-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Bilobed flap in facial reconstruction
Authors: Z. Dvořák 1; V. Vavrek 2; T. Kubek 1; L. Streit 1; I. Stupka 1; J. Veselý 1
Authors place of work: Masaryk University Brno, Faculty of Medicine, and St. Anne´s University Hospital, Department of Plastic and Aesthetic Surgery, Brno, Czech Republic 1; Military Hospital Brno, Department of Surgery, Brno, Czech Republic 2
Published in the journal: ACTA CHIRURGIAE PLASTICAE, 61, 1-4, 2019, pp. 10-15
INTRODUCTION
The beginning of history of bilobed flap starts in the 20th century. The first publication appeared in German literature in 1918 by the Dutch surgeon J. F. S. Esser. Esser described the bilobed flap like two approximately equal transposition flaps used to cover distal nose defects. Total lobe angle was 180° or more1.
In 1953, Zimany published his experience with the bilobed flap in several anatomical sites including the face, the abdomen and the heel. He studied the range of tissue movements that can be used in this reconstruction. He pointed out the possibility that the second lobe could be smaller than the first to improve coverage of the defect2.
Later in the 20th century, McGregor and Soutar discussed the use of the bilobed flap with a smaller angle of the flaps, which caused less skin deformities2.
Zitelli3 made one of the latest modifications. The reconstruction was based on an angle of rotation of up to 50° between the lobes. Total angle of the bilobed flap did not reach more than 90° to 100°. This reduced tension around the pivot point and also the distortion that occurred in previous transposition reconstructions.
Deficiencies in the anatomical sites were gradually modified by using the bilobed flap. Yenidunya et al.4 demonstrated the use in frontal and infraorbital localizations.
The use of bilobed flap in 11 cases of necrotizing fasciitis in the posterior cervical region is reported by El-Khatiba5. This publication reports excellent results in plastic surgery with this technique, where the bilobed fasciocutaneous flap was designed based on the musculocutaneous perforators of the trapezius muscle. The same principle was used by Atik et al.6 who treated 20 cases of meningomyelocele with approximate size of the defects of 38 cm2.
Mutaf et al.7 demonstrated the application of this technique in the anterior cervical region and globally in post-traumatic reconstructions of the auricle where the conditions were not good and it was impossible to use the temporoparietal fascia.
Hsieh et al.8 used the bilobed flap to cover radial forearm area after the harvest of the radial forearm flap. This radial forearm flap is used in various locations in reconstructive surgery. Typically, skin graft is used to cover the donor site but with significant healing problems. The bilobed flap has proven to be a suitable technique either from aesthetic point or in terms of rapid mobilisation postoperatively.
MATERIAL AND METHODS
Authors collected the case histories of patients who underwent the reconstruction surgery at the Department of Plastic and Aesthetic Surgery of St. Anne´s University Hospital in Brno, Czech Republic. The retrospective analysis conducted between 1st January 2007 to 31st December 2016. We found 203 cases, in which bilobed flaps were used to repair skin defects. There were 199 patients, 101 men (50.8%) and 98 (49.2%) women. The bilobed flap was used twice in the same person for four times. Once in a man and three times in women. Totally there were 102 bilobed flaps used in men and 101 in women.
RESULTS
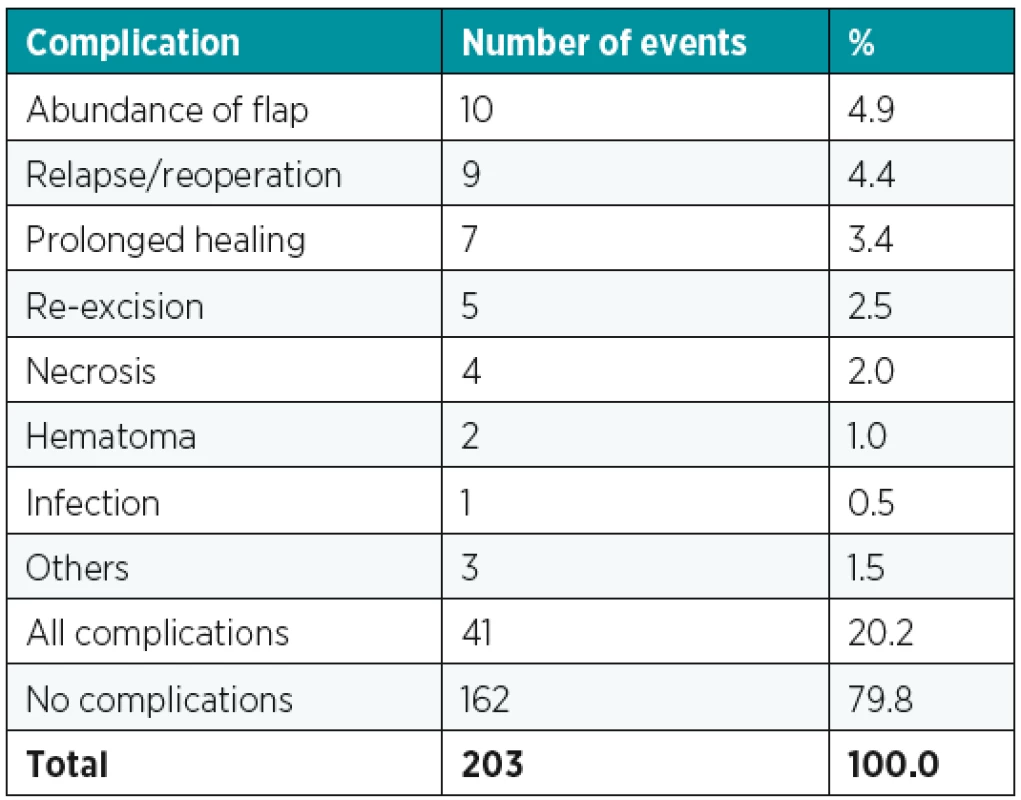
Average age of patients was 76 years. The youngest patient was 38 years old and the oldest was 98 years old. The most common disease was carcinoma (Chart 1). Histologically, basal cell carcinoma (83.3%), squamous cell carcinoma (4.9%), and melanoma (1.5%). Although basal cell carcinoma was the most prevalent among skin defects, the case selection included other pathology such as actinic keratosis, keratoacanthoma, lentigo maligna, trauma and others as well (Table 1). Basal cell carcinoma was the most common in men and women. Other diseases were distributed almost equally (Table 2). We divided complications to a relapse/reoperation, abundance of the flap, infection, necrosis, prolonged healing, hematoma, re-excision and others. The most common was abundance of the flap, 10 times more common (Chart 2). The next most common was relapse/reoperation in 9 cases, prolonged healing in 7 cases and reexcision in 5 cases. Necrosis occurred 4 times after bilobed flap, there was 1 case of infection and 2 cases of hematoma. Other complications occurred three times (Table 3).
Graph 1. Distribution of pathology 
Tab. 1. Distribution of pathology 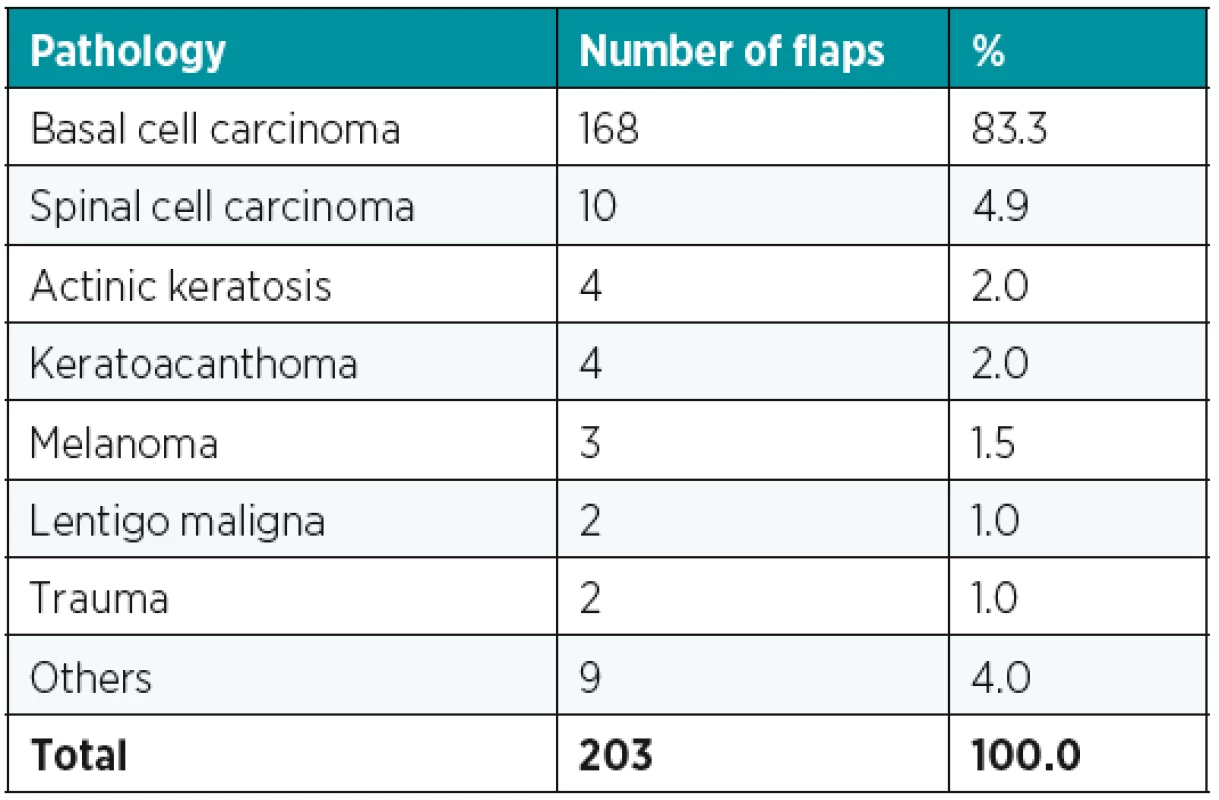
Tab. 2. Gender distribution of pathology 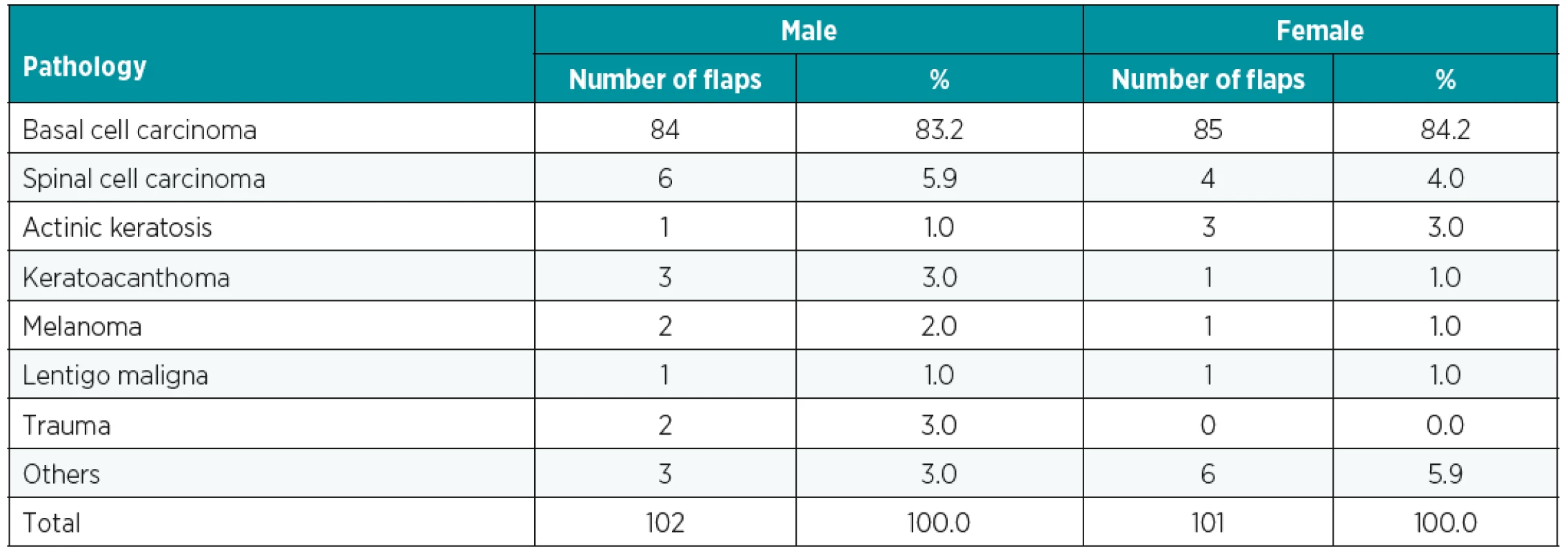
The most common complications affected the nasal region (65.9%), periorbital area (9.8%) and other parts of the body (24.4%). The predominant nasal complications are caused by the numbers of bilobed flaps used in this area (79.3%). That also means that bilobed flap is most commonly used for reconstruction of nasal defects compared to other regions in our geographic area. In men, the overall rate of complications was 20.6% (21). The most common were abundance of the flap, re-excision and relapse/reoperation (3.9%). There were 81 bilobed flaps without complications (79.4%). Women had the same rate of complications (19.8%). On the first place was abundance of the flap in 6 cases. Prolonged healing and relapse/reoperations occurred 5 times. Infection and hematoma did not occur (Table 4).
Tab. 4. Complications between genders 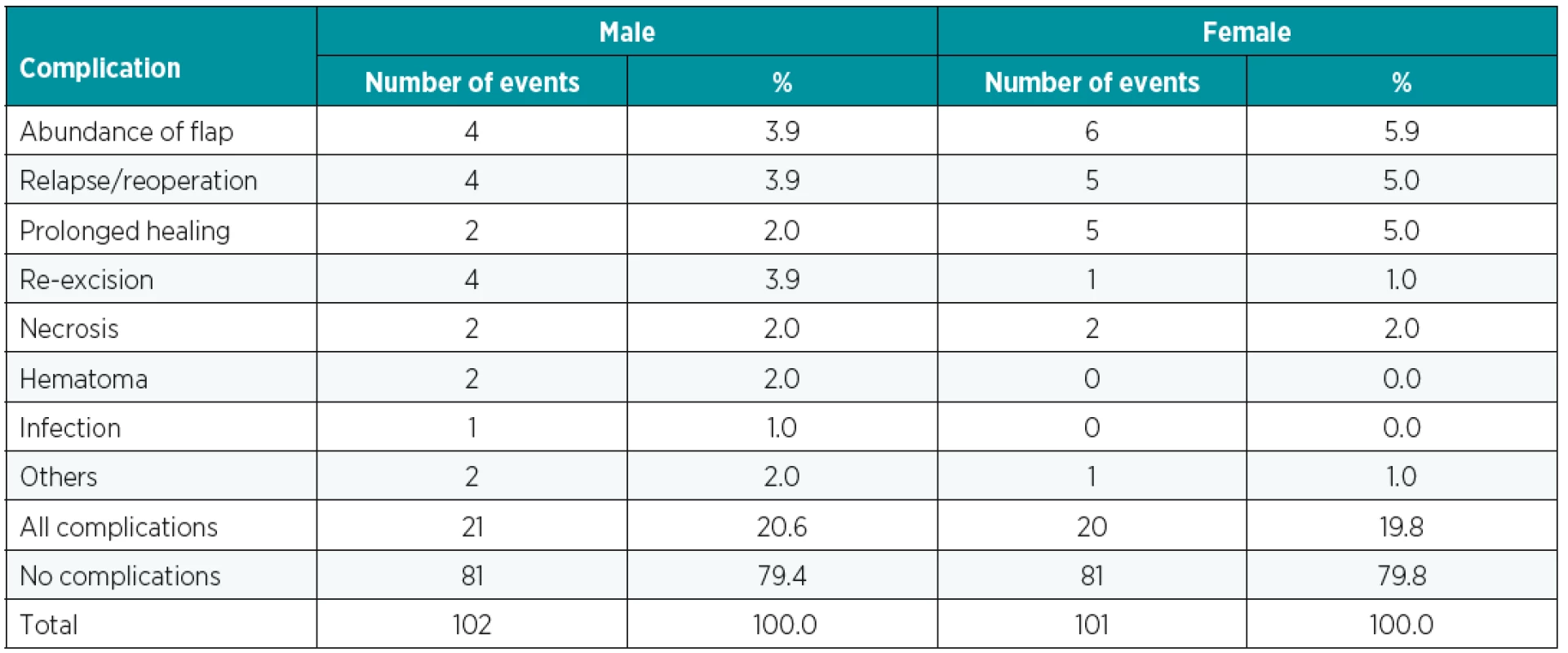
Fig. 1. a,b. Preoperative marking (Author’s archive) 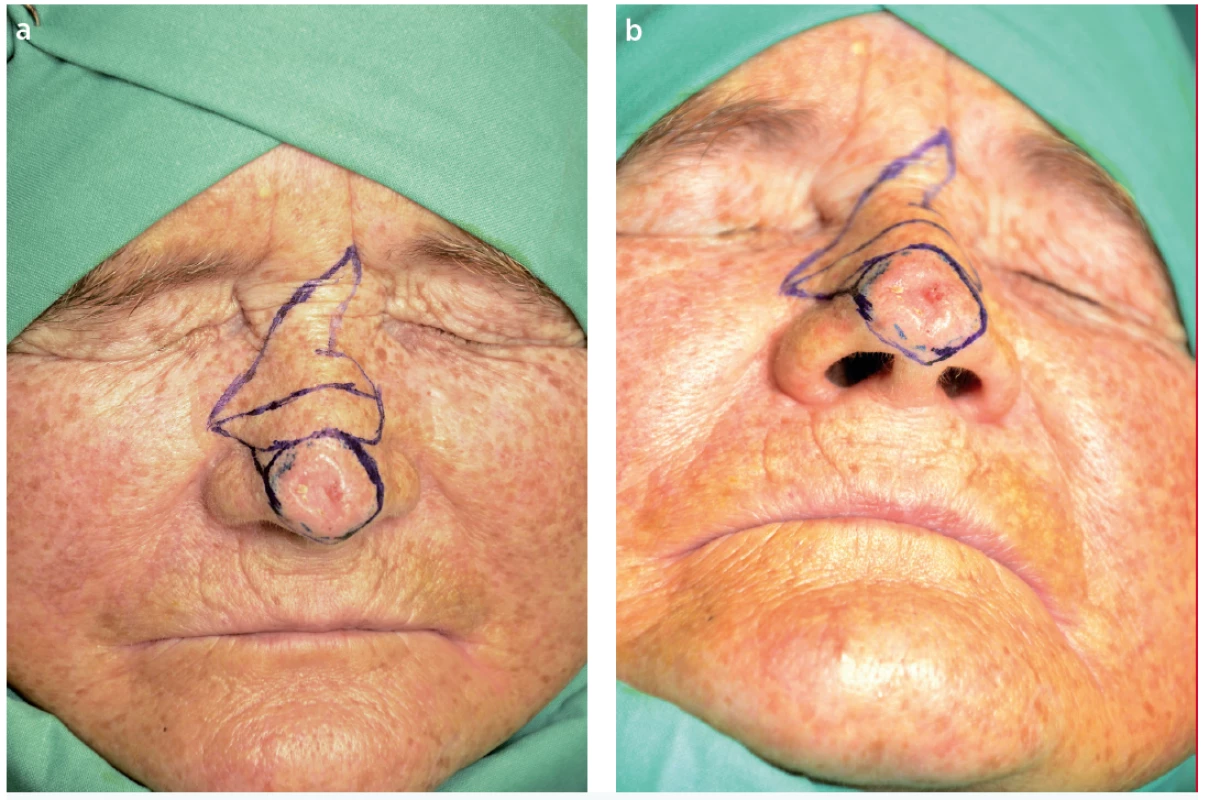
Fig. 2. Postoperative result (Author’s archive) 
DISCUSSION
Zitelli3 described his modification of bilobed flap in 1989. Zitelli used bilobed flap to repair 20 wounds. There were two complications reported in this case report (10%). It was superficial epidermal necrosis of the primary flap and slight tip necrosis of the primary flap. He also claimed that no patients required reoperation for abundance of soft tissue. Bilobed flap was usually indicated after excision of basal cell carcinoma up to 1.5 cm diameter on the nose.
Analysis by McGregor and Soutar2 in 1981 studied 80 bilobed flaps in 77 patients. The most common site of bilobed flap was the nose (50) and the face (18). In 60 cases, the pathology was basal cell carcinoma, in 11 cases benign skin lesion. Patients were 29 to 86 years old. Only 44 patients attended for follow up. From an aesthetic point of view, colour, shape distortion, contour and appearance of scars were observed in the study. Unsatisfactory results in McGregor and Soutar article occured in 13 transposition reconstructions of the 44 flaps (29.5%).
Another study by Moy et al.9 reviewed 171 patients who underwent bilobed flap repairs of the distal nose region. Bilobed flap was used after excision of skin cancer on the nose. The incidence of complications was low after the use of bilobed flap to repair defects, however some occurred. The main complications in the study of Moy et al. included wound infection, trapdooring, partial flap necrosis and distortion of alar rim. Complications occurred in 20% of cases. Partial flap necrosis occurred in 7%, which was the main complication.
Retrospective analysis by Tissiani et al.10 followed up 42 patients who underwent 45 tissue reconstructions. There were 93% of all reconstructions due to a tumour resection. The most common body part was the face (71%) followed by the trunk (20%) and the limbs (8.9%). The nose was the most involved in the reconstructions, followed by the cheek (25%) and the frontotemporal (18.7%) and infraorbital regions (15%). Patients were 17 to 85 years old, the mean was 62 years. The rate of complications in this study was 20%. Complications included epithelial desquamation, infection, partial necrosis, trapdoor of the scar.
Yazici et al.11 report the outcomes of the bilobed flap used for inferior and lateral periorbital defects after tumour excision. The case report involved 20 patients (10 male and 10 female), 48 to 86 years old. The patients were 67 years old on average. Basal cell carcinoma was present in 18 patients and other two patients had a diagnosis of squamous cell carcinoma and pilomatrixoma. Total number of complications was 10 (50%), divided in four major complications including canthal webbing, permanent pin-cushion skin deformity and ptosis and six minor complications including pin-cushion flap deformity and pyogenic granuloma. No infection, haemorrhage or necrosis occured. In 2006, Mutaf et al.7 described the use of bilobed cervical flap as a new technique in total ear reconstruction for patients with an unfavourable temporoauriculomastoid region. The technique was used in seven patients. The age ranged from 9 to 52 years. The reason for plastic surgery was burn injury (3), surgical ablation (2), avulsion injury (1) and a dog bite (1). All patients healed uneventfully and there were excellent results. Only one patient had a complication, mild venous stasis at the distal end of the flap (14.2%).
The bilobed flap looks like an extremely flexible reconstruction surgery. It can be used theoretically in any parts of the human body. The bilobed flap was most commonly indicated to cover defects after oncological resections. Complications which occurred in our study are comparable to other studies. In the total of 203 cases, complications occurred in 41 reconstructions (20.2%). It is necessary to note the fact that our cohort included patients with mean age of 76 years and the oldest patient was 98 years old. This retrospective study suggests the possibility to use the bilobed flap at higher age also without increasing the occurrence of complications. The highest rate of complications was abundance of the flap (4.9%). Perhaps shortening of the lobes can lead to decreased incidence of abundances. Proper design and surgical technique of the bilobed flap can also reduce the risk of complications. On the other hand, there are other factors, which have an influence on the excellent aesthetic and functional results (patient, age, comorbidity, etc.).
Fig. 3. a,b,c,d. Reconstruction of suborbital area using the bilobed flap. (Author’s archive)
a) Preoperative marking, b) During the operation, c) After reconstruction, d) Postoperative result
CONCLUSION
The bilobed flap is a transposition – rotational local flap, which can be used in various anatomical sites and with different aetiology of the defect. It provides a wide range of reconstruction surgery with excellent results. The main advantages of the bilobed flap include tissue and colour similarity, low incidence of complications, simple execution and the possibility to use in different sizes and ages. The bilobed flap in different modifications should always be considered in the reconstruction of extensive defects of the face.
Conflict of interest: Authors have no conflicts of interest to disclose.
Funding: Authors declare that this study has received no financial support.
Ethical requirements. All procedures performed in this study were in accordance with ethical standards of the institutional and/or national research committee and with the Helsinki declaration and its later amendments or comparable ethical standards.
Vladimír Vavrek, MD
Department of Surgery of Military Hospital Brno
Zábrdovická 3
636 00 Brno
Czech Republic
E-mail: vladimir.vavrek@gmail.com
Zdroje
1. Esser JFS. Gestielte lokale Nasenplastik mit zweizipfligem Lappen, Deckung des sekundären Defektes vom ersten Zipfel durch den zweiten. Dtsch. Z. Für Chir. 1918, 143 : 385–90.
2. McGregor JC, Soutar DS. A critical assessment of the bilobed flap, Br. J. Plast. Surg. 1981, 34 : 197–205.
3. Zitelli JA. The bilobed flap for nasal reconstruction, Arch. Dermatol. 1989, 125 : 957–9.
4. Yenidunya MO, Demirseren ME, Ceran C. Bilobed flap reconstruction in infraorbital skin defects. Plast. Reconstr. Surg. 2007, 119 : 145–50.
5. El-Khatib HA. Bilobed fasciocutaneous flap for reconstruction of the posterior neck after necrotizing fasciitis. Plast. Reconstr. Surg. 2004, 114 : 885–9.
6. Atik B, Tan O, Kiymaz N, Yilmaz N, Tekes L. Bilobed fasciocutaneous flap closure of large meningomyeloceles. Ann. Plast. Surg. 2006, 56 : 562–4.
7. Mutaf M, Isk D, Atik B, Bulut O. Versatility of the bilobed cervical skin flap for total ear reconstruction in the unfavorable temporoauriculomastoid region. Plast. Reconstr. Surg. 2006, 118 : 652–62.
8. Hsieh CH, Kuo YR, Yao SF, Liang CC, Jeng SF. Primary closure of radial forearm flap donor defects with a bilobed flap based on the fasciocutaneous perforator of the ulnar artery. Plast. Reconstr. Surg. 2004, 113 : 1355–60.
9. Moy RL, Grossfeld JS, Baum M, Rivlin D, Eremia S. Reconstruction of the nose utilizing a bilobed flap. Int. J. Dermatol. 1994, 33 : 657–60.
10. Tissiani LAL, Alonso N, Carneiro MH, Bazzi K, Rocco M. Versatility of the bilobed flap. Rev. Bras. Cir. Plástica. 2011, 26 : 411–7.
11. Yazici B, Çetinkaya A, Çakirli E. Bilobed flap in the reconstruction of inferior and/or lateral periorbital defects. Ophthal. Plast. Reconstr. Surg. 2019, 29 : 208–14.
Štítky
Chirurgia plastická Ortopédia Popáleninová medicína Traumatológia
Článek České souhrnyČlánek Acknowledgemets to reviewers
Článok vyšiel v časopiseActa chirurgiae plasticae
Najčítanejšie tento týždeň
2019 Číslo 1-4- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Kombinace metamizol/paracetamol v léčbě pooperační bolesti u zákroků v rámci jednodenní chirurgie
- Antidepresivní efekt kombinovaného analgetika tramadolu s paracetamolem
- Srovnání analgetické účinnosti metamizolu s ibuprofenem po extrakci třetí stoličky
- Metamizol v terapii akutních bolestí hlavy
-
Všetky články tohto čísla
- The impact of aesthetic plastic surgery on body image, body satifaction and self-esteem
- Bilobed flap in facial reconstruction
- Free-flap monitoring: review and clinical approach
- Giant basal carcinoma on the forehead and why should prevent them - case report
- Use of medial femoral condyle flap and anterolateral thigh free flap in proxymal tibial posttraumatic non-union with multiple anastomosis - case report
- Reconstruction of deep head burn with a free flap - a case study
- České souhrny
- Acknowledgemets to reviewers
- Acta chirurgiae plasticae
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- The impact of aesthetic plastic surgery on body image, body satifaction and self-esteem
- Free-flap monitoring: review and clinical approach
- Bilobed flap in facial reconstruction
- Use of medial femoral condyle flap and anterolateral thigh free flap in proxymal tibial posttraumatic non-union with multiple anastomosis - case report
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy