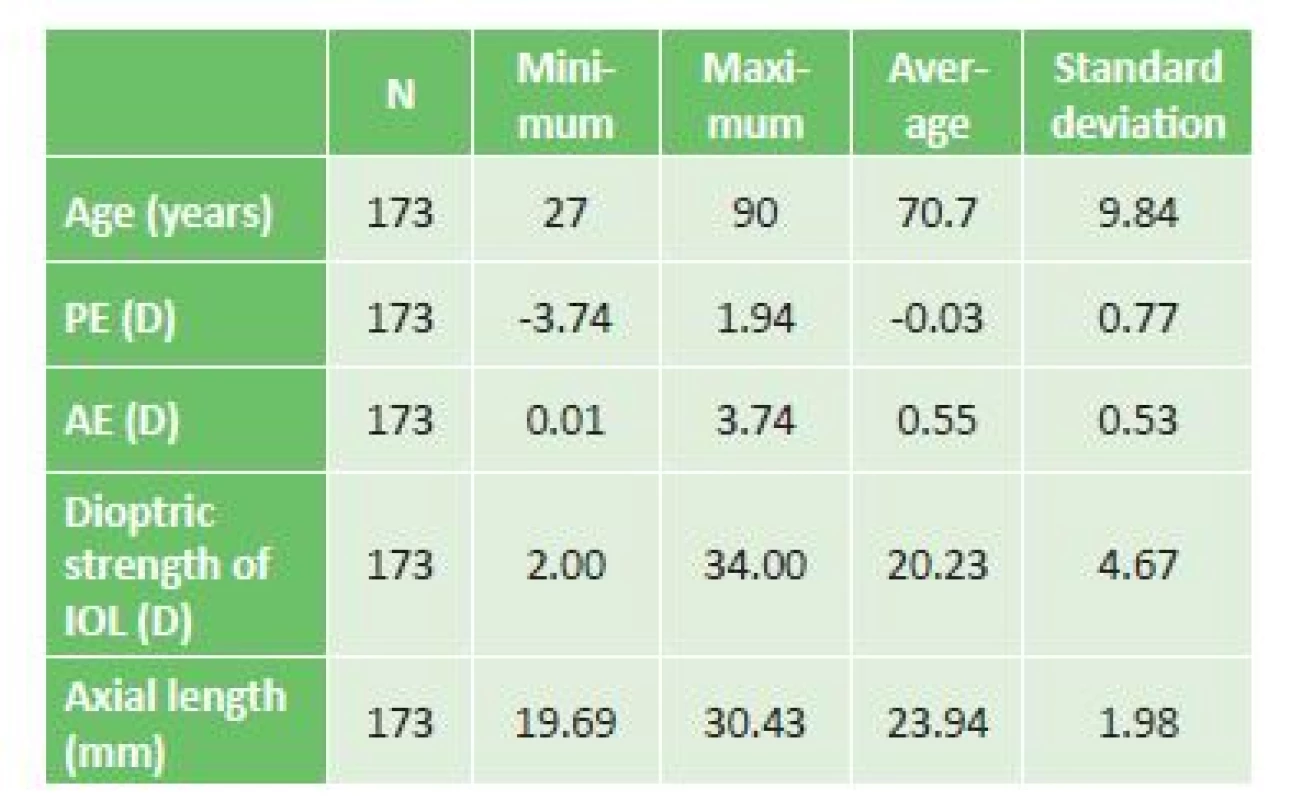
AE – absolute error
IOL – intraocular lens
We compared the differences between the sexes in the prediction error of postoperative refractions (table 2). The differences in PE and MAE were not statistically significant (p > 0.05).
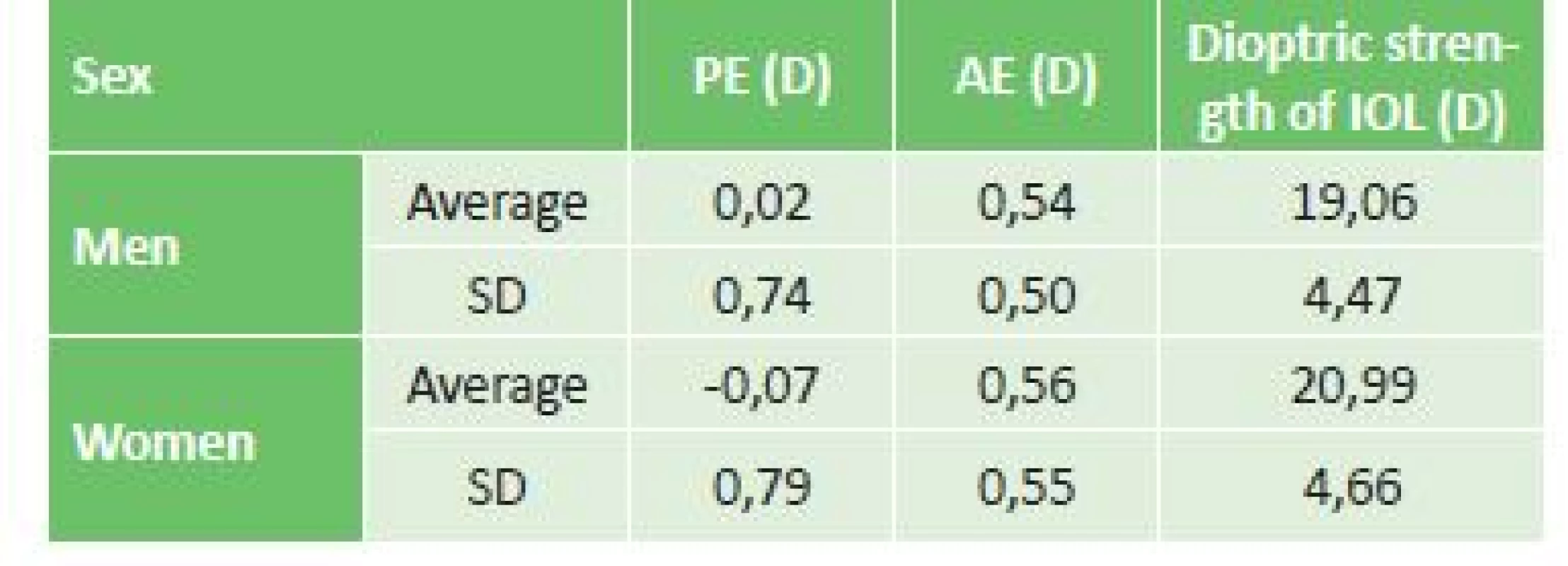
AE – absolute error
SD – standard deviation
IOL – intraocular lens
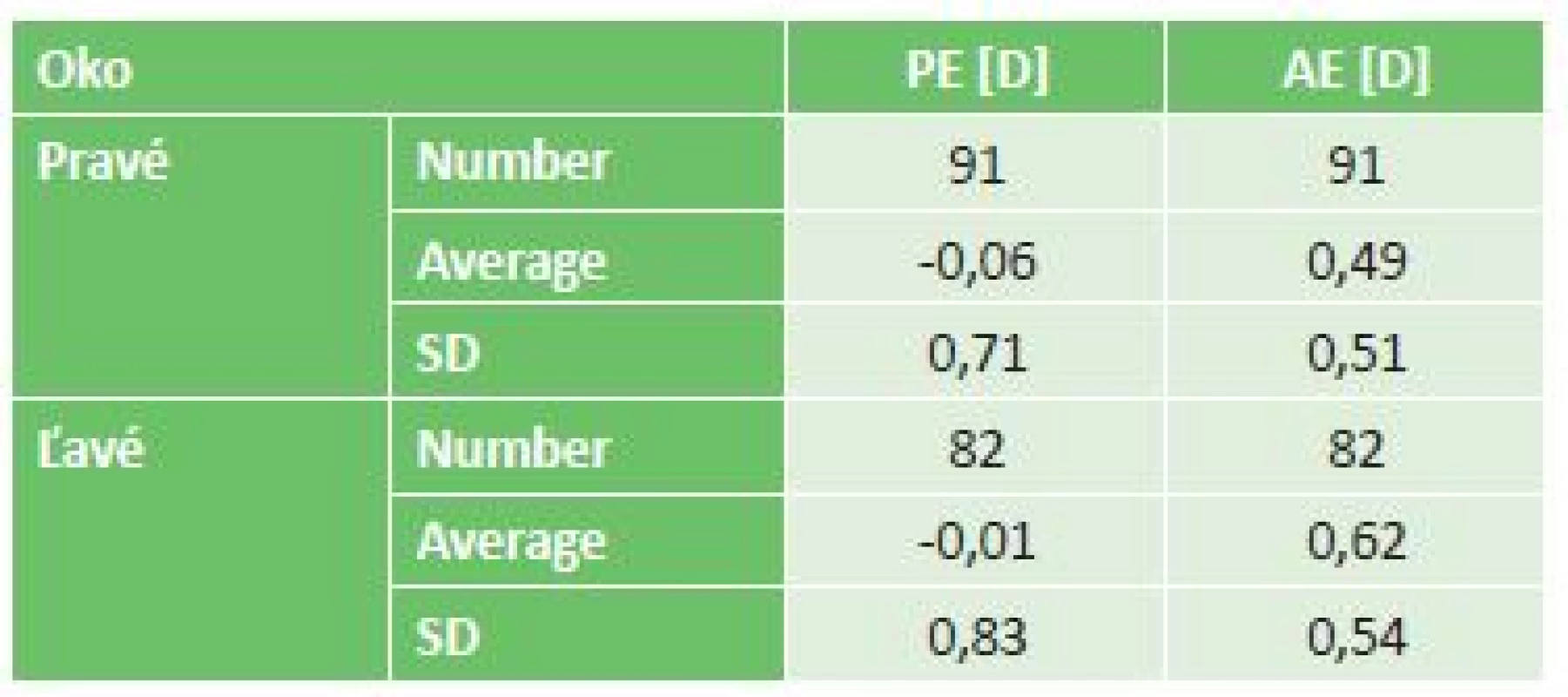
The postoperative prediction error of refraction between the right and left eye was neither clinically nor statistically significant (table 3).
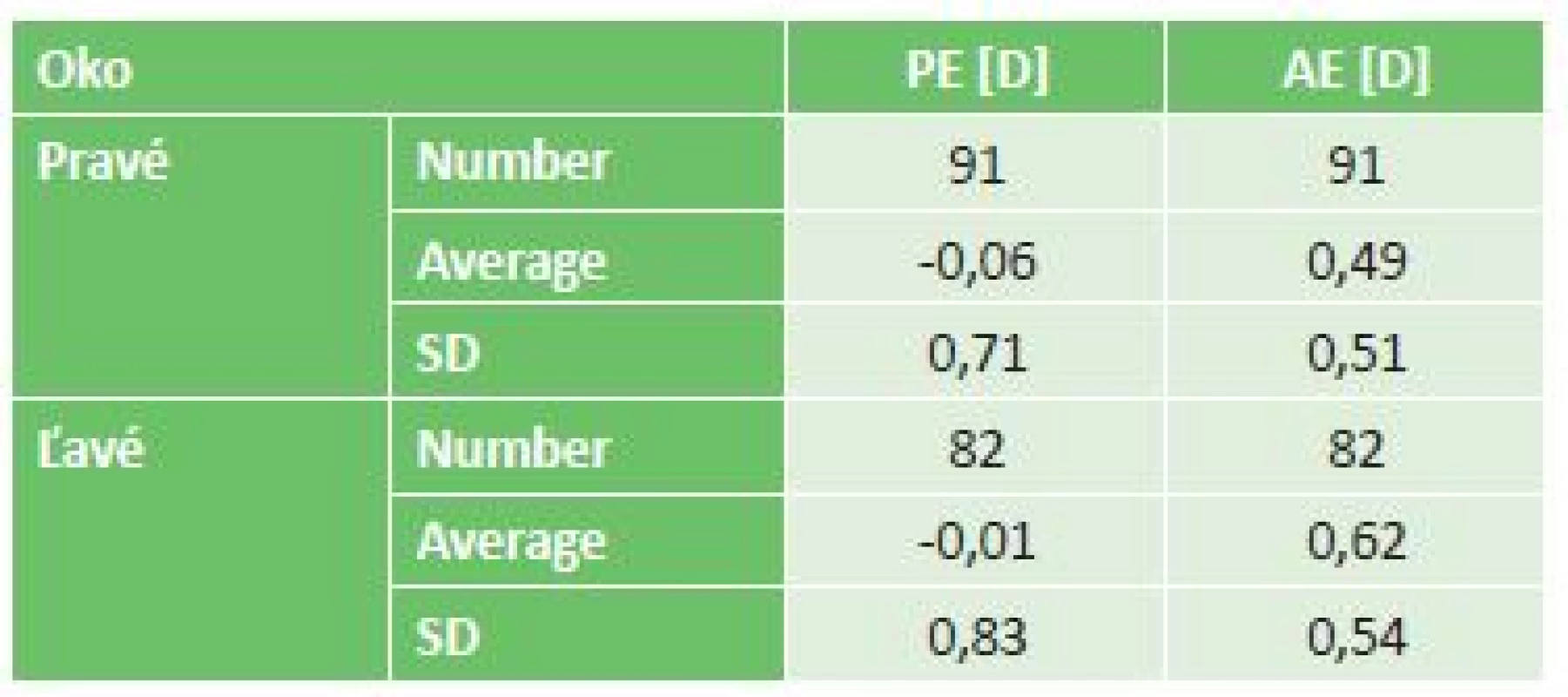
AE – absolute error
SD – standard deviation
Various models for calculating the dioptric strength of the IOL are used at our centre for the individual axial lengths of the eye, and for this reason we performed a mutual comparison of the precision of the models (table 4). In addition to the comparison of models, we also displayed the average dioptric strength of the implanted IOL for the individual models.
AE – absolute error
SD – standard deviation
IOL – intraocular lens
The prediction error of refraction and the absolute value of refraction are not statistically significant. The clinical significance is also not marked. The results indicate that the Hoffer-Q and Holladay models, which rank among the newer generations of models, manifest a slight myopic shift of postoperative refraction. The average dioptric strength of the implanted lens differs markedly for the individual models, which is probably linked with the different axial length of the eyes in which the given models were used.
We analysed which types of IOL attained the best postoperative results. At our centre, certain models are preferred more for certain patients. For example, the three-piece IOL Tecnis® ZA9003 is used far more often for non-standard eyes, such as eyes with high myopia, where we expect a loosening of the suspension apparatus. In those eyes with a longer axial length, the incidence of imprecisions in the measurement and in the postoperative result is higher (4), and as a result the data could be distorted to the detriment of this type of IOL. On the basis of this assumption, we decided to compare the individual types of IOL only in eyes with an axial length of 22 to 26 mm (models SRK-II and Holladay). The postoperative results for the individual types of IOL are shown in table 5.
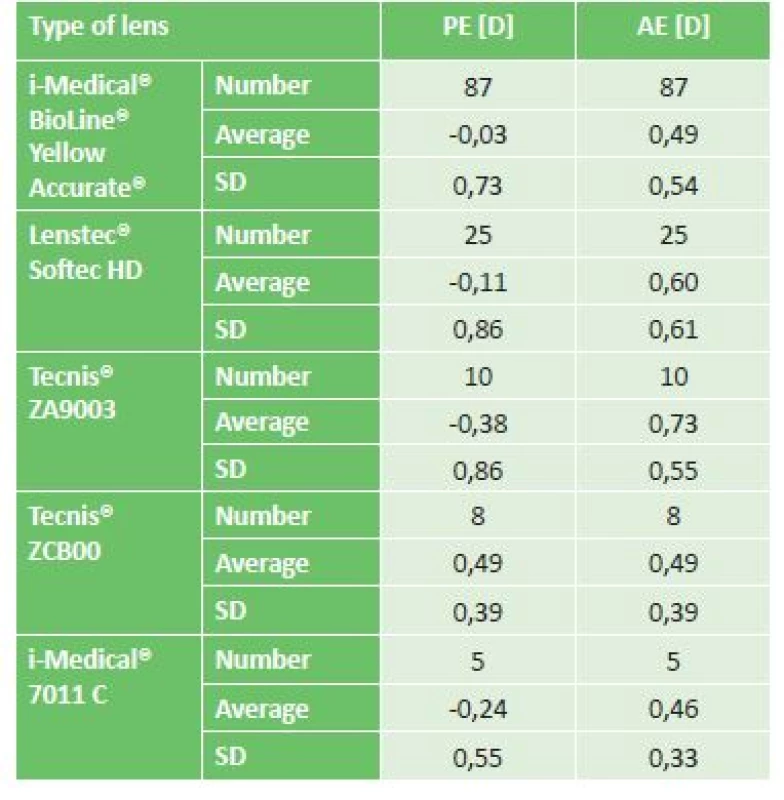
PE – prediction error
AE – absolute error
SD – standard deviation
IOL – intraocular lens
The difference in the results between the individual IOLs in table 5 did not reach statistical significance. In order to verify the above-mentioned empirical observation that eyes with an extreme axial length attain worse postoperative results of refraction, we analysed the correlation between the absolute difference of postoperative refraction and the strength of the implanted IOL, which is indirectly linked with axial length. The correlation was neither clinically nor statistically significant (r = 0.05; p > 0.05).
We also analysed the hypothesis concerning whether increasing age may be linked with a worse postoperative result. We calculated the correlation between the absolute difference of postoperative refraction and age, in which we in fact observed a negative correlation, which was nevertheless not statistically significant (r = -0.07; p > 0.05).
DISCUSSION
It ensues from our results that cataract surgery with the implantation of an IOL is a very precise and predictable procedure with regard to the refractive result. From our observed parameters we demonstrated that the average prediction errors of refractions between the sexes were not statistically significant. On average, in men the implanted IOL was 1.93 D weaker than in women, which is probably linked with the fact that on average eyes are longer in men than in women (3, 5).
Upon a comparison of the models used at our centre, we did not find either a statistically or a clinically significant difference in their success rate. We may however take into account the fact that the Hoffer-Q and Holladay models, which rank among the newer generations of models, manifest a slight myopic shift of postoperative refraction. The average dioptric strength of the implanted lens differs markedly for the individual models, which is probably linked with the different axial length of the eyes in which the given models were used. We compared our results for the individual models and axial lengths with a similarly constructed study, in which the Hoffer Q model recorded PE = -0.22 D and MAE = +0.499 D, the Holladay model PE = +0.12 D and MAE = +0.405 D, the SRK/T model PE = -0.20 D and MAE = +0.484 D (6). SRK-II ranks among the oldest models and is not favoured by the majority of today's studies. However, according to our results and other publications (7) it represents a very precise model, which confirms that the choice of model should be down to the experience of the centre.
Upon a comparison of the precision of predicting postoperative refraction, we did not find any statistically significant differences. The results may have been imprecise to a certain extent with regard to the unequal representation of the individual types of IOL, in which the numbers of ZA9003, ZCB00 and 7011C were markedly lower than the numbers of BioLine Yellow and Softec HD. Our results differ slightly from the study comparing only the IOLs ZA9003 and ZCB00 (8), in which their postoperative results were PE (ZA9003) = 0.11 ± 0.47 D, MAE (ZA9003) = 0.40 ± 0.27 D, PE (ZCB00) = 0.01 ± 0.47 D, MAE (ZCB00) = 0.39 ± 0.35 D. However, in this foreign study less strict inclusion criteria were used for length of eye, covering 22 mm to 28 mm. Despite the fact that in our study we did not demonstrate a statistically significant difference in the postoperative results between lenses, for our purposes we drew a certain clinical conclusion which was confirmed also by our observations that the IOL ZCB00 manifests a slight hypermetropic shift of postoperative refraction.
The dependency between the precision of the postoperative results and age was not statistically significant.
The dependency between the dioptric strength of the IOL and the precision of the postoperative results was not statistically significant. This observation demonstrates that a correctly chosen sample for both longer and shorter eyes also produces very precise results, which is in accordance also with other studies on long eyes (9-12). Some authors have observed an increase of imprecision in short and long eyes (4, 13, 14).
CONCLUSION
In our study we demonstrated that cataract surgery with the implantation of an artificial intraocular lens is, upon the selection of a suitable model for calculation of the IOL, a very predictable procedure, which very precisely adjusts not only refraction but also improves connected visual acuity, as demonstrated by several observations (15, 16). Taking into account the postoperative results for the given centre upon the selection of the required artificial intraocular lens may further improve predictability.
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company.
Received: 22. 7. 2018
Accepted: 31. 8. 2018
Available on-line: 18. 3. 2019
MUDr. Ivajlo Popov, FEBO
Klinika oftalmológie LFUK a UNB Ružinov,
Bratislava, Slovensko
Email: ivajlo.popov@gmail.com
Sources
1. Apple, D.J., J. Sims: Harold Ridley and the invention of the intraocular lens. Surv Ophthalmol, 40(4); 1996 : 279-92.
2. Lundstrom, M., M. Dickman, Y. Henry, et al.: Risk factors for refractive error after cataract surgery: Analysis of 282 811 cataract extractions reported to the European Registry of Quality Outcomes for cataract and refractive surgery. J Cataract Refract Surg, 44(4); 2018 : 447-452.
3. Popov, I., Valaskova J., Stefanickova J., et al.: Výpočet zastúpenia refrakčných chýb slovenskej populácie za použitia gullstrandovho modelu oka. Cesk Slov Oftalmol, 73(3); 2017 : 113-117.4. Roessler, G.F., T.S. Dietlein, N. Plange, et al.: Accuracy of intraocular lens power calculation using partial coherence interferometry in patients with high myopia. Ophthalmic Physiol Opt, 32(3); 2012 : 228-33.
5. Fotedar, R., J.J. Wang, G. Burlutsky, et al.: Distribution of axial length and ocular biometry measured using partial coherence laser interferometry (IOL Master) in an older white population. Ophthalmology, 117(3); 2010 : 417-23.
6. Kane, J.X., A. Van Heerden, A. Atik, et al.: Intraocular lens power formula accuracy: Comparison of 7 formulas. J Cataract Refract Surg, 42(10); 2016 : 1490-1500.
7. Ozcura, F., S. Aktas, H.M. Sagdik, et al.: Comparison of the biometric formulas used for applanation A-scan ultrasound biometry. Int Ophthalmol, 36(5); 2016 : 707-12.
8. Mednick, Z.D., D.K. Varma, X. Campos-Moller, et al.: Refractive predictability of a 3-piece intraocular lens platform versus its 1-piece counterpart. Can J Ophthalmol, 52(2); 2017 : 146-149.
9. Terzi, E., L. Wang, T. Kohnen: Accuracy of modern intraocular lens power calculation formulas in refractive lens exchange for high myopia and high hyperopia. J Cataract Refract Surg, 35(7); 2009 : 1181-9.
10. Aristodemou, P., N.E. Knox Cartwright, J.M. Sparrow, et al.: Formula choice: Hoffer Q, Holladay 1, or SRK/T and refractive outcomes in 8108 eyes after cataract surgery with biometry by partial coherence interferometry. J Cataract Refract Surg, 37(1); 2011 : 63-71.
11. Bang, S., E. Edell, Q. Yu, et al.: Accuracy of intraocular lens calculations using the IOLMaster in eyes with long axial length and a comparison of various formulas. Ophthalmology, 118(3); 2011 : 503-6.
12. Wang, J.K., C.Y. Hu, S.W. Chang: Intraocular lens power calculation using the IOLMaster and various formulas in eyes with long axial length. J Cataract Refract Surg, 34(2); 2008 : 262-7.
13. Zheng, Q., Z. Zhao, H. Lian, et al.: [The analysis of refractive error of long axial high myopic eyes after IOL implantation]. Zhonghua Yan Ke Za Zhi, 51(4); 2015 : 276-81.
14. Long, T., Y.-S. Huang, L.-X. Xie: Refractive accuracy after intraocular lens implantation in pediatric cataract.Int J Ophthalmol , 5(4); 2012 : 473-477.
15. Velika, V., Hejsek L., Raiskup F.: Klinické výsledky implantace dvou typů multifokální rotačně asymetrické nitrooční čočky. Cesk Slov Oftalmol, 73(1); 2017 : 3-12.
16. Halas, M., Pesko K., Olah Z., et al.: Vplyv sferickych a asferickych umelych vnutroocnych sosoviek na kvalitu centralnej ostrosti zraku a kontrastnej citlivosti. Cesk Slov Oftalmol, 66(5); 2010 : 209-12.
Labels
OphthalmologyArticle was published in
Czech and Slovak Ophthalmology

2018 Issue 4
-
All articles in this issue
- Diagnosis of Familial Hypercholesterolaemia on First Sight? The Role of the Ophthalmologist in Identifying Patients with Familial Hypercholesterolaemia
- Vertical Strabismus – Indication of Surgical Techniques on the Inferior Rectus Muscle
- Keratopigmentation (Corneal Tattoo) – Our First Experience
- Correction of Myopia and Myopic Astigmatism by Implantation of a Phakic Posterior Chamber Implantable Collamer Lens
- Digital Eye Strain in a Population of Young Subjects
- EFFECT OF MULTIPLE VARIABLES ON THE REFRACTIVE ERROR AFTER CATARACT SURGERY
- Czech and Slovak Ophthalmology
- Journal archive
- Current issue
- About the journal
Most read in this issue
- Vertical Strabismus – Indication of Surgical Techniques on the Inferior Rectus Muscle
- Keratopigmentation (Corneal Tattoo) – Our First Experience
- Diagnosis of Familial Hypercholesterolaemia on First Sight? The Role of the Ophthalmologist in Identifying Patients with Familial Hypercholesterolaemia
- Correction of Myopia and Myopic Astigmatism by Implantation of a Phakic Posterior Chamber Implantable Collamer Lens
