-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
REJUVENATION OF THE AGING FACE USING FRACTIONAL PHOTOTHERMOLYSIS AND INTENSE PULSED LIGHT: A NEW TECHNIQUE
Autoři: P. Mezzana; M. Valeriani
Působiště autorů: Gestione Servizi Medici e Chirurgici, Laser Centre, Rome, Italy
Vyšlo v časopise: ACTA CHIRURGIAE PLASTICAE, 49, 2, 2007, pp. 47-50
INTRODUCTION
Photoaging is an inevitable occurrence for people who have a fair skin type, who live in a sunny climate, and who enjoy the outdoors. In the past the remedies for this condition were limited to dermabrasion or chemical peeling. Both dermabrasion and chemical peels have hazards of their own. With phenol peels, cardiac and renal toxicity was real concern (1–6). There is an increasing demand for an effective and safe laser treatment that repairs photoaged skin. Two treatment modalities, ablative skin resurfacing (ASR) and nonablative dermal remodeling (NDR), have been developed to address this demand. All currently available laser treatments, however, exhibit significant problems, and these laser systems typically operate safely and effectively only over a narrow, patient-dependent treatment range (7–10). This study aimed to analyze a new protocol of fractional rejuvenation and intense pulsed light (11–20) for skin rejuvenation regarding its efficacy, safety, and complications. Fractional photothermolysis, a novel concept for treating the sequelae of cutaneous photoaging, creates a pattern of microscopic zones of tissue coagulation that heal over several weeks while the skin retains a normal appearance. Rather than creating a global tissue effect at the surface of the target tissue, or in the dermis alone, this treatment creates injury in a tiny fraction of the skin treated, coagulating multiple columns of tissue of about 100–120 μm in diameter, extending through the epidermis and deeply into the dermis for about 500 μm (21–24).
Even though the epidermis in these microthermal zones (MTZs) is coagulated, it remains intact, leaving no raw surface. The large volume of normal tissue surrounding the MTZ on all sides provides a generous reservoir of source cells for healing. Over several weeks the body extrudes the coagulated tissue, replacing it with new healing tissue (22–23). Since this process is invisible to the naked eye, there is no downtime. Over the course of multiple treatments most of the skin surface is replaced, and the appearance of rhytids, scars, varied pigment irregularities, and vascular lesions is improved. Treatment is usually offered in a series of 4 weekly visits. This fractional approach is a revolutionary means of effecting tissue removal without an open wound or recovery time. It produces the predictable resurfacing effects of tissue removal, treats pigmentary changes such as solar lentigines, improves rhytids, and stimulates tissue remodeling, all with no recovery time (26–29).
Conceptually, this seems to be a safe, desirable approach to treating photodamaged skin. This rapidly evolving technology is claimed to produce a clearly visible clinical result without a significant number of non responders; preliminary clinical data confirm these results (24). Intense pulsed light is a noncoherent light produced by a flash lamp, which has been introduced over the past few years to improve the photodamage aspect of the skin. Using different cutoff filters allows selection of the desired wavelengths (11).
The effect on the skin texture and general appearance is achieved by long waves that heat the collagen deep in the dermis, thus achieving some tightening of the skin. The effect on vascular and pigmented lesions is achieved by photothermal damage either to the blood vessels through absorption in hemoglobin or to the absorption in melanin-pigmented lesions. The light pulses and the delays between them, which are shorter than the thermal relaxation time of the epidermis, preserve it from the thermal damage. At the same time, the duration of the pulses and the delays are shorter than the thermal relaxation time of the targets, thus ensuring their selectivedestruction.
PATIENTS AND METHODS
We collected our data over a 5-month period (from August 2006 to December 2006). Twenty-nine patients (27 women and 2 men), age ranging from 40 to 73 years, answered our questionnaire and were included in the study. The patients included had Fitzpatrick skin types II to IV: 10 patients type II, 10 patients type III, and 9 patients type IV. All procedures were performed by one physician. Patients with any suspicion of skin cancer, serious systemic disease or pregnancy were not included. The patients signed a detailed informed consent.
The device used was Matisse PL® by Quantasystem s.p.a, Italy. This new device has an erbium glass (1540 nm) laser for fractional phothermolysis and an intense pulsed light source with handpiece 570–1200 nm for photorejuvenation.
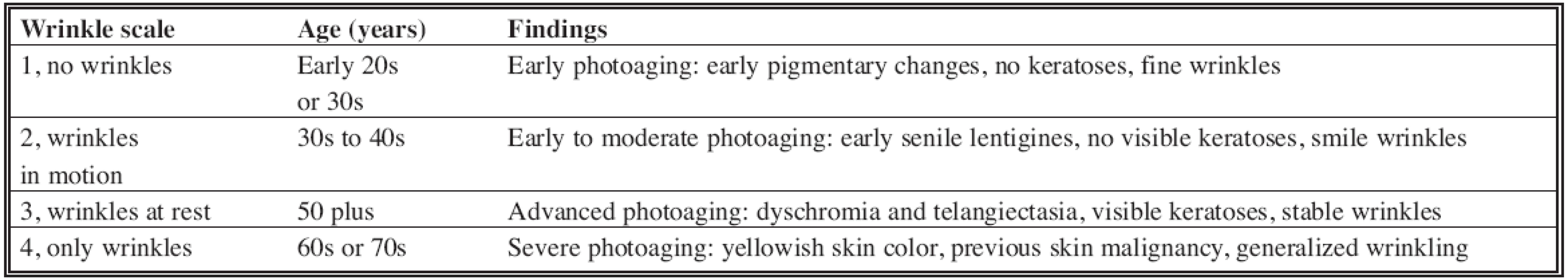
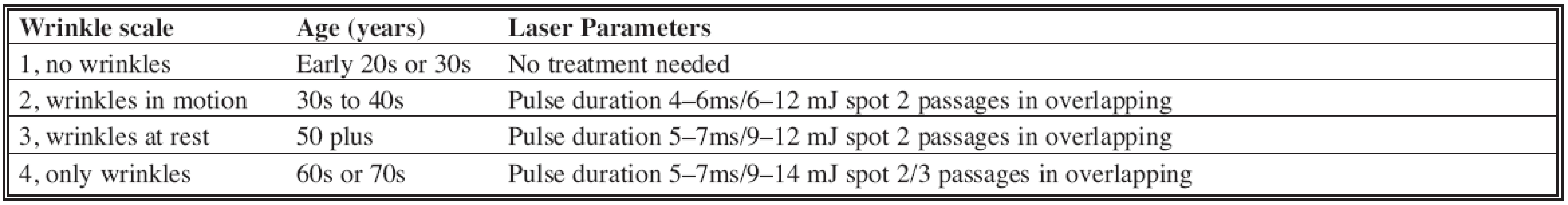
Patients should avoid taking oral retinoids for at least 3–6 months prior to treatment, and topical retinoids should be discontinued at least 2 weeks before treatment. The treatment is performed in the office. The treatment area is cleansed with a mild abrasive cleanser. The laser head is moved over the treatment area, using an overlapping technique, so that a total of 2–4 passes are made over each area. The skin is kept cool during the treatment. The energies and pulse durations were varied based on the grade of photoaging according to Glogau Wrinkle Scale (Table 1) and Fitzpatrick skin type.
In Fitzpatrick skin types V–VI, to avoid post-inflammatory hyperpigmentations it is better to use the treatment parameters of the Glogau Wrinkle Scale 2 in every case (Table 2).
Immediately after treatment a sensation of heat or “sunburn” is common, lasting about 30 minutes, and is easily relieved by cool compresses, and only moisturizers and zinc sunscreens are used on the face. In the week after treatment the skin may become somewhat dry and red. This “bronzed” appearance and dryness is from the surface of each laser “spot” separating and sloughing off. During this time potentially irritating skin products such as AHAs or retinoids should be avoided. In most cases, the redness and bronzing will gradually improve over a week or so.
The intervals and number of sessions vary also with Glogau Wrinkle Scale (Table 3).
Tab. 3. Intervals between sessions and number of sessions 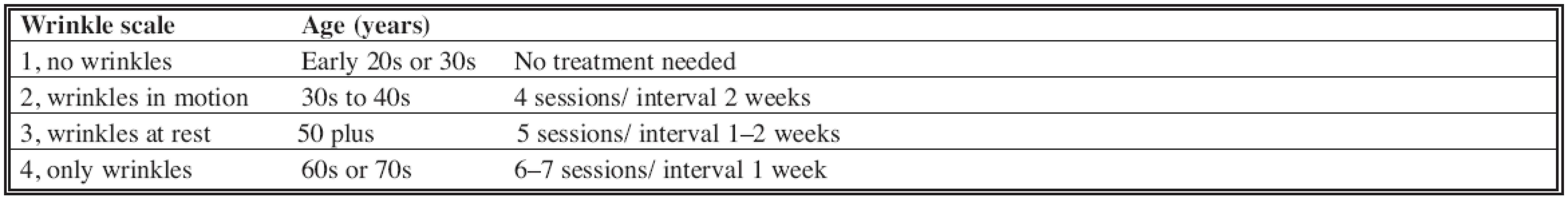
The patients underwent between four and seven treatments of fractional photorejuvenation and subsequently three sessions of intense pulsed light with an interval between sessions of two weeks.
For intense pulsed light sessions the amount of energy used varied between 10 and 20 J/cm2. The cut-off filter used was 570–1200 nm. The pulse duration varied from 10 to 20 ms, two burst mode with a pulse delay time of 20 ms. The parameters were obtained according to theskin and lesion diagnosis and refined according to the response of the skin.
The mean duration of the treatments was 30 minutes. At the end of the treatment cold wet gauzes were applied to the skin for a few minutes. No creams or ointments were used after the procedure, and the patients were allowed to apply hypoallergenic makeup. A complete sun block was used 1 month before and after each treatment, and sun exposure was avoided as much as possible.
The patients filled out a detailed questionnaire concerning their satisfaction level, side effects, and complications 2 to 4 months after their last treatment. Another physician rated the results using the same parameters.
RESULTS
In the questionnaire, patients satisfaction was evaluated and graded on a scale from 0 to 5, with 5 = excellent, 4 = very good, 3 = good, 2 = moderate improvement,1 = mild improvement, and 0 = no improvement. Anurse collected the patient rating at the office visit and had no connection with the physician rating, which was also performed at the office visit.
The satisfaction rate is demonstrated in Table 4.
Tab. 4. The satisfaction of the patients 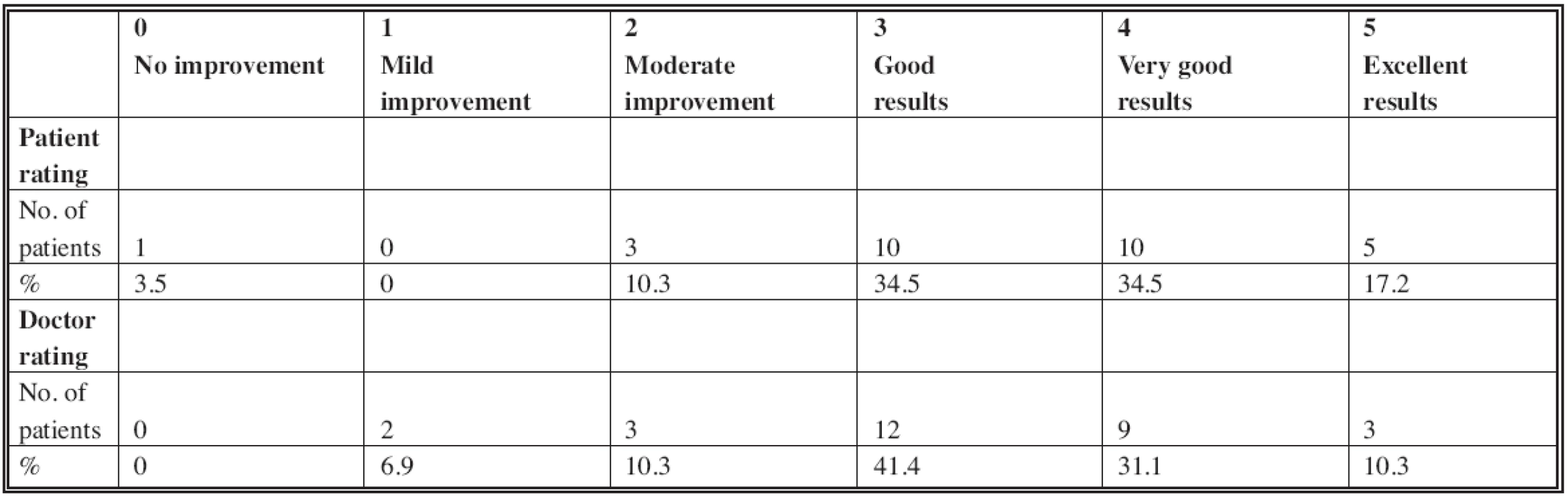
The rates given by the neutral physician were not significantly different from the patients’ rates. The majority of the patients, 25 (86.2 percent), had some burning sensation for a few hours after treatments (especially after fractional rejuvenation), whereas 4 patients did not report any discomfort. The most common side effect was redness.
Oedema was noted by eight patients after fractional rejuvenation (27.6 percent). Small blisters that regressed spontaneously 1 to 5 days after treatment were reported by 2 patients (6.9 percent). (Fig. 1a, b.)
Fig. 1a. Pre-treatment image of a 65-year-old woman Fig. 1b. After 6 sessions of fractional rejuvenation and 3 sessions of IPL 
DISCUSSION
The main advantage of using nonablative fractional rejuvenation and intense pulsed light for the treatment of photoaging is that they allow a short recovery time with lower complication rates compared with the other methods, such as laser resurfacing and chemical peeling. Nonablative fractional rejuvenation – rather than creating a global tissue effect at the surface of the target tissue, or in the dermis alone – creates injury in a tiny fraction of the skin treated, coagulating multiple columns of tissue of about 100–120 μm in diameter, extending through the epidermis and deeply into the dermis. The penetration of light into the skin is much deeper than with carbon dioxide or Erbium:YAG (Er:YAG) laser wavelengths (21–24). Each pulse of laser light fired into the skin creates a column of coagulated tissue, extending from the surface of the epidermis into the dermis with a gradual skin resurfacing effect session after session without downtime (25–29). The use of intense pulsed light after the fractional rejuvenation allows us to enhance the effects of this new procedure especially in skin pigmentation disorders and telangiectasia and to continue to stimulate the deep dermal component.
CONCLUSIONS
On the basis of the data presented in this article the new procedure can be considered a “lunchtime” procedure. It is performed without any type of sedation and it is easy to perform. The time needed to complete the facial area is only 15 to 30 minutes. Since this is a new technology, there are no other studies that describe the combination of fractional rejuvenation and intense pulsed light for the treatment of photoaging. The results presented in this work show that together these nonablative procedures are safe and produce very good results. A long-term follow - up study will determine how long the good endpoints will last.
Zdroje
1. Fisher GJ., Wang ZQ., Datta SC., Varani J., Kang S., Voorhees JJ. Pathophysiology of premature skin aging induced by ultraviolet light. N. Engl. J. Med., 337, 1997, p. 1419.
2. Ernster VL., Grady D., Miike R., Black D., Selby J., Kerlikowske K. Facial wrinkling in men and women by smoking status. Am. J. Public Health, 85, 1995, p. 78.
3. Kadunce D., Burr R., Gress R., Kanner R., Lyon JL., Zone JJ. Cigarette smoking: Risk factor for premature facial wrinkling. Ann. Intern. Med., 114, 1991, p. 840.
4. Yin L., Morita A., Tsuji T. Skin aging induced by ultraviolet exposure and tobacco smoking: Evidence from epidemiological and molecular studies. Photodermatol. Photoimmunol. Photomed., 17, 2001, p. 178.
5. Sander C., Chang H., Salzmann S., et al. Photoaging is associated with protein oxidation in human skin in vivo. J. Invest. Dermatol., 118, 2002, p. 618.
6. Aizen E., Gilhar A. Smoking effect on skin wrinkling in the aged population. Int. J. Dermatol., 40, 2001, p. 431.
7. Kauvar ANB., Dover JS. Facial skin rejuvenation: Laser resurfacing or chemical peel – Choose your weapon. Dermatol. Surg., 27, 2001, p. 209.
8. Khatri KA. The effects of variable pulse width of Er:YAG laser on facial skin. Dermatol. Surg., 27, 2001, p. 332.
9. Rostan EF., Fitzpatrick RE., Goldman MP. Laser resurfacing with a long pulse erbium:YAG laser compared to the 950 ms pulsed CO2 laser. Lasers Surg. Med., 29, 2001, p. 136.
10. Ross EV., Miller C., Meehan K., et al. One-pass CO2 versus multiple - pass Er:YAG laser resurfacing in the treatment of rhytides: Acomparison side-by-side study of pulsed CO2 and Er:YAG lasers. Dermatol. Surg., 27, 2001, p. 709.
11. Bitter PH. Noninvasive rejuvenation of photodamaged skin using serial, full-face intense pulsed light treatments. Dermatol. Surg., 26, 2000, p. 835.
12. Negishi K., Tezuka Y., Kushikata N., Wakamatsu S. Photorejuvenation for Asian skin by intense pulsed light. Dermatol. Surg., 27, 2001, p. 627.
13. Goldberg DJ., Cutler KB. Nonablative treatment of rhytids with intense pulsed light. Lasers Surg. Med., 26, 2000, p. 196.
14. Goldberg DJ., Samady JA. Intense pulsed light and Nd:YAG laser non-ablative treatment of facial rhytids. Lasers Surg. Med., 28, 2001, p. 141.
15. Moreno-Arias GA., Ferrando J. Intense pulsed light for melanocytic lesions. Dermatol. Surg., 27, 2001, p. 397–400.
16. Prieto VG., Sadick NS., Lloreta J., Nicholson J., Shea CR. Effects of intense pulsed light on sundamaged human skin, routine, and ultrastructural analysis. Lasers Surg. Med., 30, 2002, p. 82.
17. Negishi K., Wakamatsu S., Kushikata N., Tezuka Y., Kotani Y., Shiba K. Full-face photorejuvenation of photodamaged skin by intense pulsed light with integrated contact cooling: Initial experiences in Asian patients. Lasers Surg. Med., 30, 2002, p. 298.
18. Kullick MI. Photorejuvenation: Using intense pulsed light technology in a cosmetic surgery practice. Aesthetic Surg. J., 21, 2001, p. 255.
19. Weiss RA., Weiss MA., Beasley KL. Rejuvenation of photoaged skin: 5 years results with intense pulsed light of the face, neck, and chest. Dermatol. Surg., 28, 2002, p. 1115.
20. Lin JY., Chan HH. Pigmentary disorders in Asian skin: treatment with laser and intense pulsed light sources. Skin Therapy Lett., 11, 2006, p. 8.
21. Hantash BM., Bedi VP., Sudireddy V., Struck SK., Herron GS., Chan KF. Laser-induced transepidermal elimination of dermal content by fractional photothermolysis. J. Biomed. Opt., 11, 2006, p. 411.
22. Hasegawa T., Matsukura T., Mizuno Y., Suga Y., Ogawa H., Ikeda S. Clinical trial of a laser device called fractional photothermolysis system for acne scars. J. Dermatol., 33, 2006, p. 623.
23. Behroozan DS., Goldberg LH., Dai T., Geronemus RG., Friedman PM. Fractional photothermolysis for the treatment of surgical scars: a case report. J. Cosmet. Laser Ther., 8, 2006, p. 35.
24. Geronemus RG. Fractional photothermolysis: current and future applications. Lasers Surg. Med., 38, 2006, p. 169.
25. Behroozan DS., Goldberg LH., Glaich AS., Dai T., Friedman PM.
Fractional photothermolysis for treatment of poikiloderma of civatte. Dermatol. Surg., 32, 2006, p. 298.
26. Laubach HJ., Tannous Z., Anderson RR., Manstein D. Skin responses to fractional photothermolysis. Lasers Surg. Med., 38, 2006, p. 142.
27. Rokhsar CK., Fitzpatrick RE. Related Articles, Links: The treatment of melasma with fractional photothermolysis: a pilot study. Dermatol. Surg., 31, 2005, p. 1645.
28. Fisher GH., Geronemus RG. Related Articles, Links: Short-term side effects of fractional photothermolysis. Dermatol. Surg., 31, 2005, p.1245; discussion 1249.
29. Manstein D., Herron GS., Sink RK., Tanner H., Anderson RR. Fractional photothermolysis: a new concept for cutaneous remodeling using microscopic patterns of thermal injury. Lasers Surg. Med., 34, 2004, p. 426.
Štítky
Chirurgia plastická Ortopédia Popáleninová medicína Traumatológia
Článek ČESKÉ/SLOVENSKÉ SOUHRNY
Článok vyšiel v časopiseActa chirurgiae plasticae
Najčítanejšie tento týždeň
2007 Číslo 2- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Kombinace metamizol/paracetamol v léčbě pooperační bolesti u zákroků v rámci jednodenní chirurgie
- Antidepresivní efekt kombinovaného analgetika tramadolu s paracetamolem
- Srovnání analgetické účinnosti metamizolu s ibuprofenem po extrakci třetí stoličky
- Možnosti využití metamizolu v léčbě akutních primárních bolestí hlavy
-
Všetky články tohto čísla
- HYPERBARIC OXYGENOTHERAPY AS A POSSIBLE MEANS OF PREVENTING ISCHEMIC CHANGES IN SKIN GRAFTS USED FOR SOFT TISSUE DEFECT CLOSURE
- POLAND SYNDROME IN A FEMALE PATIENT RECONSTRUCTED BY ENDOSCOPICALLY ASSISTED TECHNIQUE
- DEVELOPMENT PREDICTION OF SAGITTAL ITERMAXILLARY RELATIONS IN PATIENTS WITH COMPLETE UNILATERAL CLEFT LIP AND PALATE DURING PUBERTY
- REJUVENATION OF THE AGING FACE USING FRACTIONAL PHOTOTHERMOLYSIS AND INTENSE PULSED LIGHT: A NEW TECHNIQUE
- UTILIZATION OF INTENSE PULSED LIGHT IN THE TREATMENT OF FACE AND NECK ERYTHROSIS
- ČESKÉ/SLOVENSKÉ SOUHRNY
- Acta chirurgiae plasticae
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- HYPERBARIC OXYGENOTHERAPY AS A POSSIBLE MEANS OF PREVENTING ISCHEMIC CHANGES IN SKIN GRAFTS USED FOR SOFT TISSUE DEFECT CLOSURE
- DEVELOPMENT PREDICTION OF SAGITTAL ITERMAXILLARY RELATIONS IN PATIENTS WITH COMPLETE UNILATERAL CLEFT LIP AND PALATE DURING PUBERTY
- REJUVENATION OF THE AGING FACE USING FRACTIONAL PHOTOTHERMOLYSIS AND INTENSE PULSED LIGHT: A NEW TECHNIQUE
- POLAND SYNDROME IN A FEMALE PATIENT RECONSTRUCTED BY ENDOSCOPICALLY ASSISTED TECHNIQUE
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy