Multiple sclerosis in the otoneurology outpatient clinic: interdisciplinary cooperation between otoneurologist and neurologist
Problematika roztroušené sklerózy v otoneurologické ambulanci, mezioborová spolupráce otoneurologa a neurologa
Úvod: Roztroušená skleróza (RS) je chronické víceložiskové zánětlivé onemocnění CNS s podílem autoimunitních i neurodegenerativních dějů v patogenezi. V ambulanci otoneurologa jsou vyšetřováni pacienti s nedoslýchavostí, tinitem, vertigem, kteří v konečném důsledku mohou být nově diagnostikovanými nemocnými s roztroušenou sklerózou. Otoneurolog může být tím prvním lékařem, který vysloví suspekci na roztroušenou sklerózu a odešle pacienta na MR a neurologické vyšetření. Včasná diagnostika a následná léčba může znamenat oddálení trvalé invalidity. Cíl: Analýza výskytu pacientů s RS v otoneurologické ambulanci během dvacetiletého období. Zvýšit povědomí o diagnóze RS v otoneurologické ambulanci. Metoda a materiál: Retrospektivně byla vyhodnocena data 11 pacientů (0,18 %) (5 mužů, 6 žen, věk 25–58 let) s roztroušenou sklerózou nebo suspekcí na roztroušenou sklerózu z celkového počtu 6 000 nově vyšetřených pacientů v otoneurologické ambulanci (v období 2000–2021). Výsledky: U 11 pacientů byla suspekce na roztroušenou sklerózu či probíhající roztroušenou sklerózu. U 4 pacientů otoneurologické vyšetření přispělo k prvozáchytu roztroušené sklerózy otoneurologem. Prvním příznakem RS byla nedoslýchavost, tinitus, instabilita, postinfekční porucha vizu. Závěr: Otoneurolog by měl vždy myslet na to, že náhlá ztráta sluchu, tinitus, vertigo mohou být prvním projevem roztroušené sklerózy. Včasná diagnostika roztroušené sklerózy zvyšuje léčebnou šanci pacienta na zpomalení vývoje nemoci. Terapie zahájená v době prvních klinických příznaků má vyšší úspěšnost stran oddálení invalidity. V rámci diagnostiky RS je velmi důležitá interdisciplinární spolupráce otoneurologa s neurologem.
Klíčová slova:
roztroušená skleróza – percepční nedoslýchavost – tinitus – závrať – otoneurologie
Authors:
Pastorková N. 1; Holý R. 2,3; Procházková K. 3,4; Mayerová K. 1; Vašina L. 1; Lacman J. 5; Musilová Š. 1; J. Astl 2,3
Authors‘ workplace:
Military University Hospital Prague, Department of Neurology
1; Military University Hospital Prague, Department of Otorhinolaryngology and Maxillofacial Surgery
2; 3rd Faculty of Medicine, Charles University, Prague
3; University Hospital Královské Vinohrady, Prague, Department of Otorhinolaryngology 3FM CU and UHKV, Prague
4; Military University Hospital Prague, Department of Radiodia gnostics
5
Published in:
Otorinolaryngol Foniatr, 70, 2021, No. 3, pp. 161-166.
Category:
Overview
Introduction: Multiple sclerosis (MS) is a chronic multifocal inflammatory disease affecting the CNS, with autoimmune and neurodegenerative processes involved in its pathogenesis. Otoneurology outpatient clinic patients presenting with hearing loss, tinnitus, and vertigo may eventually be newly diagnosed MS patients. An otoneurologist specialist may be the first physician to suspect MS and refer the patient for an MRI and neurological examination. Early diagnosis and subsequent treatment of MS can delay permanent disability. Aim: Analysis of the incidence of MS patients in an otoneurological outpatient clinic during a twenty-year period. To increase the otoneurologists’ awareness of MS diagnosis. Methods and materials: Of 6,000 patients, who were newly examined in an otoneurology outpatient clinic between 2000 and 2021, data of 11 patients (0,18%) (5 male/6 female, aged 25–58 years) with MS or suspected of MS were retrospectively evaluated. Results: In 11 patients, MS was suspected or ongoing. In 4 of those patients, otoneurological examination contributed to the first detection of MS by an otoneurologist. The first MS symptoms included hearing loss, tinnitus, instability, and post-infection visual disorder. Conclusion: The otoneurologist must consider that sudden hearing loss, tinnitus, and vertigo may be the first manifestations of MS. Early diagnosis of MS increases the likelihood that with treatment, the progression of the disease will be slowed. Interdisciplinary cooperation between the otoneurologists and neurologists is very important for the diagnosis of MS.
Keywords:
Multiple sclerosis – sensorineural hearing loss – Tinnitus – Vertigo – otoneurology
Introduction
Multiple sclerosis (MS) is a chronic multifocal inflammatory disease of the CNS with a share of autoimmune and neurodegenerative processes in pathogenesis [1].
McDonald diagnostic criteria are used to diagnose MS. McDonald diagnostic criteria for MS are clinical, radiographic and laboratory criteria used in the diagnosis of multiple sclerosis (Tab. 1). They were originally introduced in 2001 and revised multiple times, most recently in 2017 [2].
Tab. 1. K diagnostice MS se používají diagnostická kritéria McDonald [2].
![McDonald diagnostic criteria are used to diagnose MS [2].<br>
Tab. 1. K diagnostice MS se používají diagnostická kritéria McDonald [2].](https://www.prelekara.sk/media/cache/resolve/media_object_image_small/media/image_pdf/de0e2ea869778542ba0efb2ef754d15c.png)
If MS is suspected by virtue of a clinically isolated syndrome (CIS) but the 2017 McDonald criteria are not completely met, the diagnosis is ‘possible MS’ [2].
An otoneurologist may meet (infrequently) with a patient who has multiple sclerosis (MS) in an otoneurology (OTN) outpatient clinic during the examination of patients with cochleovestibular disorders who suffer from idiopathic sensorineural hearing loss (ISSNHL), tinnitus, vertigo or instability. Similarly, in patients with already diagnosed MS, an otoneurologist may encounter sudden cochleovestibular symptoms such as deafness, tinnitus and various types of vertigo/instability. Other OTN symptoms that may be caused by MS: dysphonia, dysarthria, dysphagia, olfactory change, trigeminal neuralgia, paresis n. VII, deterioration in the smell functions [1].
MS and brain stem evoked response audiometry (BERA):
Some publications report that in patients without a clinically manifest brainstem lesion, abnormal BERA may reveal clinically silent deposits and demonstrate dissemination of the demyelination process. The findings of the BERA examination are either completely normal or clearly pathological [1, 3].
According to Pichanič, among the initial most common symptoms are eye disorders – retrobulbar and intraocular neuritis. The functioning of the cranial nerves – most often the optic, facial and statoacoustic nerves – is usually disturbed [3]. Deafness is quite rare. A larger deposit of demyelination can cause hearing damage on both sides. If unilateral deafness develops, the onset is abrupt and it progresses within two days. In the MS group, 40% of the patients have significant hearing disturbance compared to the control group [3]. Tinnitus – the subjective sensation of noise in the ear – is common [3].
Vestibular symptomatology counts among the early symptoms of the disease, therefore videonystagmographic (VNG) examination is an important method [3, 4].
In patients with MS, vertigo often has the characteristics of a feeling of insecurity, a sinking
falling, the feeling of being on a ship. Sometimes there is nausea, vomiting [3, 4]. Various abnormalities of eye movements are described in VNG tests. Examination of saccadic movements and smooth pursuit eye movements shows these are often disrupted and disintegration is described [3, 4]. Spontaneous nystagmus (Ny) may be seen in dizziness. It can be part of Charcot‘s triad – staccato speech, intention tremor and nystagmus. Internuclear ophthalmoplegia causes various types of spontaneous nystagmus. Coarse horizontal nystagmus and gaze evoked nystagmus on one or both sides are among the most commonly reported [3, 4]. Isolated vertical nystagmus upwards can also be captured [3–6].
In the caloric test, the literature describes abnormal reactivity of hyperreflexia, hyporeflexia and a directional predominance of nystagmus. There are frequent abnormalities of optokinetic nystagmus – rhythm disorders and inversion [3, 6].
Materials and methods
Retrospectively evaluated data of 11 patients (6 female and 5 male) with suspected or proven MS in the OTN outpatient clinic. All the patients were examined in the period from 1/2000 to 3/2021 at the OTN outpatient clinic and subsequently at the neurology outpatient clinic. Age range 25–58 years. The average age was 38 years. During the stated period, 6,000 new patients were examined in the OTN outpatient clinic. In the OTN outpatient clinic, we examine an average of 300 new patients per year. The patients underwent otoneurological and audiological examinations: ENT examination, pure tone audiometry (125–8,000 Hz), tympanometry, examination of stapedial reflex, tinnitus masking, brain stem evoked response audiometry (click – 90dB) (BERA), videonystagmography (VNG), posturography. MRI scans of the brain were performed. Subsequently, neurologic examination at the neurology outpatient clinic followed. Lumbar puncture (LP) – cerebrospinal fluid was collected by a neurologist. Evaluation of whether the patient meets/does not meet the McDonald criteria.
Our study was followed according to the Declaration of Helsinki. Due to the retrospective type and character of the study, approval by the local ethics committee was not required (retrospectively evaluated small cohort of 11 patients).
Results
Over a 21-year period, only 11 patients (from 6,000 patients = 0.18%) with suspected MS or proven MS were detected in the OTN outpatient clinic.
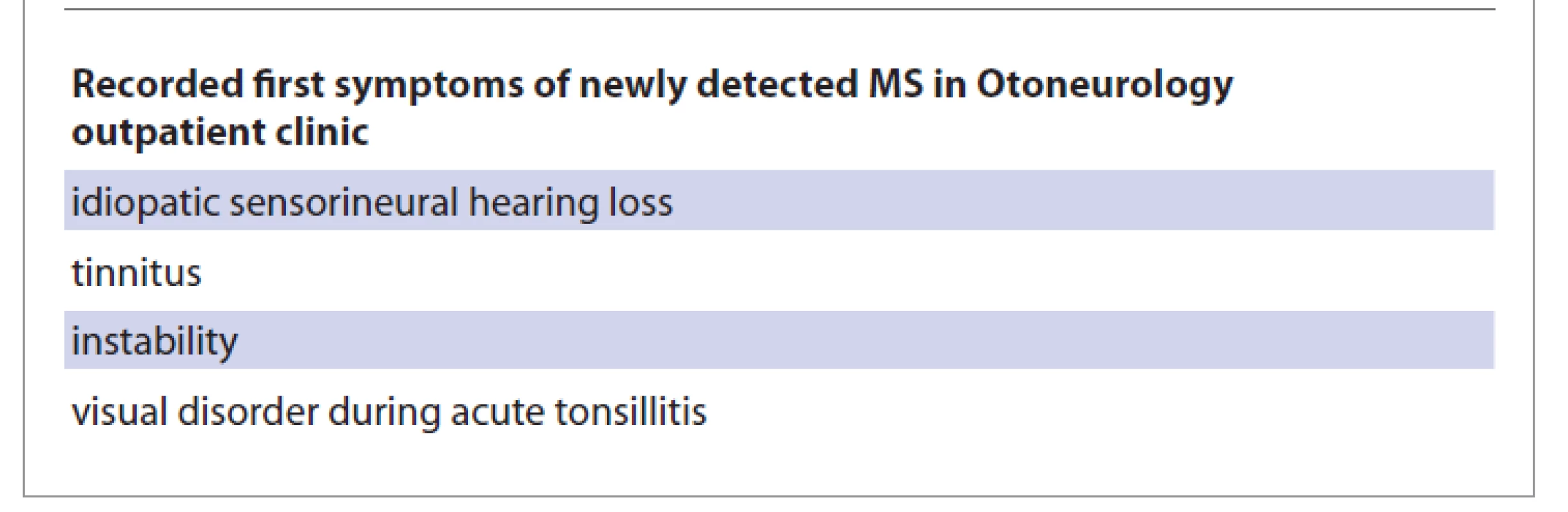
In 4 patients, examination in the OTN outpatient clinic contributed to the first capture of MS by an otoneurologist. The first symptoms of MS were hearing loss, tinnitus, instability, post-infection vision disorder during acute tonsillitis (Tab. 2).
Tab. 2. Vyšetření v otoneurologické ambulanci přispělo k prvnímu časnému
zachycení MS otoneurologem. První příznaky nově zjištěné RS v otoneurologické
ambulanci.
Sudden deafness has also been reported in long-term MS.
Overview of patients
Female patient No. 1 (age: 25 years): first symptom of ISSNHL, pathological record of BERA (invaluable sinusoid), instability, brain MRI – demyelination, first capture of MS by the otoneurologist.
McDonald criteria at the time of OTN examination: not fulfilled
Female patient No. 2 (age: 50 years): MS lasting 25 years, acute ENT symptom ISSNHL (deafness), tinnitus, rotatory vertigo, irritating spontaneous nystagmus. After corticoid treatment and hyperbaric oxygen therapy, hearing returned to normal, vertigo disappeared.
McDonald criteria at the time of OTN examination: fulfilled
Female patient No. 3 (age: 43 years): first symptom of sensorineural hearing loss since childhood, normal BERA, normal VEP, MRI non-specific, lumbar puncture recommended by MS centre, MS confirmed according to the results of the lumbar puncture procedure.
Conclusion: clinically isolated syndrome (CIS).
McDonald criteria at the time of OTN examination: not fulfilled, only CIS
Female patient No. 4 (age: 27 years): The first symptom – vision disorder during acute tonsillitis, normal hearing, without vertigo. Brain MRI ordered. MR result: suspected MS. In the white matter of both cerebral hemispheres multiple hypersignal bearings with a diameter of about 10 mm. Some of the lesions have indicated mild perifocal oedema LP – the cerebrospinal fluid finding confirmed MS.
First capture of MS by the otoneurologist. McDonald criteria at the time of OTN examination: fulfilled
Male patient No. 5 (age: 40 years): referred from the MS centre for further examination for tinnitus and instability. Pure tone audiometry, VNG, posturography tests without pathology.
Brain MRI second reading – non-specific finding, MS not proven.
McDonald criteria at the time of OTN examination: not fulfilled
Female patient No. 6 (age: 58 years): the first sign – incontinence, diplopia five years later, paresis n. abducens (VI cra - nial nerve), new symptom: tinnitus. Audiometry without hearing loss, BERA: asymmetry of intervals I–III, III–V, VNG spontaneous horizontal nystagmus – to the left, VEP abnormal recording of prolonged latency of both sides of the P100 wave. LP – the cerebrospinal fluid finding confirmed MS. MS confirmed by a neurologist.
McDonald criteria at the time of OTN examination: fulfilled
Male patient No. 7 (age: 29 years): post-stress tinnitus, corticoid treatment and hyperbaric oxygen therapy without effect, MRI suspicion of demyelination, LP – cerebrospinal fluid negative, second reading of brain MR – MS unlikely – small deposits nonspecific.
MS not confirmed.
McDonald criteria at the time of OTN examination: not fulfilled
Male patient No. 8 (age: 49 years): long-term sensorineural hearing loss with tinnitus, intensification of tinnitus after 6 years, pathological record of BERA (left side – wave III and V. latency extension), VNG: caloric hyporeflexion of the right labyrinth.
Brain MRI – In T2W and FLAIR multiple hypersignal small deposits in the white matter of both cerebral hemispheres up to 5 mm in size periventricular and subcortical. LP – finding MS positive, first capture of MS by the otoneurologist.
McDonald criteria at the time of OTN examination: fulfilled
Female patient No. 9 (age: 34 years): tinnitus in the right ear from a young age, the first symptom of MS – paresis of the upper limb, MR of the brain and spinal cord – conclusion: multiple deposits in the white matter supratentorial and infratentorial and in the cervical spinal cord. MS confirmed by a neurologist. 11 years after the diagnosis of MS, rotatory vertigo has appeared. OTN tests: Audiometry, BERA, VNG and posturography without pathology.
McDonald criteria at the time of OTN examination: fulfilled
Male patient No. 10 (age: 30 years): the first symptom ISSNHL, tinnitus and instability.
Pure tone audiometry: sensorineural hearing loss in the left ear, VNG without pathology, posturography – anteroposterior titubation. Corticosteroid treatment and hyperbaric oxygen therapy without effect. Brain MRI: in the T2W image multiple hypersignal deposits in the white matter of both cerebral hemispheres up to 10 mm in size. The lesions are located periventricularly in the deep white matter as well as subcortically and supratentorially. MR cervical spine: Conclusion: Demyelinating plaque on the left in the posterior spinal cord 15 x 3 x 2 mm without postcontrast saturation. LP – the cerebrospinal fluid finding confirmed MS, first capture of MS by the otoneurologist.
McDonald criteria at the time of OTN examination: fulfilled
Male patient No. 11 (age: 29 years): at 27 years of age (2019) ISSNHL with tinnitus of the right ear, treatment of vasodilatory infusion and hyperbaric oxygen therapy with effect, hearing recovered, tinnitus persists. Brain MR – no signs of MS, secondary finding of two lipomas (quadrigemine cistern area and left orbit tip). After two years (January 2021) disorder of left eye pressure, new tinnitus of the left ear, headache parietally left side. Ophthalmological examination – perimeter – failure in the upper half of the left eye, retrobulbar neuritis of the left eye. ENT examination – sensorineural hearing loss and tinnitus bilaterally, pathological BERA (bilaterally elongated wave III). Neurological examination – hyperreflexia on the lower limbs with irritative phenomena. New MR of the brain and cervical spine – in the T2W image a unique hypersignal lesion 5 x 3 mm frontally paraventricularly left. LP – cerebrospinal fluid positivity in the sense of MS, oligoclonal intrathecal IgG synthesis. Neurological conclusion: clinically isolated syndrome (CIS). Therapy – corticosteroid pulse (Solu-Medrol). Ordered consultation in MS centre.
McDonald criteria at the time of OTN examination: yet not fulfilled only CIS
Discussion
In the OTN outpatient clinic, we can meet with patients with an established MS diagnosis. Some of the cochleovestibular symptoms may appear de novo. This way, we have encountered sudden deafness, tinnitus and balance disorder. The otoneurologist must always consider MS in the differential diagnosis of otoneurological symptoms.
However, an otoneurologist can also be the first physician to express suspicion of MS during an OTN examination. Such suspicion is then confirmed after the completion of further examinations. In the OTN outpatient clinic, we examine an average of 300 new patients per year. In the last 5 years, intensive interdisciplinary cooperation between a neurologist and an otoneurologist has been introduced in our hospital, which is constantly deepening. Its goal is to increase the frequency of detection of early stages of MS and CIS.
MS detected early in the OTN outpatient clinic means an opportunity for the patient to delay the development of the disease. This is when starting the treatment of MS at the time of the first clinical symptoms (CIS). This indicates the importance of early diagnosis of MS.
In four of the cases we recorded in our patients, the first symptom of MS was tinnitus, sensorineural hearing loss, instability or post-infectious vision disorder.
Otoneurologists Hahn, Alpini and Ozunlu [6, 8, 9] indicate that MS begins at a younger age, affecting mainly women. Among the typical disorders are optic nerve neuritis, sensory and motor disorders, as well as cerebellar disorders. Equilibrium oculomotor disorders are also common when spontaneous central-type nystagmus, optokinetic disorder and internuclear ophthalmoplegia are detected in particular [6, 8, 9].
In our cohort of 11 patients, spontaneous nystagmus was detected only once in VNG, in a female patient with a sudden onset of deafness and a pre-existing diagnosis of MS.
According to Havrdová [10], the following disorders of the vestibular system are typical in patients with MS – dizziness, a feeling of rotation and insecurity in space. Then there is nystagmus. Havrdová further states that the vestibular nuclei and brainstem pathways are affected, which leads to the central vestibular syndrome that we see frequently in MS [9].
Čada et al. [4] state that any nystagmus other than the horizontal-rotational type should be suspected of central aetiology. In terms of their duration, vertigo-associated problems in MS are reported to last for days [4]. The instability we detected in our patients in four cases was one of the first symptoms that lasted for weeks, months or years.
The Eker et al. case report describes a sudden hearing loss to be a manifestation of MS [11].
Japanese authors report ISSNHL in six patients (3.5%) in a cohort of 173 patients with MS [12]. According to de Seze et al., ISSNHL resulting from the disease in the first year could be a good prognostic factor. In their cohort of 400 MS patients, sudden hearing loss occurred in 3.5% [13].
According to Di Stadio et al. [14], ISSNHL is a relatively common symptom (in 17%) in the initial phase of MS. The authors emphasise that in practice, an otorhinolaryngologist should always consider MS in young women with ISSNHL without a previous history of hearing disorders [14].
In a cohort of our 11 patients, ISSNHL was observed in three cases. Once it was the first symptom of MS. And once, deafness was recorded in a patient who had been suffering from MS for 25 years. After treatment (corticosteroids, vasodilator infusions, hyperbaric oxygen therapy) the hearing was completely restored ad integrum. In their cohort of 32 patients with MS, Polish authors describe tinnitus in 6.2% of them [15].
Australian authors describe a case report of an 11-year-old girl whose tinnitus and hearing loss were the first symptoms of MS [16]. In our group of 11 patients, we recorded tinnitus in three patients as one of the first symptoms of MS.
The most common finding of the BERA examination is a decrease in the amplitude of the V-wave, or the absence of a V-wave. In other cases, the absolute latency may be prolonged or the interpeak intervals I–III and III–V may be prolonged [1, 17,18]. In our group of 11 patients we recorded abnormal BERA in three patients. MS was confirmed in all of these patients. Our pathologic findings of the BERA examination: invalu - able sinusoid; asymmetry of intervals I–III, III–V; left side-wave III and V latency extension. Normal findings of the BERA examination: in two patients with confirmed MS.
Conclusions
Otoneurologists must consider MS in the differential diagnosis of cochleo-vestibular diseases. Sudden sensorineural hearing loss, tinnitus and instability/vertigo may be the first symptoms of MS. Sudden deafness may recur in ongoing MS.
Early diagnosis of a patient with MS in the outpatient clinic of an otoneurologist increases the patient‘s chances of slowing the progression of the disease.
Regarding the diagnosis of MS, the interdisciplinary cooperation of an otoneurologist with a neurologist is very important. This cooperation is constantly deepening and its goal is to increase the frequency of detection of early stages of MS and CIS.
Conflict of interest
All the authors declare that in connection with the topic, origin and publication of this manuscript they have no conflicts of interest and the origin of the manuscript was not supported by any pharmaceutical company.
ORCID autorů
N. Pastorková ORCID 0000-0002-5970-5131,
R. Holý ORCID 0000-0003-1112-6197,
J. Lacman ORCID 0000-0001-7439-1161,
J. Astl ORCID 0000-0002-8022-0200.
Submitted: 30. 3. 2021
Accepted: 1. 6. 2021
as. MUDr. Richard Holý, Ph.D.
Klinika otorinolaryngologie a maxilofaciální chirurgie
3. LF UK a ÚVN
U vojenské nemocnice 1200
169 02 Praha 6
Sources
1. MacMahon H, El Refaie A. The audiovestibular manifestations as early symptoms of multiple sclerosis: a scoping review of the literature. Ir J Med Sci 2021. Online ahead of print. Doi: 10.1007/s11845-021-02508-3.
2. Thompson AJ, Baranzini SE, Geurts J et al. Multiple sclerosis. Lancet 2018; 391 (10130): 1622–1636. Doi: 10.1016/S0140-6736 (18) 30 481-1.
3. Pichanič M. Klinická otoneurológia. Martin: Osveta 1992.
4. Čada Z, Černý R, Čakrt O et al. Závratě. Tobiáš 2017.
5. Bischoff C, Schreiber H, Bergmann A. Background information on multiple sclerosis patients stopping ongoing immunomodulatory therapy: a multicenter study in a community-based environment. J Neurol 2012; 259 (11): 2347–2353. Doi: 10.1007/s00415-012-6499-1.
6. Alpini D, Caputo D, Hahan A et al. Grading brainstem involvement in multiple sclerosis – by means of electro-oculography. J Neurovirol 2000; 6 Suppl 2: S156–S159.
7. Sasaki O, Ootsuka K, Taguchi K et al. Multiple sclerosis presented acute hearing loss and vertigo. J Otorhinolaryngol Relat Spec 1994; 56 (1): 55–59. Doi: 10.1159/000276609.
8. Ozunlu A, Mus N, Gulhan M. Multiple sclerosis: a cause of sudden hearing loss. Audiology 1998; 37 (1): 52–58. Doi: 10.3109/00206099809072961.
9. Hahn A. Otoneurologie. Praha: Grada 2015.
10. Havrdová E. Roztroušená skleróza. Cesk Slov Neurol N 2008; 71/104 (2): 122–132.
11. Eker A, Kaymakamzade B, Kurne AT et al. Sudden Sensoryneural Hearing Loss As a Rare Attack Type in Multiple Sclerosis. Noro Psikiyatr Ars 2018; 55 (4): 380–382. Doi: 10.5152/npa. 2017.19270.
12. Tanaka M, Tanaka K. Sudden hearing loss as the initial symptom in Japanese patients with multiple sclerosis and seropositive neuromyelitis optica spectrum disorders. J Neuroimmunol 2016; 298 : 16–18. Doi: 10.1016/j.jneuroim.2016.06.004.
13. de Seze J, Borgel F, Brudon F. Patient perceptions of multiple sclerosis and its treatment. Patient Prefer Adherence 2012; 6 : 263–273. Doi: 10.2147/PPA.S27038.
14. Di Stadio A, Dipietro L, Ralli M et al. Sudden hearing loss as an early detector of multiple sclerosis: a systematic review. Eur Rev Med Pharmacol Sci 2018; 22 (14): 4611–4624. Doi: 10.26355/eurrev_201807_15520.
15. Jozefowicz-Korczynska M, Lukomski M. Neuro-otologic findings in multiple sclerosis. Pol Merkur Lekarski 2005; 19 (111): 423–425.
16. Rodriguez-Casero MV, Mandelstam S, Kornberg AJ et al. Acute tinnitus and hearing loss as the initial symptom of multiple sclerosis in a child. Int J Pediatr Otorhinolaryngol 2005; 69 (1): 123–126. Doi: 10.1016/j.ijporl.2004.08.006.
17. Bareš M. Evokované potenciály v diagnostice roztroušené sklerózy mozkomíšní. Neurol Praxi 2002; 3 (5): 244–248.
18. Jurovčík M, Kabelka Z, Myška P et al. SSEP – nová objektivní metoda vyšetření sluchu. Otorinolaryngol Foniatr 2001; 50 (2): 95–98.
Labels
Audiology Paediatric ENT ENT (Otorhinolaryngology)Article was published in
Otorhinolaryngology and Phoniatrics

2021 Issue 3
-
All articles in this issue
- The professional journal Otorhinolaryngology and Phoniatrics celebrates 70 years
- Acute vertigo in the ENT emergency
- Evaluation of speech in patients after cochlear implantation – Motol Speech Scale
- Congenital malformations of the inner ear
- Gastric choristoma of hypopharynx in neonate
- Erdheim-Chester disease – case report
- Ultrasound-guided percutaneous ethanol injection therapy of neck cysts as an alternative to surgery
- Komentář ke článku „Hodnocení řeči u pacientů po kochleární implantaci – Motol Speech Scale“
- Odpověď autorů na komentář ke článku „Hodnocení řeči u pacientů po kochleární implantaci – Motol Speech Scale“
- Odešel prim. MUDr. Jiří Sušický
- Vzpomínka na MUDr. Luďka Šefce
- Vzpomínka na doc. MUDr. Miloslava Hroboně, CSc.
- Multiple sclerosis in the otoneurology outpatient clinic: interdisciplinary cooperation between otoneurologist and neurologist
- Otorhinolaryngology and Phoniatrics
- Journal archive
- Current issue
- About the journal
Most read in this issue
- Congenital malformations of the inner ear
- Acute vertigo in the ENT emergency
- Ultrasound-guided percutaneous ethanol injection therapy of neck cysts as an alternative to surgery
- Evaluation of speech in patients after cochlear implantation – Motol Speech Scale
