Keratopigmentation (Corneal Tattoo) – Our First Experience
Authors:
P. Žiak 1,2; K. Kapitánová 2,1; J. Halička 1,2; P. Mojžiš 3
Authors‘ workplace:
Očná klinika JLF UK a UN Martin (prednosta kliniky MUDr. Žiak Peter, PhD.
1; UVEA Mediklinik, Martin- Priekopa (medicínsky riaditeľ MUDr. Žiak Peter, PhD. )
2; Oční centrum Teplice, Premium Clinic, s. r. o., (lekársky riaditeľ MUDr. Mojžiš Peter, PhD., FEBO)
3
Published in:
Čes. a slov. Oftal., 74, 2018, No. 4, p. 140-144
Category:
Original Article
doi:
https://doi.org/10.31348/2018/1/3-4-2018
Overview
Introduction: Keratopigmentation or corneal tattooing represents an unique cosmetic solution for corneal leucomas and also for other pathological changes affecting cornea or iris. Procedure is based on pigment insertion into the corneal stroma. Goal is to improve the appearance of the affected eye. These days are most frequently used tattoo kits with different sterilised inks made primary for skin tattooing. As a new possibility there are also available biocompatible micronized mineral pigments.
Methods: Authors will introduce four case reports of four patients with corneal leucomas, who wanted to undergo the corneal tattooing to improve the cosmetic appearance of their blind eyes. Authors decided for keratopigmentation with an use of inks intended primary for skin tattooing.
Results: In all four patients was the final appearance of tattooed cornea more than satisfying. Postoperative examination didn´t detect diffusion, fading, colour changes of the pigments. No complications such as toxic or immune reaction due to the pigment were recorded. All four patients were subjectively fully satisfied with the cosmetic result of the keratopigmentation.
Conclusion: Based on the first experience authors consider keratopigmentation to be a safe and relatively uncomplicated surgical method. Corneal tattooing is also quite cheap, does not require patient´s hospitalization and postoperative reconvalescence in usually short term.
Key words: keratopigmentation, corneal tattoo, corneal leucoma, blind eye
INTRODUCTION
Keratopigmentation (KPT) or corneal tattooing is a method based on the insertion of pigments into the corneal stroma. It is usually used to improve the cosmetic appearance in blind eyes with corneal leucoma in cases where for various reasons it is not possible to perform another procedure (exenteration of the eyeball, keratoplasty). It is possible to use corneal tattooing also on sighted eyes, e.g. eyes with defects of the iris or fixed mydriasis (3) (most often following injuries), or also in the case of leukocoria (5). A risk is posed above all by toxic reaction to the used pigment of the stromal keratocytes, endothelium and structures of the anterior chamber, in addition to which there is a risk of keratitis to corneal ulcer, as well as progressive fading, diffusion or change of the original colour of the pigment, excessive or insufficient pigmentation. Another problem may be a different resulting colour in comparison with the other eye (2). A number of techniques exist for corneal tattooing, from simple surface colouring of the cornea via corneal pigmentation with the aid of needle pigment applicators, insertion of colouring into the corneal stroma using lamellar intrastromal cannulas, up to pigment application beneath the corneal lamella created with the aid of a femtosecond laser (5). At present, several types of pigments are available which can be used for corneal pigmentation. Probably the first ever historical use of reduced copper sulphate in the process of KTP was by the creator of systematic medical science and healer of the gladiators Claudius Galen in the second half of the second century AD (1). Later other substances were also applied, such as Indian and Chinese ink, powdered metal substances, organic pigments, animal uveal pigment, gold and platinum chlorides, as well as soot. These substrates had various limitations, especially low stability of the resulting colour and a limited spectrum of the attainable colours. At present, commercially available kits of sterilised pigments for regular skin tattooing are predominantly used for corneal tattooing (4), another suitable substrate is biocompatible micronised mineral pigments, which provide good colour stability, zero toxicity and a good cosmetic effect (3). Cosmetic contact lenses may appear to be the simplest cosmetic solution for corneal leucomas. However, in practice the majority of patients have poor tolerance of such lenses. A significant problem is also the availability of suitable cosmetic contact lenses, as well as their price. Cosmetic keratoplasty usually does not have the best prognosis, and is problematic also due to the shortage of corneas from donors. As a result the most frequent solution is ultimately evisceration of the eyeball and insertion of an acrylate or glass prosthesis. For the patient this represents a painful and mutilating procedure, which is also the reason why many patients reject this solution. In fact the cosmetic effect of leucoma is highly undesirable and stigmatises the patient, with the result that many patients even avoid social contact, suffer a loss of self-esteem and experience psychological problems. A number of studies have been published on the potential use of KTP for improving the cosmetic effect in patients with leucomas with an excellent result and patient satisfaction. Despite this fact, experiences with corneal tattooing are limited worldwide, which to a substantial extent is a consequence of the unavailability of commercially produced pigments (2, 3, 4, 8). However, for patients with an unstable structure of the corneal surface, for example with active angiogenesis, recurrent erosions of the epithelium and irregularities of the corneal surface, corneal tattooing is usually unsuitable (6).
MATERIAL AND METHOD OF STUDY
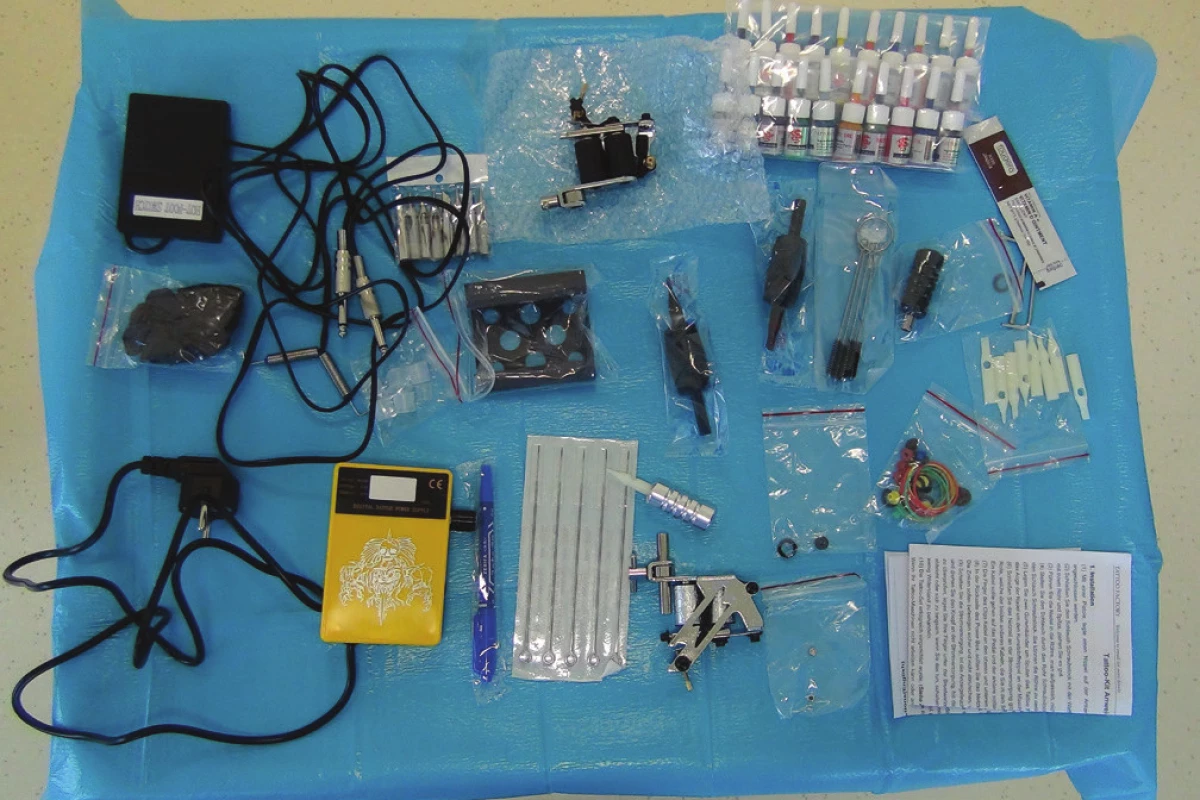
On the basis of the published data (4), we chose commonly available tattooing pigments designated primarily for skin tattooing as the medium for keratopigmentation. These were purchased in a kit containing a spectrum of 20 sterile inks of various colours, together with the technical accessories and sterile needles required for their application (Fig. 1). All the patients signed an informed consent form before the operation. The procedure was performed in the form of one-day outpatient surgery, under local anaesthesia with the use of eye drops (Benoxi gtt., UnimedPharma, Slovak Republic). The used pigments are composed of an organic pigment component, glycerine and distilled water. We created the optimum shade by mixing the available colour tints with reference to the colour of the patient's other eye. For the application of the pigments into the corneal stroma we used a coil tattooing instrument with an adjustable working output of up to 17 V (optimum 9-12 V). With regard to the frequent presence of scarry structures on the surface of the corneal stroma, as well for good control of the depth to which the pigment was to be applied, we always performed abrasion or keratectomy on the level of the corneal stroma. In the first phase of the actual tattooing we inserted black pigment into the area of the presumptive pupil, and we subsequently tattooed the desired colouring of the other sections of the cornea by repeat application of mixed pigment with the aid of the tattooing instrument. Checking the colour of the cornea of the healthy eye helped us mix the colour tone of the pigment. We completed the operation by the placing of a therapeutic soft contact lens (Cooper Vision, USA). We usually left the lens in the eye for a period of 7-10 days.
We administered local antibiotic therapy 5 times per day over the course of 14 days (Oftaquix gtt., Santen, Finland; or Tobrex gtt., Alcon, Novartis, Switzerland). After the removal of the therapeutic contact lens an antibiotic cream was added to the local therapy (Tobrex ung., Alcon, Novartis, Switzerland) for 7 to 10 days, applied for the night. Subsequently the patient was advised to apply artificial tears according to subjective requirement, for an individual length of time after surgery.
CASE REPORT 1
A 35-year-old man with leucoma in the blind left eye following a perforating injury in childhood reported to our clinic with a request for assistance in seeking a solution to the appearance of his “unsightly left eye”. The patient works as a chef abroad.
According to the healthcare documentation, the patient had undergone a number of operations on his left eye (including pars plana vitrectomy) in connection with the trauma in the past. Objective best corrected central visual acuity (BCVA) in the right eye was 1.0, and in the left eye there was presence of amaurosis. There was a dense leucoma on the cornea of the left eye, in the centre with an indication of zonular changes. There was also a presence of divergent strabismus (ex anopsia) in the left eye. By means of an ultrasonographic B scan we verified high total inveterate amotio retinae, intraocular pressure was lower upon palpation – it was not possible to measure pressure with a tonometer. The finding in the right eye was physiological. The patient did not tolerate a cosmetic contact lens, on the basis of information obtained via the internet he sought out the possibility of a corneal tattoo in the left eye. We did not have experience of KTP at our clinic at that time, but we decided to study the issue and according to possibilities comply with the patient's request.
During the procedure we performed chelation of the cornea with 3% EDTA solution, we removed calcified residual matter from the corneal surface, and also performed surface keratectomy by knife. After smoothing the surface of the corneal stroma, KTP was performed – the area of the pupil was pigmented with black colour, the area of the iris by combined blue and green pigment. During the procedure we also extracted an old episcleral filling and sutured the conjunctiva. Botulotoxin (BOTOX plvino., Allergan Pharmaceuticals, Ireland) was applied preoperatively to the region of the musculus rectus lateralis in a dose of 4 units, we applied a therapeutic contact lens to the cornea. A video showing the course of the operation is published on the website https://youtu.be/b7LAV6pB_hs.
During a follow-up examination 3 days after the operation, the eyeball was only slightly superficially injected, in slight divergence, with assessable intrabulbar structures of the eye without signs of inflammatory reaction. We extracted the therapeutic contact lens on the 10th day after the procedure, the cornea was completely pre-epithelialised, which we examined by fluorescein. After four months the cosmetic effect was macroscopically satisfactory, and the patient was subjectively very satisfied. Upon an examination on a slit lamp there were no signs of inflammation present, and no formation of neovascularisations. At the same time we repeated the application of botulotoxin into the musculus rectus lateralis (Fig. 2 and 3). As a rule it is necessary to repeat the application of botulotoxin every three to four months, thus at the time when the previous dose is losing effect (8).


CASE REPORT 2
The second patient was a 57-year-old woman with a blind, originally evidently blunt-sighted left eye – in 2005 total inoperable retinal detachment was diagnosed, with seclusion and occlusion of the pupil and complicated cataract. Later the condition was evaluated on the basis of a USG B scan as massive preretinal haemorrhage and haemophthalmos of old origin, amaurosis. The patient requested at least a cosmetic solution to her condition, since she had long felt stigmatised by the markedly altered external appearance of her left eye. She refused evisceration of the eye. Upon an examination the blind left eyeball was tubercular and slightly hypotonic upon palpation, the cornea with dense leucoma did not enable differentiation of the other ocular structures.
We indicated KTP for the patient for cosmetic reasons. The aim was to create the appearance of a pupil with the aid of black pigment applied to the centre of the cornea, and the appearance of an iris by means of circular application of a mixture of blue, grey and green tints of pigment to such an extent as to ensure that the result was as similar as possible to the second, healthy eye.
One week after the procedure the cornea was completely pre-epithelialised, the eyeball was pacific, the patient without complaints. After 3 months pigmentation of the cornea was unchanged, with regard to the present tuberculosis of the eyeball, the smaller diameter of the cornea had a slightly disruptive effect. However, we did not proceed with supplementing the tattoo because the patient was satisfied with the result (Fig. 4 and 5).
CASE REPORT 3
The third patient was a 44-year-old man with amaurosis and corneal leucoma of the right eye following a penetrating injury in 2001, who had been repeatedly operated on in the past. The left eye was pseudophakic and after pars plana vitrectomy with membranectomy and peeling of the internal limiting membrane. The patient requested a cosmetic solution of the right eye.
Objectively there was presence of slight palpation hypotonia in the right eye, cornea with dense leucoma, and with regard to the intraocular structures the periphery of the iris was visible only dimly. According to the patient's healthcare documentation, pars plana vitrectromy had been performed on this eye in the past, with the application of silicone oil, later with the occurrence of secondary glaucoma. We performed tattooing of the cornea of the right eye.
Under instillation anaesthesia we removed the altered corneal epithelium, and subsequent keratopigmentation was performed similarly as on the previous patients. We left a soft therapeutic contact lens for 7 days, antibiotic therapy with eye drops (Oftaquix gtt., Santen, Finland) was applied for 14 days. On the 7th postoperative day the eyeball was pacific, the epithelium virtually healed, we removed the therapeutic contact lens. Subjectively the patient had only a slight tingling feeling. After 6 weeks the patient was without subjective complaints and was satisfied with the result of the tattoo, the colouring of the cornea was sufficient (Fig. 6 and 7).

CASE REPORT 4
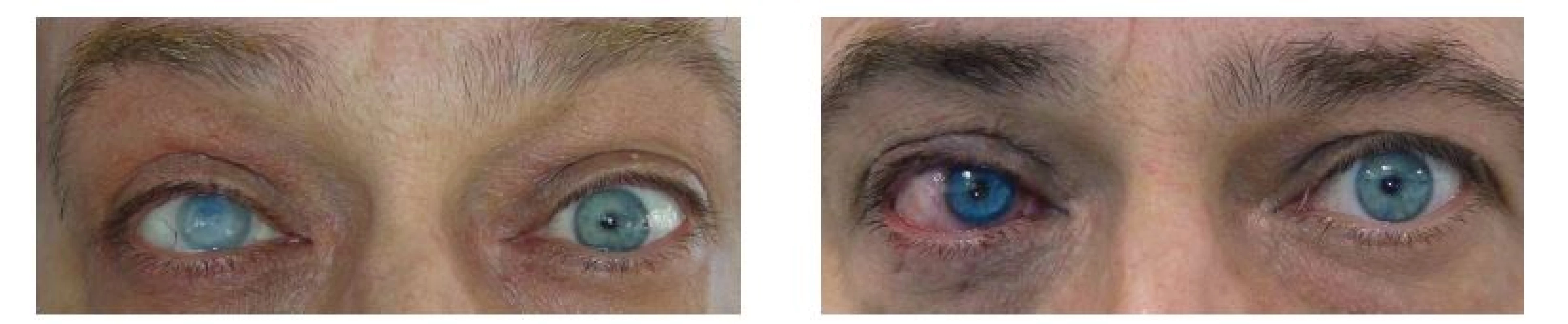
The fourth patient was a 50-year-old woman with high myopia and myopic chorioretinopathy, who had been repeatedly operated on in the past for reattachment of the retina of the right eye (equatorial cerclage with silicone implant, application and subsequent evacuation of silicone oil with multiple pars plana vitrectomy). The patient later lost vision in her right eye, probably as a result of secondary glaucoma. Objective finding on anterior segment of right eye: injection of bulbar conjunctiva with mild chemosis, on cornea diffuse vascularised leucoma, the other ocular structures could not be differentiated due to the finding on the cornea. We added a USG B scan – silicone oil was left in the cavity of the vitreous body of the right eye after the last pars plana vitrectomy. On palpation the eyeball was slightly hypotonic, the cerclage strip was visibly forced out on the eyeball at number 12. We extracted this under local anaesthesia. With the use of brown, yellow and red tints we mixed a pigment with a colouring close to that of the iris of the left eye, as usual black colour was used for the creation of the pupil. Following abrasion of the corneal epithelium under instillation anaesthesia, we inserted the pigments into the corneal stroma with a needle applicator, a therapeutic contact lens was applied and a local antibiotic was administered into the conjunctival sac in drop form (Tobrex gtt., Alcon, Novartis, Switzerland).
At a follow-up examination 7 days after the procedure, the patient felt no pain, the cornea was completely pre-epithelialised, and we removed the therapeutic contact lens. The local antibiotic treatment was administered for 7 more days. One month after the procedure, the pigmentation of the cornea was stable, even if less pronounced in the area surrounding the “pupil”, which we had expected on the day of actual tattooing. However, the patient was satisfied with the cosmetic effect, and as a result we did not proceed with supplementing the pigmentation (Fig. 8 and 9).
DISCUSSION
At present the preferred solution for patients with a blind, cosmetically seriously damaged eye is to wear a coloured contact lens, which however is not well tolerated by all patients. Perforating keratoplasty with all its known limitations and risks is also only an occasionally used option. In the most severe and otherwise unmanageable cases, the last available option is one of the mutilating procedures – evisceration or enucleation of the eyeball with adaptation of the prosthesis (2).
Within this narrow spectrum of options, keratopigmentation represents a unique cosmetic solution of leucomas and other pathological changes of the cornea or iris. It concerns a relatively undemanding procedure, both for the patient and for the operating surgeon, with a practically immediate result. Despite this, it is used relatively rarely.
The most modern approach in corneal tattooing today consists in the use of micronised mineral corneal pigments, which according to the studies conducted to date are excellently tolerated by the cornea. They may represent a permanent solution to the cosmetic problem thanks to the reliable stability of the resulting colour even over an observation period of several years (1), as well as due to their zero toxicity. They were registered by the Spanish Ministry of Health in the year 2001, and in a study from 2007 first officially used by the method of superficial and intralamellar corneal colouring (1). They can be purchased via a website focusing on keratopigmentation for cosmetic and therapeutic reasons. This website also offers other accessories required for the use of these highly specialised pigments.
The above-described technique of corneal tattooing which we chose also represents an effective and at the same time very affordable alternative, which on the basis of our results so far has demonstrated itself to be an adequate, economical, safe and stable solution for patients with serious cosmetic changes of the anterior segment of a blind eye.
As of today, we have performed tattooing on a total of 17 patients, therefore 17 eyes, at our clinic. In 16 cases this concerned a blind eye with corneal leucoma, in one eye only there was an indication of congenital basal coloboma of the iris. In this case tattooing was performed only partially, limited to the area corresponding to the defect of the iris. The resulting appearance of the afflicted eye immediately after the procedure was satisfactory in the majority of cases. The period of complete convalescence was usually less than 14 days, in two cases with deteriorated trophic function of the cornea the recovery took longer. In one case repeat application of an amniotic membrane was required due to lack of healing of the corneal defect. Follow-up examinations on our first four patients after more than 6 months did not detect any more serious complications in the sense of diffusion of the colouring and fading of the colour of the cornea (the first patient is now more than 12 months after KTP without change of the local finding). There was also no new development of active angiogenesis in the cornea, either toxic or immune reaction to the used ink. Subjectively the patients are satisfied with the cosmetic effect.
CONCLUSION
Based on our experience, keratopigmentation – corneal tattoo is a suitable alternative for improving the appearance of a blind eye with corneal leucoma. It may be a procedure with a long-term to permanent cosmetic effect. KTP with the use of commonly available tattooing pigments produced a satisfactory aesthetic result in the majority of patients. With the exception of one case with a non-healing corneal defect, we did not observe any more serious complications in the to-date monitoring period, and even after 6 months the result appears to be stable.
On the basis of these results we consider KTP to be a relatively safe and simple surgical procedure for a cosmetic solution to corneal leucomas. The advantage is its affordability, immediate result and short time of convalescence required.
The limits of our study are given by the relatively small number of observed patients, as well as the short observation period. A question so far remains with regard to the long-term stability of corneal pigmentation over the course of several years.
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company.
Note: this study was published in the form of a lecture entitled “Unsightly eye” on the day of 7 October 2016 at the Prague Ophthalmology Festival
Received: 28. 5. 2018
Accepted: 29. 8. 2018
Available on-line: 18. 3. 2019
MUDr. Karolína Kapitánová
Klinika Oftalmológie JLF UK a UN Martin,
Kollárova 2, 036 59 Martin
e-mail: kapitanova.k@gmail.com
Sources
1. Alio JL., SirerolB., Walewska - Szafran A. et al.: Corneal Tattooing (keratopigmentation) to restore cosmetic appearance in severely impaired eyes with new mineral micronized pigments.Br J Ophthalmol [online]. August 2009[cit. 12 júna 2017]. Dostupné na: www.ncbi.nlm.nih.gov/pubmed/19679571
2. Alio JL., Rodriguez AE., El Bahrawy M.et al.: Keratopigmentation to Changethe Apparent Color of the Human Eye: A Novel Indication for Corneal Tattooing. Cornea [online]. Apríl 2016 [cit. 12 júna 2017]. Dostupné na www.ncbi.nlm.nih.gov/pubmed/26845312
3. Amesty M., Alio JL., Rodriguez AE.et al.: Corneal tolerance to micronised mineral pigments for keratopigmentation. Br J Ophthalmol [online]. December 2014 [cit. 12 júna 2017]. Dostupné na: http://bjo.bmj.com/content/98/12/1756
4. Garrido-Hermosillaa AM., Ángeles-Figueroab RA., Gessa-Sorrocheb M.: Surgical intrastromal keratopigmentation using tattoo ink. ArchSocEspOftalmol [online]. Júl 2014 [cit. 12 júna 2017]. Dostupné na: www.sciencedirect.com/science/article/pii/S2173579414001509
5. Kymionis GD., Ide T., Galor A.et al.: Femtosecond-Assisted Anterior Lamellar Corneal Staining–Tattooing in a Blind Eye With Leukocoria. Cornea [online]. Február 2009 [cit. 12 júna 2017]. Dostupné na www.ncbi.nlm.nih.gov/pubmed/19158567
6. Liu X., Shen JH., Zhou Q.et al.: Personalised lamellar keratoplasty and keratopigmentation in Asian corneal leucoma patients. Int J ClinExp Med [online]. Jún 2015 [cit. 12 júna 2017]. Dostupné na: www.ijcem.com/files/ijcem0008318.pdf
7. Rowe FJ., Noonan CP.: Botulinum toxin for the treatment of strabismus. Review. Cochrane Database of Systematic Reviews [online].2017, Issue 3. [cit. 29 júna 2018]. Dostupné na: http://cochranelibrary-wiley.com/doi/10.1002/14651858.CD006499.pub4
8. Stodůlka, P.: Tetováž rohovky. 1. bilaterální česko-slovenské sympozium očních lékařů. Sborník abstrakt, Luhačovice, 6/ 2001.
Labels
OphthalmologyArticle was published in
Czech and Slovak Ophthalmology

2018 Issue 4
-
All articles in this issue
- Diagnosis of Familial Hypercholesterolaemia on First Sight? The Role of the Ophthalmologist in Identifying Patients with Familial Hypercholesterolaemia
- Vertical Strabismus – Indication of Surgical Techniques on the Inferior Rectus Muscle
- Keratopigmentation (Corneal Tattoo) – Our First Experience
- Correction of Myopia and Myopic Astigmatism by Implantation of a Phakic Posterior Chamber Implantable Collamer Lens
- Digital Eye Strain in a Population of Young Subjects
- EFFECT OF MULTIPLE VARIABLES ON THE REFRACTIVE ERROR AFTER CATARACT SURGERY
- Czech and Slovak Ophthalmology
- Journal archive
- Current issue
- About the journal
Most read in this issue
- Vertical Strabismus – Indication of Surgical Techniques on the Inferior Rectus Muscle
- Keratopigmentation (Corneal Tattoo) – Our First Experience
- Diagnosis of Familial Hypercholesterolaemia on First Sight? The Role of the Ophthalmologist in Identifying Patients with Familial Hypercholesterolaemia
- Correction of Myopia and Myopic Astigmatism by Implantation of a Phakic Posterior Chamber Implantable Collamer Lens