-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Pandemic fear and psychological resilience in pregnant women after the pandemic – a study in Turkey
Pandemický strach a psychická odolnost u těhotných žen po pandemii – studie v Turecku
Cíl: Cílem této studie bylo prozkoumat u těhotných žen míru strachu, deprese, stresu a úzkosti spojených s pandemií, a to v různých trimestrech v období po pandemii, a určit jejich souvislost s psychickou odolností. Metody: Do studie bylo zařazeno celkem 250 žen, z toho 125 těhotných a 125 zdravých kontrol. Ženy byly dále rozděleny do tří skupin podle trimestru těhotenství. K měření deprese, úzkosti, stresu a psychické odolnosti byla použita škála deprese, úzkosti a stresu (DASS-21 – Depression Anxiety Stress Scale 21), škála strachu z epidemie (EDAS – Epidemic Disease Anxiety Scale) a zkrácená škála psychické odolnosti (SPRS – Short Psychological Resilience Scale). Výsledky: Těhotné ženy měly významně vyšší celkové skóre DASS-21 [19 (4–42) ], oproti zdravým kontrolám [11 (1–42) ], p = 0,001. Prevalence deprese, úzkosti a stresu u těhotných byla 23,2 %, 44 % a 20 % oproti 12,8 %, 31,2 % a 9,6 % u zdravých kontrol. Celkové skóre DASS-21 bylo nejvyšší v I. trimestru (21,2 ± 5,8) a III. trimestru (22,8 ± 8,9) a nejnižší v II. trimestru (16,1 ± 6,9). U DASS-21 byla zaznamenána pozitivní korelace s celkovým skóre EDAS a se subškálou vnímání pandemie. Celkové skóre SPRS mělo negativní korelaci s úzkostí, stresem a celkovým skóre DASS-21. Závěr: V období po pandemii byla u těhotných žen zaznamenána vyšší míra deprese, úzkosti, stresu a strachu z pandemie než u netěhotných žen. U těhotných žen byla zjištěna negativní korelace mezi psychickou odolností a depresí, úzkostí či stresem. Tyto závěry svědčí o tom, že pandemie negativně ovlivňuje mentálního zdraví těhotných žen a rovněž ukazují důležitost služeb poskytujících psychickou podporu při ochraně jejich duševního zdraví.
Klíčová slova:
Pregnancy – pandemic-related fear – psychological resilience
Authors: M. Akkuş 1
; Fatih Akkuş 2
Authors place of work: Department of Psychiatry, Faculty of Medicine, Kütahya Health Sciences University, Kütahya, Turkey 1; Division of Perinatology, Faculty of Medicine, Necmettin Erbakan University, Konya, Turkey 2
Published in the journal: Ceska Gynekol 2024; 89(1): 22-28
Category: Původní práce
doi: https://doi.org/10.48095/cccg202422Summary
Aims: The aim of this study was to investigate the levels of pandemic-related fear, depression, stress and anxiety in pregnant women in different trimesters after the pandemic and to examine their relationship with psychological resilience. Methods: A total of 250 women were included in the study, including 125 pregnant women and 125 healthy controls. The participants were divided into three groups according to their trimester of pregnancy. The Depression-Anxiety-Stress Scale 21 (DASS-21), the Epidemic Disease Anxiety Scale (EDAS) and the Short Psychological Resilience Scale (SPRS) were used to measure depression, anxiety, stress and psychological resilience. Results: Pregnant women had significantly higher DASS-21 total scores [19 (4–42) ] than healthy controls [11 (1–42) ], P = 0.001. The prevalence of depression, anxiety and stress was 23.2%, 44% and 20% respectively in pregnant women compared to 12.8%, 31.2% and 9.6% in healthy controls. DASS-21 total scores were highest in the 1st (21.2 ± 5.8) and 3rd (22.8 ± 8.9) trimesters and lowest in the 2nd (16.1 ± 6.9) trimesters. The DASS-21 total score was positively correlated with the EDAS total score and the pandemic perception subscale. SPRS total score was negatively correlated with anxiety, stress and DASS-21 total score. Conclusion: Pregnant women experienced higher levels of depression, anxiety, stress, and pandemic anxiety than non-pregnant women in the post-pandemic period. Psychological resilience was negatively associated with depression, anxiety, and stress in pregnant women. These findings indicate that the pandemic negatively affects the mental health of pregnant women and the importance of providing psychological support services to protect their mental health.
Keywords:
strach spojený s pandemií – psychická odolnost – těhotenství
Introduction
Epidemic diseases are those that occur in a community or area at a higher rate than expected and have either single or multiple sources of origin [1]. Multiple factors, such as viruses, bacteria, fungi, and parasites, can cause epidemics. Epidemics can significantly impact public health, causing widespread illness, mortality and social and economic disruption [2]. Outbreaks may disproportionately impact vulnerable groups such as the elderly, children, pregnant women, immunocompromised people, and those with inadequate access to health care [3].
Pregnancy is a transformational and sensitive time in a woman‘s life, with physical, emotional, and psychological changes [4]. Pregnant women exhibit heightened vigilance regarding their own health and the well-being of their unborn child. Adverse life occurrences, such as the onset of an infectious disease outbreak, can elicit substantial stress responses. Pandemics instigate a sense of uncertainty, enforce a multitude of constraints and modifications, and introduce a considerable array of stress-inducing factors [5].
Psychological resilience denotes an individual‘s ability to manage and adapt to stressful and challenging circumstances. This characteristic is individual, dynamic and contextual, and its development may be influenced by the social environment [6]. Psychological resilience during pregnancy can be seen as a protective factor in coping with stress [7].
The apprehension and distress experienced by pregnant women in the face of epidemics have been extensively examined and reported in research investigations [8]. However, pregnant women‘s post-pandemic fears and their relationship with anxiety, depression, stress and psychological resilience have not been sufficiently analyzed. The aim of this article is to examine pandemic-related fear, depression, stress and anxiety experienced by pregnant women in different trimesters after the pandemic and their relationship with psychological resilience.
Methods
Participant Selection and Procedures
A total of 250 women, including 125 pregnant women and 125 healthy controls, were included in the study. Participants were divided into three groups according to trimester. The 1st trimester group consisted of pregnant women who attended our clinic for a fetal heartbeat examination, had a confirmed positive fetal heartbeat and did not report any complaints such as bleeding, pain or nausea and vomiting. The 2nd trimester group consisted of pregnant women who had a detailed ultrasound scan, underwent screening for genetic disorders and whose test results were normal or no abnormalities were detected. The 3rd trimester group consisted of pregnant women who attended routine antenatal care without complaints of bleeding, pain or premature rupture of membranes. In addition, participants in the 3rd trimester with conditions such as gestational hypertension, gestational diabetes, or fetal growth restriction were excluded. Inclusion criteria included the following:
- participants were at least 18 years old;
- participants‘ native language was Turkish;
- participants were able to give informed consent.
On the other hand, the exclusion criteria were as follows:
- individuals with cognitive impairment or diagnosed mental illness were excluded;
- those who had been hospitalized for psychiatric reasons in the previous 30 days were also excluded;
- individuals with conditions that prevented them from completing the questionnaires were not included in the study.
Participants were given detailed information about the confidentiality of the study and it was emphasized that their personal information and responses would be handled with the utmost care and kept strictly confidential. Participants were clearly informed that they had the right to refuse to complete the questionnaire without giving a reason. The research was conducted in accordance with the tenets of the Declaration of Helsinki, ensuring ethical integrity throughout the study. Prior to their participation, all participants gave informed consent, indicating that they voluntarily agreed to participate in the study.
The study was carried out with the permission of Necmettin Erbakan University Clinical Researches Ethics Committee (Date: 09.09.2022, Decision No: 2022/3963). The study was conducted during a period when pandemic measures were lifted, between 15 September 2022 and 1 March 2023.
Measures
The Depression Anxiety Stress Scale 21 (DASS-21)
The questionnaire used in this study is a self-reported scale commonly used to assess symptoms of depression, anxiety and stress. It consists of a total of 21 items, with each item corresponding to one of three constructs: depression, anxiety and stress. Participants were asked to indicate the extent to which they had experienced certain symptoms in the past week using a 4-point Likert scale. Scores for each subscale (depression, anxiety and stress) are calculated by summing the scores given to the relevant items. High scores on the scale indicate increased levels of depression, anxiety or stress in individuals [9]. The Turkish validity and reliability study of the DASS-21 was conducted by Yilmaz et al. [10].
Epidemic Disease Anxiety Scale (EDAS)
EDAS consists of items that capture different dimensions of pandemic-related anxiety, including fear of contracting the pandemic, concerns about the health and safety of oneself and loved ones, concerns about the social, quarantine and economic consequences of the pandemic, and uncertainty about the future. The Pandemic Anxiety Scale consists of 18 items and four subscales [11].
The Short Psychological Resilience Scale (SPRS)
This scale was first developed by Smith et al. [12] to measure the self-recovery potential and psychological resilience of individuals. A Turkish validity and reliability study was conducted by Doğan et al. [13]. The 5-point Likert-type scale consists of six items. The total score of the scale ranges from 6 to 30, with higher scores indicating more resilience and lower scores indicating less resilience.
Statistics
SPSS version 26 software was used to analyze the data. The Kolmogorov-Smirnov test and histograms were utilized to verify normality. For comparisons of continuous data between two groups, the independent t-test was applied to data with a normal distribution and presented as mean ± SD. The Mann-Whitney U-test was used for non-normally distributed data and expressed as [median (Min.–Max.) ]. An ANOVA Test was carried out to compare three groups of data that fit the normal distribution. Subsequently, a Bonferroni-corrected multiple comparison test (post hoc test) was employed to establish differences between the subgroups. For three-group comparisons that did not fit the normal distribution, a Kruskal-Wallis test was used, followed by the Mann-Whitney U-test with Bonferroni correction to determine differences between subgroups. The study utilized both the Chi-square and Fisher exact tests to compare categorical data, with results being reported as n (%). In addition, Pearson‘s correlation analysis was conducted to examine the correlations between DASS-21, EDAS, and SPRS scores alongside their respective subscale scores. Statistically significant was defined as a P-value below 0.05.
Tab. 1. Demographic and clinical characteristics of pregnant women and healthy controls. // Demografické a klinické charakteristiky těhotných žen a zdravotnických kontrol. 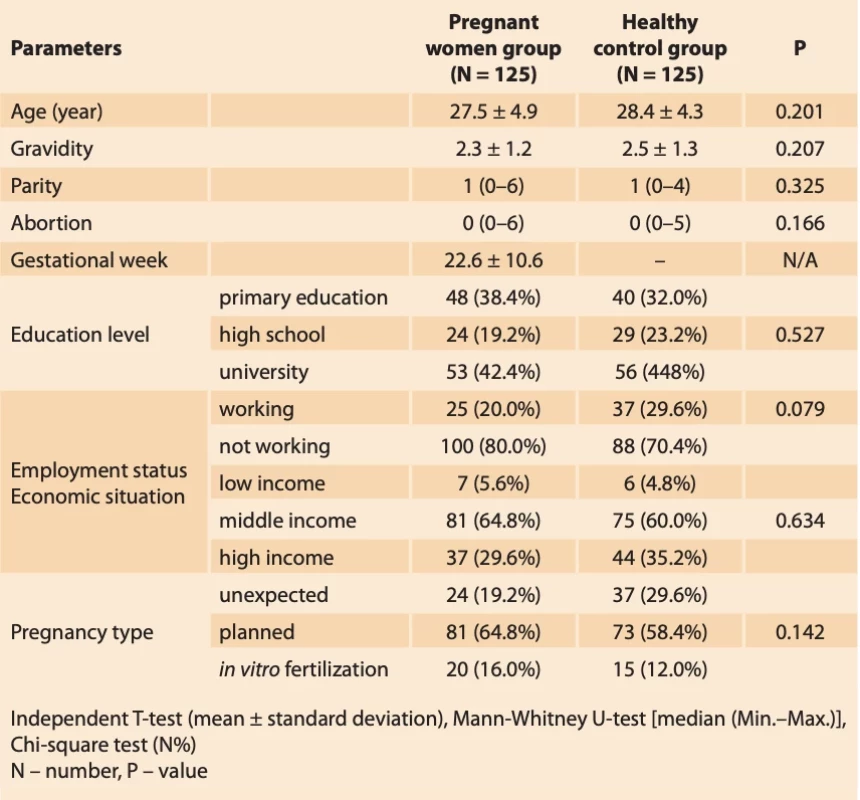
Results
The study involved 250 participants, 125 pregnant women and 125 healthy women. The two groups were similar in terms of age, gravidity, parity, abortion, level of education, employment status, economic status and type of pregnancy. The mean gestational age of the pregnant group was 22.6 ± 10.6 weeks, ranging from 6 to 40 weeks (Tab. 1).
DASS-21 scores were significantly higher in pregnant women compared to the healthy control group. In the subgroups of the scale, depression, anxiety and stress scores were significantly higher in pregnant women (P = 0.001). Positive scores for depression (29% vs. 12.8%; P = 0.032), anxiety (44.0% vs. 31.2%; P = 0.037) and stress (20.0% vs. 9.6%; P = 0.021) corresponded to higher prevalence rates. Regarding EDAS, pregnant women exhibited higher total scores compared to healthy controls (43.3 ± 10.4 vs. 40.3 ± 12.6; P = 0.043). Furthermore, pregnant women had higher epidemic scores (13.9 ± 4.6 vs. 12.4 ± 4.8; P = 0.019). However, no significant difference was observed in economic and quarantine scores. In terms of psychological resilience as measured by the SPRS, pregnant women exhibited slightly higher resilience scores compared to healthy controls but without statistical significance (21.2 ± 3.3 vs. 20.4 ± 3.5; P = 0.073) (Tab. 2).
Tab. 3 compares the socio-demographic characteristics, psychological distress, epidemic anxiety and psychological resilience of pregnant women (N = 125) between trimesters. Age, gravidity, parity and history of abortion did not differ significantly between trimesters. Total DASS-21, anxiety and stress scores were significantly higher in the 1st and 3rd trimesters compared to the 2nd trimester (P = 0.0001, P = 0.001, P = 0.001 respectively). Using the scale cut-off scores, the lowest rate of depression was observed in the 2nd trimester (N = 4; 9.8%), followed by the 1st trimester (N = 11; 26.8%) and the highest rate in the 3rd trimester (N = 14; 32.6%). EDAS did not show a significant difference in terms of total score (P = 0.131), but the epidemic score was higher in the 3rd trimester (P = 0.001). There was a significant difference in SPRS between trimesters (P = 0.006), with the highest endurance in the 2nd trimester.
Tab. 2. Comparison of scale scores between pregnant women and healthy female controls. // Srovnání škálového skóre mezi těhotnými ženami a kontrolami zdravých žen. 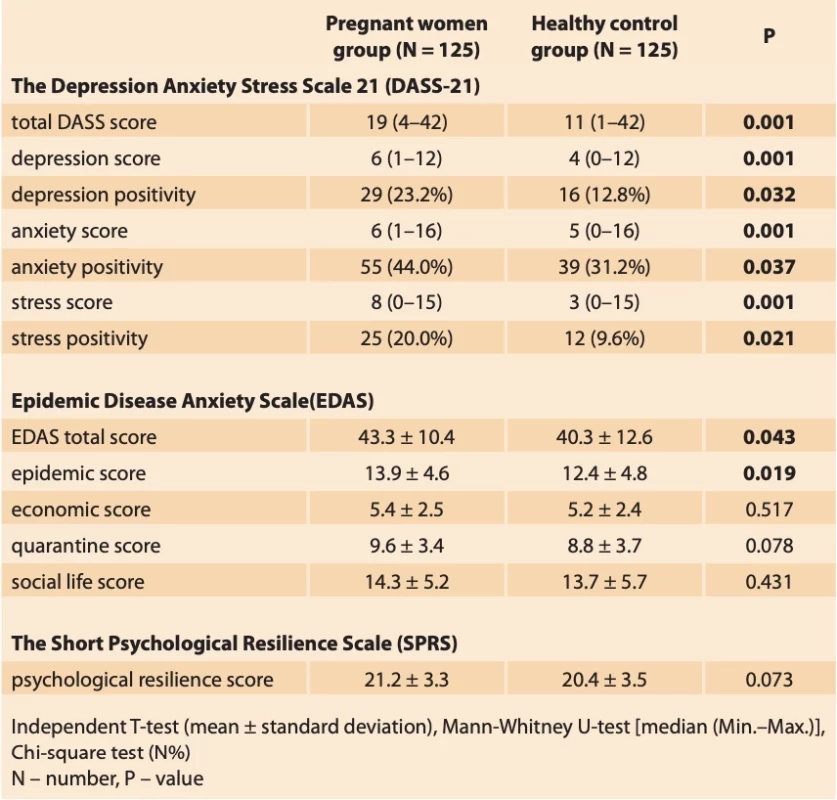
Significant pairwise group comparison results were as follows:
For the DASS-21 total score: 1st trimester vs. 2nd trimester (P = 0.006), 1st trimester vs. 3rd trimester (P = 0.963), and 2nd trimester vs. 3rd trimester (P= 0.001) (post hoc test: One-way ANOVA, Bonferroni correction).
For anxiety score: 1st trimester vs. 2nd trimester (P = 0.006), 1st trimester vs. 3rd trimester (P = 0.416), and 2nd trimester vs. 3rd trimester (P = 0.001) (post hoc test: One-way ANOVA, Bonferroni correction).
For stress score: 1st trimester vs. 2nd trimester (P = 0.001), 1st trimester vs. 3rd trimester (P = 1.00), and 2nd trimester vs. 3rd trimester (P = 0.001) (post hoc test: One-way ANOVA, Bonferroni correction).
For epidemic score: 1st trimester vs. 2nd trimester (P = 1.00), 1st trimester vs. 3rd trimester (P = 0.0001), and 2nd trimester vs. 3rdtrimester (P = 0.001) (post hoc test: One-way ANOVA, Bonferroni correction).
For SPRS score: 1st trimester vs. 2nd trimester (P = 0.032), 1st trimester vs. 3rd trimester (P = 1.00), and 2nd trimester vs. 3rd trimester (P = 0.010) (post hoc test: One-way ANOVA, Bonferroni correction).
The DASS-21 total score was positively and significantly associated with all three subscales of depression (R = 0.816; P = 0.001), anxiety (R = 0.896; P = 0.001) and stress (R = 0.814; P = 0.001). The DASS-21 total score was also positively correlated with the EDAS total score (R = 0.235; P = 0.008) and the pandemic perception subscale (R = 0.390; P = 0.001). The DASS-21 total score was also positively correlated with the economic perception subscale (R = 0.224; P = 0.012). The SPRS total score was negatively correlated with anxiety (R = –0.240; P = 0.007) and stress (R = –0.243; P = 0.006). The SPRS total score was significantly negatively correlated with the DASS-21 total score (R = –0.228; P = 0.011). The EDAS total score was positively and significantly correlated with the epidemic perception subscale (R = 0.669; P = 0.001),economic perception subscale (R = 0.394; P = 0.001), and quarantine subscale (R = 0.700; P = 0.001) (Tab. 4).
Discussion
It has been found that conditions such as depression, anxiety, stress and sleep disorders have increased worldwide after the pandemic. In a meta-analysis examining the prevalence of psychiatric comorbidities during the COVID-19 pandemic, it was reported to be common in different subpopulations (pregnant women, elderly, disabled people, etc.) [14]. In our study, it was found that pregnant women experienced higher depression, anxiety, stress and pandemic anxiety than non-pregnant women in the post-pandemic period. In addition, psychological resilience was found to be negatively associated with depression, anxiety, stress and pandemic anxiety.
There are many studies in the literature showing that the pandemic negatively affects the mental health of pregnant women, increasing depression, anxiety and stress levels [15,16]. Taugeer et al. [17] in a study involving 3411 pregnant women examined the effect of the COVID-19 pandemic on pregnant women and found higher levels of depression, anxiety and stress than in non-pregnant women. In a study conducted during the pandemic period, Songco et al. [18] discovered that women in the perinatal period exhibited higher levels of anxiety and depression. During the COVID-19 period in Turkey, it was discovered through a study conducted on pregnant women that the levels of anxiety and depression were prevalent in 64.5% and 56.3% respectively [19]. In our study, anxiety, depression and stress levels were found to be high in pregnant women in accordance with the literature.
Fear of epidemics was found to be higher in pregnant women than in non-pregnant women [20,21]. The potential correlation between the outcome and significant increase in depression, anxiety, and stress levels of expectant mothers can be attributed to the reduced social support resulting from the pandemic period, challenges in obtaining prenatal health care services, and anxiety about the prospective risks of the disease.
Psychological resilience plays an effective role in coping with stress during pregnancy. Research has revealed that those who possess elevated levels of psychological resilience tend to encounter fewer instances of depression and anxiety [22]. According to research conducted by Killgore et al. [23], it was observed that persons with lower levels of psychological resilience during the pandemic exhibited higher levels of depression and anxiety. Additionally, these individuals had greater challenges in effectively managing the adverse impacts of the pandemic on their mental well-being [24]. In our study, in accordance with the literature, a negative relationship was found between the level of psychological resilience, depression, anxiety and stress in the pregnant group, while no relationship was found with the fear of epidemic disease. This may be related to the decrease in the effect of the pandemic during the period of the study. The fear of epidemic disease may have decreased with the reduction of protective measures after the pandemic, increased social interaction, and brought a closer understanding of the prognosis of pregnant women with COVID-19.
Anxiety level during pregnancy may differ between trimesters [25]. Saadati et al. [26] did a study including a sample of 300 pregnant women, whereby it was shown that levels of anxiety and depression were comparatively elevated during the 3rd trimester in relation to the preceding trimesters. In our country, Karatayli et al. [27] found similar results in their study. In our study, anxiety, depression and stress levels were found to be high in the 1st and 3rd trimesters. The heightened levels during the 1st trimester can be attributed to the process of adjusting to the pregnancy, while the increased levels during the 3rd trimester could be due to impending childbirth, care of the newborn, and adaptation to a new lifestyle.
Tab. 3. Comparison of sociodemographic characteristics, psychological distress, epidemic anxiety and psychological resilience in pregnant women be- tween trimesters. // Srovnání sociodemografických charakteristik, psychické tísně, epidemické úzkosti a psychické odolnosti u těhotných žen mezi trimestry. 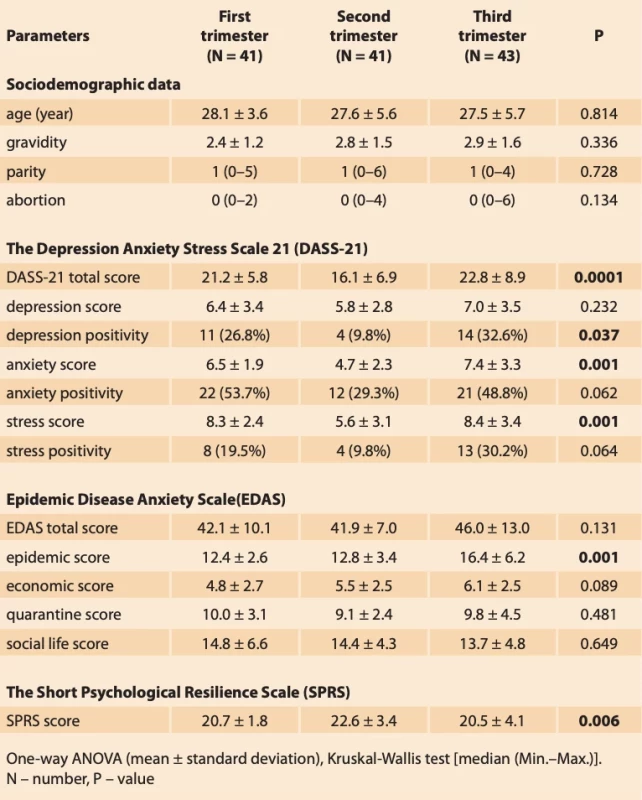
Tab. 4. Correlation matrix of psychological scales (DASS-21, EDAS and SPRS) in pregnant women after the pandemic. // Korelační matice psychologických škál (DASS-21, EDAS a SPRS) u těhotných žen po pandemii. 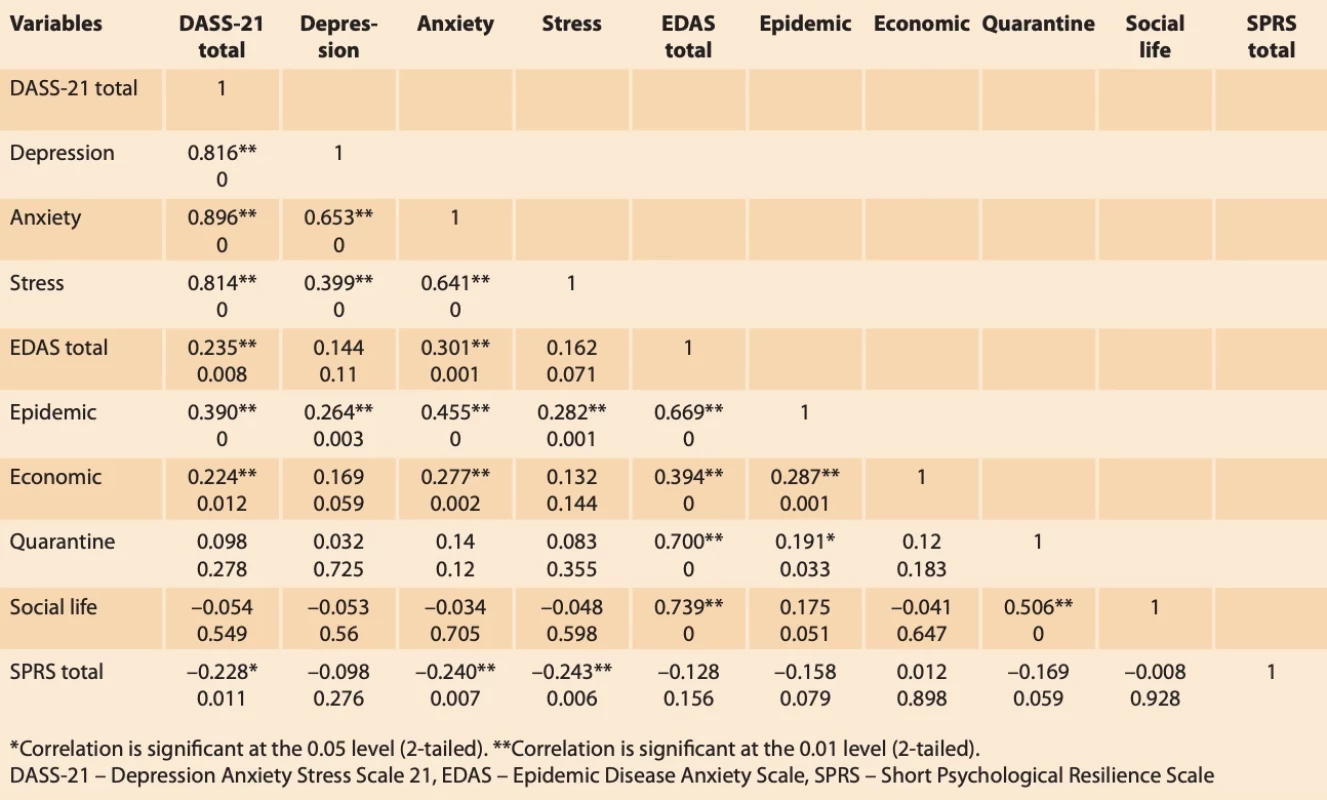
Our study had some limitations. Firstly, being a cross-sectional study, it is not possible to monitor psychological changes in the same pregnant women in all trimesters. Secondly, the sample size was partially insufficient. In addition, psychological assessment of pregnant women was based only on self-report scales.
Conclusion
In our study, it was found that pregnant women experienced higher levels of depression, anxiety, stress and pandemic anxiety than non-pregnant women in the post-pandemic period, and psychological resilience was negatively associated with depression, anxiety and stress. These findings indicate that the pandemic negatively affects the mental health of pregnant women and the importance of providing psychological support services to protect the mental health of pregnant women.
Submitted/Doručeno: 23. 9. 2023
Accepted/Přijato: 25. 9. 2023Fatih Akkuş, MD
Division of Perinatology
Faculty of Medicine
Necmettin Erbakan University
Hocacihan Mah. Abdulhamid Han Cad. No: 3
42080 Selçuklu/Konya
Turkey
fakkus1987@gmail.com
Zdroje
1. Zhang SX, Arroyo Marioli F, Gao R et al. A second wave? What do people mean by COVID waves? A working definition of epidemic waves. Risk Manag Healthc Policy 2021; 14 : 3775–3782. doi: 10.2147/RMHP.S326051.
2. Türk A, Bingül BA, Ak R. The economic and social impacts of pandemics in history. Gaziantep Univ J Soc Sci 2020; 19 (COVID-19 Special Issue): 612–632. doi: 10.21547/jss.766717.
3. Lin YH. The spread of the epidemic among vulnerable groups and related epidemic prevention issues. Hu Li Za Zhi 2022; 69 (6): 4–5. doi: 10.6224/jn.202212_69 (6).01.
4. Chung E, Leinwand LA. Pregnancy as a cardiac stress model. Cardiovasc Res 2014; 101 (4): 561–570. doi: 10.1093/cvr/cvu013.
5. Preis H, Mahaffey B, Heiselman C et al. Pandemic-related pregnancy stress and anxiety among women pregnant during the coronavirus disease 2019 pandemic. Am J Obstet Gynecol MFM 2020; 2 (3): 100155. doi: 10.1016/j.ajogmf.2020.100155.
6. Ozdemir C, Akbas Gunes N. The effect of diet and regular exercise on psychological resilience in obese or overweight women. Int J Clin Pract 2021; 75 (8): e14320. doi: 10.1111/ijcp.14320.
7. Alves AC, Souza RT, Mayrink J et al. Measuring resilience and stress during pregnancy and its relation to vulnerability and pregnancy outcomes in a nulliparous cohort study. BMC Pregnancy Childbirth 2023; 23 (1): 396. doi: 10.1186/s12884-023-05692-5.
8. Wu Y, Zhang C, Liu H et al. Perinatal depressive and anxiety symptoms of pregnant women during the coronavirus disease 2019 outbreak in China. Am J Obstet Gynecol 2020; 223 (2): 240.e1–240.e9. doi: 10.1016/j.ajog.2020.05. 009.
9. Lovibond SH, Lovibond PF. Manual for the depression anxiety stress scales. Sydney: Psychology Foundation of Australia 1995.
10. Yilmaz Ö, Boz H, Arslan A. The validity and reliability of depression stress and anxiety scale (DASS21) Turkish short form. Finans Ekonomi ve Sosyal Araştırmalar Dergisi 2017; 2 (2): 78–91.
11. Hizli G, Ünübol H, Tutgun-Ünal A et al. Epidemic anxiety scale: validity and reliability study. Psikiyatride Güncel Yaklaşımlar 2020; 12 (Suppl 1): 382–397. doi: 10.18863/pgy.808280.
12. Smith BW, Dalen J, Wiggins K et al. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med 2008; 15 (3): 194–200. doi: 10.1080/10705500802222972.
13. Doğan T. Adaptation of the brief resilience scale into Turkish: a validity and reliability study. J Happiness Well-Being 2015; 3 (1): 93–102.
14. Zhao YJ, Jin Y, Rao WW et al. The prevalence of psychiatric comorbidities during the SARS and COVID-19 epidemics: a systematic review and meta-analysis of observational studies. J Affect Disord 2021; 287 : 145–157. doi: 10.1016/ j.jad.2021.03.016.
15. Bermúdez-González M, Álvarez-Silvares E, Santa-María-Ortiz JK et al. Impact of the COVID-19 pandemic on maternal anxiety during pregnancy: a prevalence study. Clin Invest Ginecol Obstet 2022; 49 (4): 100776. doi: 10.1016/j.gine.2022.100776.
16. Tomfohr-Madsen LM, Racine N, Giesbrecht GF et al. Depression and anxiety in pregnancy during COVID-19: a rapid review and meta-analysis. Psychiatry Res 2021; 300 : 113912. doi: 10.1016/j.psychres.2021.113912.
17. Tauqeer F, Ceulemans M, Gerbier E et al. Mental health of pregnant and postpartum women during the third wave of the COVID-19 pandemic: a European cross-sectional study. BMJ Open 2023; 13 (1): e063391. doi: 10.1136/ bmjopen-2022-063391.
18. Songco A, Minihan S, Fox E et al. Social and cognitive vulnerability to COVID-19-related stress in pregnancy: a case-matched-control study of antenatal mental health. J Affect Disord 2023; 325 : 739–746. doi: 10.1016/ j.jad.2023.01.053.
19. Kahyaoglu Sut H, Kucukkaya B. Anxiety, depression, and related factors in pregnant women during the COVID-19 pandemic in Turkey: a web-based cross-sectional study. Perspect Psychiatr Care 2021; 57 (2): 860–868. doi: 10.1111/ppc.12627.
20. Naghizadeh S, Mirghafourvand M. Relationship of fear of COVID-19 and pregnancy-related quality of life during the COVID-19 pandemic. Arch Psychiatr Nurs 2021; 35 (4): 364–368. doi: 10.1016/j.apnu.2021.05.006.
21. Lok KY, Ko RW, Fan HS et al. International survey on fear and childbirth experience in pregnancy and the postpartum period during the COVID-19 pandemic: study protocol. BMJ Open 2021; 11 (8): e050132. doi: 10.1136/ bmjopen-2021-050132.
22. Liu J, Yan X, Chu L et al. Mediating role of mental resilience between sleep quality and mindfulness level of pregnant women screened by prenatal diagnosis. J Healthc Eng 2022; 2022 : 7011836. doi: 10.1155/2022/7011 836.
23. Killgore WD, Taylor EC, Cloonan SA et al. Psychological resilience during the COVID-19 lockdown. Psychiatry Res 2020; 291 : 113216. doi: 10.1016/j.psychres.2020.113216.
24. Verdolini N, Amoretti S, Montejo L et al. Resilience and mental health during the COVID-19 pandemic. J Affect Disord 2021; 283 : 156–164. doi: 10.1016/j.jad.2021.01.055.
25. Priyambada K, Pattojoshi A, Bakhla AK. A study of antenatal anxiety: comparison across trimesters. Int J Reprod Contracept Obstet Gynecol 2017; 6 (5): 1810–1814.
26. Saadati N, Afshari P, Boostani H et al. Health anxiety of pregnant women and its related factors during the pandemic of Corona virus. Research Gater 2020. doi: 10.21203/rs.3.rs-268 40/v1.
27. Karataylı S, Gezginç K, Ilgaz F et al. The comparison of depression anxiety and quality of life levels among trimesters of pregnancy. Gynecol Obstet Reprod Med 2010; 16 (2): 79–83.
Štítky
Detská gynekológia Gynekológia a pôrodníctvo Reprodukčná medicína
Článok vyšiel v časopiseČeská gynekologie
Najčítanejšie tento týždeň
2024 Číslo 1- Ne každé mimoděložní těhotenství musí končit salpingektomií
- I „pouhé“ doporučení znamená velkou pomoc. Nasměrujte své pacienty pod křídla Dobrých andělů
- Mýty a fakta ohledně doporučení v těhotenství
- Gynekologické potíže pomáhá účinně zvládat benzydamin
-
Všetky články tohto čísla
- Předoperační a pooperační staging u karcinomu endometria – prospektivní studie
- Význam vaginální tamponády po laparoskopické sakrokolpopexi – retrospektivní studie
- Diskrepance stagingové a peroperační klasifikace endometriózy pánve dle #Enzian 2021
- Pandemic fear and psychological resilience in pregnant women after the pandemic – a study in Turkey
- Occurrence of acute retrobulbar hemorrhage during birth
- Occult invasive cervical cancer, FIGO stage III, with a negative Pap smear test – clinical presentation and brief review of the literature
- Primary perineal endometriosis – a case report and literature review
- Faktory zvyšující riziko malignity při nálezu endometriálního polypu v ultrazvukovém obraze
- Ženský orgazmus, reprodukce a párové vztahy
- Uterovesical fistula and its treatment in Sub-Saharan Africa
- Pôrodný plán – jeho právne a medicínske implikácie
- Nová doporučení k informování pacientů a dárců gamet v asistované reprodukci
- Diagnostika a léčba endometriózy
- Česká gynekologie
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Faktory zvyšující riziko malignity při nálezu endometriálního polypu v ultrazvukovém obraze
- Diagnostika a léčba endometriózy
- Význam vaginální tamponády po laparoskopické sakrokolpopexi – retrospektivní studie
- Ženský orgazmus, reprodukce a párové vztahy
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



