The importance of the detail forensic-neuropathological examination in the determination of the diffuse brain injuries
Význam detailního forenzně-neuropatologického vyšetření při diagnostice difuzního poškození mozku
Současná klasifikace rozděluje traumatické poškození mozku na fokální či difúzní poranění a primární či sekundární poškození. V článku chceme zdůraznit význam forenzně-neuropatologického vyšetření při stanovení diagnózy difúzního poranění mozku.
V těchto případech se často nepodaří ani pomocí sofistikovaných klinických vyšetřovacích metod jako CT a MRI, ani rutinním forenzně-patologickým vyšetřením po smrti zjistit ložiskové změny v mozku, přestože se pacient prezentoval těžkou neurologickou poruchou.
U 80 pacientů s uzavřeným poraněním hlavy bylo provedeno forenzně-neuropatologické vyšetření fixovaného mozku a imunohistochemické vyšetření monoklonální protilátkou proti beta-amyloid prekurzor proteinu. U 14 případů (17,7 %) byla absence jakýchkoli masivních intrakraniálních lézí difúzního poranění mozku.
Forenzně-neuropatologické vyšetření bylo jedinou cestou, jak stanovit diagnosu poškození mozku, které způsobilo vážnou neurologickou poruchu a ve většině případů bylo příčinou smrti. Tato metoda již byla zahrnuta do Doporučení č. 99 Evropské rady a tím se stala nevyhnutelnou součástí běžné soudně-lékařské praxe.
Klíčová slova:
difuzní axonální poškození – difuzní vaskulární poškození – uzavřená poranění hlavy – traumatické poškození mozku – difuzní poškození mozku
Authors:
N. Davceva 1; V. Janevska 2; B. Ilievski 2; L. Spasevska 2; R. Jovanovic 2
Authors‘ workplace:
Institute of Forensic Medicine, criminology and medical deontology, Faculty of medicine, “Vodnjanska” No 19, 1000 Skopje, Republic of Macedonia
1; Institute of Pathology, Faculty of medicine, “50 Division”, 1000 Skopje, Republic of Macedonia
2
Published in:
Soud Lék., 57, 2012, No. 1, p. 2-6
Category:
Original Article
Overview
According to the contemporary classification, traumatic brain damage is divided on focal and diffuse brain injuries, and primary and secondary brain damage. The aim of this paper is to emphasize the necessity of the forensic-neuropathological examination in the determination of the diffuse brain injuries. In those injuries frequently neither the most sophisticated clinical-investigation techniques like CT and MRI, nor the routine post-mortem forensic pathological examination, give any results with discovering an intracranial mass lesion, despite the fact that patients had manifested a serious brain failure.
In a series of 80 cases with closed head injuries where forensic-neuropathological examination has been undertaken (examination of a fixed brain tissue and immunohistochemistry using monoclonal antibodies against β-amyloid precursor protein), the occurrence of the diffuse brain injuries in the absence of any other massive intracranial lesion has been established in 14 (17,7%) of the cases. Hence, forensic-neuropathological examination has been the only way to establish the diagnosis of the brain injury that caused a serious brain failure and in most of them occurred as a concrete cause of death. This method has already been affirmed in the forensic medicine science and has been implemented in a Recommendation No 99 of the Council of Europe where medico-legal autopsy rules are given, thus, establishing it as an unavoidable part of the daily forensic medicine practice.
Keywords:
diffuse axonal injury – diffuse vascular injury – closed head injuries – traumatic brain damage – diffuse brain damage.
The forensic medical importance of cranial-cerebral injuries (CCI) lies in the fact that they are the single most important factor in death due to trauma in almost half of all traumatic deaths (1). CCI is a complex entity where injuries of all anatomical structures of the head (scalp, skull, and intracranial structures) have to be analyzed together in the process of the reconstruction of the mechanism of injury and death. Because of the soft consistency and fragility of the brain tissue, liable to a rapid progression of autolision and putrefaction, appropriate examination and more complicated processing techniques are required to establish the diagnosis (1). This paper is focusing on diffuse brain injuries (DBI) and the role of the forensic-neuropathological examination in a process of their diagnosing.
With the introduction of the concept of focal and diffuse brain injuries, it became clear that the final outcome of one particular closed head injury doesn’t depend on the extensity of the local focal lesion as much as it depends on the occurrence of diffuse brain injuries (2,3). Primary diffuse brain injuries as diffuse axonal injury (DAI) and diffuse vascular injurY (DVI) are today clearly defined, both clinically and pathologically (3–6). DBI that are occurring secondarily, as a result of pathophisiologic and biomechanic mechanisms initiated by the primary brain injury, are brain swelling and the hypoxic-ischemic brain lesion.
The remarkable significance of DBI has been stressed by Gennarelli who found that almost 50 % of all cases who sustained closed head injury didn’t show any intracranial mass lesion, both clinically with the most subtle investigation techniques (CT, MRI) or post-mortem, using the routine forensic-medical examination (7). In those cases it is usually concluded that the patient has sustained diffuse brain injuries, which, in order to be diagnosed, appropriate and complete forensic-neuropathological examination is essential.
The necessity of this examination is cited in the Recommendation No 99 adopted by the Committee of Ministers of the Council of Europe on 2 February 1999, about the harmonization of the medico-legal autopsy rules: “In a obvious or suspected head injury (for example if a detailed examination is required or putrefaction is present), fixation of the whole brain is recommended before its dissection” (8).
Recognizing that many of the more challenging problems in forensic practice lie in the field of neuropathology (4), Forensic science international journal published a special issue dedicated to Forensic neuropathology. There has been described the procedure how to efficiently perform a neuropathological examination for an accurate and reliable legal statement (9). Several questions have been cited which have to be answered by the forensic doctor after completed forensic neuropathological examination: 1. Has there been a head injury?; 2. When did it occur?; 3. What were the likely mechanisms of injury?; 4. What is the nature and distribution of the pathologies?; Are there any premorbid lesions that might need to be considered in the clinico-pathological correlations?
What is essential in the procedure of forensic-nauropathological examination is that the most obvious structural damage may not be the most important (10), that’s why one should look actively after changes in the predilection brain regions in a purpose to perceive the diffuse brain injury. Samples from the predilection regions undergo special staining, depending on what has to be visualized with the particular staining technique.
Following new standards established in the field of the forensic neuropathology in the last ten years, the aim of this paper is to present a real necessity of performing forensic-neuropathological examination in the daily forensic practice and particularly, in which cases it is an unavoidable part of the forensic medical examination.
MATERIAL AND METHODS
We investigated a total of 80 cases of fatal closed head injuries with a purpose to set apart and document those cases where brain injury could has been perceived only with complete forensic-neuropathological examination. Those were cases which commonly manifested serious impairment of the brain function leading to death, but none of those cases has shown any intracranial mass lesion (intracranial hemorrhage or focal brain injuries like contusions and intracerebral hemorrhages). Hence, the impairment of the brain in those cases could have happened only as a result of the occurrence of diffuse brain injury.
For investigated 80 cases we obtained the following information: type of the traumatic event causing brain injury (traffic accident, fall or blow); time of survival; the depth of the coma as the most reliable indicator of the impairment of the brain function for cases that survived long enough to be clinically investigated; pathoanatomical feature: presence of scull fractures, intracranial hemorrhage (epidural, subdural or subarachnoid); focal brain damage (contusions and intracerebral hemorrhages) and diffuse brain damage (DAI, DVI, brain swelling and hypoxic-ischemic brain lesion).
Forensic autopsy was performed in all the cases. The injury mechanism was analyzed based on the injuries of the scalp, skull, intracranial structures and the brain tissue. Any presence of subarachnoid hemorrhage, epidural and subdural hematoma, and the presence of the focal injuries to the brain tissue were noted.
This was followed by a forensic neuropathological examination (9) of fixed brains in 10% buffered formalin. Macroscopic examination of 1cm thick coronal sections has been made and documented in photographs. The occurrence of DAI on a macroscopic examination has been perceived by a focal lesion in the corpus callosum or in the dorso-lateral segment of the rostral brain stem (Figure 1). DVI was seen as multiple tiny or spotty hemorrhages throughout the white matter, especially prominent in the frontal and temporal lobes (Figure 4).

Sampling has been done from the brain areas already known to be predilection for the occurrence of diffuse axonal damage: the body and the splenium of the corpus callosum; the posterior limb of the internal capsule; the pons and superior cerebellar peduncles (4).
With a purpose of visualizing the diffuse axonal damage, in addition to the conventional haematoxylin - eosin staining, immunohistochemical staining with application of antibody against β-APP was performed, by the method of Sheriff et al. (11): antigen retrieval in citrate buffer (pH 5.0), incubation with antibody against β-APP (Mouse anti-alzheimer precursor protein A4 monoclonal antibody, clone 22 C 11, diluted 1 : 200, Chemicon International, Temecula, CA) overnight at 4C. The enzyme complex used was ABC (Universal VECTASTAIN ABC-Peroxidase kit, Vector Labs, Burlingame, CA) with a secondary antibody - biotinylated anti-mouse IgG (Biotinylated Anti-mouse IgG, produced in horse, Vector Labs). Diaminobenzidine (Peroxidase Substrate Kit (DAB) Vector Labs) was used for visualization.
On a microscopic examination, DAI was diagnosed with a finding of widespread axonal damage with traumatic pattern throughout the white brain matter including white matter bundles (12, 13). Damaged axons had to be seen as single or small groups of swollen “varicosity”-like β-APP positive axons (Figure 2a) or as “retraction balls” (Figure 2b) diffusely distributed throughout the white matter. This feature had to be seen in at least three different brain regions, of which at least one located above and one below the tentorium (4). DVI on a microscopic examination could have been seen by a feature of pericapilar, periarterious and perivenous hemorrhages.

RESULTS
From a total of 80 investigated cases, in 14 (17.7 %) postmortem diagnosis of the brain injury could has been established only with a complete forensic-neuropathological examination (Table 1).
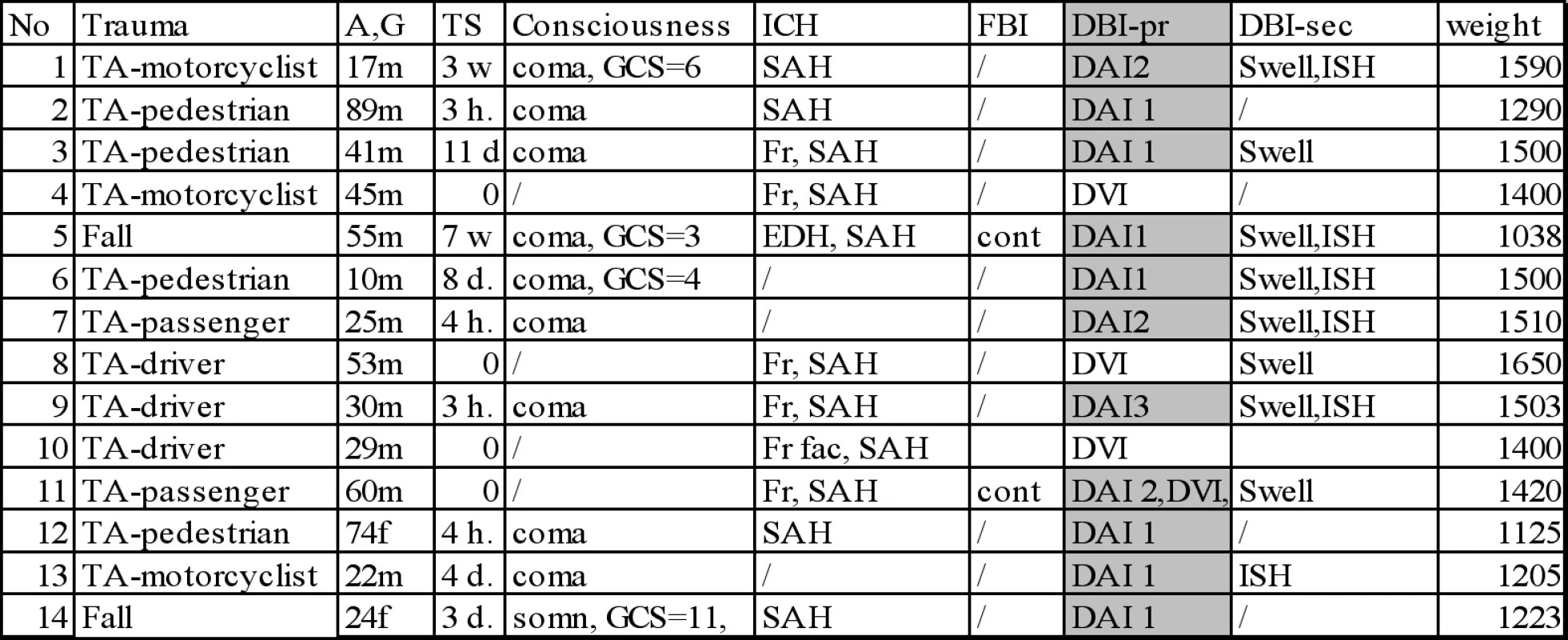
Regarding the type of the trauma, in 12 out of 14 cases closed head injury was caused by traffic accident (4 pedestrian, 2 passengers, 3 motorcyclists, 3 drivers) and in two cases it was caused by fall from a height more than 2 meters. Time of survival ranged between seconds and 1.5 month.
All those cases commonly showed serious impairment of the brain function manifested by the state of the consciousness i.e. 9 out of 14 cases have been in deep coma with GCS (Glasgow Coma Score) between 3 and 7, one case showed upper grade of GCS, and in the rest of cases death occurred before they could have been clinically investigated. With a post-mortem examination, in none of those cases was found any intracranial mass lesion that could have been considered as a cause of death. Regarding the intracranial hemorrhages, none of cases showed the presence of subdural hematoma; one case was survived after surgical evacuation of epidural hematoma, and in 11 cases was found localized circumscript subarachnoid hemorrhage that can’t be considered as cause of death. Concerning the focal brain damage, only two out of 14 cases have shown little contusions restricted to a gray brain matter and in none of the cases had any intracranial hemorrhage.
With a performance of the complete forensic-neuropathological examination by the employed method, in all 14 cases it was established the presence of diffuse brain injury. In 11 cases (13.7 % of 80 investigated cases) the diagnosis of DAI was established, which was perceived with macroscopic examination in cases 1.7 and 11 (lesion in Corpus callosum) and 9 (lesion in the brainstem), and all cases were diagnosed with a microscopic examination by abovementioned criteria. In 5 cases (5 % of 80 cases) the DVI was diagnosed, and in one case the presence of both DAI and DVI was established.
DISCUSSION
Diffuse axonal injury
Our results show that DAI was the sole cause of the impairment of the brain function leading to death in 13.7 % of cases (from a total of 80 cases), and its diagnosis could have been established only with a complete forensic-neuropathological examination. The incidence of DAI in closed head injuries is much higher, between 30 and 50 % (7), but according to the results of this study, in 13.7 % of cases it was the sole patho-anatomical feature of the injury of the brain.
DAI is an acceleration-deceleration injury typical for traffic accidents, but also occurs in cases of fall of a considerable height, where forces of acceleration and deceleration initiate shearing and strain forces with a consecutive degeneration of axons in the white brain matter (14). DAI is clinico-pathologic entity, clinically defined by immediate primary coma leading to death, and pathologically must be diagnosed by the feature of diffuse axonal damage in the white brain matter (3). With those characteristics, DAI frequently occurs as a sole and concrete cause of death, from where is its big forensic medical significance. Additionally, its occurrence also points to a certain biomechanism of the head trauma.
On a macroscopic examination DAI can be perceived by the feature of the focal lesion in corpus callosum, defined as second grade of DAI (grading system by Adams et al. 1989) (15), and in the dorso-lateral segment of the rostral brainstem, defined as third grade of DAI. Frequently there isn’t any macroscopic feature, and the feature that is very indicative of the occurrence of DAI is the gliding hemorrhages or slit-like hemorrhages in the white brain matter (Figure 3).


The diagnosis must be confirmed by a microscopic feature of damaged β-APP positive axons, diffusely spread in the white brain matter with traumatic pattern and distribution (3,12,13). Damaged axons should be seen as sole or small groups of swollen “varicosity”-like axons or as torn and retracted like retraction balls.
Diffuse vascular injury
DVI is a kind of diffuse brain injury typical for cases where head injury obviously occurred as a result of the impact of the high intensity force. The medical doctor will perceive extensive injuries to the scalp and the bone tissue, but almost nothing to the brain tissue, except for minute spotty hemorrhages diffusely arranged throughout the white brain matter, which are particularly pronounced in the front poles of the frontal and temporal lobes.
This kind of injury is classically described as incompatible with life and is probably restricted to patients who die very soon, several hours the longest, after head injury (6). A research of 11 cases with DVI has shown that the longest time of survival has been 4 hours, and 73 % of cases died instantly (16). The longest time of survival reported is 11 hours (17).
DVI with its short time of survival frequently occurs as a concrete cause of death in head trauma; that is why the diagnosing of the DVI in forensic medical practice has a big forensic medical significance and importance. Due to the abovementioned fragility and susceptibility to autolysis of the brain tissue, the examiner may overlook minor spotty hemorrhages on a fresh tissue and this is the reason why the examination must be done to a fixed brain tissue.
Concerning the mechanism of DVI, some authors equalized the DVI and DAI occurrence mechanisms with a conclusion that both lesions are triggered by the same mechanism, pointing out that the degree of axonal and vascular lesion is determined by the intensity of the acceleration of the head (18). The same research paper reports that DVI as an entity is restricted to traffic accident cases. However, another research undoubtedly indicate the presence of DVI not only in traffic accident cases, but also in cases of a falling of a height, and a strong correlation between DVI and fractures of the skull, as a proof that the direct impact of a force upon the head plays a great role in a process of the occurrence of DVI (16). Additionally, unlike DAI that was clearly proved and produced in experiments with subhuman primates, DVI has hitherto not been produced in the same manner, which is why it still remains an enigma in the forensic neuropathology regarding the mechanism of occurrence.
In conclusion, diffuse brain injuries occur as a concrete and sole cause of death in nearly every fifth case with closed head injury. In those cases there isn’t any intracranial mass lesion and the diagnosis of the diffuse brain injury can be established only with a complete forensic-neuropathological examination.
The procedure of forensic-neuropathological examination is scientifically ascertained and affirmed in the forensic medicine and already implemented in the Recommendation No 99 of the Council of Europe about the medico-legal autopsy rules.
Hence, employing complete forensic-neuropathological examination is essential for all cases with closed head injury, especially where this injury is not obvious but suspected, why it must be considered as unavoidable part of the daily forensic medicine practice.
Address for correspondence:
Dr. Davceva Natasha
Institute of Forensic Medicine, criminology and medical deontology
Faculty of medicine Skopje
“Vodnjanska” No 19, 1000 Skopje, Republic of Macedonia
tel: + 389 2 3177 044, fax: + 389 2 3178 831, mob: + 389 70 958 324
e-mail: drdavcevamk@yahoo.com, drdavceva@yahoo.com
Sources
1. Kalimo H. Forensic neuropathology: an important heading in legal medicine. Forensic Sci Int 2004;146 : 71–72.
2. Graham DI, Gennarelli TA. McKintosh TK. Trauma in: Greenfield’s neuropathology 7-th edn. E.Arnold: London; 2002 : 823 – 898.
3. Geddes JF, Whitwell HL, Graham DI. Traumatic axonal injury: practical issues for diagnosis in medicolegal cases. Neuropath Appl Neurobio 2000; 26 : 105–116.
4. Geddes JF, Vowles GH, Beer TW, Ellison DW. The diagnosis of diffuse axonal injury: implications for forensic practice. Neuropath Appl Nevrobiol. 1997; 23 : 339–347.
5. Omalu BI. Diagnosis of traumatic diffuse axonal injury. Letter to the editor. Am J Forensic Med Pathol 2004; 25 (3): 270–272.
6. Pearl GS. Traumatic neuropathology. Clinics Lab Med. 1998; (18): 39–64.
7. Gennarelli TA. The spectrum of traumatic axonal injury. Neuropathol Appl Neurobiol. 1996; 22 : 509–513.
8. Brinkmann B. Harmonisation of medico-legal autopsy rules Int J Leg Med. 1999; 113 : 1–14.
9. Kalimo H, Saukko P, Graham D Neuropathological examination in forensic context. Forensic Sci Int. 2004; 146 : 73–81.
10. Graham DI, Adams JH, Nicoll JA, Maxwell WL; Gennarelli TA. Brain Pathol. 1995; 5(4):397–406.
11. Sheriff FE, Bridges LR, Sivaloganatham S Early detection of axonal injury after human head trauma using immunocytochemistry for B-amyloid precursor protein. Acta Neuropathol. 1994; 87 : 55–62
12. Graham DI, Smith C, Reichard R et al. Trials and tribulations of using ß-amyloid precursor protein immunohistochemistry to evaluate traumatic brain injury in adults. Forensic Sci Int 2004; 146 : 89–96.
13. Reichard RR, Smith C, Graham DI The significance of β-APP immunoreactivity in forensic practice. Neuropathol Appl Neurobiol 2005; 31 : 304–313.
14. Povlishock JT, Jenkins JW. Are the pathobiological changes evoked by traumatic brain injury immediate and irreversible? Brain Pathol 1995; 5 : 415–426.
15. Adams JH, Doyle D, Ford I, Gennarelli TA, Graham DI. Diffuse axonal injury: definition, diagnosis and grading. Histopathol. 1989; 15 : 49–59.
16. Davceva N. Dilemmas surrounding the occurrence mechanism of cerebral diffuse vascular injury. Romanian J Leg Med. 2010; 18 - 2 : 115–121.
17. Dolinak D, Matshes E. Medicolegal neuropathology. CRC Press. 2002 New York.
18. Pittella JE, Gusmao SN. Diffuse vascular injury in fatal road accident victims: its relationship to diffuse axonal injury. J Forensic Sci. 2003; 48 (3): 626–630.
Labels
Anatomical pathology Forensic medical examiner ToxicologyArticle was published in
Forensic Medicine

2012 Issue 1
-
All articles in this issue
- Evaluation of childhood medicolegal autopsies in Bratislava and Trnava regions, Slovakia
- The importance of the detail forensic-neuropathological examination in the determination of the diffuse brain injuries
- Immunohistochemistry and serum values of S-100B, glial fibrillary acidic protein, and hyperphosphorylated neurofilaments in brain injuries
- Forensic Medicine
- Journal archive
- Current issue
- About the journal
Most read in this issue
- Immunohistochemistry and serum values of S-100B, glial fibrillary acidic protein, and hyperphosphorylated neurofilaments in brain injuries
- The importance of the detail forensic-neuropathological examination in the determination of the diffuse brain injuries
- Evaluation of childhood medicolegal autopsies in Bratislava and Trnava regions, Slovakia









