-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Diagnosis and treatment of Eagle’s syndrome and possible complications
Authors: V. Kozakovičová 1; A. Onderka 1,2; O. Res 1; J. Stránský 1; A. Kondé 3,4; J. Štembírek 1,2,5
Authors place of work: Clinic of Oral and Maxillofacial Surgery, University Hospital Ostrava, Czech Republic 1; Department of Craniofacial Surgery, Faculty of Medicine, University of Ostrava, Czech Republic 2; Department of Applied Mathematics, Faculty of Electrical Engineering and Computer Science, VSB – Technical University of Ostrava, Czech Republic 3; Department of the Deputy Director for Science, Research and Education, University Hospital Ostrava, Czech Republic 4; Laboratory of Molecular Morphogenesis, Institute of Animal Physiology and Genetics, Czech Academy of Sciences, Brno, Czech Republic 5
Published in the journal: ACTA CHIRURGIAE PLASTICAE, 65, 3-4, 2023, pp. 98-105
doi: https://doi.org/10.48095/ccachp202398Introduction
Eagle’s syndrome (ES) is defined as a group of symptoms associated with the elongation of the styloid process (SP) of the temporal bone or with ossification of the stylohyoid ligament [1]. This condition had, however, been described much earlier, as early as 1652 when the Italian surgeon Pietro Marchetti described intermittent respiratory distress as a symptom related to a prolonged SP. Still, only in 1973 was the syndrome defined by a German otorhinolaryngologist W. W. Eagle as pain that is caused by an excessive or shape-abnormal SP and ossification of the stylohyoid ligament [2–4]. This definition is still valid today.
Despite some interindividual variability, the normal length of SP measures generally around 20 mm. Currently, elongated SP is defined as one over 30 mm in length [4–7]. Elongated SP is a relatively common condition, occurring in approx. 4–7% of the population [8]. ES is more common in women in the third to fifth decades of their lives. Of those, only 4% can suffer from one of the clinical symptoms of ES, with one-sided pain in the cervical region being the most common [9].
Clinical symptoms of ES vary based on the structure affected by the elongated SP. This is influenced by the length, width, shape, angle of its action on the surrounding tissues, and the degree of calcification of the stylohyloid ligament [10]. The common symptoms include pain in the orofacial region or pharynx, otalgia, dysphagia, headache, sensation of a foreign body in the neck, pain in the submandibular region, or pain when sticking the tongue out. In special cases, we may observe taste perception disturbances, voice changes, tinnitus, or vertigo [3,11].
The questions of why ES manifests only in a small group of patients with the elongated SP and what triggers this condition remain largely unanswered. Trauma in the SP region, which leads to its elongation, or a personal history of tonsillectomy count among possible triggers [12]. In the literature, the connection between ES and dental procedures (e. g. wisdom tooth extraction) is also described [7].
The non-specificity of individual symptoms makes the diagnosis difficult. The palpability of the tip of the elongated SP through the tonsillar bed or, in case of significant elongation (about 7.5 cm), also in the submandibular/retroangular region is one of the important clinical signs of ES [13]. Therefore, imaging methods such as X-ray in the lateral head projection, OPG, and/or CT are required for establishing the diagnosis. SP is easily detectable at the lateral skull projection, although a problem can arise in patients with bilateral elongation, where overlaying shadows may make evaluation difficult. OPG is another useful imaging option, as it shows both processes as well as the temporomandibular joint and teeth. Interestingly, OPG measurements have confirmed the difference in mean SP length between men and women, with males tending to have, on average, 2 mm longer SP [14]. CT is currently considered the gold standard, ideally in combination with 3D reconstruction (Fig. 1) allowing to view the SP from multiple angles, to determine its exact width, length, and shape, as well as the full relation of the SP to the surrounding structures, particularly to large vessels. 3D reconstruction can also help to detect the potential compression of carotid arteries by the SP and, therefore, exclude another cause of cerebral ischemia [15–17].
There are several radiological classifications of SP according to the radiographic findings. The Langleis classification, characterizing the type of SP elongation and the pattern of stylohyoid ligament ossification, is one of the oldest ones [18].
Fig. 1. 3D reconstruction of CT scans in a patient with left-sided SP elongation. 
SP elongation types:
- type I – elongated – continuous SP extending over 30 mm;
- type II – pseudoarticulated – a less common type, in which a pseudoarticulation is formed by two mineralized parts, combined with mineralized ligaments in a false joint;
- type III – segmented – formed by two or more unconnected segments of the elongated SP or of the segmentally mineralized ligament.
Ossification patterns:
- circumferential calcification – long SP with a fine circumferential shadow of the cortica;
- partial calcification – a thicker shadow of the SP cortica with lighter areas inside;
- nodular calcification – a scalloped outline, potentially with lighter areas;
- full calcification – fully radiopaque, without lighter zones.
Alternatively, O’Caroll’s classification modified by Thun Szretter classified SP into four types according to the length [19]:
- type A – the apex of the SP projects over the foramen mandibulae;
- type B – the apex of the SP reaches between the foramen mandibulae and the angle of the mandible;
- type C – the apex of the SP extends below the level of the mandibular angle.
In patients with symptoms of carotid artery dissection caused by the irritation of the vessel wall by elongated SP, CT-angio or MRI-angio are used in the investigation to show potential subintimal hematoma and blood flow through the vessels [20].
ES can be treated either conservatively or surgically (by amputation of the elongated SP or ossified ligament using an extraoral or intraoral approach; Fig. 2, 3) [4,21].
From a surgical perspective, it should be noted that the location is anatomically relatively complex, which bears a risk of relatively high-risk of complications, such as trauma to the cranial nerves (in particular, VII, IX, and XII). This is due to the topographic location of the SP, which lies laterally to the cranial nerves VII and XII, the occipital artery, and the posterior belly of the digastric muscle. The facial nerve arises from the stylomastoid foramen and continues laterally through the parotid gland. The internal jugular vein with the internal carotid artery and the cranial nerves IX, X, XI, and XII lie medially to the SP [22].
Although classification for diagnosing elongated SP is at present clearly defined, this disease is being largely overlooked. Hence, this paper aimed to evaluate the incidence of ES at our workplace, as well as the success rate of surgical treatment and rate of complications at our department.
Methods
All patients referred to our department and diagnosed with temporomandibular joint disease were included in the retrospective evaluation. From these patients, those with a diagnosis of ES according to WHO were selected and their basic demographic parameters (gender, age), the length of SP on the CT scan, history of trauma in the SP region, clinical status before and after surgery, and any postoperative complications (deficiency of the facial (VII), glossopharyngeal (IX), and hypoglossal (XII) nerves) were recorded and evaluated.
In view of the small size of the resulting cohort, only methods of descriptive statistics were used for data analysis. The median and range (i.e., minimum and maximum) were chosen to describe the numerical variables. Absolute frequencies supplemented with relative frequencies (percentages) were used for the description of categorical variables. Associations of selected parameters were visualized using paired box plots. All analyses were performed in R software (version 4.2.3).
Fig. 2. Exposure of the SP from the extraoral approach. 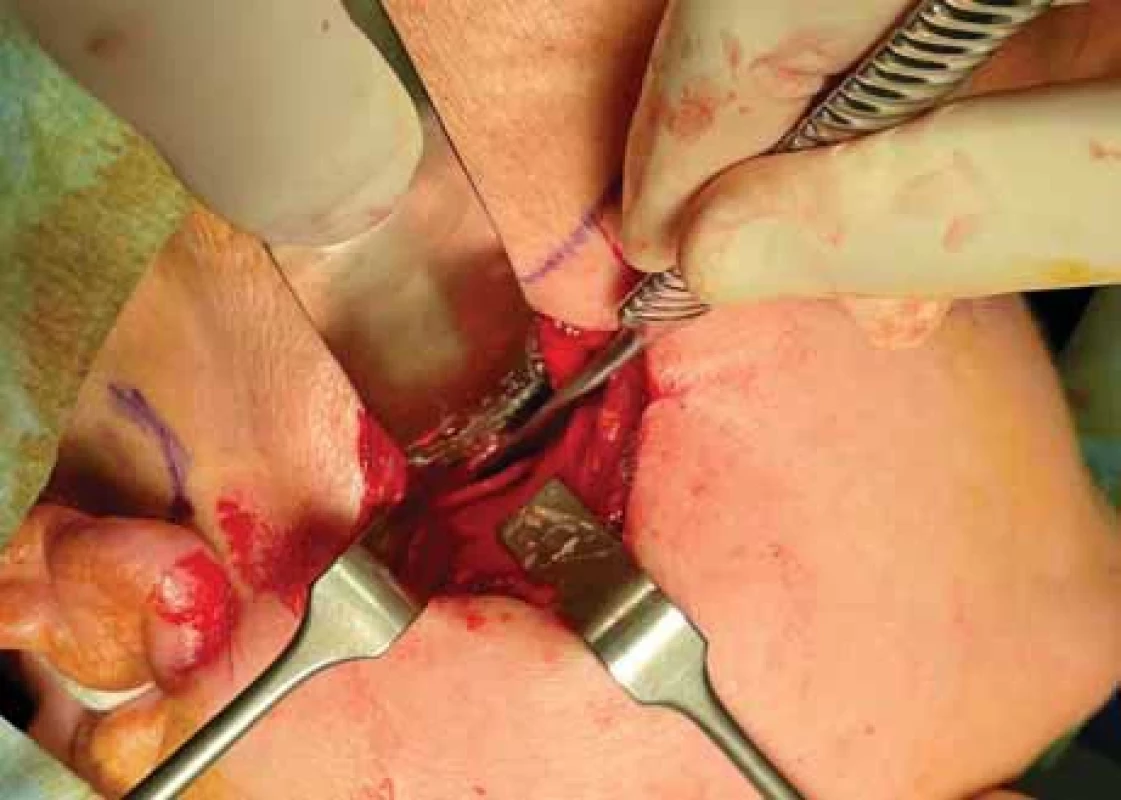
Fig. 3. Resected part of the SP. 
Results
In 2019–2023, ES was detected in nine individuals out of 2,716 patients diagnosed at our workplace with temporomandibular joint disease, i.e., the prevalence in this specific group was 0.33%. All nine patients were referred for surgical therapy. One of these patients did not turn up for the surgery and was excluded from further evaluation.
The final cohort thus consisted of eight patients, of which two were males (25%) and six were females (75%). All of them were at the age of 30 to 70, with a median age of 47 years. Three of them (38%) reported an injury in the facial area in their personal history – one had a car accident, another suffered an injury during aggressive rehabilitation, and the last one had a mandibular infraction fracture caused by a blow. None of the patients had a personal history of tonsillectomy.
In all patients, pain was the primary clinical symptom. Four individuals presented also with tinnitus, and three with vertigo. The median SP length was 40 mm on the right and 34 mm on the left (Tab. 1, Graph 1).
In all eight patients, surgery under general anesthesia using the extraoral approach was performed. The surgery was performed always only on one side (the symptomatic one) – on the right side in six patients, left-sided surgery was only performed in two patients. Seven out of the eight patients (88%) reported an improvement of their condition after the surgery, the problems failed to improve only in one patient. As illustrated in Graph 2, complete remission of the problems was observed predominantly in patients with shorter preoperative SP lengths; due to the small number of patients, however, this association could not be statistically evaluated. Interestingly, all three patients with the longest SP lengths had two features in common: a) they were symptomatic on the side with the shorter SP (and, therefore, their surgery was performed on the shorter side) and b) the surgery did not lead to a full resolution of the symptoms.
Postoperative complications such as deficit of the marginal branch of the facial nerve (n. VII.), limited sticking the tongue out (n. XII), and velopharyngeal insufficiency (n. IX) occurred in three cases (38%, Tab. 2) with longer SP (Graph 3). The marginal branch recovered within a year. One patient with velopharyngeal insufficiency improved after four months but the gradual improvement was complicated by a subsequent thyroidectomy, during which the recurrent laryngeal nerve was damaged; in the last patient with velopharyngeal insufficiency, the n. XII was also injured.
Tab. 1. Description of the patient group (N = 8). 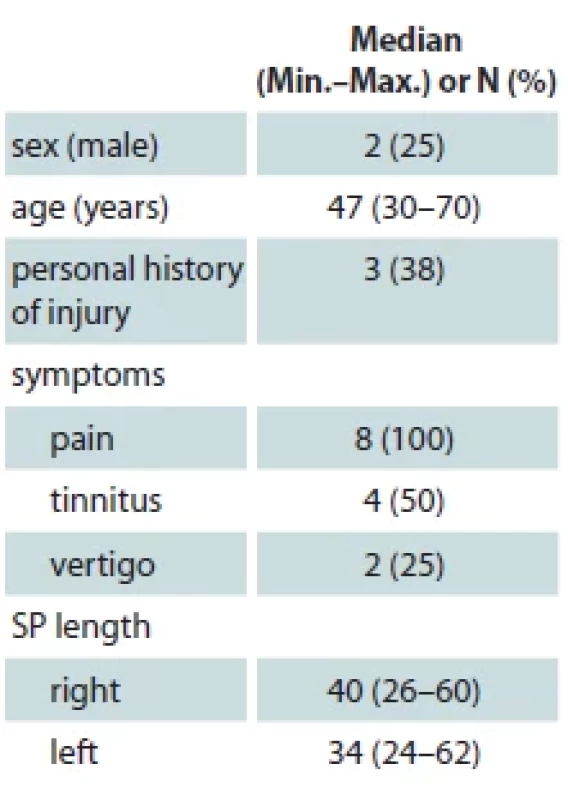
Values are expressed as median (minimum–maximum) or absolute and relative (%) frequencies. Graph 1. Paired boxplots of the right and left SP lengths in individual patients (N = 8). 
Graph 2. Visualization of the association between the SP length and postoperative improvement 
(full – green, partial – blue, none – red, N = 8). Discussion
ES etiology
Several hypotheses explaining the cause of ES have been proposed. Eagle himself described two types of the syndrome – the “styloid” and the “stylocarotic” syndrome [1,2]. The first, so-called “classic styloid syndrome”, occurs after tonsillectomy or another surgical procedure in the oropharynx and is characterized by isolated pain on the ipsilateral side of the neck in the tonsillar fossa. Other symptoms include dysphagia, odynophagia, tinnitus, a sensation of increased salivation, or a foreign body sensation in the throat. Very rarely, a voice change may also occur [1]. Eagle hypothesized that these symptoms are caused by the irritation of the cranial nerves V (trigeminal nerve), VII (facial nerve), IX (glossopharyngeal nerve), and X (vagus nerve) in the vicinity of the SP. The irritation is caused by the entrapment of one of the nerves in the granulation tissue forming after tonsillectomy [3]. According to a more recent theory, soft tissue damage during tonsillectomy can cause ossification of the stylohyoid ligament [6], which usually occurs between the 2nd and 12th month after the surgery [2].
The other type, so-called stylocarotic syndrome, is caused by excessive pressure of the SP on the internal and external carotid arteries in patients with no history of tonsillectomy. Symptoms then arise through irritation of the sympathetic plexus around the vessels. Pain in the eye and/or in the parietal region may occur. As cluster headaches and migraines manifest in the same way, the diagnosis is easy to confuse with these more common problems. Rarely, aphasia and visual field blackouts or even episodes of syncope may occur. Even more rarely, the patient may develop carotid dissection, manifesting as recurrent transient ischemic attacks or even hemiplegia [1,15,23].
The “post-traumatic” hypothesis suggests that the cause could lie in the compression of the neurovascular structures arising from the granulation tissue resulting from a fracture of the SP or of the ossified ligament as a consequence of blunt force. This theory is supported by the fact that ES often develops in patients following car accidents or assaults [6,24]. Another theory explains the development of complaints by underlying tendonitis in the stylohyoid ligament resulting from degenerative and inflammatory changes. It assumes that ossification of the SP and stylohyoid ligament are relatively common anatomical variations. This theory could explain radiographic findings of elongated SP and ossified stylohyoid ligaments in children and young adults with no previous history of trauma or surgery in the oropharynx. According to this theory, a gradual loss of soft tissue elasticity occurs at the interface between the lesser horns of the hyoid bone and the attachment of the stylohyoid ligament throughout life. This results in an increase in resistance while performing movement and, subsequently, in the development of secondary tendonitis [25].
Curiously, none of the patients in our group had a personal history of oropharyngeal surgery; we can, therefore, say that none of our cases was the “classic” ES. On the other hand, a possible association with a personal history of trauma could be observed in three patients. In one patient, who underwent intensive neck rehabilitation and some time later she lost consciousness without any cardiological defect, we can assume that this episode was provoked by increased traumatization of the sympathetic plexus. Another patient was expected to suffer from the stylocarotic etiology (due to the symptoms described above). As his complaints have only partially regressed, we can discuss both treatment failure (if the diagnosis was correct), or another, so far unknown, cause.
Tab. 2. Descriptive statistics of the patient group – surgery, complications, effect of the surgery. 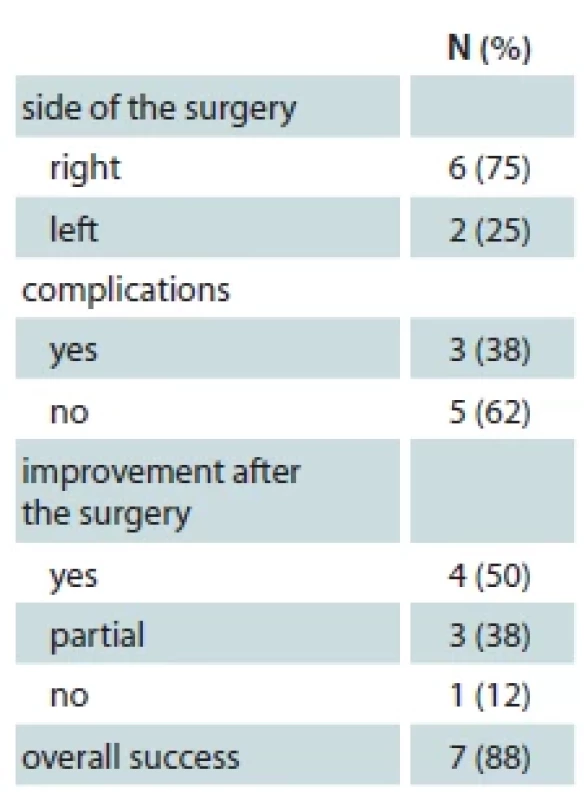
Values represent absolute and relative frequencies (%). Graph 3. Visualization of the association between the SP length and postoperative complications (yes – red, no – green, N = 8). 
Conservative treatment
Conservative treatment involves the use of medications, namely non-steroidal and anti-inflammatory analgesics in combination with antidepressants or anticonvulsants (gabapentin, amitriptyline, valproate, carbamazepine) depending on the symptoms. Minimally invasive therapy in the form of the application of long-term local anaesthetics with depot steroids is also possible. These can be applied intraorally to the tonsillar fossa after tonsillectomy or transcutaneously to the ligament of the hyoid bone [26,27]. Physiotherapy for pain reduction, aiming to relax muscles that are over the long term compressed as a result of the extended SP, is another possible treatment modality [9]. Conservative treatment is, however, often ineffective and in most cases, surgical solution is preferred. Conservative treatment is being considered particularly in patients with borderline SP length (approx. 30 mm) or in patients who disagree with the surgical solution. The effect of conservative therapy is, unfortunately, usually relatively short-term (months), but symptom improvement can help us diagnose ES. It can be also used in the post-operative period [28,29]. Another, although rarely used, approach that can be considered borderline between surgical and conservative treatment is manual breakage of the SP under local anesthesia through the intraoral approach. This technique is, however, considered relatively ineffective, not providing relief in most cases. Moreover, it is associated with a high-risk of damage to the important structures in the vicinity of the SP. For these reasons, it is usually not used these days [30].
Surgical treatment
The two most common surgical approaches are the intraoral and extraoral approach. In the intraoral approach, the surgeon first locates the SP in the tonsillar fossa. If a tonsil is present, it is removed in the first step. The incision is then made anteriorly to the tonsillar fossa and, after palpating the tip of the SP, it is bluntly dissected and exposed in the cranial direction as far as possible. The periosteum is dissected and the SP is resected as far as possible (or as necessary). Finally, the muscles and mucosa are sutured in layers. When using the intraoral approach, the SP cannot be resected up to the base, but even partial resection can lead to the resolution of the problems. This method is safe, simple and quick, with the additional major advantage of the absence of a scar on the neck. The surgery itself can even be performed under local anesthesia. The disadvantages include the possible risk of infection of the deep neck spaces, the risk of damage to large vessels, the limited visibility of the surgical field, and only partial resection of the SP. Despite being a safe surgical technique, it is not recommended for bilateral SP resection due to the high postoperative discomfort and risk of airway edema or contracture [31,32]. The problem of limited visibility in the surgical field can be resolved by the use of an endoscope [33].
The extraoral (transcervical) approach was first described by Loeser and Caldwell in 1942 [34]. The 4–5 cm long skin incision is performed submandibularly in an arch guided by a skin crease. The incision starts at the anterior margin of the sternocleidomastoideus (SCM) muscle in its upper two-thirds. It runs two to three fingers from the inferior margin of the mandible and continues towards the hyoid bone. Platysma and, subsequently, the superficial layer of the deep cervical fascia are intersected, reaching the inferior pole of the submandibular gland and the anterior border of the SCM muscle. The submandibular gland is pulled anteriorly and the SCM muscle is pushed backward. After palpating the extended SP, the posterior bellies of the digastricus and stylohyoideus muscles are pulled down. The overlying fascia, tendon, and periosteum are intersected and the surrounding tissues are retracted from the tip of the SP. The SP periosteum is removed as much as possible, ideally down to the base. The actual styloidectomy can be performed piezosurgically, using a reciprocating saw, drill, or Luer forceps. A vacuum drain is introduced and the wound is closed in layers [30,35,36]. The advantages of the extraoral approach include the clear identification of surrounding structures, the possibility of full SP resection, a lower risk of airway edema or of bacterial infection of cervical spaces, and, last but not least, greater patient comfort. The extraoral approach is generally recommended in cases of the stylocarotic type to prevent the risk of damage to large vessels. Unlike the intraoral approach, it is possible to resect both SPs a the same time [37]. Disadvantages include the necessity of general anesthesia, longer duration of the surgery, and, especially, the scar and the risk of facial nerve injury. Several modifications of this approach have been developed to minimize the scar and make it as little visible as possible. One such approach uses the incision for a face-lift, another one applies a preauricular incision extended to the inner side of the tragus. An endoscopic retroauricular approach has been also described [37–39]. Most recently, a technique using perioperative CT navigation has been developed and described [40].
Follow-up usually takes place for a period of one year in intervals of three months, the first follow-up for stitches removal is typically 7–10 days after the surgery. A follow-up OPG and early initiation of physiotherapy are also recommended [32]. Several studies report the success rate of both surgical and conservative treatment to be approximately 80%; in the case of conservative treatment, however, the improvement is often rather short-lived. Nevertheless, problems corresponding to the preoperative condition may cause retraction of the nerve into the scar or insufficient shortening of the SP [13].
Outcomes in our study group
In our patient group, 88% of patients reported at least partial improvement after the surgical treatment from the extraoral approach. Complete improvement after surgery was more likely in patients with shorter SP lengths. The fact that none of the three patients with bilateral SP > 45 mm improved fully presents us with a new question: Should these patients be surgically treated bilaterally? In a way, it is logical that shortening of the SP only on one side when the SP is bilaterally excessively long could fail to resolve problems. However, this has not been studied so far and in view of the low number of patients in our study, we can state this only as a hypothesis for further research. Moreover, it is interesting that all these patients suffered from problems on the side with the shorter SP.
Postoperative complications such as deficit of the mandibular marginal branch of the facial nerve (n. VII), limited sticking the tongue out (n. XII), or velopharyngeal insufficiency (n. IX) occurred in three cases of our group, all of them were cases with surgical removal of relatively large parts of the SP. Recovery of the facial nerve (n. VII) function occurred within 1 year after surgery. Rehabilitation with a physiotherapist was part of the post-operative care. In another patient with velopharyngeal closure deficiency (n. IX), improvement occurred spontaneously after 4 months, but the situation was complicated by the follow-up operation – thyroidectomy, when the recurrent laryngeal nerve was affected. The fact that all complications occurred in cases with SP original lengths over 45 mm indicates that it is necessary to be extremely cautious when performing surgery on patients with such extremely long SP – in such cases, the nerves often run in very close vicinity of the removed bone.
Neuropraxia of the cranial nerve XII has been described in the literature as a complication caused by its irritation during the unavoidable manipulation of this nerve in the vicinity of the SP, which temporarily manifested as limited sticking the tongue out, which spontaneously diminished after 6 months. Speech and swallowing were not affected [41]. We have also encountered complications associated with the damage to the cranial nerve XII leading to limited sticking the tongue out in our third patient. The condition was complicated by an injury to the nerve IX as well. After 8 months from the surgery, the condition was improving but has not reached full recovery.
As recommended in the literature [32], a follow-up OPG is performed in all patients in our department and if a post-operative complication is detected, rehabilitation/physiotherapy shortly follows.
Conclusions
In view of the wide spectrum of clinical manifestations, ES should be kept in mind in patients coming with symptoms including pain in the orofacial region or pharynx, otalgia, dysphagia, headache, sensation of a foreign body in the neck, pain in the submandibular region or pain when sticking the tongue out. This is especially true in patients with temporomandibular joint disease as well as in those with post-traumatic conditions or problematic teething or wisdom teeth removal. When this diagnosis is suspected, it is advisable to perform a CT scan with 3D reconstruction and determine the length of the SP. ES can be treated by conservative methods but surgical solutions are chosen more often due to their relatively high and long-term success rate. It is, however, necessary to respect the anatomical placement of the SP and bear in mind the possible complications of the surgery, especially in patients with long SP (approx. over 45 mm). Our results also suggest that in patients with bilaterally extremely long SPs, further research should focus on answering the question of whether bilateral surgery could be more successful than simply performing surgery on the symptomatic side.
Roles of authors
Veronika Kozakovičová – review of literature, manuscript writing, patient treatment;
Arnošt Onderka – review of literature, manuscript writing;
Oldřich Res – final manuscript approval, patient treatment;
Jiří Stránský – final manuscript approval, patient treatment;
Adéla Kondé – statistical analyses;
Jan Stembirek – manuscript writing, final manuscript approval, patient treatment.
Grant support: Ministry of Health of the Czech Republic – MZ ČR – RVO – FNOs/2023.
Disclosure: This manuscript has not been published and is not under consideration for publication elsewhere. We have no conflicts of interest to disclose. All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the Helsinki Declaration and its later amendments or comparable ethical standards.
Zdroje
1. Eagle WW. Symptomatic elongated styloid process; report of two cases of styloid process-carotid artery syndrome with operation. Arch Otolaryngol. 1949, 49 (5): 490–503.
2. Piagkou M., Anagnostopoulou S., Kouladouros K., et al. Eagle‘s syndrome: a review of the literature. Clin Anat. 2009, 22 (5): 545–558.
3. Fusco DJ., Asteraki S., Spetzler RF. Eagle‘s syndrome: embryology, anatomy, and clinical management. Acta Neurochir (Wien). 2012, 154 (7): 1119–1126.
4. Sharifi A., Kouhi A. Management of eagle syndrome. Curr Opin Otolaryngol Head Neck Surg. 2023, 31 (4): 276–280.
5. Kaufman SM., Elzay RP., Irish EF. Styloid process variation. Radiologic and clinical study. Arch Otolaryngol. 1970, 91 (5): 460–463.
6. Murtagh RD., Caracciolo JT., Fernandez G. CT findings associated with Eagle syndrome. AJNR Am J Neuroradiol. 2001, 22 (7): 1401–1402.
7. Li S., Blatt N., Jacob J., et al. Provoked Eagle syndrome after dental procedure: a review of the literature. Neuroradiol J. 2018, 31 (4): 426–429.
8. Chourdia V. Elongated styloid process (Eagle‘s syndrome) & severe headache. Indian J Otolaryngol Head Neck Surg. 2002, 54 (3): 238–241.
9. Wong ML., Rossi MD., Groff W., et al. Physical therapy management of a patient with Eagle syndrome. Physiother Theory Pract. 2011, 27 (4): 319–327.
10. Gervickas A., Kubilius R. Peculiarities of the investigation, clinics and treatment of stylohyoid syndrome and glossopharyngeal neuropathy. Medicina (Kaunas). 2004, 40 (10): 943–948.
11. González-García N., Porta-Etessam J., García-Azorín D. Eagle syndrome: toward a clinical delimitation. Neurologia (Engl Ed). 2021, 36 (6): 412–417.
12. Saccomanno S., Quinzi V., D‘Andrea N., et al. Traumatic events and Eagle syndrome: is there any correlation? A systematic review. Healthcare (Basel). 2021, 9 (7): 825.
13. Ghosh LM., Dubey SP. The syndrome of elongated styloid process. Auris Nasus Larynx. 1999, 26 (2): 169–175.
14. Balcioglu HA., Kilic C., Akyol M., et al. Length of the styloid process and anatomical implications for Eagle‘s syndrome. Folia Morphol (Warsz). 2009, 68 (4): 265–270.
15. Chuang WC., Short JH., McKinney AM., et al. Reversible left hemispheric ischemia secondary to carotid compression in Eagle syndrome: surgical and CT angiographic correlation. AJNR Am J Neuroradiol. 2007, 28 (1): 143–145.
16. Raina D., Gothi R., Rajan S. Eagle syndrome. Indian J Radiol Imaging. 2009, 19 (2): 107–108.
17. Smoot TW., Taha A., Tarlov N., et al. Eagle syndrome: a case report of stylocarotid syndrome with internal carotid artery dissection. Interv Neuroradiol. 2017, 23 (4): 433–436.
18. Langlais RP., Miles DA., Van Dis ML. Elongated and mineralized stylohyoid ligament complex: a proposed classification and report of a case of Eagle‘s syndrome. Oral Surg Oral Med Oral Pathol. 1986, 61 (5): 527–532.
19. Galletta K., Siniscalchi EN., Cicciù M., et al. Eagle syndrome: a wide spectrum of clinical and neuroradiological findings from cervico-facial pain to cerebral ischemia. J Craniofac Surg. 2019, 30 (5): e424–e428.
20. Peng J., Liu Z., Luo C., et al. Treatment of cervical artery dissection: antithrombotics, thrombolysis, and endovascular therapy. Biomed Res Int. 2017, 2017 : 3072098.
21. De Ravin E., Frost AS., Mady LJ., et al. Transcervical styloidectomy for Eagle syndrome. Head Neck. 2022, 44 (6): 1492–1495.
22. Yavuz H., Caylakli F., Yildirim T., et al. Angulation of the styloid process in Eagle‘s syndrome. Eur Arch Otorhinolaryngol. 2008, 265 (11): 1393–1396.
23. Farhat HI., Elhammady MS., Ziayee H., et al. Eagle syndrome as a cause of transient ischemic attacks. J Neurosurg. 2009, 110 (1): 90–93.
24. Mann A., Kujath S., Friedell ML., et al. Eagle syndrome presenting after blunt trauma. Ann Vasc Surg. 2017, 40 : 295.e5–295.e8.
25. Camarda AJ., Deschamps C., Forest D. I. Stylohyoid chain ossification: a discussion of etiology. Oral Surg Oral Med Oral Pathol. 1989, 67 (5): 508–514.
26. Glogoff MR., Baum SM., Cheifetz I. Diagnosis and treatment of Eagle‘s syndrome. J Oral Surg. 1981, 39 (12): 941–944.
27. Nickel J., Sonnenburg M., Scheufler O., et al. Eagle syndrome: diagnostic imaging and therapy. Rontgenpraxis. 2003, 55 (3): 108–113.
28. Salamone FN., Falciglia M., Steward DL. Eagle‘s syndrome reconsidered as a cervical manifestation of heterotopic ossification: woman presenting with a neck mass. Otolaryngol Head Neck Surg. 2004, 130 (4): 501–503.
29. Kim SM., Seo MH., Myoung H., et al. Osteogenetic changes in elongated styloid processes of Eagle syndrome patients. J Craniomaxillofac Surg. 2014, 42 (5): 661–667.
30. Chase DC., Zarmen A., Bigelow WC., et al. Eagle‘s syndrome: a comparison of intraoral versus extraoral surgical approaches. Oral Surg Oral Med Oral Pathol. 1986, 62 (6): 625–629.
31. Baharudin A., Rohaida I., Khairudin A. Transoral surgical resection of bilateral styloid processes elongation (eagle‘s syndrome). Acta Inform Med. 2012, 20 (2): 133–135.
32. Müderris T., Bercin S., Sevil E., et al. Surgical management of elongated styloid process: intraoral or transcervical? Eur Arch Otorhinolaryngol. 2014, 271 (6): 1709–1713.
33. Matsumoto F., Kase K., Kasai M., et al. Endoscopy-assisted transoral resection of the styloid process in Eagle‘s syndrome. Case report. Head Face Med. 2012, 8 : 21.
34. Fini G., Gasparini G., Filippini F., et al. The long styloid process syndrome or Eagle‘s syndrome. J Craniomaxillofac Surg. 2000, 28 (2): 123–127.
35. Bertossi D., Albanese M., Chiarini L., et al. Eagle syndrome surgical treatment with piezosurgery. J Craniofac Surg. 2014, 25 (3): 811–813.
36. Papadiochos I., Papadiochou S., Sarivalasis ES., et al. Treatment of Eagle syndrome with transcervical approach secondary to a failed intraoral attempt: surgical technique and literature review. J Stomatol Oral Maxillofac Surg. 2017, 118 (6): 353–358.
37. Williams JV., McKearney RM., Revington PJ. Eagle‘s syndrome: a novel surgical approach to the styloid process using a preauricular incision. J Oral Maxillofac Surg. 2011, 69 (6): 1617–1622.
38. Cicciù M. Real opportunity for the present and a forward step for the future of bone tissue engineering. J Craniofac Surg. 2017, 28 (3): 592–593.
39. Chen R., Liang F., Han P., et al. Endoscope-assisted resection of elongated styloid process through a retroauricular incision: a novel surgical approach to Eagle syndrome. J Oral Maxillofac Surg. 2017, 75 (7): 1442–1448.
40. Spalthoff S., Zimmerer R., Dittmann O., et al. Piezoelectric surgery and navigation: a safe approach for complex cases of Eagle syndrome. Int J Oral Maxillofac Surg. 2016, 45 (10): 1261–1267.
41. de Barros JF., Rodrigues MV., Barroso LA., et al. Eagle syndrome: an underdiagnosed cause of orofacial pain. BMJ Case Rep. 2021, 14 (1): e238161.
Jan Štembírek, MD, MDD, PhD
Clinic of Oral and Maxillofacial Surgery
University Hospital Ostrava
17. listopadu 1790/5
708 52 Ostrava
Czech Republic
e-mail: jan.stembirek@fno.czSubmitted: 10. 9. 2023
Accepted: 7. 2. 2024Štítky
Chirurgia plastická Ortopédia Popáleninová medicína Traumatológia
Článok vyšiel v časopiseActa chirurgiae plasticae
Najčítanejšie tento týždeň
2023 Číslo 3-4- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Kombinace metamizol/paracetamol v léčbě pooperační bolesti u zákroků v rámci jednodenní chirurgie
- Antidepresivní efekt kombinovaného analgetika tramadolu s paracetamolem
- Metamizol v terapii akutních bolestí hlavy
- Srovnání analgetické účinnosti metamizolu s ibuprofenem po extrakci třetí stoličky
-
Všetky články tohto čísla
- Editorial
- Diagnosis and treatment of Eagle’s syndrome and possible complications
- Scalp arteriovenous malformations – 20 years of experience in a tertiary healthcare centre
- The comparison of effectivity in breast cancer prevention between skin sparing and subcutaneous mastectomy – 20 years of experience
- Avascular necrosis of the maxilla after orthognathic surgery, a devastating complication? A systematic review of reported cases and clinical considerations
- 3D maxillofacial surgery planning – one decade development of technology
- A primary cutaneous carcinosarcoma of the retro auricular region, how to treat and literature review
- Combination of cable ties and barbed sutures for fasciotomy closure – two case reports
- Skin grafting on amputated lower limb, norepinephrine-induced ischemic limb necrosis – case report
- Abdominal wall reconstruction for extensive necrosis following abdominoplasty in a patient with subcostal scars – case report
- Acta chirurgiae plasticae
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Diagnosis and treatment of Eagle’s syndrome and possible complications
- Avascular necrosis of the maxilla after orthognathic surgery, a devastating complication? A systematic review of reported cases and clinical considerations
- 3D maxillofacial surgery planning – one decade development of technology
- Skin grafting on amputated lower limb, norepinephrine-induced ischemic limb necrosis – case report
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



