-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Biliopancreatic endoscopy
prof. Marco Bruno – Gastro Update Europe 2019, Budapest
Authors: Tytgat G.
Authors place of work: Department Gastroenterology and Hepatology, Academic Medical Center, Amsterdam, The Netherlands
Published in the journal: Gastroent Hepatol 2020; 74(2): 171-173
Category: Congress review
Developments in endoscopic ultrasound (EUS), biliopancreatic endoscopy and endoscopic complications were discussed. Microbial contamination of endoscopic equipment remains a major (unsolvable?) problem for the endoscopist. Over the past 17 years (y), 32 documented duodenoscope-related outbreaks with multi-drug resistant microorganisms, involving over 400 patients and leading to death in over 20 patients, have been reported. Endoscopic contamination and patient infection have also occurred without breaches in the re-processing procedures. Scope contamination after a procedure is approx. 8 – 10 log10; manual cleaning leads to a reduction with approx. 4 – 6 log10 and further automated high level disinfection to another approx. 4 – 6 log10 reduction. The total reduction amounts to approx. 8 – 12 log10 leading to a low margin of safety of approx. 0 – 2 log10. Sratches and shredding in bending sections and remaning adherent debris interfere with the cleaning/ disinfection efficacy. These results were again confirmed in a nation-wide duodenoscope culture study, showing that 22% of the duodenoscopes were contaminated with one or more microorganisms with 20 or more colony forming units and that 39% of the endoscopic retrograde cholangiopancreatography (ERCP) centers had at least one contaminated duodenoscope hanging in the dryer cabinet. Contamination was not confined to a specific duodenoscope type but appeared related to the complex scope design and the inability to sufficiently clean all its intricate surfaces. A recent American Food and Drug Administration safety communication reads: „For high concern organisms, defined as organisms that are more often associated with disease, such as Escherichia coli and Pseudomonas aeruginosa, updated culturing results appear to show that up to 5.4% of properly collected samples test positive. Combined with strict adherence to the duodenoscope manufacturer’s reprocessing instructions, the following supplemental measures may further help reduce the risk of infection transmission associated with the use of duodenoscopes: microbiological culturing; ethylene oxide sterilisation; use of a liquid chemical sterilant processing system; repeat high-level disinfection“. Perhaps the last recommendation is the most sensible and realistic or shall we be using only disposable (duodeno)endoscopes in the not-to-distant future?
In a previous large scale Dutch controlled trial, a minimally invasive step-up approach was shown to be superior at a follow-up of 6 months (m), to primary open surgical necrosectomy in patients with (infected) necrotizing pancreatitis. The endpoint (mortality/ major complications) was respectively 40 vs. 69%. Recently, the late outcome after approx. 86 m was superior for the step-up approach with significantly less new-onset multi-organ failure/ systemic complications, incisional hertnia and need for pancreatic enzyme therapy.
Lumen-apposing metal stents are increasingly being used in the drainage of pancreatic walled-off necrosis instead of plastic pig-tail stents. A recent meta-analysis showed a comparable overall clinical success rate of 88% with both modalities. Also the difference in pooled adverse event rates of resp. 11 vs. 16% was not significant, leaving the choice to the endoscopist’s preference. The overall similar outcomes between expandable metal vs. pig-tail plastic was again shown in a British study with comparable technical and clinical success (above 90%), stent duration of an average 55 days and recurrence rates of around 5 – 6%. What was different was the higher rate of bleeding, 15 vs. 3%, with about half the bleeding in the metal stent cohort related to the development of a pseudo-aneurysm, necessitating vascular embolization. Other publications have drawn attention to this dreadful aneurysmal complication, caused by excessive pressure trauma of vessels in the wall of the necrotic cavity by the expandable metal stents. Patients should be prewarned of such potential complications.
Quite revolutionary is the rapidly spreading experience with EUS-guided gastrointestinal connections mainly for palliation of malignant obstruction. In one such study, EUS-guided choledochoduodenostomy was carried out in 46 patients with inoperable malignant distal bile duct obstruction. Technical and clinical success was respectively 93 and 98%. Adverse events occurred in 12% (stent food impaction, delayed bleeding and stent migration). Reaching the papilla for ERCP can be challenging, for example after gastric bypass surgery with Roux-en-Y anastomosis for therapy of morbid obesity. Reaching the papilla may be attempted with a balloon-fitted endoscope. Alternatively, the gastric pouch may be reconnected transmurally under EUS guidance. In a multicenter study, EUS-guided gastrogastrostomy was compared with endoscopy in 60 patients. Technical success by reaching the papilla was seen in 100 vs. 60% with a procedure duration of 50 min vs. 91 min, both in favor of the EUS-guided approach. Adverse effects were comparable with 10 and 7%. Several comparable studies, evaluating the efficacy of the EUS-guided transintestinal approach have been published, all indicating comparable technical and clinical success rates and comparable and sometimes even lower complication rates when compared to other modalities, such as percuteous transhepatic approches etc.
Also intriguing is the exploration of the usefulness of cholangioscopy now that the digital single-operator cholangioscope has become available. This technology was evaluated in a multicenter study with over 400 patients with difficult biliary stones, defined as: > 15 mm; > 3; intrahepatic/ cystic duct; and/ or – impacted or – associated with anatomic duct abnormality. Complete bile duct clearance, either with electrohydrolic or laser lithotripsy was obtained in 97%, in 1 session in 77%. ERCP’s for additional therapy such as stent removal or stricture treatment was necessary in 34%. The most important factor associated with technical failure was difficult anatomy or difficult cannulation. More than one session was more often necessary in patients with prior failed ERCP or in case of a prolonged initial cholangioscopy session. Current guidelines suggest cholangioscopy-guided lithotripsy as an adjunct with or without balloon dilation or mechanical lithotipsy. Novel is the evaluation of direct cholangioscopy guided laser lithotripsy. Endoscopic stone clearance was obtained in respectively 93 and 67% of the 60 patients. Dilation of the papilla was more often carried out in the conventional group and the procedure duration was substantially longer in the cholangioscopy group. The conventional approach was less successful in patients with prior ERCP attempt. The usefulness of cholangioscopy was also demonstrated for biopsy targeting of suspicious lesions, yet distinguishing between benign and malignant bile duct stricturing lesions often remains challenging. Whole exome and genome sequencing studies have defined the genetic landscape of neoplasms arising or secondarily involving the bile duct system. A 28-gene next-generation-sequencing panel (BiliSeq) was prospectively evaluated in 346 ERCP-obtained biliary specimens from 252 patients with bile duct strictures. The sensitivity and specificity of BiliSeq for malignant strictures was respectively 73 and 100%. In comparison, the sensitivity of elevated serum CA19-9 was 76% and of pathological evaluation 48%. The combination of BiliSeq and pathological evaluation increased the sensitivity to 83% and maintained a specificity of 99%. BiliSeq improved the pathological sensitivity for both biliary brushings and biopsies. Among patients with primary sclerosing cholangitis, BiliSeq had a sensitivity of 83% compared to 8% or pathological examination. Interestingly, in 8% the genomic alterations were useful in guiding therapy such as trastuzumab-based treatment for ERBB2-amplified cholangiocarcinoma. Beyond doubt, increasingly molecular-based investigations will be incorporated in diagnostic/ therapeutic endoscopy.
The explosive interest in pancreatic cysts has continued during the past year. The overall subtyping of cystic lesion is illustrated in the fig. 1.
Fig. 1. Pancreatic cysts. What are we looking for? 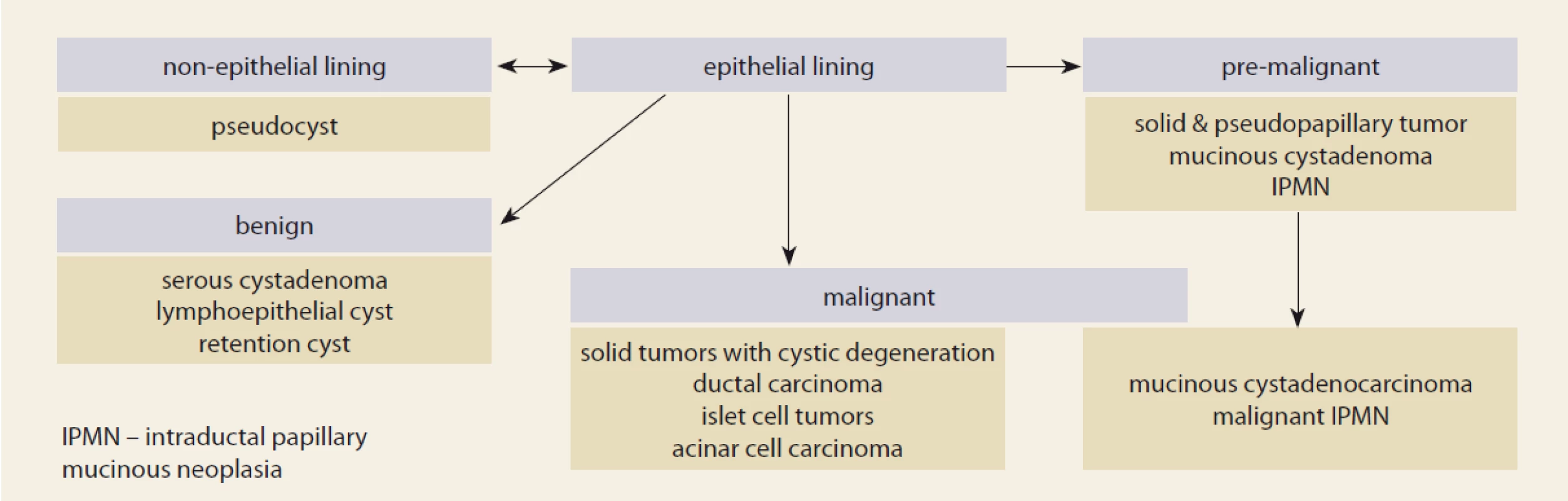
Fine needle aspiration cytology was the standard technology when trying to characterize the nature of the cystic lesion but attention is increasingly switching to the use of newly designed catheter-guided biopsy needles. Novel is the development of catheter-guided microbiopsy forceps for targeted biopsy of the cystic wall. In 28 patients the micro-biopsy procedure was technically successful in 86%. Biopsies were generally of good quality and contributed to the diagnosis in over 70%. Adverse events occurred in 11%, usually mild pancreatitis. Such results were confirmed in another cohort of 56 patients where the procedure was technically successful in all. Mild adverse events were seen in 16%, most commonly intracystic bleeding. Specimens were considered adequate for histology in 84%, leading to an overall diagnostic accuracy, combining histology and cytology of 84%. What the proper and cost-effective indications will be for use of micro-biopsy forceps equipment needs further larger scale detailed multicenter evaluation.
The Gastro Update Europe 2020 will be held on September 4–5, 2020 in Bratislava, Slovakia. For more information visit www.gastro-update-europe.eu.
Prof. Guido Tytgat, MD, PhD
Department of Gastroenterology andHepatology
Academic Medical Center
Meibergdreef 9
1105 AZ Amsterdam
The Netherlands
Štítky
Detská gastroenterológia Gastroenterológia a hepatológia Chirurgia všeobecná
Článok vyšiel v časopiseGastroenterologie a hepatologie
Najčítanejšie tento týždeň
2020 Číslo 2- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Kombinace metamizol/paracetamol v léčbě pooperační bolesti u zákroků v rámci jednodenní chirurgie
- Antidepresivní efekt kombinovaného analgetika tramadolu s paracetamolem
- Parazitičtí červi v terapii Crohnovy choroby a dalších zánětlivých autoimunitních onemocnění
- Srovnání analgetické účinnosti metamizolu s ibuprofenem po extrakci třetí stoličky
-
Všetky články tohto čísla
- Covid-19 a játra
- Editorial
- Doporučený postup České hepatologické společnosti ČLS JEP pro diagnostiku a léčbu nealkoholové tukové choroby jater
- Infection in patients hospitalised with advanced chronic liver disease (cirrhosis) – single-centre experience
- De novo non-alcoholic fatty liver disease after liver transplantation – as diagnosed by magnetic resonance
- Doporučení pro léčbu idiopatických střevních zánětů v době pandemie covid-19
- Odporúčania slovenskej Pracovnej skupiny pre IBD pri SGS pre liečbu biosimilárnymi anti-TNF biologikami u dospelých a detských pacientov
- Endoskopická drenáž infikované ohraničené pankreatické nekrózy s komplikovaným průběhem – kazuistika
- Čtyřleté zkušenosti s monitorováním farmakokinetiky infliximabu a adalimumabu u pacientů s idiopatickými střevními záněty
- Vedolizumab v léčbě Crohnovy choroby ve světle nových poznatků
- Laserová litotripse zaklíněného biliárního konkrementu v tlustém střevě
- Anderson-Fabryho choroba a postižení gastrointestinálního traktu
- Gastroenterologie a gastrointestinální endoskopie v podmínkách pandemie viru SARS-CoV-2
- Devadesátiny doc. MU Dr. Miloše Sedláčkové, CSc.
- Životní jubileum As. MU Dr. Hany Dvořákové, CSc.
- Komentář k článku: Caha M, Politová P, Vlk R et al. Překvapivá příčina úmrtí pacienta s krvácením do horního trávicího traktu. Gastroent Hepatol 2020; 74(1): 50–53. doi: 10.14735/ amgh202050.
-
Novel Pancreatic Developmentsprof. Peter Layer – Gastro Update Europe 2019, Budapest
Nové poznatky o pankreatu -
Biliopancreatic endoscopy
prof. Marco Bruno – Gastro Update Europe 2019, Budapest - Novel Developments In Intestinal Endoscopy<br> prof. Oliver Pech – Gastro Update Europe 2019, Budapest
- Výběr z mezinárodních časopisů
- Kreditovaný autodidaktický test
- Gastroenterologie a hepatologie
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Covid-19 a játra
- Endoskopická drenáž infikované ohraničené pankreatické nekrózy s komplikovaným průběhem – kazuistika
- Doporučený postup České hepatologické společnosti ČLS JEP pro diagnostiku a léčbu nealkoholové tukové choroby jater
- Doporučení pro léčbu idiopatických střevních zánětů v době pandemie covid-19
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



