-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
HYPERBARIC OXYGENOTHERAPY AS A POSSIBLE MEANS OF PREVENTING ISCHEMIC CHANGES IN SKIN GRAFTS USED FOR SOFT TISSUE DEFECT CLOSURE
Autoři: J. Švehlík Jr. 1; M. Zábavníková 1; Š. Guzanin 1; G. Švehlíková 2; Sr. J. Švehlík 2
Působiště autorů: Clinic of Plastic, Reconstructive and Aesthetic Surgery, University Hospital of L. Pasteur and Medical Faculty of UPJŠ, Košice, and 1; Center for Hyperbaric Oxygenotherapy, Zdravotnícke zariadenie Košice-Juh, Slovakia 2
Vyšlo v časopise: ACTA CHIRURGIAE PLASTICAE, 49, 2, 2007, pp. 31-35
INTRODUCTION
The exploitation of skin grafts of various thickness in the field of plastic and general surgery is one option for soft tissue and skin defect closure in all body regions where it is not suitable to use a local or distant flap. The plastic surgeon is very often confronted with this operation algorithm, the only variation being whether he uses a split skin graft or a full thickness graft. An aseptic
approach during the operation, precise preparation of recipient bed by means of haemostasis, taking the most convenient part of the skin (character, structure and thickness), its preparation and subcutaneous fat abrasion, proper fixation on the recipient area and partial immobilization of the body are the essential principles and requirements (1). Even if a surgeon follows these rules,
his attempt is often associated with graft failure (partial or total) caused by graft ischemia and necrosis, often with concomitant bacterial infection – according to various surgical departments, this can be up to 21% (2).Transferred tissues are characterized by low oxygen tension, often below 15 mm Hg. Oxygen tension of about 30–40 mm Hg is substantial for proper collagen synthesis and fibroblasts proliferation. As fibroblast is a facultative anaerobic cell its stimulation is caused by either hypoxia or/and hyperoxia (3).
One of the possible methods positively affecting the amount of accepted skin grafts is to include hyperbaric oxygenotherapy (HBO) in the therapeutic process of the patients. This treatment is responsible for increasing the fraction of physically dissolved oxygen in blood plasma and interstitial fluid to a concentration twenty times higher than under physiological conditions. Theoretically
it would be possible to provide tissue oxygenation without presence of hemoglobin (4).HBO also significantly improves direct oxygen diffusion through the epidermal barrier. Oxygen diffusion is directly proportional to its concentration and pressure. Under the conditions that characterize a hyperbaric chamber, the oxygen penetrates up to 70 micrometers into the skin with the help of direct diffusion, which means that it can pass to the area of dermal plexuses. In
this part of dermis it penetrates into arterial and venous blood of papillary plexuses (2). By providing sufficient oxygenation of poorly perfused tissues and transplants it enhances fibroblastic activity and collagen synthesis,which creates a matrix for vascular growth and neovascularization. Daily tissue oxygen level elevation provides functional capillary growth, fibroblast proliferation,
collagen synthesis and angiogenesis, and in this way hyperbaric oxygenotherapy reduces the proportion of unsuccessful transfers to 50% (21%–12%) (2). Even though this method is not indicated for each patient with a skin graft, its effect is evident in patients with a potential risk of primary or secondary graft failure (3). Examples are shown in Table 1.Tab. 1. Positive effect of HBO in selected conditions 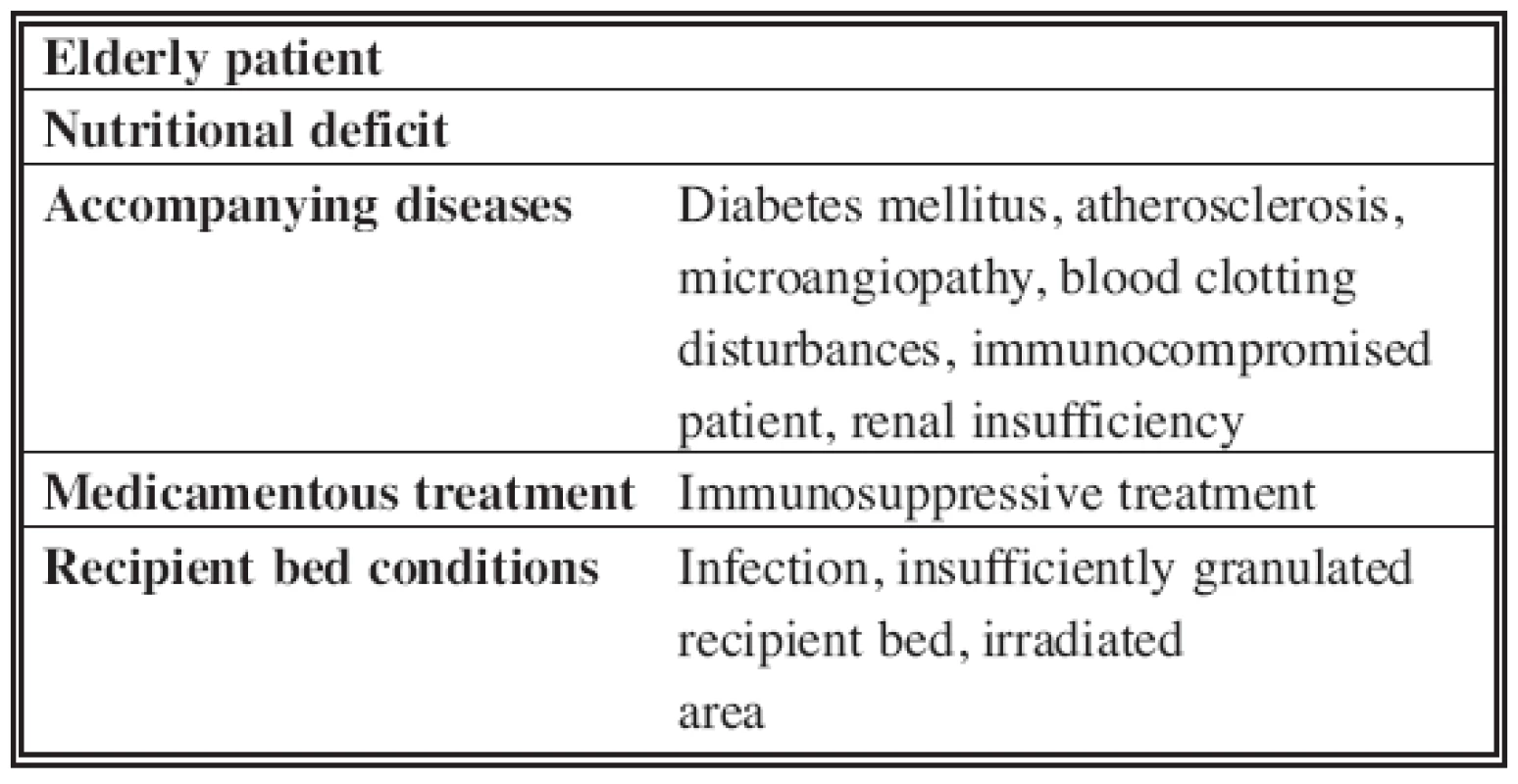
PATIENTS AND METHODS
In our present work we describe three selected patients of a 91-member group. These patients were recommended to our facility from the Clinic of plastic, aesthetic and reconstructive surgery, the Traumatology clinic and the Vascular surgery department at the University Hospital of L. Pasteur due to non healing of soft tissue defects of different character (Table 2).
Tab. 2. Patients with non-healing soft tissue defects of different character 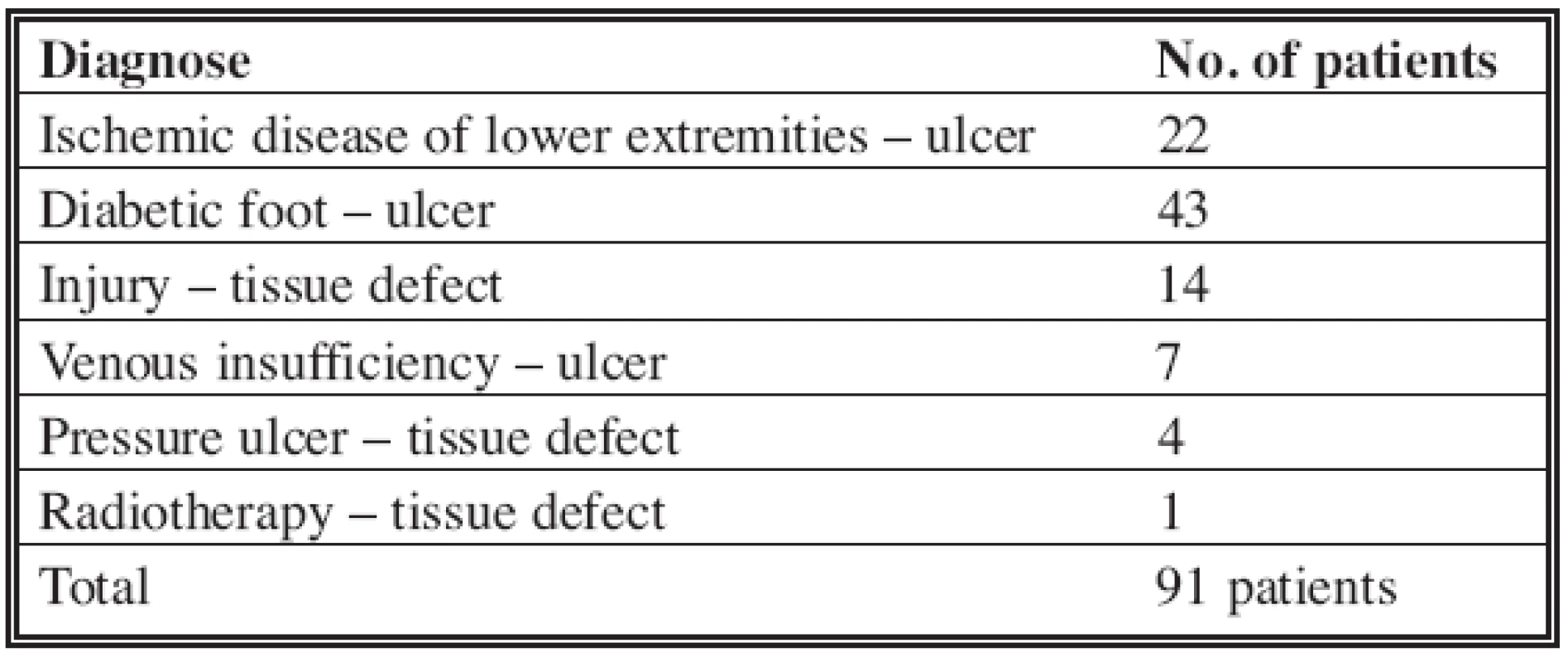
In all cases the reason for problematic wound healing was one of those mentioned above. All available approaches were used to ensure graft survival, starting with harvesting
the most convenient part of the skin, bolster dressing fixation, immobilization, regular bandage changes, bolster dressing removal, broad-spectrum antibiotic therapy. Despite the increased care there were repeated graft failures and necroses, partial or total, and infection. Another option was chosen to promote healing for these patients: the hyperbaric chamber treatment. They were exposed on 8 occasions (min. 6 – max. 10) on average at pressure 2 ATA every second day, each time for 90 minutes with 100% oxygen in monoplace chamber, with treatment being
interrupted at the weekend. Each third day the patient was examined by a surgeon concentrating on granulation tissue formation and cleaning of the defect. Antibiotic therapy was administered according to microbiological wound status. When prepared, the defect was covered with skin graft. The day after operation the patient resumed with HBO treatment. They usually underwent
16 sessions post operation on average (min. 10 – max. 20), with bolster dressing being removed on 4th–5th day post operation and wound status evaluation. In cases with small graft necrosis, this was usually spontaneously healed by the end of hyperbaric treatment (48 days on average).The first patient was a 32-year-old male after occupational injury with opened fracture of the middle third of the right leg with dislocation, several soft tissue defects and massive wound contamination. Fracture reposition and osteosynthesis were performed primarily. The patient’s status was postoperatively complicated by soft tissue necrosis 15 cm x 7 cm in size. We indicated treatment in the hyperbaric chamber. The patient underwent 16 sessions, which were followed by necrotic tissue demarcation, its separation and granulation tissue formation on the surface of the wound. A split skin graft was placed on the wound bed. After the transplantation the patient underwent 10 more sessions (Fig. 1a, b, c).
Fig. 1a. Patient with soft tissue necrosis of the middle third of the right leg Fig. 1b. After necrosis demarcation and separation Fig. 1c. Healing with spilt skin graft after 26 sessions 
In the second case we were dealing with a 72-year-old patient with open fracture of the middle third of the right leg with serious compartment syndrome and muscle necrosis. Radical necrectomy, fasciotomy and split skin grafting were performed. Hyperbaric chamber treatment was indicated. The patient completed 17 sessions (Fig. 2a, b, c, d) .
Fig. 2a. Patient after partial necrectomy with small remains of necrotic tissue Fig. 2b. Partial split skin grafting and necrectomy Fig. 2c. Secondary split skin graft Fig. 2d. Patient healed after 17 sessions 
The third case was a 59-year-old patient after an operation for Achilles tendon rupture. The patient had been suffering from diabetes mellitus for 17 years with permanent insulin treatment. Postoperatively, status complicated with wound dehiscence and soft tissue gangrene 10 cm x 8 cm in size. After necrectomy and debridement, the wound was covered with split skin graft, and he underwent 19 sessions in the hyperbaric chamber (Fig. 3a, b, c).
Fig. 3a. Achilles tendon rupture with wound dehiscence and inflammation Fig. 3b. Soft tissue defect covered with split skin graft Fig. 3c. Patient healed after 19 sessions 
RESULTS
Our aim was also to evaluate and compare whole or partial skin graft survival in our selected group with data in the literature. The grade of graft survival was evaluated 14 days post operation, at the time of suture removal.
We compared (Table 3):
Tab. 3. Comparation of entire/partial skin graft survival in our selected group of patients 
* The reason may be concomitant disease as well as higher incidence of infection, haematoma and seroma. 1. Entire graft survival;
2. Partial graft survival;
- a) Due to infection,
- b) Due to haematoma + seroma,
- c) Idiopathic – due to concomitant disease;
3. Entire graft loss.
Complete graft survival was obtained in 67.8% of patients, partial survival due to infection in 19.2%, due to haematoma or seroma in 3.2%, and graft loss of unknown origin (probably due to concomitant diseases) in 9.8%. Entire graft failure was not observed. According to the literature, partial or total graft failure was recorded in 21% patients (2). In our group, which consisted only of patients with former graft failure and serious concomitant diseases, we received a result of 32.2%. It is also important that none of the patients has had entire graft failure.
DISCUSSION
Even though hyperbaric oxygenotherapy is a treatment of choice for problematic wounds in the developed world, only now are Slovak doctors and medical staff becoming familiar with this technique. When properly indicated, it can significantly influence wound healing in a short time, especially in patients with a predisposition to problematic healing. Nowadays these patients are wholly dependent on long-term inpatient and outpatient care, with an enormous amount of bandage changes, debridements, necrectomies, broad-spectrum antibiotics application, operations, etc. In most cases the wound suffers from chronic lack of oxygen. Hyperbaric atmosphere exposition promotes adequate oxygen supply, and the oxygen itself attacks bacterial oxidative
mechanisms and inhibits their growth and multiplication. According to the work of renowned authors, the scheme for HBO application should be as follows:- End pressure at a chamber should be raised to a level of 2–2.5 ATA,
- The exposure should last for 60–90 minutes (depending on facility type and patient condition),
- Initial treatment should consist of two sessions per day,
- The optimum approach would consist of recipient bed preparation over 20 sessions of HBO, followed by 20 sessions after skin grafting (2, 3).
CONCLUSION
Hyperbaric oxygenotherapy is a conventional treatment method for a large number of patients in the USA, the older EU member states and some Central and Eastern European countries. Let us hope it is only a matter of time before it also becomes the treatment of choice for indicated diseases in Slovakia. HBO reduces the time needed for wound to heal up, it helps to return the patient into socially and economically active life, and it improves the relationship between the patient and his or her doctor. A further factor of some significance is the reduction of health insurance expenses for patients with chronic soft tissue defects, because only healthy individuals can contribute to the system we all depend on.
Address for correspondence:
Ján Švehlík, MD.
Nižná Hutka 121
040 18 Košice okolie
Slovak Republic
E-mail: jsvehlik@yahoo.co.uk
Zdroje
1. Guzanin Š., Sabovčík R., Kačmár, P. Selected Chapters of Plastic and Reconstructive Surgery. Košice: UPJŠ, 2004, p. 19–21.
2. Jain KK. Hyperbaric Oxygen Therapy in Wound Healing in Plastic Surgery. Dermatology. Textbook of Hyperbaric Medicine. Göttingen:
Hogrefe & Huber Publishing, 1996, p. 200–224.
3. Kindwall EP., Whelan HT. Hyperbaric Oxygen in Skin Grafts and Flaps. Hyperbaric Medicine Practice. Flagstaff, AZ: Best Publishing
Company, 2002, p. 795–813.
4. Švehlík J. Klinické použitie hyperbaroxie. Atestačná práca. Bratislava: ILF, 1988.
Štítky
Chirurgia plastická Ortopédia Popáleninová medicína Traumatológia
Článek ČESKÉ/SLOVENSKÉ SOUHRNY
Článok vyšiel v časopiseActa chirurgiae plasticae
Najčítanejšie tento týždeň
2007 Číslo 2- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Kombinace metamizol/paracetamol v léčbě pooperační bolesti u zákroků v rámci jednodenní chirurgie
- Antidepresivní efekt kombinovaného analgetika tramadolu s paracetamolem
- Metamizol v terapii akutních bolestí hlavy
- Srovnání analgetické účinnosti metamizolu s ibuprofenem po extrakci třetí stoličky
-
Všetky články tohto čísla
- HYPERBARIC OXYGENOTHERAPY AS A POSSIBLE MEANS OF PREVENTING ISCHEMIC CHANGES IN SKIN GRAFTS USED FOR SOFT TISSUE DEFECT CLOSURE
- POLAND SYNDROME IN A FEMALE PATIENT RECONSTRUCTED BY ENDOSCOPICALLY ASSISTED TECHNIQUE
- DEVELOPMENT PREDICTION OF SAGITTAL ITERMAXILLARY RELATIONS IN PATIENTS WITH COMPLETE UNILATERAL CLEFT LIP AND PALATE DURING PUBERTY
- REJUVENATION OF THE AGING FACE USING FRACTIONAL PHOTOTHERMOLYSIS AND INTENSE PULSED LIGHT: A NEW TECHNIQUE
- UTILIZATION OF INTENSE PULSED LIGHT IN THE TREATMENT OF FACE AND NECK ERYTHROSIS
- ČESKÉ/SLOVENSKÉ SOUHRNY
- Acta chirurgiae plasticae
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- HYPERBARIC OXYGENOTHERAPY AS A POSSIBLE MEANS OF PREVENTING ISCHEMIC CHANGES IN SKIN GRAFTS USED FOR SOFT TISSUE DEFECT CLOSURE
- DEVELOPMENT PREDICTION OF SAGITTAL ITERMAXILLARY RELATIONS IN PATIENTS WITH COMPLETE UNILATERAL CLEFT LIP AND PALATE DURING PUBERTY
- REJUVENATION OF THE AGING FACE USING FRACTIONAL PHOTOTHERMOLYSIS AND INTENSE PULSED LIGHT: A NEW TECHNIQUE
- POLAND SYNDROME IN A FEMALE PATIENT RECONSTRUCTED BY ENDOSCOPICALLY ASSISTED TECHNIQUE
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



