-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Combination of cable ties and barbed sutures for fasciotomy closure – two case reports
Authors: K. Bulić 1,2; E. Brenner 1; L. Bulić 1; M. Lorencin Bulić 3; H. Kisić 2
Authors place of work: University Hospital Centre Zagreb, Zagreb, Croatia 2; Dubava University Hospital, Zagreb, Croatia 3
Published in the journal: ACTA CHIRURGIAE PLASTICAE, 65, 3-4, 2023, pp. 147-149
doi: https://doi.org/10.48095/ccachp2023147Introduction
Fasciotomy is the only option for urgent treatment of compartment syndrome. However, even a successful decompression can result in a large wound which can jeopardize the endangered extremity. Secondly, considering the wound becomes increasingly difficult to close primarily with time, options for wound closure should be evaluated as soon as possible. Closure is traditionally done by covering the wound with a split-thickness skin graft, and while this is simple, reliable, and generally available, it carries substantial morbidity. Several novel techniques were proposed for closure of fasciotomy wounds, some of which are simple but less effective, and others which are more complicated and often entail increased costs [1–3]. The use of negative pressure therapy increases the probability of primary wound closure, and can also be a useful adjunct to skin grafting. Two methods for fasciotomy wound closure that have recently gained popularity are the absorbable barbed suture and cable tie systems [4,5]. After analysing both techniques, we decided to combine them in a way we thought would achieve fast and effective wound closure.
Case description
Our combined method was tried on two patients. The first was a 35-year-old patient who underwent left ulnar nerve reconstruction four months prior. Three hours after surgery, he started displaying signs of compartment syndrome. Fasciotomy of the forearm was performed, releasing the anterior compartment. Muscles appeared well-perfused and contracting. The arm was placed in strict elevation and anti-edematous therapy was given. Over the next 2 days, the swelling of the muscles subsided, and closure of the wound was initiated on the 3rd postoperative day. Cable ties were sterilized and then assembled during the operation. We followed the instructions given by Govaert et al. [5] and positioned surgical staples evenly 2 cm apart (Fig. 1). Before inserting the cable ties, we positioned two absorbable barbed suture systems with the running intradermal technique starting from the edge of the wound as described by Özyurtlu et al. [4]. The wound was dressed with Vaseline gauze and sterile moist drapes. Postoperatively, the extremity was continuously held in an elevated position. The tightening commenced on the second day of closure and was performed bedside with i.v. analgesia. The tightening and approximation of the wound were performed every 48 hrs. Complete wound closure was achieved on the eighth postoperative day. Cable ties were removed 5 days later and the skin staples after 2 weeks (Fig. 2).
The second is a 39-year-old patient who sustained an open fracture of his left tibia. External fixation and end-to--end repair of the anterior tibial artery were performed. Two hours after surgery, he started displaying signs of compartment syndrome. Fasciotomy was performed through medial and lateral approaches. The leg was strictly elevated and the closure process was identical to the first patient, initiated three days after the fasciotomy. Complete closure of the wound was achieved in 2 weeks.
Fig. 1. Left forearm fasciotomy wound after application of cable ties plus absorbable barbed suture. 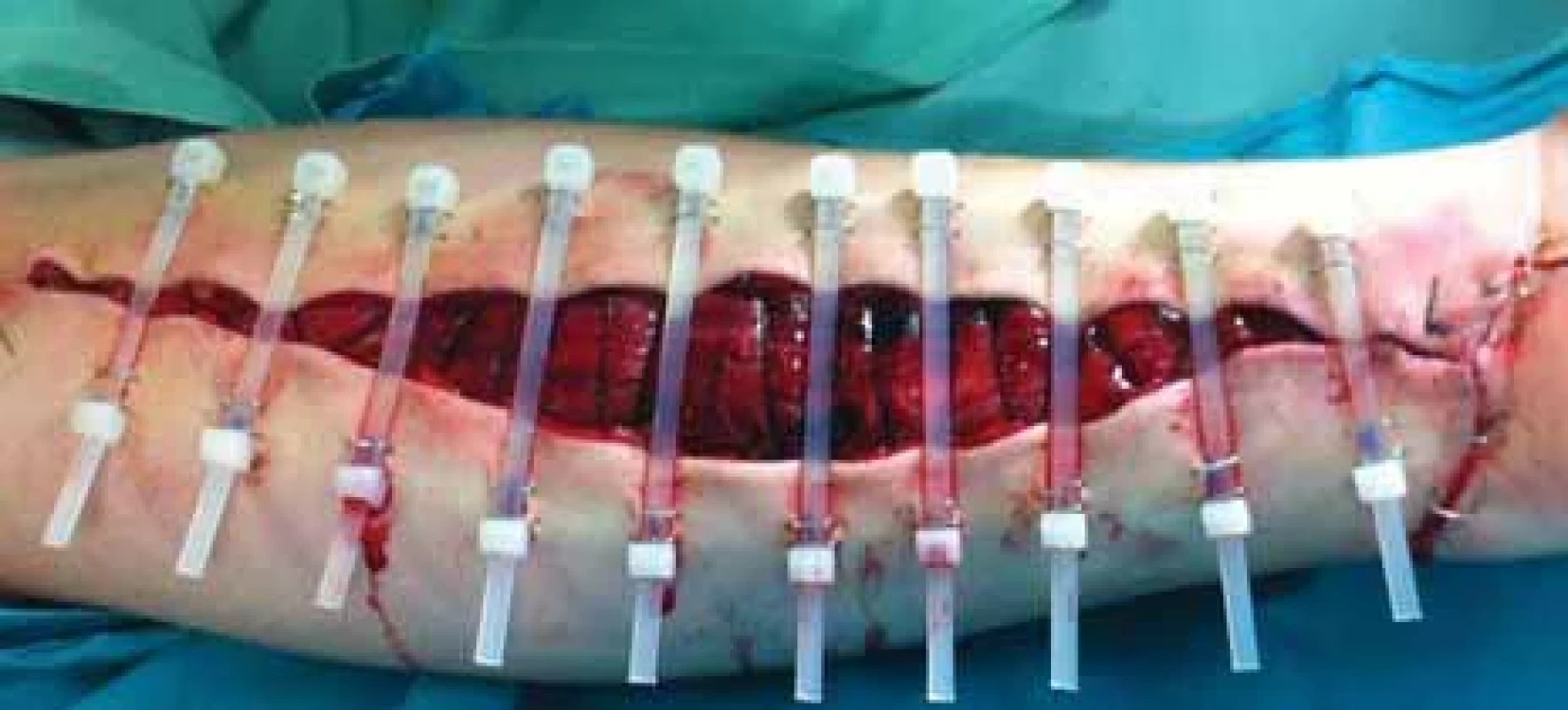
Fig. 2. Left forearm fasciotomy wound after removal of skin staples. 
Discussion
Both techniques have already been described in the literature as very successful. Govaert et al. described their experience with Ty-raps, which is a commercial brand of cable ties [5]. They reported their experience with 13 patients and 23 extremity fasciotomy wounds with excellent results in 91% of cases and only one patient required revision. In addition to excellent results, the authors emphasised the low cost and general availability of the technique. The second technique, described by Özyurtlu et al. [4], was reported in a five-case pilot study. In all patients, they achieved wound closure in mean 8.6 days (8–14), with no reported complications. They described their method as easy, rapid, and effective. By analysing both methods we found that each had its own shortcomings. The Ty-raps alone achieved dermotraction only on the part of the wound where the cable ties were positioned. The parts of the wound between the ties were lagging behind. In those spaces the skin edges became inverted and they were more difficult to advance. Once the wound was completely closed, this produced an uneven scar with prolonged scar formation. Secondly, the cable ties can cause pressure sores on the underlying skin. Absorbable barbed suture closure devices alone had the drawback of exhibiting tension for wound closure only on small segments which can lead to suture detachment from the wound edge and a mandated return to the OR.
Conclusion
By combining these two methods we feel we have found a way to overcome shortcomings of both. The absorbable barbed suture, when positioned correctly, helps to achieve dermotraction in the spaces between cable ties and reduces skin edge inversion by guiding skin edges towards each other, while the cable ties relieve the tension on the V-lock and reduce the chance of suture detachment. We believe that the combination of these two techniques has the potential to produce superior results to each technique performed separately, at a comparable cost and duration of closure.
Roles of authors
Kresimir Bulić and Hrvoje Kisić – clinical procedures;
Luka Bulić, Eva Brenner and Mia Lorencin Bulić – manuscript preparation;
Kresimir Bulić – supervision.
All authors have reviewed the manuscript and agree with its submission.
Conflict of interest: The authors disclose that they have no conflicts of interest.
Funding: This paper has received no funding.
Disclosure: All procedures performed in this study involving human participants were in accordance with ethical standards of the institutional and/or national research committee and with the Helsinki declaration and its later amendments or comparable ethical standards.
Zdroje
1. Barnea Y., Gur E., Amir A., et al. Delayed primary closure of fasciotomy wounds with Wisebands, a skinand soft tissue-stretch device. Injury. 2006, 37 (6): 561–566.
2. Ismavel R., Samuel S., Boopalan PR., et al. A simple solution for wound coverage by skin stretching. J Orthop Trauma. 2011, 25 (3): 127–132.
3. Zannis J., Angobaldo J., Marks M., et al. Comparison of fasciotomy wound closures using traditional dressing changes and the vacuum-assisted closure device. Ann Plast Surg. 2009, 62 (4): 407–409.
4. Özyurtlu M., Altınkaya S., Baltu Y., et al. A new, simple technique for gradual primary closure of fasciotomy wounds. Ulus Travma Acil Cerrahi Derg. 2014, 20 (3): 194–198.
5. Govaert GA., van Helden S. Ty-raps in trauma: a novel closing technique of extremity fasciotomy wounds. J Trauma. 2010, 69 (4): 972–975.
Eva Brenner
School of Medicine
University of Zagreb
Salata street 2
10000 Zagreb, Croatia
e-mail: eva.brenner13@gmail.comSubmitted: 22. 9. 2023
Accepted: 7. 2. 2024Štítky
Chirurgia plastická Ortopédia Popáleninová medicína Traumatológia
Článok vyšiel v časopiseActa chirurgiae plasticae
Najčítanejšie tento týždeň
2023 Číslo 3-4- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Kombinace metamizol/paracetamol v léčbě pooperační bolesti u zákroků v rámci jednodenní chirurgie
- Antidepresivní efekt kombinovaného analgetika tramadolu s paracetamolem
- Metamizol v terapii akutních bolestí hlavy
- Srovnání analgetické účinnosti metamizolu s ibuprofenem po extrakci třetí stoličky
-
Všetky články tohto čísla
- Editorial
- Diagnosis and treatment of Eagle’s syndrome and possible complications
- Scalp arteriovenous malformations – 20 years of experience in a tertiary healthcare centre
- The comparison of effectivity in breast cancer prevention between skin sparing and subcutaneous mastectomy – 20 years of experience
- Avascular necrosis of the maxilla after orthognathic surgery, a devastating complication? A systematic review of reported cases and clinical considerations
- 3D maxillofacial surgery planning – one decade development of technology
- A primary cutaneous carcinosarcoma of the retro auricular region, how to treat and literature review
- Combination of cable ties and barbed sutures for fasciotomy closure – two case reports
- Skin grafting on amputated lower limb, norepinephrine-induced ischemic limb necrosis – case report
- Abdominal wall reconstruction for extensive necrosis following abdominoplasty in a patient with subcostal scars – case report
- Acta chirurgiae plasticae
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Diagnosis and treatment of Eagle’s syndrome and possible complications
- Avascular necrosis of the maxilla after orthognathic surgery, a devastating complication? A systematic review of reported cases and clinical considerations
- 3D maxillofacial surgery planning – one decade development of technology
- Skin grafting on amputated lower limb, norepinephrine-induced ischemic limb necrosis – case report
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



