-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Ectopic pregnancies: a retrospective cohort analysis in a tertiary reference center in the Northeast Region of Brazil
Ektopická gravidita: retrospektivní kohortová analýza v referenčních centrech 3. úrovně v severovýchodním regionu Brazílie
Cíl:
Cílem této studie bylo prozkoumat klinické a epidemiologické charakteristiky, aspekty spojené s léčbou a výsledky u pacientek s ektopickou graviditou, které byly přijaty v nemocnicích 3. úrovně v severovýchodním regionu Brazílie.
Typ studie:
Retrospektivní kohortová studie, která zahrnula 101 pacientek s ektopickým těhotenstvím od února 2016 do února 2017.
Pracoviště:
Assis Chateaubriand Maternity School, Fortaleza, Ceará, Brazil.
Metody:
V studii jsme se soustředili na demografické charakteristiky, gynekologicko-porodnickou anamnézu, symptomy při přijetí, příslušné vyšetření [(β-hCG), transvaginální ultrazvuk, hladinu hemoglobinu] a léčbu.
Výsledky:
Průměrný věk pacientek byl 28 ± 6,6 let (14–48 let). Nejčastějšími symptomy byly abdominální bolest (96 %) a vaginální krvácení (82,4 %). Většina pacientek (53,5 %) neměla žádné rizikové faktory, pokud ano, byla to hlavně anamnéza předešlého ektopického těhotenství (16,9 %). Při přijetí mělo 63,4 % pacientek symptomy ruptury ektopické gravidity, 5,9 % pacientek bylo hemodynamicky nestabilních. Z pacientek s prasklou ektopickou graviditou až 61 % již vyhledalo lékařskou pomoc v jiném nemocničním zařízení. S ohledem na dostupné terapeutické metody, 78,2 % pacientek podstoupilo chirurgický zákrok (27,2 % laparoskopicky), u 16,8 % byl využit metotrexát a 5 % podstoupilo expektační management. Z pacientek léčených metotrexátem 41,2 % podstoupilo dodatečnou chirurgickou léčbu pro elevaci β-hCG (57,1 %) nebo pro klinické symptomy ruptury ektopické gravidity (42,9 %).
Závěr:
Pacientky byly ve většině případů přijaty s pokročilým stadiem ektopické gravidity, což dělalo konzervativní a levnější přístup složitějším. Přesto výsledky byly uspokojivé, s nízkým počtem komplikací a mateřských úmrtí.
klíčová slova
ektopická gravidita, metotrexát, epidemiologie, laparoskopie, laparotomie
Authors: F. D. E. Cordeiro 1; G. J. A. Alves 1,2; Edward Araujo Júnior 3
; L. E. E. Feitosa 1
Authors place of work: Department of Maternal and Child, Federal University of Ceará (UFC), Fortaleza-CE, Brazil 1; Department of Gynecology and Obstetrics, University of Fortaleza (UNIFOR), Fortaleza-CE, Brazil 2; Department of Obstetrics, Paulista School of Medicine – Federal University of São Paulo (EPM-UNIFESP), São Paulo-SP, Brazil 3
Published in the journal: Ceska Gynekol 2018; 83(6): 434-439
Category: Retrospektivní studie
Summary
Objective:
The objective of this study was to investigate the clinical and epidemiological characteristics of patients with ectopic pregnancy admitted to a tertiary center in the Northeast Region of Brazil and the aspects related to the treatment and outcomes in these women.
Design:
This was a retrospective cohort study of 101 patients diagnosed with ectopic pregnancy between February 2016 and February 2017.
Setting:
Assis Chateaubriand Maternity School, Fortaleza, Ceará, Brazil
Methods:
The data collected included demographic characteristics, gynecological-obstetric history, symptoms at admission, complementary examinations [chorionic gonadotropin (β-hCG) blood test, transvaginal ultrasound, and hemoglobin level], and treatment given.
Results:
The mean patient age was 28 ± 6.6 years (14–48 years). Abdominal pain (96%) and vaginal bleeding (82.4%) were the most prevalent symptoms. No risk factors were identified in most of the patients (53.5%), whereas the most frequently identified risk factor (16.9%) was a history of previous ectopic pregnancy. At admission, 63.4% of patients presented ruptured ectopic pregnancy and 5.9% had hemodynamic instability. Among the patients with ruptured ectopic pregnancy, 61% had already sought care at another center. With regard to the therapeutic options, 78.2% underwent surgery (27.2%, laparoscopy), 16.8% used methotrexate (MTX), and 5% underwent expectant management. Among those who received MTX, 41.2% needed subsequent surgery because of elevated blood β-hCG level (57.1%) and clinical signs of ruptured ectopic pregnancy (42.9%).
Conclusion:
The patients were admitted at an advanced stage of ectopic pregnancy, which made a more conservative and less costly treatment difficult. However, the outcomes were clinically satisfactory, with low complication rates and no maternal deaths.
Keywords
ectopic pregnancy, methotrexate, epidemiology, laparoscopy, laparotomy
INTRODUCTION
Ectopic pregnancy is defined as the implantation of the embryo outside the endometrial cavity [18]. Consistent data in relation to Brazilian epidemiology are scarce in the literature; however, based on international studies, it is estimated that 1.2%–1.4% of pregnancies are ectopic [19]. Ectopic pregnancies are associated with significant morbidity and mortality, accounting for approximately 75% of first-trimester maternal deaths and for 9% of all pregnancy-related deaths. Early diagnosis and management are the strategies with the most impact on reducing morbidity and mortality [9].
Most cases of ectopic pregnancy occur in the uterine tubes (98%), and the ampulla is the most common implantation site (80%) [5]. Although the etiology is not fully understood, several risk factors have been established, such as previous tubal surgery, previous ectopic pregnancy, use of an intrauterine device, pelvic inflammatory disease, salpingitis, infertility, and smoking [1].
Patients with ectopic pregnancy presenting to the emergency department more often present vaginal bleeding and abdominal pain and more rarely signs of hypovolemic shock. The diagnosis is based on clinical findings, blood chorionic gonadotropin (β-hCG) levels, and transvaginal ultrasound (TVUS). The combination of these tests is not always conclusive, and in some cases, surgical approach is both diagnostic and therapeutic, particularly in cases with hemodynamic instability [17].
An ectopic pregnancy can be treated using the following three approaches: expectantly, with medications, or surgically. Although it is a condition that has been described for centuries, there is still no consensus regarding its treatment [10].
The objective of this study was to describe the epidemiological and demographic characteristics of patients with a diagnosis of ectopic pregnancy admitted to a referral service in the Northeast Region of Brazil and the initial clinical presentation, diagnostic parameters, and treatment strategies for the condition.
MATERIALS AND METHODS
This was a retrospective cohort study including all women diagnosed with ectopic pregnancy and treated during the period from February 2016 to February 2017 at the Assis Chateaubriand Maternity School, Fortaleza, Ceará in the Northeast Region of Brazil. Initially, 109 patients with a diagnosis of ectopic pregnancy on admission were included; however, the medical records of eight patients were excluded because two could not be located and six received a different definitive diagnosis following histopathological analysis. Thus, the final analysis included 101 women. This study was approved by the Research Ethics Committee of the Federal University of Ceará, and because it was a retrospective study, informed consent was not required.
The patients were selected for expectant management if the ectopic pregnancy was intact, blood β-hCG levels were <200 mUI /L, and no heartbeats were detected. Follow-up was performed with β-hCG level testing every 48 h until its negativation. If there was an increase in the β-hCG level, the patient was readmitted for a different form of treatment.
To be eligible for management with methotrexate (MTX), the patients had to have an intact ectopic pregnancy. There was no standardization of the blood β-hCG level limits or of the size of the mass in the selection of the patients to be selected for this type of treatment. The treatment regimen used in tubal ectopic pregnancies was a single intramuscular dose (50 mg/m2) of MTX, which was repeated after 7 days if there was a drop of <15% in the β-hCG level between days 4 and 7 after the single dose. For non-tubal ectopic pregnancies, the treatment regimen used was multiple intramuscular doses (1 mg/kg) of MTX on days 1, 3, 5, and 7, alternating with folic acid (0.1 mg/kg) taken orally on days 2, 4, 6, and 8. The multiple-dose regimen could be interrupted before the administration of all four doses if there was a drop in the β-hCG level of >15% within 48 h.
The patients received surgical treatment when the ectopic pregnancy had ruptured, when they were not eligible for the other methods, or when they refused non-surgical treatment. The choice between the laparotomic and laparoscopic approaches was dependent on hemodynamic stability, as well as on the availability of the videolaparoscopic apparatus.
Data collected included demographic characteristics, gynecological-obstetric history, symptoms at admission, complementary exams performed [blood β-hCG level, TVUS, and hemoglobin (Hb) level], and treatment. The data were transferred to an Excel 2007 spreadsheet (Microsoft Corp., Redmond, WA, USA) and analyzed using the IBM© SPSS© Statistics software, version 22.0 (IBM© Corp., Armonk, NY, USA). The Student‘s t test was used to compare the ruptured and intact tubal pregnancy groups. A significance level of p < 0.05 was used.
RESULTS
The frequency of ectopic pregnancies in relation to the number of live births during the period analyzed was 1.97 of 100. The mean age[± standard deviation (SD)] of the patients was 28 ± 6.6 years, with a range of 14-48 years (Table 1). Symptoms at admission included abdominal pain in 96% of patients, vaginal bleeding in 82.4%, and both in 80.2%. Among the patients, 31.7% were primigravida and 33.6% had a history of previous cesarean delivery. In terms of risk factors, there was a predominance of a history of previous ectopic pregnancy (16.8%). With regard to location, 92% of patients exhibited tubal ectopic pregnancy (Table 2).
Tab. 1. Maternal characteristics 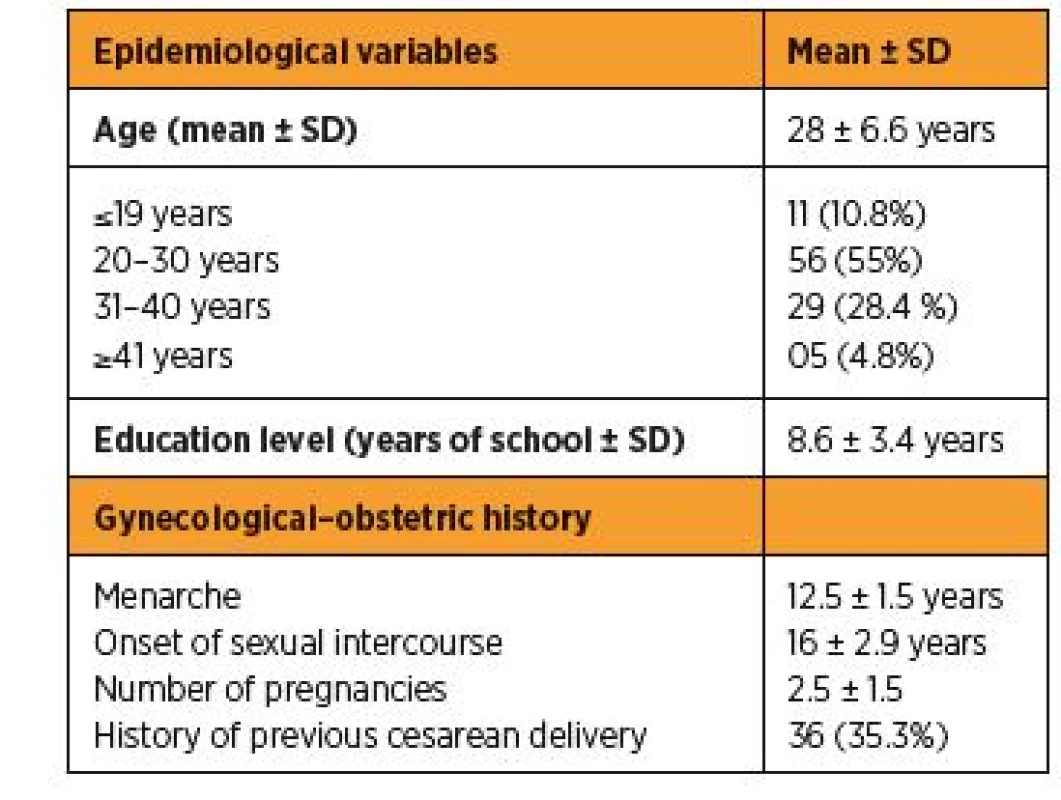
SD – standard deviation Tab. 2. Frequency distribution of ectopic pregnancies by location, type of initial treatment, and risk factors 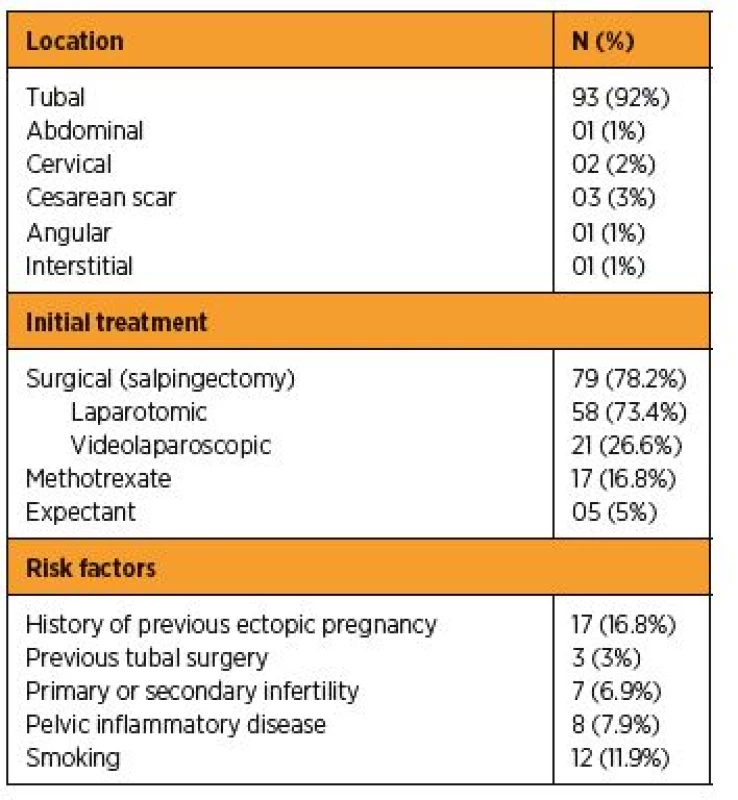
At admission, 63.4% of the patients were diagnosed with ruptured ectopic pregnancy and 5.9% with hemodynamic instability. Among the patients with ruptured ectopic pregnancies, 61% had already sought medical care in another center. Comparing the intact and ruptured pregnancies, the mass sizes on TVUS were smaller in the patients with intact ectopic pregnancy (p = 0.003) and there were no statistical differences in the other variables between the two types of ectopic pregnancy (Table 3). TVUS with the finding of free fluid in the cavity had a sensitivity of 87% and a specificity of 88% for the diagnosis of ruptured ectopic pregnancy compared with the intraoperative finding of hemoperitonitis.
Tab. 3. Comparison between intact and ruptured ectopic pregnancies 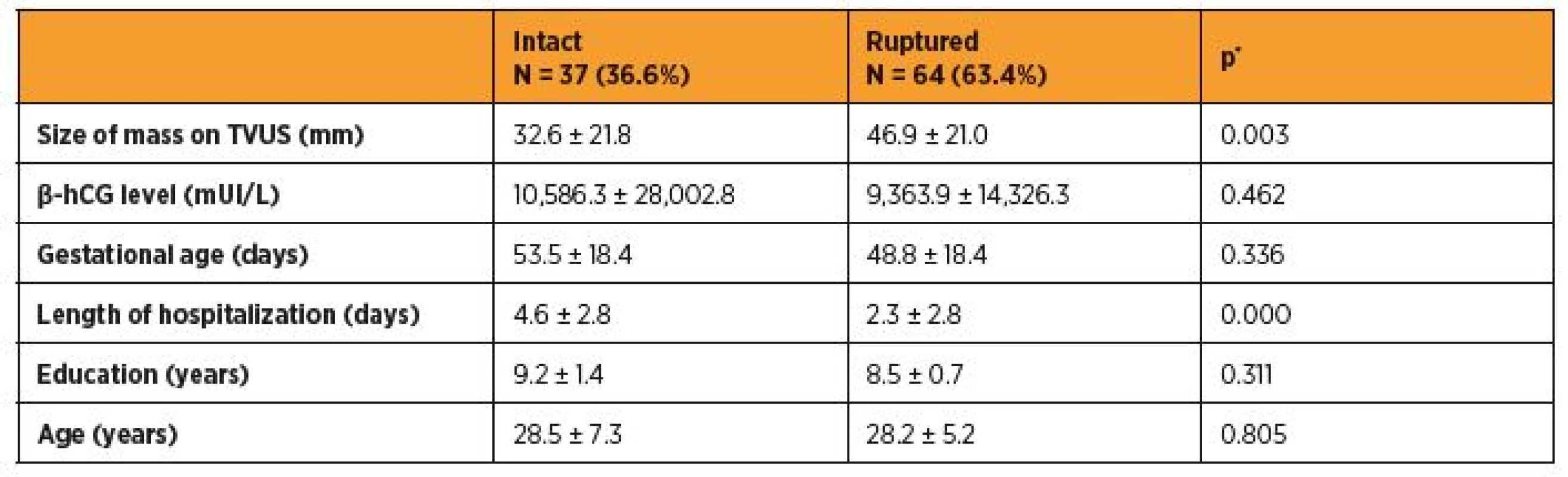
TVUS: transvaginal ultrasound
*Student’s t testWith regard to the initial treatment, 79 (78.2%) patients underwent surgery (26.6%, laparoscopically), 17 (16.8%) were clinically treated with MTX, and 5 (5%) were maintained on expectant management. The analysis of the relation between the initial treatment modality and hospitalization time showed that the patients who underwent surgery spent a lower mean number of days in the hospital than the others (2.5 vs. 5.0 days; p < 0.05). Among the patients who were administered MTX, 41.2% required complementary surgery for the elevation of blood β-hCG levels (57.1%) and for clinical signs of rupture (42.9%). The initial blood ?-hCG level (p = 0.055) and the size of the mass on TVUS (p = 0.962) were not statistically significant in terms of clinical treatment with MTX. Expectant management was successful in all the patients.
With regard to complications, only one patient needed a hysterectomy for difficult-to-control bleeding and 8% of the patients needed blood transfusions. The mean Hb in the patients who received transfusion was 6.3 g/dL and that in patients who did not receive transfusions was 11.1 g/dL. None of the patients died from ectopic pregnancy during the study period or required treatment in the intensive care unit.
DISCUSSION
The prevalence of ectopic pregnancy in relation to the number of live births during the period analyzed was 1.97 of 100. In Brazil, there are no records of the prevalence of ectopic pregnancies that would allow broader comparisons. A standalone study conducted in a university department reported a rate of 1.02 of 100 during the period from 2000 to 2004 [7].
The frequency of symptoms at admission was similar to that reported in other studies in the literature. According to Tay et al. [23], ectopic pregnancies usually present after 7 weeks of amenorrhea, with symptoms including abdominal pain in 97% of patients and vaginal bleeding in 79%. However, considering only these medical history and physical examination data, it is not possible to confirm or rule out ectopic pregnancy. Differential diagnosis with spontaneous abortion, ovarian torsion, pelvic inflammatory disease, appendicitis, and other causes of acute abdomen is mandatory. Complementary exams assist in this differentiation; however, in some patients, the definitive diagnosis is only made after surgery.
The presence of known risk factors may increase the degree of suspicion, but the absence of these factors does not reduce this suspicion. Our analysis showed that more than 50% of the patients had no risk factors, which is consistent with the data already described in the literature [13]. We observed no statistical difference in the analyzed factors between the patients with intact and ruptured ectopic pregnancy.
In terms of the location of the ectopic pregnancy, we observed a higher frequency of non-tubal pregnancies compared with that described in the literature (8% vs. 2%) [5], most likely because this study was conducted in a tertiary high-complexity center that receives cases referred from the entire state of Ceará, Northeast Region of Brazil.
Compared with other emergency cases, we observed a higher rate of ruptured ectopic pregnancies at admission [4, 22]. According to Belic et al. [3], 80% of cases of ectopic pregnancy can be diagnosed prior to rupture. Women who present with ruptured ectopic pregnancies probably had previously ignored prodromal symptoms because tubal rupture is rarely sudden given that trophoblast invasion occurs gradually [23].
In recent decades, TVUS has become one of the main methods for the diagnosis of ectopic pregnancies. Data from the literature show that between 87% and 99% of tubal pregnancies can be reliably diagnosed using TVUS [11, 24]. In our case series, TVUS with the finding of free fluid in the cavity had a sensitivity of 87% and a specificity of 88% for the diagnosis of ruptured ectopic pregnancy when compared to intraoperative findings of hemoperitonitis.
With regard to the initial treatment, 78.2% underwent surgery (26.6%, laparoscopy). This rate was higher than that reported in a study from the United Kingdom, where there are programs focused on early diagnosis (78.2% vs. 69.0%). The discrepancy was even higher when we evaluated the surgical technique used, with 99% of patients undergoing laparoscopy technique in the United Kingdom. 11 This discrepancy is mostly due to late diagnosis and the lack of technical and professional conditions for using videolaparoscopy.
The efficacy and safety of clinical treatment with MTX in patients with ectopic pregnancy have been widely demonstrated [21]. Treatment with MTX was used in 16.8% of patients, with a success rate of 59%. Considering that there was no standard protocol in place in our center during the study period, a comparison of the success rate with that reported in the literature would not be valid. Nevertheless, the success rates of MTX reported in the literature ranged from 75% to 96%, depending on the level of the blood β-hCG level [8]. Although no association between the blood β-hCG levels and success rate was shown in our study, this relationship is already well-established [16]. Blood β-hCG levels of < 5.000 mUI/L at the beginning of treatment correspond to success rates of 96% and those of 5.000–9.999 mUI/L correspond to success rates of 85% [15, 20]. The mean ± SD of β-hCG level in patients who were administered MTX in this study was 18.434 ± 1.777 mUI/L, which explains the success rate being lower than that described in other studies [2, 12].
Although expectant treatment is not recommended by some international protocols, there is growing evidence that it is safe and can be used in up to one-third of patients with ectopic pregnancies with success rates of 59%-71%, provided it is used in stable patients with low blood β-hCG levels and who are able to attend clinical follow-up [14, 25]. In our case series, only five (5%) patients underwent expectant management because of the low probability of clinical follow-up due to low socioeconomic levels. The success rate of expectant treatment was 100%, with only one patient being readmitted for surgical treatment for worsening symptoms of abdominal pain and suspicion of rupture (not confirmed intraoperatively). This case was not considered a failure of expectant management, but rather a diagnostic error with regard to rupture. However, the small sample size did not allow drawing conclusions about the efficacy of the expectant treatment.
Blood transfusion was performed in only 8% of the patients, a rate lower than that reported by other centers that also had high rates of tubal rupture at admission [6, 22]. Studies conducted in India [22] and Nigeria [6] showed transfusion rates of 60% and 65%, respectively, even with mean Hb levels higher than those observed in our study. This difference was probably a result of awareness programs established in our center and restricting blood transfusions to patients with hemodynamic instability.
CONCLUSION
In summary, these results corroborate the idea that attention to patients with ectopic pregnancy must be improved. The rate of early diagnosis was low, and most of the patients were hospitalized with a clinical diagnosis of tubal rupture, which has higher morbidity and mortality rates. Advances in early diagnosis allow minimally invasive surgical treatments, as well as clinical approaches such as the use of MTX.
Prof. Edward Araujo Júnior, PhD
Rua Belchior de Azevedo, 156 apto. 111 Torre Vitoria
São Paulo-SP, Brazil
CEP 05089-030
e-mail: araujojred@terra.com.br
Zdroje
1. Ankum, WM., Mol, BW., Van der Veen, F., Bossuyt, PM. Risk factors for ectopic pregnancy: a meta-analysis. Fertil Steril, 1996, 65(6), p. 1093–1099.
2. Barnhart, KT., Gosman, G., Ashby, R., Sammel, M. The medical management of ectopic pregnancy: a meta-analysis comparing „single dose“ and „multidose“ regimens. Obstet Gynecol, 2003, 101(4), p. 778–784.
3. Belics, Z., Gérecz, B., Csákány, MG. Early diagnosis of ectopic pregnancy. Orv Hetil, 2014, 155(29), p. 1158–1166.
4. Berry, J., Davey, M., Hon, MS., Behrens, R. A 5-year experience of the changing management of ectopic pregnancy. J Obstet Gynaecol, 2016, 36(5), p. 631–634.
5. Bouyer, J., Coste, J., Fernandez, H., et al. Sites of ectopic pregnancy: a 10 year population-based study of 1800 cases. Hum Reprod, 2002, 17(12), p. 2224–2230.
6. Cornelius, AC., Onyegbule, A., Onyema Uchenna, ET., Duke, OA. A five year review of ectopic pregnancy at Federal Medical Centre, Owerri, South East, Nigeria. Niger J Med, 2014, 23(3), p. 207–212.
7. Fernandes, AM., Moretti, TB., Olivotti, BR. [Epidemiological and clinical aspects of ectopic pregnancies at a university service between 2000 and 2004]. Rev Assoc Med Bras (1992), 2007, 53(3), p. 213–216.
8. Guvendag Guven, ES., Dilbaz, S., Dilbaz, B., et al. Comparison of single and multiple dose methotrexate therapy for unruptured tubal ectopic pregnancy: a prospective randomized study. Acta Obstet Gynecol Scand, 2010, 89(7), p. 889–895.
9. Hamid, AAA., Yousry, A., Radi, SAE., et al. Clinical audit of ectopic pregnancy. Electronic Physician, 2017, 9(3), p. 4009–4013.
10. Hsu, JY., Chen, L., Gumer, AR., et al. Disparities in the management of ectopic pregnancy. Am J Obstet Gynecol, 2017, 217(1), p. 49.e1–49.e10.
11. Kirk, E., Papageorghiou, AT., Condous, G., et al. The diagnostic effectiveness of an initial transvaginal scan in detecting ectopic pregnancy. Hum Reprod, 2007, 22(11), p. 2824–2828.
12. Lipscomb, GH. Medical management of ectopic pregnancy. Clin Obstet Gynecol, 2012, 55(2), p. 424–432.
13. Marion, L., Meeks, GO. Ectopic pregnancy: History, incidence, epidemiology, and risk factors. Clin Obstet Gynecol, 2012, 55(2), p. 376–386.
14. Mavrelos, D., Nicks, H., Jamil, A., et al. Efficacy and safety of a clinical protocol for expectant management of selected women diagnosed with a tubal ectopic pregnancy. Ultrasound Obstet Gynecol, 2013, 42(1), p. 102–107.
15. Menon, S., Colins, J., Barnhart, KT. Establishing a human chorionic gonadotropin cutoff to guide methotrexate treatment of ectopic pregnancy: a systematic review. Fertil Steril, 2007, 87(3), p. 481–484.
16. Nowak-Markwitz, E., Michalak, M., Olejnik, M., Spaczynski, M. Cutoff value of human chorionic gonadotropin in relation to the number of methotrexate cycles in the successful treatment of ectopic pregnancy. Fertil Steril, 2009, 92(4), p. 1203–1207.
17. Orazulike, NC., Konje, JC. Diagnosis and management of ectopic pregnancy. Womens Health (Lond), 2013, 9(4), p. 373–385.
18. Pisarska, MD., Carson, SA., Buster, JE. Ectopic pregnancy. Lancet, 1998, 351(9109), p. 1115–1120.
19. Rana, P., Kazmi, I., Singh, R., et al. Ectopic pregnancy: a review. Arch Gynecol Obstet, 2013, 288(4), p. 747–757.
20. Sagiv, R., Debby, A., Feit, H., et al. The optimal cutoff serum level of human chorionic gonadotropin for efficacy of methotrexate treatment in women with extrauterine pregnancy. Int J Gynaecol Obstet, 2012, 116(2), p. 101–104.
21. Soliman, KB., Saleh, NM., Omran, AA. Safety and efficacy of systemic methotrexate in the treatment of unruptured tubal pregnancy. Saudi Med J, 2016, 27(7), p. 1005–1010.
22. Tahmina, S., Daniel, M., Solomon, P. Clinical analysis of ectopic pregnancies in a Tertiary Care Centre in Southern India: A six-year retrospective study. J Clin Diagn Res, 2016, 10(10), p. QC13–QC16.
23. Tay, JI., Moore, J., Walker, JJ. Ectopic pregnancy. BMJ, 2000, 320(7239), p. 916–919.
24. van Mello, NM., Mol, F., Ankum, WM., et al. Ectopic pregnancy: how the diagnostic and therapeutic management has changed. Fertil Steril, 2012, 98(5), p. 1066–1073.
25. van Mello, NM., Mol, F., Verhoeve, HR., et al. Methotrexate or expectant management in women with an ectopic pregnancy or pregnancy of unknown location and low serum hCG concentrations? A randomized comparison. Hum Reprod, 2012, 28(1), p. 60–67.
Štítky
Detská gynekológia Gynekológia a pôrodníctvo Reprodukčná medicína
Článek Rejstřík
Článok vyšiel v časopiseČeská gynekologie
Najčítanejšie tento týždeň
2018 Číslo 6- Ne každé mimoděložní těhotenství musí končit salpingektomií
- I „pouhé“ doporučení znamená velkou pomoc. Nasměrujte své pacienty pod křídla Dobrých andělů
- Mýty a fakta ohledně doporučení v těhotenství
- Gynekologické potíže pomáhá účinně zvládat benzydamin
-
Všetky články tohto čísla
- The effect of myomectomy on the morphology uterine and tubal factor of infertility
- Radiofrequency endometrial ablation – new possibility of heavy menstrual bleeding conservative treatment
- Perinatal mortality and morbidity in Slovak Republic in the years 2007–2015
- Ectopic pregnancies: a retrospective cohort analysis in a tertiary reference center in the Northeast Region of Brazil
- Asherman‘s syndrome: the description of two case reports
- Gynecological tumor triplicity
- Fetal and neonatal alloimmune thrombocytopenia
- Strumal carcinoid of the ovary – report of two cases and review of literature
- New potential biomarkers for preeclampsia prediction
- Surrogate motherhood: the contradicitons in terminology
- Etiology, risk factors, and methods of postpartum depression prevention
- Informace z 15. mezinárodního sympozia imunologie reprodukce a 50. výročního mezinárodního koordinačního výboru reprodukční imunologie - Varna, Bulharsko, 15.–17. 6. 2018
- Zápis z jednání volební komise pro volby výboru Sekce pro otázky menopauzy České gynekologické a porodnické společnosti ČLS JEP
- Zápis z jednání volební komise pro volby výboru Sekce ultrazvukové diagnostiky České gynekologické a porodnické společnosti ČLS JEP
- Stárnutí kmenových buněk – kdy je nejvhodnější jejich odběr?
- Rejstřík
- Česká gynekologie
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Etiology, risk factors, and methods of postpartum depression prevention
- Radiofrequency endometrial ablation – new possibility of heavy menstrual bleeding conservative treatment
- Asherman‘s syndrome: the description of two case reports
- Perinatal mortality and morbidity in Slovak Republic in the years 2007–2015
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



