-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Sarkoidosis and its Eye Ocular Manifestation (an Analysis of Six Case Report)
Authors: P. Sokačová 1; J. Krásný 1; J. Kozák 2; A. Srp 3; J. Šach 4; J. Tomášová Borovanská 1; V. Votava 5
Authors place of work: Oční klinika FN Královské, Vinohrady, Praha, přednosta prof. MUDr. P. Kuchynka, CSc. 1; Stomatochirurgická klinika FN Motol, Praha, přednosta doc. MUDr. J. Kozák, CSc. 2; Radiodiagnostická klinika FN Královské Vinohrady, Praha, přednosta doc. MUDr. V. Janík CSc. 3; Ústav patologie FN Královské Vinohrady a 3. LF UK, Praha, přednosta doc. MUDr. T. Jirásek, Ph. D. 4; Klinika tuberkulózy a respiračních nemocí VFN, Praha, přednosta prof. MUDr. J. Homolka, DrSc. 5
Published in the journal: Čes. a slov. Oftal., 73, 2017, No. 5-6, p. 189-197
Category: Původní práce
Summary
Aim:
To introduce the range of eye changes in sarcoidosis in the individual casuistics.Materials:
At the Ophthalmic Clinic of Teaching Hospital Královské Vinohrady in Prague were examined and treated six patients with ocular forms of sarcoidosis in the years from 1998 to 2015. Three patients were unilateral lesions of the lacrimal gland without systemic symptoms. One patient experienced orbital inflammatory syndrome that accompanied the hilar form of pulmonar sarcoidosis. Two other patients underwent intraocular inflammation, panuveitis / iridocyclitis and bilateral intermedial uveitis. Both of these patients also had systemic affections of mediastinal lymph nodes and lung, in the first of these, signs of neurosarcoidosis first appeared.Results:
In the treatment of lacrimal glands, the diagnosis was determined by histological examination of the removed lacrimal gland in external orbitotomies, also, the orbital process has been verified by biopsy and the subsequent comprehensive examination revealed the systemic process. Definitive diagnosis of sarcoidosis was established bioptically in both uveitides and has also been demonstrated in imaging methodologies including galli scintigraphy. All patients were successfully treated with corticosteroid therapy.Conclusion:
Biopsy results have always been a surprise in orbital processes. Both cases of uveitis were associated with systemic involvement and initiated comprehensive investigation which showed the need for interdisciplinary collaboration in the diagnosis and treatment of sarcoidosis.Key words:
sarkoidosis, biopsy, corticosteroids, gallii scintigraphy, MRI, uveitisINTRODUCTION
Sarcoidosis is a chronic multisystemic granulomatous disorder of unclear etiology, characterised by the occurrence of non-caseifying granulomas. From an immunological perspective it is possible to speak of an abnormal immune reaction to an unknown noxious substance of an antigenic nature. It concerns a chronic inflammatory pathology, in which the target of the inflammatory reaction is individual organs. Activation of macrophages and T-lymphocytes occurs, followed by the production of inflammation mediators. The clinical manifestations of sarcoidosis are very diverse. According to the localisation of the affliction, they are divided into the form of pulmonary and extrapulmonary, the latter of which include ocular manifestations, namely orbital, conjunctival and uveal, as well as affliction of the optic nerve. The course of sarcoidosis is acute (subacute) and chronic. The extent of the manifestations may be asymptomatic, oligosymptomatic and generalised. The development of the pathology is not always the same, possibilities include healing ad integrum, healing with a defect which may progress, or transition to clinical latency with detectable organ lesions, although functionally the condition is normalised. At present opinions on the etiology of sarcoidosis are fairly divergent. On the one hand the significance of predisposition is assessed, and on the other there is a search for a hypothetical triggering agent. To date no theory of the etiopathogenesis has been reliably demonstrated, and the possibility that a number of factors share in the origin of this pathology has not been excluded.
Sarcoidosis therefore remains the focus of interest of scientific research worldwide, with the aim of improving the capacities of targeted diagnosis and treatment. This is attested to by numerous publications over the course of recent years. In 2016 it was possible to find approximately 750 citations in PUBMED, of which two were multi-disciplinary communications by Czech authors. Since the 1950s, 7 articles with a total of 10 observations have been published to date in Czechoslovak and later Czech and Slovak ophthalmology. On the basis of the attestation study we have decided to present a complex view of this issue with an overview of the literature, and point to the necessity of inter-disciplinary co-operation.
Diagnosis of sarcoidosis
In order to confirm a diagnosis of sarcoidosis it is necessary to conduct a comprehensive examination. Due to the diversity of the pathology, diagnosis is generally difficult, as attested to below by our cohort. Methods are presented which are of fundamental significance for diagnosis, or belong among traditional examinations.
In laboratory examination it is possible to detect non-specific changes in the blood count, e.g. normochromic and normocytic anaemia, leukopenia, lymphopenia, monocytosis and eosinophilia. Sedimentation is increased in approximately 30% of patients, in addition to which there may be pathological liver tests, primarily alkaline phosphatase. Presence of hypercalcaemia above 2.6 mmol/l and hypercalciuria above 7.5 mmol/24 hours loses diagnostic and prognostic significance. Immunological examination with the aid of specific blood tests also so far only supplements the clinical information. A separate examination is of angiotensin converting enzyme I (ACE), which is an enzyme produced primarily by the endothelia of pulmonary capillaries and circulating monocytes. However, because the monocyte macrophage system is activated upon sarcoidosis, there is an increased formation of ACE, which can be detected in the bronchoalveolar fluid and in serum. A disadvantage is lower sensitivity (30 to 60%), as a result of which negativity of ACE in sarcoidosis is not excluded.
Due to the pulmonary form of sarcoidosis, imaging methods rank among the fundamental diagnostic methods. Skiagram of the chest is acknowledged as the standard examination thanks to its simplicity and universality. The changes are highly characteristic of sarcoidosis: stage I is characterised by bilateral hilar lymphadenopathy, and with concurrent affliction of the pulmonary parenchyma this concerns stage II. Parenchymal pulmonary affliction with reticulonodulation, without signs of lymphadenopathy, represents stage III, and upon the appearance of fibrotic changes this concerns stage IV. Galli scintigraphy (isotope of gallium 67 is non-specifically uptaken by activated macrophages, cancer and reticular cells). The only specific finding for sarcoidosis (90% of patients) is the “lambda panda” image. On scintigraphy, symmetrical activity is demonstrated in the lachrymal and salivary glands, and in the nasal mucosa – the head of the patient resembles a panda. At the same time, the displayed bilateral lymphadenopathy resembles the Greek letter lambda. High resolution computer tomography (HRCT) ranks among the basic methods suitable for the diagnosis and monitoring of sarcoidosis. Magnetic resonance (MR) is used in sarcoidosis primarily in the diagnosis and monitoring of neurosarcoidosis, where it very precisely displays intraparenchymatous and meningeal changes of the CNS (central nervous system). It is also of fundamental significance for the diagnosis of orbital processes from the perspective of the topographic finding for assignment of a biopsy.
Other examination methods include bronchoscopy, which in differential diagnostics may on one hand exclude other pathologies of the bronchi, and then above all serve for confirmation of the diagnosis with the aid of a pulmonary biopsy. It is most often supplemented by a bronchoalveolar lavage (BAL), in which the aspirated bronchoalveolar fluid is examined cytologically (lymphocytic alveolitis has a non-specific increase in the absolute number of inflammatory cells in 90%), and immunological tests are also conducted.
Diagnosis of ocular form of sarcoidosis (more precisely intraocular inflammations) rests upon a conclusion of the “1st International Workshop on Ocular Sarcoidosis” from 2006. If the result of the biopsy is not positive, a combination of diagnostic criteria and examinations is used, see below.
Own cohort
During the period of 1998 to 2015, a total of six patients with manifestations of orbital and intraocular sarcoidosis were observed and treated at the Department of Ophthalmology at the Královské Vinohrady University Hospital. With regard to the different localisation and form, patients are classified into four diagnostic observations, as they progressively reported to the centre with their symptoms.
Observation of an inflammatory pseudotumour of the lachrymal gland without general manifestations of sarcoidosis
In April 1998 a 43 year old woman (case report no. 1) and in May a 45 year old man (case report no. 2) were examined. The last patient who reported to us in 2007 with similar complaints was a 61 year old woman (case report no. 3).
The patients stated long-term lachrymation of the eye with irregular swelling of the upper eyelid, which gradually progressed over the course of two to three months and became a permanent symptom, only in the oldest patient the onset of the problem was more acute, over the course of six weeks. These complaints were accompanied by a feeling of pressure behind the eyeball. The patients did not state disorders of motility of eyes in the sense of double vision. The orbital finding before and after surgery is presented in fig. 1 (only in the last patient this concerns an image 2 weeks after a histological verification excluding lymphoma, in which protrusion and depression of the bulb still persisted, confirmation of sarcoidosis was subsequent). The clinical symptoms and set of examinations are summarised in table 1. According to the finding on MR of the orbit (and CNS) it was not possible to exclude an isolated malignant process in the sense of alveolar carcinoma with the possibility of lymphoma in the region of the lachrymal gland. For this reason it was decided to embark upon surgical intervention, with the aim of removing the lachrymal gland in its entirety. An external osteoplastic orbitotomy of the sec. Krönlain was conducted in co-operation with the Department of Stomatosurgery at Motol University Hospital at the latest two months after the initial examination. The histological verification demonstrated a bordered granulomatous non-caseifying inflammation of the lachrymal gland, with multinuclear cells. The histological image was always evaluated as sarcoidosis. For this reason, the examination was supplemented with ACE and liver tests, the skiagram of the chest was re-assessed, and galli scinitigraphy of the lungs was performed. The neurological examination did not detect affliction of the cranial nerves or other symptoms. The complex examination therefore did not demonstrate manifest clinical systemic form of sarcoidosis. However, pneumologists recommended general immunosuppressant therapy with corticoids. Medrol was administered in a dose of 1 mg/kg/day for a period of 14 days, with gradual discontinuation over the course of three months. The clinical orbital picture after surgery and subsequent therapy was normalised, only in the 61 year old patient a mild depression persisted due to more difficult healing with regard to age. At repeated six-monthly follow-up examinations neither relapse nor further symptoms of systemic sarcoidosis appeared, and after three years further observation was discontinued.
Tab. 1. Clinical-diagnostic findings in patients with inflammatory pseudotumour of the lachrymal gland. 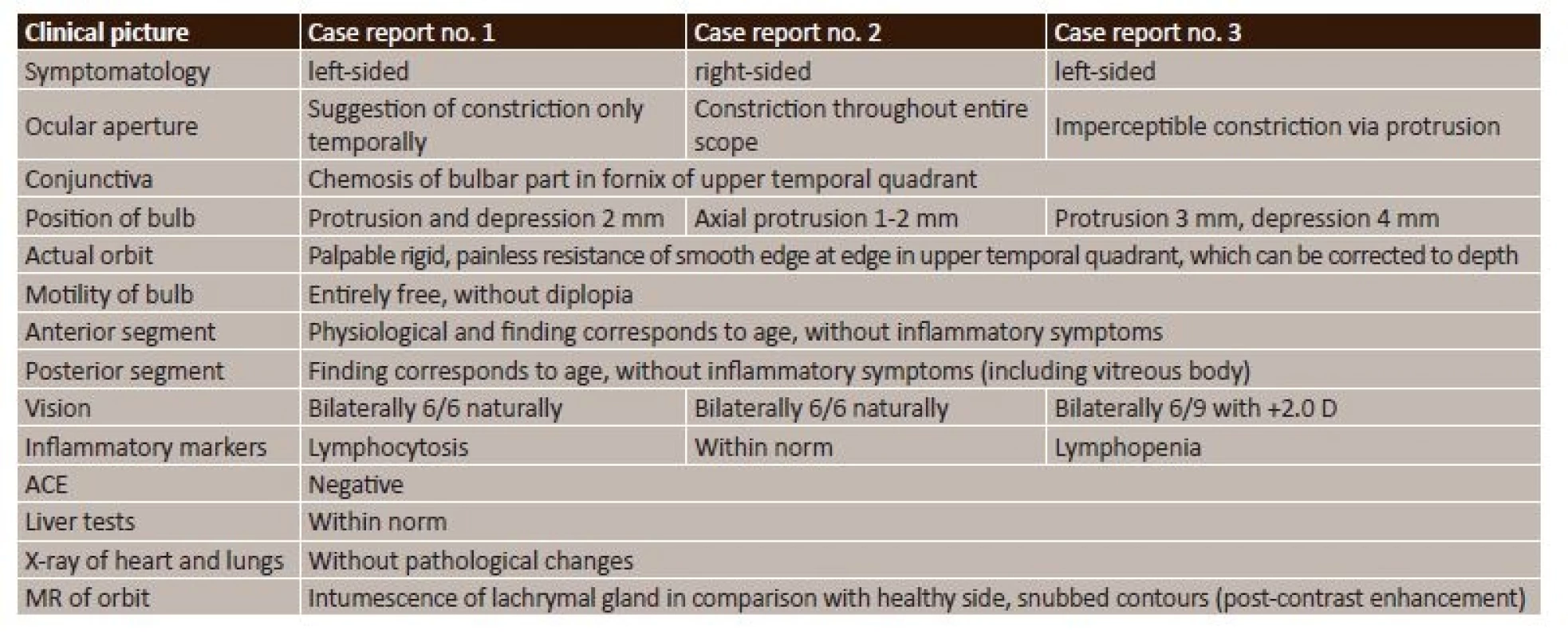
Fig. 1. Clinical picture before determination of histological diagnosis (right) and condition after pacification following external orbitotomy (left) in patients with inflammatory pseudotumour of the lachrymal gland. Top case report no. 1, middle case report no. 2, bottom case report no. 3 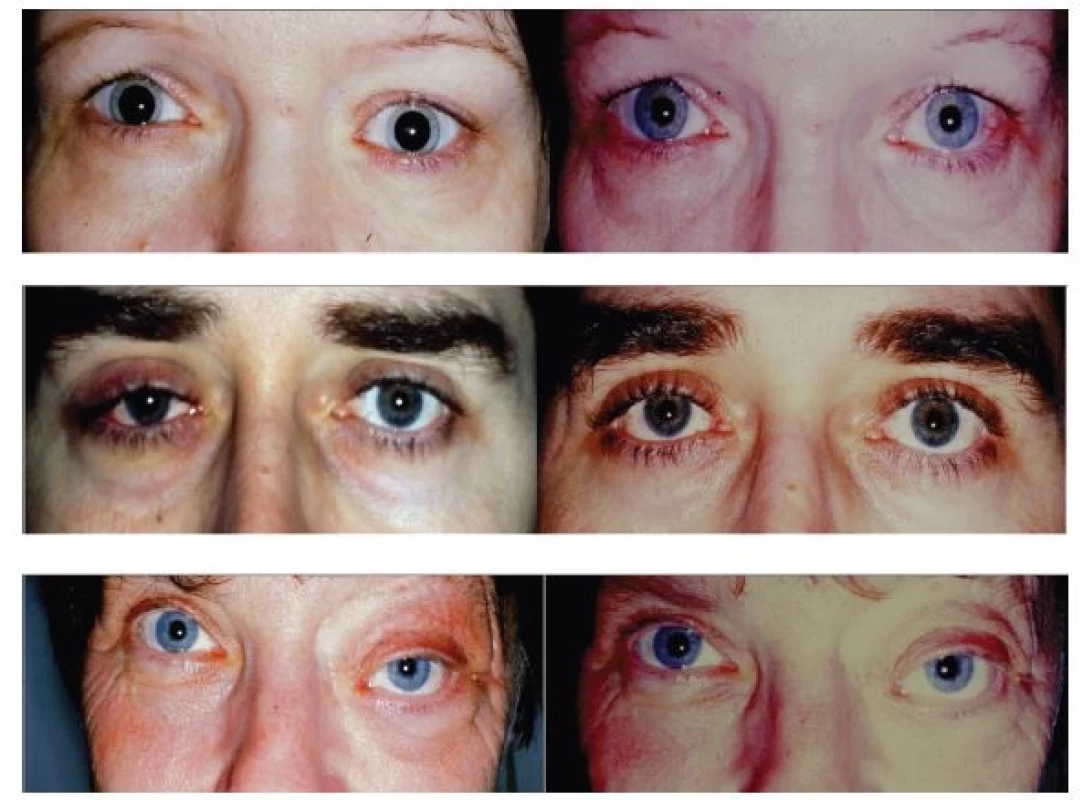
Observation of orbital sarcoidosis – orbital inflammatory syndrome and intrathoracic manifestation
Case report no. 4 presents a 55 year old woman who was first examined in March 2001, when she herself found a formation on the lower edge of the right orbit. At an examination at an outpatient clinic (fig. 2), there was tangibly palpation stiff, painless resistance maintaining its original shape, motility of the bulb was free in all directions, without diplopia. The finding on the anterior segment was without pathological changes, and on the ocular fundus the papilla was bordered, in a myopic conus – fundus myopicus with diffuse thinning of the RPE. VRE 6/9 p. with own correction -11.0 D.
Fig. 2. Clinical picture of orbital affliction in right eye (a), finding of orbital tumour on MR (b), image of galli scan (c) and histological verification of orbital biopsy (d) in patient with orbital inflammatory syndrome and intrathoracic manifestation of sarcoidosis 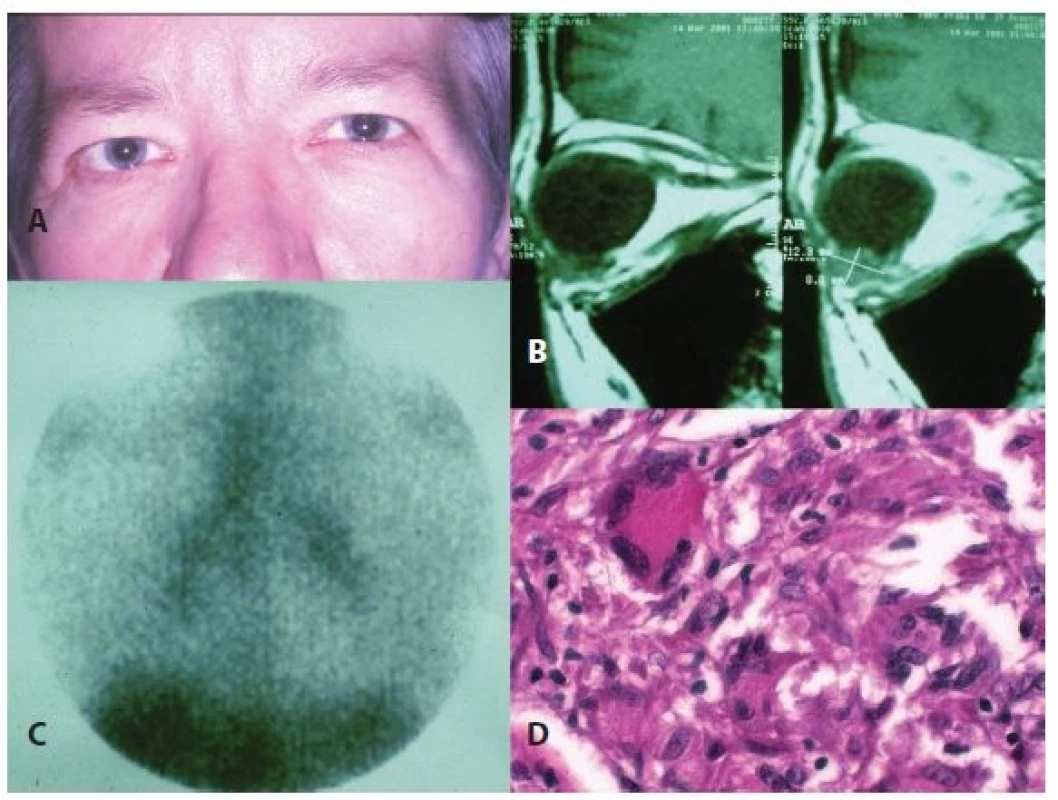
In the left eye the bulb is in slight convergence, dragging in movement in abduction and upwards temporally. The finding on the anterior segment, with the exception of conjunctival scars nasally and temporally, as well as the finding on the fundus, was analogous with that in the right eye. VLE fingers to ½ m with own correction -12.0 D (in anamnesis 2x operation for strabismus and amblyopia), IOP 18/17 mm Hg, Hertl 18-105-17.
MR orbit: Non-enhancing formation 12.3 x 8.8 mm on lower edge of orbit in right eye, due to its character suspicion of lymphoma, inflammatory changes or other etiology cannot be excluded (fig. 2). The same month a lower anterior orbitotomy was performed for the purpose of histological verification of the process.
Histological finding: granulomatous inflammatory infiltrate of orbit, non-caseifying, multinuclear cells predominantly of Langhans type, most probably sarcoidosis of the orbit (fig. 2).
A complex examination was conducted during hospitalisation at the Department of Tuberculosis and Respiratory Disorders at the General University Hospital in Prague with the following results: HRCT demonstrated mediastinal and hilar lymphadenopathy, galli scan demonstrated lambda sing (fig. 2) and BAL confirmed lymphocytic alveolitis. Diagnosis: 2nd degree intrathoracic sarcoidosis. Treatment was commenced in April 2001, with Prednisone 40 mg daily in the morning for two weeks, with decreasing tendency to February 2002. A follow-up MR in October 2001 demonstrated postoperative scarred changes in the right orbit, but without a pathological formation. The patient remained under observation, the last examination in 2014 was without signs of recurrence.
Observation of panuveitis in right eye and iridocyclitis in left eye secondary to neurosarcoidosis and hilar lymphadenopathy
Case report no. 5 observes the development of complex systemic sarcoid pathology in a 64 year old man from the beginning of 2009, when suspicion of sarcoidosis was stated at an examination at the department of pneumonology. He was first examined at the Department of Ophthalmology at Královské Vinohrady University Hospital in May of the same year upon the request of neurologists due to peripheral paresis of the facial nerve on the left side, manifesting itself as lagophthalmos. At the same time, an inflammatory reaction was detected in the anterior chambers of both eyes, with depositing of precipitates on the endothelium in the right eye and suspect inflammatory deposit on the retina of the right eye. VRE 6/9 s – 3.75 D and VRE 6/6 s – 3.5 D. Only local therapy with corticosteroids and mydriatics was applied. Two months later diplopia occurred due to incipient paresis of the abducens in the right eye, the patient stated weight loss of 14 kg. A complex examination followed: MR of the brain was within the norm, HRCT of the chest demonstrated mediastinal and hilar lymphadenopathy and interstitial pulmonary process, a transbronchial biopsy detected numerous epitheloid granulomas of a sarcoid type with massive multinuclear cells, and BAL documented an increased number of lymphocytes. Diagnostic conclusion: 2nd degree neurosarcoidosis. General corticoid therapy was commenced with Medrol 32 mg/day within the framework of a morning dose over a period of three weeks, and then in a reducing tendency until August 2010, subsequently general therapy was not indicated from a pulmonary or neurological perspective and so was discontinued.
In November of the same year, new activity of the chorioretinal deposit appeared in the right eye (anamnestically subjectively approximately six months of slightly deteriorated vision). Bilaterally the ocular apertures were symmetrical, without lagophthalmos in the right eye, motility of the bulbs was free, without diplopia. The finding on the anterior segments did not manifest inflammatory symptoms or trophic changes. The vitreous bodies manifested slight cellular adulteration, the papillas were bordered, pink, with minor central excavation, the maculas grainy, diffusely thinned pigment sheet of retina. On the right side, beneath the lower temporal arcade, there was a perceptible larger deposit without sharply defined bordering, with a size of 1 x 1.5 PD, slightly above the niveum (fig. 3a), without signs of vasculitis, retina lying. VRE 6/9 s – 4.0 RLE 6/9 s – 3.75, reads J. no. 1 nat. bilaterally, IOP 11/12 mm Hg. OCT bilaterally – neuroretina of normal thickness, without signs of accumulation of fluid, layer of RPE preserved. FAG OPL – demonstrated only bordered activity of deposit in right eye. With regard to localisation, general therapy was not applied. Regular two-monthly follow-up examinations were conducted. In February 2012 the anterior segment remained pacific, but cellular activity increased in the vitreous body. The chorioretinal deposit in right eye beneath lower temporal arcade was larger, not sharply bordered, with a size of 1 x 2.5 PD, slightly above the niveum, in comparison with the initial examination it was more voluminous, expanded in a downward direction across the arcade in the direction of the macula. The colouring of the retina changed, in the direction toward the papilla it took on a yellowish colour, probably from saturation of the choroid (fig. 3b). The retina was without signs of vasculitis. VRE 6/6 p. s – 4.5 D, RLE 6/6 p. s – 4.25 D, reads J. no. 1 nat. bilaterally, IOP 13/14 mm Hg. Corticotherapy was recommenced with Medrol 16 mg 1-1/2-1/2 two weeks, and further in a reducing dose over the course of four months. The patient was on a maintenance dose of 4 mg of Medrol per day for 1 year, then only monitored each 6 months, the observed deposit on the lower temporal arcade in the right eye without signs of activity, bordered, flat, scarred. At the last follow-up examination in August 2015 the condition was stabilised, not progressing with regard to visual acuity, the intraocular finding was also unchanged. The chorioretinal deposit in the right eye remained flat, same size, bordered and beneath the arcade of the lower temporal vein (fig. 3c). Monitoring of the patient shall continue.
Fig. 3. Development of chorioretinal finding in three stages (a, b, c) in a patient upon simultaneous neurosarcoidosis and hilar lymphadenopathy and finding of CME together with change on OCT (d) in patient with intermediate uveitis secondary to hilar lymphadenopathy with sarcoidosis 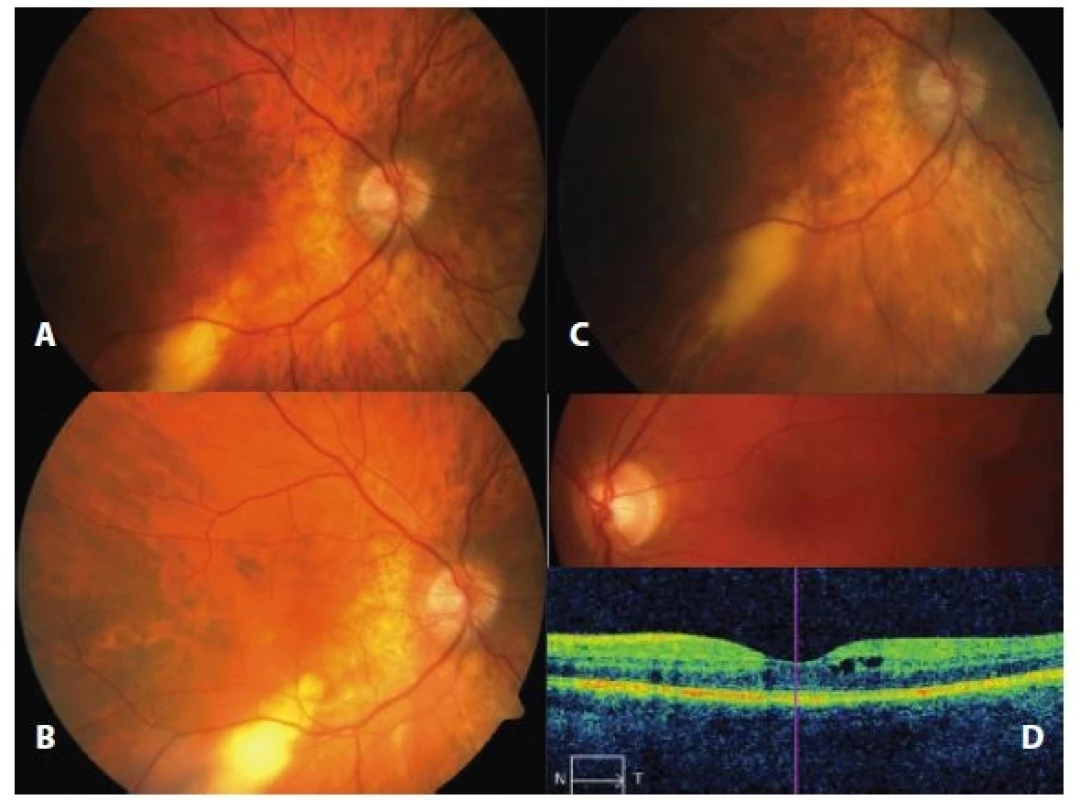
Observation of bilateral intermediate uveitis secondary to sarcoidosis hilar lymphadenopathy
Case report no. 6 describes the course of a pathology in a 39-year-old woman who reported to the Department of Ophthalmology due to acute bilateral uveitis in April 2011, having been aware of deteriorated vision and blurs in front of the right eye for two months. The examination determined cellular activity and precipitates on the corneal endothelium, flare and Tyndall effect in the anterior chambers. Pronounced cellular adulteration with defibering was confirmed in the vitreous bodies. On the funduses the papillas were bordered, in the maculas edema, peripheries of the retina without deposit changes and signs of vasculitis. VRE 1/10 p. s – 1.75, VLE 5/7.5 p. s – 1.0/135, reads J. no. 8 in right eye and J. no. 2 in left eye, IOP 12/12 mm Hg. OCT bilaterally revealed edema on the level of the neuroretina, more in right eye, layer of RPE preserved. Diagnosis: Bilateral intermediate uveitis. Treatment was commenced immediately with regard to the deterioration of visual acuity: Medrol 32-24-24 mg daily for a period of 10 days, subsequently with a reducing tendency, locally corticosteroids and mydriatics. A set of examinations followed: MR of brain and C-spine excluded demyelination plaques. X-ray of the lungs and heart showed slight prominence of hilums, more on left side, subsequent HRCT of the chest documented enlarged hilar lymph nodes bilaterally, but also paraaortally and paratracheally. A galli scan defined a lambda panda sign. A biopsy of the mediastinal nodes confirmed non-caseifying granolumas and BAL lymphocytosis. Conclusion – 1st degree sarcoidosis verified by biopsy. During the course of immunosuppressant therapy the inflammatory intraocular process was pacified. In June 2012 without signs of intermediate uveitis bilaterally, VRE 6/6 s – 1.75 and VLE 6/6 s – 1.0/135, reads bilaterally J.g. no. 1. Bilaterally, entirely physiological finding on OCT. General therapy continued only from pulmonary indication 10 mg prednisone daily for further two years. The patient was observed from an ocular perspective after six months. She did not report to us again until June 2015, due to deterioration of vision in the left eye. Upon examination the bulbs were pacific, anterior segment without inflammatory activity, vitreous body with defibering but without cellular adulteration, the retina was without deposit changes, in right eye macula without edema, but in left eye with saturation (fig. 3d), without signs of vasculitis. VRE 6/6 s – 0.5 = -0.75/65, VLE 5/10 s – 0.75/125, reads J. no. 1 in right eye, J. no. 4 in left eye, IOP 16/18 mm Hg, OCT in right eye - physiological finding, in left eye CME demonstrated with accumulation of fluid, CST 374 um (fig. 3d). FAG in left eye demonstrated only colouring of CME without further deposit changes. As a result Nevanac was applied only locally in left eye 3x daily. In the following months a further growth of CME in the left eye (CST 541 um) appeared, as a result 1.0 ml Diprophos was applied parabulbarly, after which only temporary regression of the finding was achieved (CST 274 um), but from October 2015 there was again progression of CME and in November this was added to by pronounced cellular activity in the vitreous body and snowballs in the lower temporal quadrant on the left side. For personnel reasons the patient was transferred into the care of the Centre for Uveitis in Prague, with a proposal for application of general immunosuppressant therapy. Medrol was again therapeutically administered, and the patient remained under observation.
DISCUSSION
The incidence of sarcoidosis is higher among the black race. Women are affected more frequently, and the majority of studies state a ratio of 2 : 1. Incidence is most common between the 20th and 30th, and between the 50th and 60th year of life, children are affected only rarely. It appears that this pathology is more common in mild and cold climatic conditions. Lethality is within the range of 2-4%. The respiratory organs are affected in 90-94% of all determined cases of the pathology (12). Changes on X-rays of the lungs are generally the first, often chance indication leading to diagnosis of sarcoidosis. All types of sarcoidosis of the respiratory organs are accompanied by lymphocytic alveolitis, which may be clinically entirely asymptomatic (18). Affliction of the lymph nodes is relatively frequent, stated in between 28 and 75% of patients (12). Enlargement of the spleen is stated at between 6 and 42% of cases (18), and is generally asymptomatic. Dermatological manifestations of sarcoidosis, occurring in 18 to 32% of cases (12), may be highly diverse, the most frequent manifestation is erythema nodosum. By comparison, Lupus pernio, defined in 1889 by Besnier, is the most typically described dermatological symptom. It concerns mutilating, perceptibly bordered lesions with dilated veins in the face (12, 18). Reddish-brown and soft papulonodular lesions also belong among the skin manifestations of sarcoidosis anywhere on the body. Affliction of the bones is generally asymptomatic, and its incidence fluctuates within the range of 2 to 24%. Affliction of the joints is manifested by polyarthralgia and arthritis, and is far more common than affliction of the muscles (18). Affliction of the joints also occurs in childhood age in the form of CSA (Childhood sarcoid arthritis). In differential diagnostics this must be differentiated from juvenile rheumatoid arthritis (JRA) (12), now indicated as JIA (juvenile idiopathic arthritis). CSA features a high representation of uveitis, in 80-90% of cases, and rash in 77%, with 40% ACE. This concerns polyarthritis, whereas in the case of JIA it is pauciarthritis. In JIA rash is rare, there is a low representation of uveitis and without positivity of ACE, by contrast there is present positivity of ANA. Sarcoidosis may affect any part of the nervous system, occurring in 5-7% of cases (12, 18). Most frequent are unilateral or bilateral paresis of the facial nerve, primarily of the peripheral type, stated in up to 70% (22). The optic nerve is affected in approximately 5% of cases, and is the second most common affliction of the head nerves. Affliction of the oculomotor nerves is also possible (18). Diplopia has been identified in 15% of cases (22). In one of our patients we recorded transitional diplopia, from affliction of the n. abducent (29). Sarcoidosis independently generates edema of the disc of the optic nerve, less frequently optic neuritis. Granulomatous infiltration of the optic nerve is characteristic of the pathology, despite the fact that it occurs rarely, and may be connected to affliction of the CNS. Manifestations of neurosarcoidosis may contain practically the entire neurological symptomatology – paresthesia, paralyses and convulsions in cases of peripheral neuropathy, ataxia, dementia, aphasia, epilepsy and psychosis (18). In patients with already diagnosed sarcoidosis, ocular manifestations appear depending on demographic and diagnostic criteria in 21-22% of cases (12). A large proportion of these patients are asymptomatic. According to retrospective studies, sarcoidosis is later confirmed by biopsy in 3.9-5.5% of patients with uveitis (12). In the majority of cases this concerns chronic form of uveitis with bilateral affliction (12, 18). Orbitopalpebral affliction is generally less frequent and may incorporate the lachrymal gland (3%), orbit (less than 1%) and also the conjunctiva, eyelids (12), which may however be a component of dermatological manifestations.
Acute anterior uveitis is more frequently unilateral with a finding of serous, in rarer cases fibrinous iridocyclitis, and may be a component of systemic manifestations such as erythema nodosum or bilateral hilar lymphadenopathy (12), which is designated as Löfgren's syndrome. Heerfordt-Waldenström syndrome (uveoparotid fever) is also accompanied by acute uveitis with potential affliction of the facial nerve (12). Chronic anterior uveitis is more common in patients between 40 and 60 years of age, with an image of granulomatous inflammation.
The diagnostic criteria of uveitis (16) incorporate: bilateral affliction, fatty precipitates and/or granulomatous precipitates and/or Koeppe's or Busacca's nodules on the iris, granulomas in the chamber angle and/or peripheral anterior synechiae, vitreous opacities of the character of “snowballs” or “strings of pearls”, multiple chorioretinal active or atrophic lesions in the periphery, periphlebitis (+/ - “dripping wax”) and/or retinal macroaneurysms, granulomas of the papilla of the optic nerve and/or solitary granuloma of the choroidea.
This finding is generally a component of the clinical picture of panuveitis (together with retinal vasculitis and macular edema), which is described in between 20 and 30% of cases (12). From the presented clinical pictures, independent chronic iridocyclitis was observed in two patients (32). Intermediate uveitis occurs in approximately 10% of cases. The patient usually reports a feeling of floating turbidities and a decrease of visual acuity, which was also described by our patient upon the initial manifestation and relapse. In the clinical picture it is manifested in a dual image in possible combination: vasculitis with venous occlusion in the periphery and vitritis of various intensity, from diffusely scattered cells to condensed. If these clusters appear in chains, we refer to the above-mentioned as “strings of pearls”, characteristic of sarcoidosis, but a range of other uveal syndromes may also occur (12). Posterior uveitis occurs in between 14 and 43% of patients, and may be the sole ocular manifestation of sarcoidosis. It appears that affliction of the fundus may be linked with an increased risk of affliction of the central nervous system (30), which was also manifested in one of our patients. It is manifested in granulomatous chorioretinitis with multiple small yellowish granulomas. This picture was accompanied also by affliction of the disc of the optic nerve beneath an image of papillitis (7, 32). Inflammatory changes of the papilla were a part of the manifestations of intermediate uveitis, and created a picture of panuveitis (14), or were a manifestation in acute iridocyclitis in a child patient (13). All the published observations of uveitis in our region (7, 13, 14, 32), identically as in the case of our two patients, were accompanied by pulmonary symptoms of sarcoidosis.
Diagnostic examinations (16) combine the following: negative tuberculosis test, elevation of ACE and/or elevation of serum lysozyme (in patients treated with ACE inhibitory), image of hilar lymphadenopathy on skiagram of chest, increase of liver enzymes and positive finding on chest CT upon negative X-ray of lungs. Non-invasive imaging methods have the greatest significance in the diagnosis of systemic sarcoidosis. Pathological changes on classic CT in 79% (5) or abnormal HRCT in up to 96.3% were determining for the diagnosis of the pulmonary form (3). MR of the brain was significant for diagnosis of neurosarcoidosis in 80% (5).
A combination of diagnostic criteria determines the certainty of the diagnosis of sarcoidosis (16):
- a) definitive diagnosis of sarcoidosis – positive biopsy + uveitis corresponding to ocular form of sarcoidosis;
- b) expected diagnosis of sarcoidosis – biopsy not performed, hilar lymphadenopathy + uveitis corresponding to ocular form of sarcoidosis demonstrated on skiagram of chest;
- c) probable diagnosis of sarcoidosis – biopsy not performed and negative X-ray of chest, but three clinical criteria + two positive examinations are present;
- d) possible diagnosis of sarcoidosis – negative biopsy, but four clinical criteria + two positive examinations are present.
Differential diagnosis of uveitis with etiology of sarcoidosis is diverse and difficult, because individual uveal symptoms in connection with sarcoidosis are not absolutely pathognomonic. Sophisticated photo documentation assists diagnosis, as stated in the literary data (28). Six patients were included in our cohort, always with a positive biopsy finding, thus this concerned a definitive diagnosis of sarcoidosis. We did not include a number of further patients with the above-stated symptoms in uveitis in the cohort of our study without a positive biopsy. From the perspective of possible combinations indicating this diagnosis (16) there emerged a higher representation of sarcoidosis in the etiology of uveitis. In children this is stated at from 1 to 3% (24) and in adults it fluctuates within the range of 10% (24) to 11.50% (10), in our region it was last recorded in 4% of cases, i.e. 60 patients out of 1523 observed cases of uveitis (15). The distribution of individual types of uveitis upon sarcoidosis represents 15 to 28% of anterior uveitis, 38 to 46% of intermediate inflammations and 36 to 38% of posterior together with panuveitis (24).
Orbitopalpebral affliction incorporates affliction of the conjunctiva, lachrymal gland and orbit. Nodules appear in the fornix or on the palpebral conjunctiva, in acute form they may be manifested in the form of follicular conjunctivitis or in chronic form with progressive scarring, leading to the formation of symblepharons. Large conjunctival granulomas may be reminiscent of tumours (24), but may also encroach upon the lachrymal drainage pathways (8). Conjunctival affliction is often overlooked, a large proportion of lesions are asymptomatic (24), and as a result diagnosis is not frequent. Furthermore, these types of inflammation are often locally treated with local corticosteroids, or with antibiotics without verification by biopsy, since the clinical condition improves following this therapy.
Affliction of the lachrymal gland represents the most common extraocular affliction (7-69%), mostly asymptomatic or with painless enlargement and reduced secretion of tears (24), and mostly has unilateral localisation. Biopsy diagnosis in the lachrymal gland confirms sarcoidosis in 42-63%. Granulomatous infiltration of the lacrhymal gland may cause dry eye or keratoconjunctivitis sicca (KCS) (12, 24), which we did not primarily identify in our patients. Later reduced production of tears was conditional upon loss of the lachrymal gland, but was not accompanied by KCS. Primary diagnosis is frequently difficult. In differential diagnostics it is necessary to consider above all a tumour, e.g. carcinoma. External orbitotomy is necessary, with subsequent histological verification. We confirmed a diagnosis in three of our patients, in which sarcoidosis was only a mono-organ affliction. In all of the patients the diagnosis was unexpected, mainly in the oldest patient with a six-week anamnesis, in whom we expected a malignant process. Mono-organ affliction was detected practically sixty years ago by authors from Brno (2). Orbital localisation as the primary localisation of sarcoidosis is rare, in a single Czech orbital monograph two cases are described over 30 years of observation of orbital processes (23). Orbital inflammatory syndrome, incorporating protrusion of the bulb, swelling of the eyelids, pain and rarely deterioration of vision (25), is not common. The entire process may be covered with minimal protrusion (17) as in the case of our patient. Isolated observations in recent years have demonstrated that the result of the biopsy is always surprising (17, 25), as confirmed by our first observation (6), which triggered a complex examination. As a result, it is of fundamental importance to ensure correct verification of the process in the orbit, which confirms the inflammatory process with dominance of epitheloid cells from transformed macrophages with the presence of multinuclear cells of the Langhans type, the inflammatory infiltrate has the character of non-caseifying granuloma. Upon this histological finding it is necessary to use differential diagnostics to consider, and in correlation with the clinical findings exclude further possible types of granulomatous inflammations: in first place non-caseifying productive form of tuberculous inflammation, followed by mycotic inflammation, granuloma around a foreign body or exogenously acting material, granuloma around destroyed (and possibly also secondarily expired) cyst or “necrobiotic granuloma”. A detailed histological examination of the entire material is therefore essential, also with the use of special colourings targeted at the detection of any potential microflora, or immunohistochemical examinations. The histological diagnosis of sarcoidosis is thus, within the framework of the aforementioned differential diagnostics, ultimately a de facto diagnosis determined per exclusionem (33). Upon a comparison of orbital biopsy findings over a period of 10 years, we detected sarcoidosis in 4.6% of cases (20). Affliction of the extraocular muscles and Tenon's capsule may cause diplopia and painful ophthalmoplegia, as well as focal subconjunctival hyperaemia (31). A concurrence of orbital positivity of biopsy (17, 24) with systemic affliction is stated in 34 to 50% of cases, in which the absolute majority in 88-90% are formed by bordered lesions, as in the case of our patient, unlike infiltrative processes in 10-15% (24). The orbital process may also have a benign course (34), or alternatively may be manifested simultaneously with acute iridocyclitis and nodular syndrome (14).
Generally in the treatment of systemic sarcoidosis, the “gold standard” still remains generally administered corticoids (18). In ocular forms, namely intermediate, posterior uveitis and panuveitis in the case of sight-threatening inflammations, as well as in orbital processes and inflammations of the optic nerve, generally administered corticosteroids are still recommended in first place (12, 24, 28), in a dose of 0.5 to 1 mg/kg/day (28). In the case of inflammations which do not respond to corticosteroids, systemic immunosuppressants are chosen: azathioprine, cyclosporine A, methotrexate, mycophenolate mofetil, or alternatively cytostatics: chlorambucil and cyclophosphamide (12, 24, 28). Both groups of pharmaceuticals can also be combined. In the treatment of granulomatous choroidal process, prednisone alone is ineffective, and treatment of the process took effect only after combination with methotrexate (22). A combination of systemic immunosuppressants is possible in the treatment of ocular sarcoidosis, namely methotrexate with azathioprine (14). A further degree of therapy is biological treatment indicated only in cases where the above-stated procedures are not tolerated or do not respond favourably (24), despite the risk that this treatment may induce granulomatous uveitis. Most frequently, anti-TNF-alpha therapy is used with the aid of infliximab (4, 26, 28) and adalimumab (1, 4, 26) in the case of panuveitis and multifocal choroiditis. Further anti-TNF medications for the treatment of uveitis secondary to sarcoidosis are etanercept, certolizumab and golimumab (24). In patients treated with interferon-alpha, this may be the cause of the development of granulomatous panuveitis of the type of sarcoidosis (9). Ranibizumab has been applied as a supplementary anti-VEGF treatment for choroidal neovascularisation generated upon chronic panuveitis (19). Minor neovascularisations can also be treated with laser coagulation (12). Anti-VEGF therapy (bevacizumab or ranibizumab) can be applied in the case of chronic CME (12). Complications of intraocular sarcoidosis ensue during the course of the pathology, but may be connected also with the manner of treatment, and include glaucoma, cataract, epiretinal membrane and CME (24). Secondary glaucoma is treated by means of local anti-glaucomatous agents, and in the case of insufficient compensation surgical intervention is appropriate. In the case of haemophthalmos or chronic vitreous opacities, it is possible to use pars plana vitrectomy (12). It is necessary to be aware that surgical solution of these complications brings with it a danger of severe postoperative inflammatory reaction (24).
The prognosis of sarcoidosis is generally favourable. In 2/3 of patients spontaneous remission of the pathology in clinical, radiological, functional and laboratory terms takes place within one to two years. In the remaining cases there is by contrast a tendency toward chronicity, i.e. the process becomes stationary (chronic inactive form), or progresses (chronic active form) and requires therapy. It is possible to expect recurrence in approximately 1/3 of treated patients within 2 years of the completion of therapy (18). The clinical course of intraocular sarcoidosis may be variable, and the prognosis depends on the afflicted structures of the eye. The risk is generally higher in patients with chronic uveitis who are not treated sufficiently or whatsoever (12). Long-term studies have demonstrated that 51% of patients with bilateral uveitis had vision better than 20/40 (24), or that visual acuity was better than 20/50 (27) in 89% of cases. Vision was worse than 20/120 in only 5% (24), or worse than 20/200 in 3% (27). The main cause of an irreversible deterioration of vision represents secondary glaucoma and subsequent chronic maculopathy (24). Long-term observation of a patient with immunosuppressant therapy for renal transplantation was presented in hypercalcaemia for sarcoidosis (36).
Current research into sarcoidosis is focusing on new relationships which could provide a closer specification of the pathology. New pathological relations are being sought in immunological examinations. Activation of alveolar macrophages stimulates the production of interleukin IL-1, which subsequently generates the proliferation of T-lymphocytes CD4 (helpers) subpopulation. A higher number of epitheloid cells appears, as well as increased production of lymphokines, the CD4/CD8 ratio increases (12), previously indicated as the immunoregulation index. The increase of this ratio was detected in 100% of cases in BAL in 30 patients (5). These examinations also include determination of the HLA locus, HLA-DRB1 0401 allele is considered significant (24), which is common for the black and white population. Proprionibacterium acnes was detected in granulomas of epiretinal membranes in patients with uveitis secondary to sarcoidosis. It still remains to determine the significance of this etiology in the pathogenesis of uveitis (11).
CONCLUSION
Ocular sarcoidosis may incorporate any part of the eye and its auxiliary organs. The most common manifestation is uveitis, KCS and conjunctival nodules. The ocular manifestation is presented through its symptoms in 20-30% of patients with sarcoidosis. Multi-disciplinary approaches are necessary in order to attain the best procedure in the therapy of ocular and systemic manifestation of the pathology. Corresponding treatment guarantees a good prognosis of vision.
Note: This communication processes an attestation study from 2016
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company.
MUDr. Petra Sokačová
Oční klinika FN Královské Vinohrady
Šrobárova 50, 100 34 Praha 10
e-mail: jan.krasny@fnkv.cz
Zdroje
1. Achille, M., Ilaria, P., Teresa, G., et al.: Successful Treatment with Adalimumab for Severe Multifocal Chorioiditis and Panuveitis in Presumed (Early-onset) Ocular Sarcoidosis. Int Ophthalmol, 36, 2016 : 129–135.
2. Anton, M., Pluhoš, M., Riebel, O.: Izolovaný sarkoid slzné žlázy. Čs Oftal, 15, 1959 : 375–379.
3. Babu, K., Shukla, S.B., Philips, M.: High Resolution Chest Computerized Tomography in the Diagnosis of Ocular Sarcoidosis in a High TB Endemic Population. Ocul Immunol Inflamm, 23, 2016 : 1–6.
4. Baughman, R.P., Lower E.E., Ingledue, R., Kaufman, A.H.: Management of Ocular Sarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis, 1, 2012 : 26–33.
5. Bezo, C., Maizoub, S., Nochez, Y., et al.: Ocular and Neuro-ophthalmic Manifestation of Sarcoidosis: Retrospective Study of 30 Cases. J Fr Ophthalmol, 36, 2013 : 473–480.
6. Borovanská, J., Krásný, J., Šach., J., et al: Granulomatózní zánět orbity – sarkoidóza, Sborník abstrakt z XI. výročního sjezdu ČOS, Hradec Králové, 2003, s. 84.
7. Čepilová, Z., Porubská, M., Fabianová, J.: Sarkoidóza – kazuistika. Čes a Slov Oftal, 64, 2008 : 34–37.
8. Dolinová, L.: Postižení spojivky a odvodných slzných cest sarkoidózou. Čs Oftal. 33, 1977 : 443–446.
9. Doycheva, D., Deuter, C., Stuebiger, N., Zierhut, M.: Interferon-alfa-associated Presumed Ocular Sarcoidosis. Graefes Arch. Clin. Exp. Ophthalmol. 247, 2009 : 675 – 680.
10. Engelhard, S.B., Patel, V., Reddy, A.K.: Intermediate Uveitis, Posterior Uveitis and Panuveitis in the Mid-Atlantic USA. Clin Ophthalmol, 9, 2025 : 1549–1555.
11. Goto, H., Usui, Z., Umazume, A., et al.: Proprionibacterium Acne as a Possible Pathogen of Granuloma in Patients with Ocular Sarcoidosis. Br J Ophthalmol, 111, 2017: doi: 1136/bjothalmol-2016-309248.
12. Hainovici, R., Foster, C.S.: Sarkoidosis, In. Pepose J.S., Holland G.N., Wilhelmus K.R.: Ocular Infection and Immunity, Mosby, St. Louis, 1996, p. 754–776.
13. Hanušová, H.: Oční projevy sarkoidózy v dětském věku, Čs. oftal.: 44, 1988 : 212 – 215.
14. Havlíková, M., Říhová, E., Kopřivová, J. et al: Oční projevy sarkoidózy, Čs. oftal., 1994 : 367–370.
15. Heissigereová, J., Říhová, E., Svozílková, P., et al.: Uveitidy u neinfekčních systémových onemocněních. Abstrakta Den uveitid, 2010, JS Parner s.r.o., s. 11, ISBM 978-80-87036-50-1.
16. Herbort, C.P., Rao, N.A, Mochizuki, M., et al.: 23 Collaborated Members of Soc. Com. of 1st Internat. Workshop on Ocular Sarcoidosis: International Criteria for the Diagnosis of Ocular Sarcoidosis: Results of the 1st International Workshop on Ocular Sarcoidosis, Ocular Immunol. Inflamm., 17, 2009 : 160–169.
17. Kang, J.J., Aakalu, V.K., Lin, A., Sebtabutr. P.: Orbital Granuloma Annulare as Presentation of Systematic Sarcoidosis. Orbit, 32, 2013 : 372–374.
18. Kolek, V. Sarkoidóza. Známé a neznámé. Praha: Avicenum, 1998, 239 s.
19. Konidaris, V.E., Empeslidis, T.: Ranibizumab in Choroidal Neovascularisation Associated with Ocular Sarcoidosis. BMJ Case Rep. 2013, doi: 10.136/bcr-2013-010288.
20. Krásný, J., Šach, J., Brunnerová, R., et al.: Orbitální tumory u dospělých – desetiletá studie, Čes a Slov Oftal, 64, 2008 : 219–217.
21. Mayer, G.N., Longo, M., Gomes B.B. Nobrega, M.J.: Low Dose Corticosteroid in Association wih Methotrexate for Therapy of Ocular Sarcoidosis. Report of a Case. Int. J. Retina Vitreous. 1, 2015: doi: 10.1186/s40942-0215-0006-7.
22. Menezo, V., Lobo, A., Yeo, T.K., et al.: Ocular Features in Neurosarcoidosis. Ocul Immunol Inglamm, 17, 2009 : 170–178.
23. Otradovec, J.: Choroby očnice, Avicenum, Praha, 1986, s. 177 – 178.
24. Pasadhika, S., Rosenbaum, J.T.: Ocular Sarcoidosis. Clin,. Chest Med. 36, 2015 : 669 – 683.
25. Petrarolha, S.M., Rodrigues, B.S., Filho, F.D. et al.: Unilateral Eyelid Edema as Initial Sign of Orbital Sarcoidosis. Case Rep Ophthalmol Med, 2016, doi:1.1155/2016/6912927.
26. Riancho-Zarrabeitia, L., Calvo-Rio, V., Blanco, R., et al.: Anti-TNF-alfa Therapy in Refractory Uveitis Associated with Sarcoidosis: Multicenter Study of 17 Patients. Semin Arthris Rheum, 45, 2015 : 361–368.
27. Rochepeau, P., Jamilloux, Y., Kerever, S., et al.: Long-term Visual and Systemic Prognoses of 83 Cases of Biopsy-proven Sarcoid Uveitis. Br J Ophthalmol, 110, 2016, doi: 10.1136/bjophthalmol-2016-309762.
28. Říhová, E. et al.: Uveitidy. Grada, Praha, 2009, s. 75 77.
29. Sokačová, P., Šach., J., Krásný, J.: Klinické rozhraní problematiky sarkoidózy, Abstrakta Den uveitid, 2012, JS Parner s.r.o, s. 8, ISBM 978-80-87036-61-7.
30. Spalton D.J., Sanders M.D.: Fundus Changes in Histologically Confirmed Sarcoidosis, Br. J. Ophtalmol., 65, 1981 : 348–358.
31. Stannard K, Spalton D.J.: Sarcoidosis with Infiltration of the External Ocular Muscles, Br J Ophtalmol, 69, 1985 : 562–566.
32. Szedélyová, L., Gašparová, D., Kuřátko, J.: Očné zmeny pri sarkoidóze. Čs Oftal, 35, 1979 : 12–15.
33. Šach, J.: Histopatologie. In Kuchynka, P. a spol.: Oční lékařství, (1. vyd.) Grada, Praha, 2008, s. 61–97.
34. Uher, M.: Sarkoidóza očnice s benigním průběhem. Čs oftal.19, 1963 : 333–337.
35. Wong, E.K., Husain, A., Sayer, J.A.: Sarcoidosis Presenting with Hypercalcemia Following Withdrawal of Long-term Immunosuppression in Renal Transplantation. Oxf Med Case Reports, 5, 2014 : 86–88.
Štítky
Oftalmológia
Článek Autorský rejstřík
Článok vyšiel v časopiseČeská a slovenská oftalmologie
Najčítanejšie tento týždeň
2017 Číslo 5-6- Cyklosporin A v léčbě suchého oka − systematický přehled a metaanalýza
- Dlouhodobé výsledky lokální léčby cyklosporinem A u těžkého syndromu suchého oka s 10letou dobou sledování
- Účinnost a bezpečnost 0,1% kationtové emulze cyklosporinu A v léčbě těžkého syndromu suchého oka − multicentrická randomizovaná studie
- Pomocné látky v roztoku latanoprostu bez konzervačních látek vyvolávají zánětlivou odpověď a cytotoxicitu u imortalizovaných lidských HCE-2 epitelových buněk rohovky
- Konzervační látka polyquaternium-1 zvyšuje cytotoxicitu a zánět spojený s NF-kappaB u epitelových buněk lidské rohovky
-
Všetky články tohto čísla
- OCT Findings and Long-term Follow-up Results of Vitrectomy in Patients with Optic Disc Pit and Associated Maculopathy
- PERSISTENT HYALOID ARTERY – PERFORM A SURGERY OR NOT?
- Combination of Intravitreal Corticosteroid with Anti-vegf in Macular Edema Secondary to Retinal Vein Occlusion
- Jubileum doc. MUDr. Šárky Pitrové, CSc., FEBO
- Sarkoidosis and its Eye Ocular Manifestation (an Analysis of Six Case Report)
- Results of Treatment of Diabetic Retinopathy by the Laser System PASCAL
- Ciliary body melanoma treatment by stereotactic radiosurgery
- The treatment results in patients with lmphoma disease in the orbit
- The Difference between Ganglion Cell Complex and Nerve Fiber Layer in the Same Altitudinal Halves of the Retina in Hyper-tension and Normal-tension Glaucomas
- Xerosis in Patient with Vitamin A Deficiency – a Case Report
- Recommended procedure for eye examination for infants and children of pre-school age in regular outpatient practice
- Autorský rejstřík
- Česká a slovenská oftalmologie
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Sarkoidosis and its Eye Ocular Manifestation (an Analysis of Six Case Report)
- Recommended procedure for eye examination for infants and children of pre-school age in regular outpatient practice
- PERSISTENT HYALOID ARTERY – PERFORM A SURGERY OR NOT?
- The treatment results in patients with lmphoma disease in the orbit
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy




