-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Results of Treatment of Diabetic Retinopathy by the Laser System PASCAL
Authors: J. Němčanský 1,2; A. Stepanov 3,4; S. Němčanská 1,2; H. Langrová 3,4; J. Studnička 3,4
Authors place of work: Fakultní nemocnice Ostrava, Oční klinika, přednosta MUDr. Jan Němčanský, Ph. D. 1; Ostravská univerzita v Ostravě, Lékařská fakulta, Katedra kraniofaciálních oborů, vedoucí katedry prof. MUDr. Pavel Komínek, Ph. D., MBA 2; Univerzita Karlova, Lékařská fakulta Hradec Králové, Katedra očního lékařství, vedoucí katedry prof. MUDr. Naďa Jirásková, Ph. D., FEBO 3; Fakultní nemocnice Hradec Králové, Oční klinika, přednostka prof. MUDr. Naďa Jirásková, Ph. D., FEBO 4
Published in the journal: Čes. a slov. Oftal., 73, 2017, No. 5-6, p. 198-203
Category: Původní práce
Summary
Purpose:
To evaluate anatomical, functional and clinical efficacy of the pattern scanning laser (PASCAL®) photocoagulation in patients with diabetic retinopathy.Methods:
The cohort included 91 eyes in 50 patients (average age 63 years, 24 men and 26 women) treated at the Clinic of Ophthalmology, Faculty Hospital Ostrava, from 2008 to 2013. All eyes showed the signs of diabetic retinopathy (20.9% of eyes – very severe non-proliferative diabetic retinopathy (NPDR), 79.1% of eyes - proliferative diabetic retinopathy (PDR)). All the eyes were „treatment naive“. The average duration of diabetes was 18 years, average baseline HbA1c value was 8.2 %. Panretinal photocoagulation was performed with by the means of PASCAL photocoagulator – with patterns and short duration pulses. Best corrected visual acuity (BCVA), central retinal thickness (CRT), fundus photography, biomicroscopy and complications were evaluated during the minimum of 12 months follow-up period. Statistical analysis using Shapiro-Wilk a Friedman tests with p value less than 0.05 was done.Results:
Mean baseline BCVA was 0.13 logMAR. Values 0.12, 0.15 and 0.19 logMAR were observed in the follow-up intervals at the 4th, 6th and 12th month. At the 6th month visit all 91 eyes (100 %) were stabilized, and at the 12th month visit in 5 eyes (5.5 %) progression of the disease was observed. No complications were observed during the first 12 months follow up.Conclusion.
Laser photocoagulation of the retina with the use of short pulse durations and patterns in patients with DR is an effective and safe method of treatment.Key words:
diabetic retinopathy, laser photocoagulation, patterns, low time of impulse, PascalINTRODUCTION
Laser systems are used in ophthalmology, in both the diagnosis and in the therapy of pathologies of the anterior and posterior segment of the eye. Laser photocoagulation (LPC) of the retina ranks among the traditional techniques of treatment that became standard in ophthalmology in the middle of the 20th century. In LPC the aim is to achieve the destruction of tissue which is significant in a range of vascular pathologies of the retina – diabetic retinopathy (DR), (8, 19), diabetic macular edema (DME), central or branch retinal vein occlusion (CRVO, BRVO), ocular ischemic syndrome, neovascular glaucoma and others. To date the standard technique for the performance of LPC in the case of DR is considered to be the protocol from the Diabetic Retinopathy Study (DRS) and Early Treatment Diabetic Retinopathy Study (ETDRS). This protocol is based on the technical prerequisites of the available laser systems, which produced individual impulses with a duration of 0.1-4 s, and its effectiveness was supported by therapeutic results and especially by the above-stated randomised studies (5, 6). In the past decade new technologies have been introduced into industry and medicine, which have led to the development of a new generation of laser systems. These utilise more precise and sophisticated crystals for focusing the beam itself. Upon simple stepping on the pedal, dozens of impulses with a duration of 20 ms and less are sent within tenths of a second. At the same time, with the aid of an electro-magnetic field, a mirror is rotated, progressively altering the position of the beam, so that the impulses are focused in “patterns”. The individual traces are more homogeneous and the changes of tissues are concentrated in the outer retinal layers (RPE, outer and inner segments of photoreceptors, external nuclear layer), whilst preserving the inner retinal layers (1, 7, 16). Upon threshold photocoagulation of the retina (i.e. upon visible laser trace), in which we wish to attain an effect comparable with classic photocoagulation, the optimal impulse time appears to be 20 ms. In this a higher output is used in comparison with conventional lasers, but the tissues are exposed overall to a lower energy burden. In shorter times there is a risk of rupture of the RPE (7).
The first commercially available laser of this class was the PASCAL laser (pattern scanning laser) (1).
The aim of the submitted study is to present our experience with the performance of laser photocoagulation of the retina with the aid of a laser system, using patterns and low impulse times in patients with diabetic retinopathy (DR).
METHOD
In the period from 1 June 2008 to 30 June 2013, we selected a cohort of 91 eyes of 50 patients treated at the Department of Ophthalmology at the University Hospital Ostrava. All had very advanced non-proliferative diabetic retinopathy (NPDR) or proliferative diabetic retinopathy (PDR), and at the same time there was no presence of clinically significant DME (CSME) demonstrated by biomicroscopic examination of the fundus, colour photography of the fundus and fluorescence angiography.
For all patients an anamnesis was taken, best corrected visual acuity (BCVA) was determined for distance vision on Precision Vision optotypes with notation for testing at 4 metres – ETDRS chart 1.2 R + Illuminator Cabinet Mod. 2425E (Precision Vision, First Street, La Salle, IL, USA), and the result was converted according to the conversion table into a logarithm of minimal angle of resolution (logMAR) within the range of 0.00-1.00. At the same time spectral OCT of the macula was performed on OCT Spectralis (Heidelberg Engineering, Inc., Carlsbad, California, USA). Complete panretinal photocoagulation (PRP) of the retina was performed on all patients, using patterns and times of impulses of 20 ms with the aid of a Pascal Photocoagulator (Topcon Medical Laser Systems, Inc., Santa Clara, CA, USA). First of all the output necessary for the creation of one trace was titrated, the time of an individual impulse was 20 ms, the size of the trace 400 µm and the output was progressively increased until a laser trace of grey colour was attained. A pattern was then selected, as a rule 3 x 3, 4 x 4 or 5 x 5. The complete treatment was performed in one or two episodes/sessions. A follow-up examination was conducted 4 months after the initial examination, then 6 months from the initial examination and subsequently at six months intervals until 48 months after the initial examination. At the individual intervals the parameters displayed in table 1 were observed and evaluated. The proportions of patients were also evaluated according to changes of BCVA (improvement by more than 3 rows, improvement within the range of 0.01-3 rows, deterioration within the range of 0-3 rows and deterioration by more than 3 rows according to ETDRS optotypes). In addition, the frequency of complications was analysed. The aim was also to demonstrate the clinical effect of laser photocoagulation of the retina with the aid of the innovative laser PASCAL, which was evaluated as fulfilment of the purpose (stabilisation of the clinical finding) at subsequent follow-up examinations in comparison with the initial examination.
Tab. 1. Evaluated parameters and time intervals of follow-up examinations (M – month) 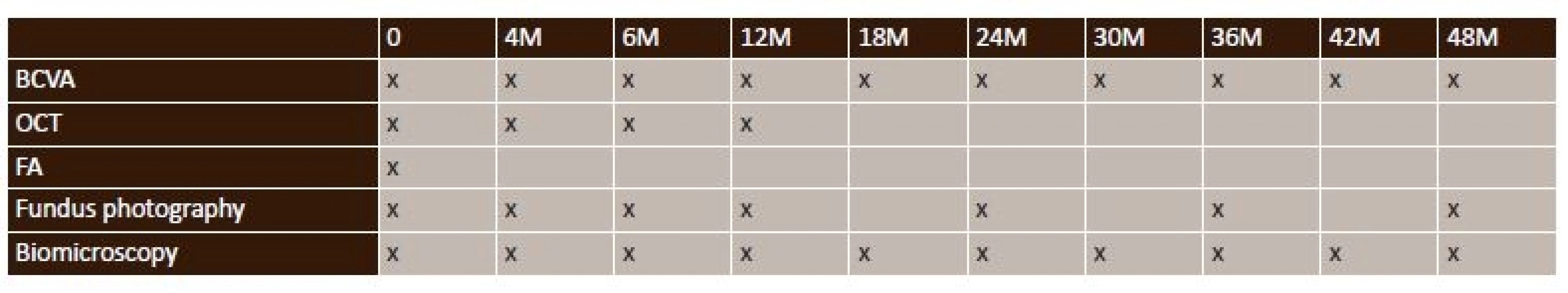
BCVA – best corrected visual acuity; OCT – optical coherence tomography; FA – fluorescence angiography; M – month Stabilisation (S) was taken as constituting a stable finding within the periphery of the retina, or an improvement thereof. A condition was evaluated as progression (P) in the case of occurrence of new vitreous or preretinal haemorrhage, the occurrence of new or progression of existing neovascularisations, the advancement of retinal detachment or in the absence of regression of existing haemorrhage. From this group we further detached the subgroup “failure of treatment” (F), when even further therapeutic intervention did not lead to stabilisation of the pathology and it was no longer possible to influence the condition therapeutically.
Using the method of descriptive statistics, we compiled a description of the variables. In addition, in the case of linked variables, a Shapiro-Wilk normality test was conducted. In order to determine the significance of changes during the observation period in linked variables, depending on their normality a dispersion analyses was used for repeated measurements, or a Friedman test. All the statistical tests were conducted as bilateral on a level of significance of 0.05. The statistical analysis was conducted with the aid of the software IBM SPSS Statistics version 22.
RESULTS
The general characteristics of the cohort are displayed in table 2. In 41 eyes a complete treatment was performed during one session, in 50 patients during 2 sessions, the mean number of applied points was 2008 (range 1600-3700, median 2000, standard deviation (SD) 485).
Tab. 2. General characteristics of cohort 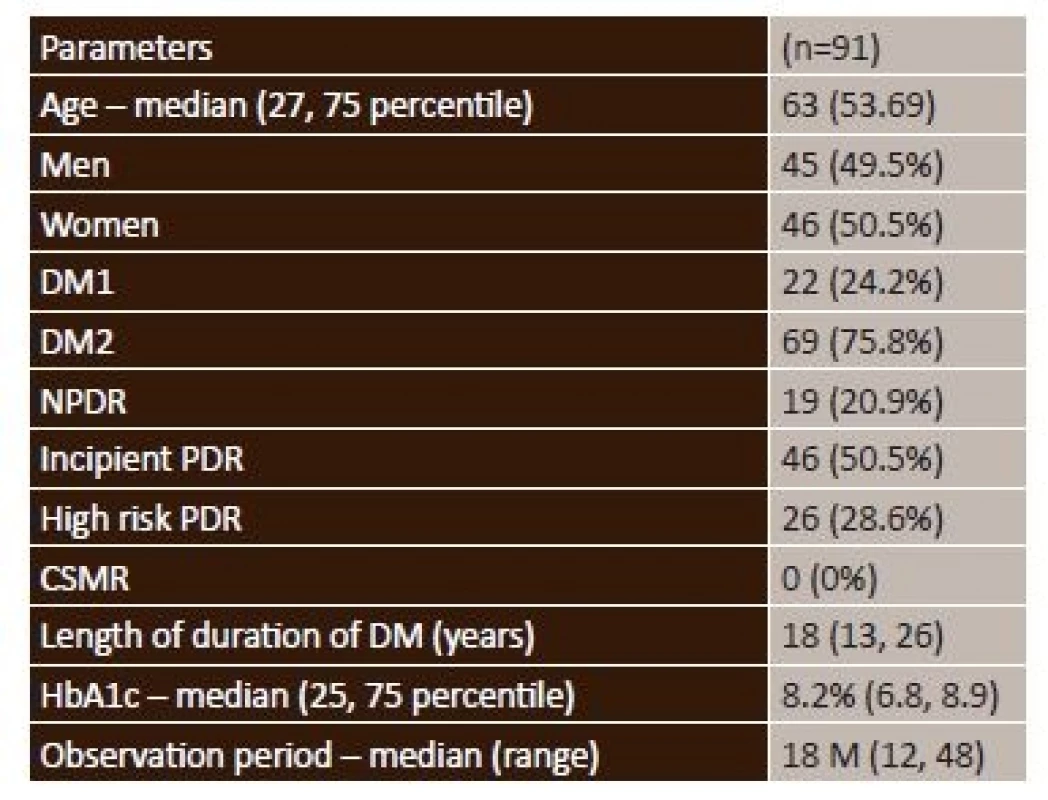
N – number of eyes; HbA1c – glycated haemoglobin; M – month Best corrected visual acuity
Initial BCVA was 0.13 logMAR, at subsequent follow-up examinations 0.12, 0.15 and 0.16 logMAR. The development of BCVA graphically, including the median and the 1st and 3rd quartile, is illustrated graphically in fig. 1 and 2. Table 3 presents an independent evaluation of the distribution of patients with an improvement within the range of 0.01-3 rows, a deterioration within the range of 0-3 rows and a deterioration by more than 3 rows of ETDRS optotypes 12 months after the beginning of observation. No improvement by more than 3 rows was recorded in any of our patients.
Fig. 1. Development of average BCVA at individual intervals (M – month) 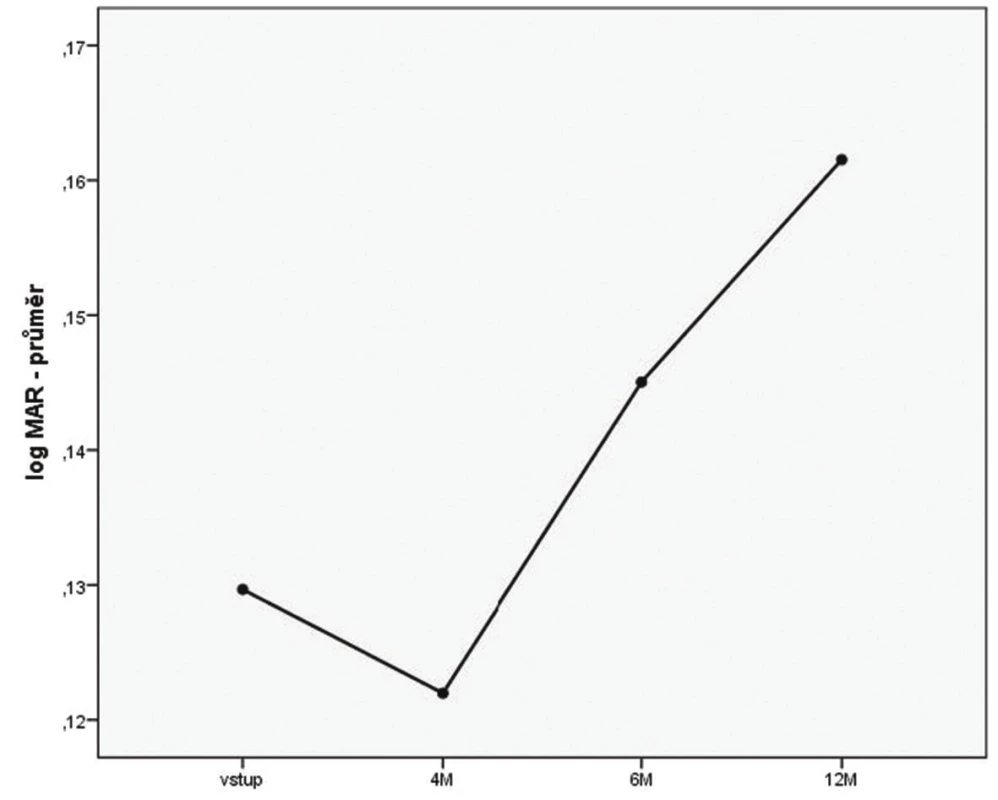
Fig. 2. Values of BCVA (logMAR) at initial visit and at individual intervals (M – month) 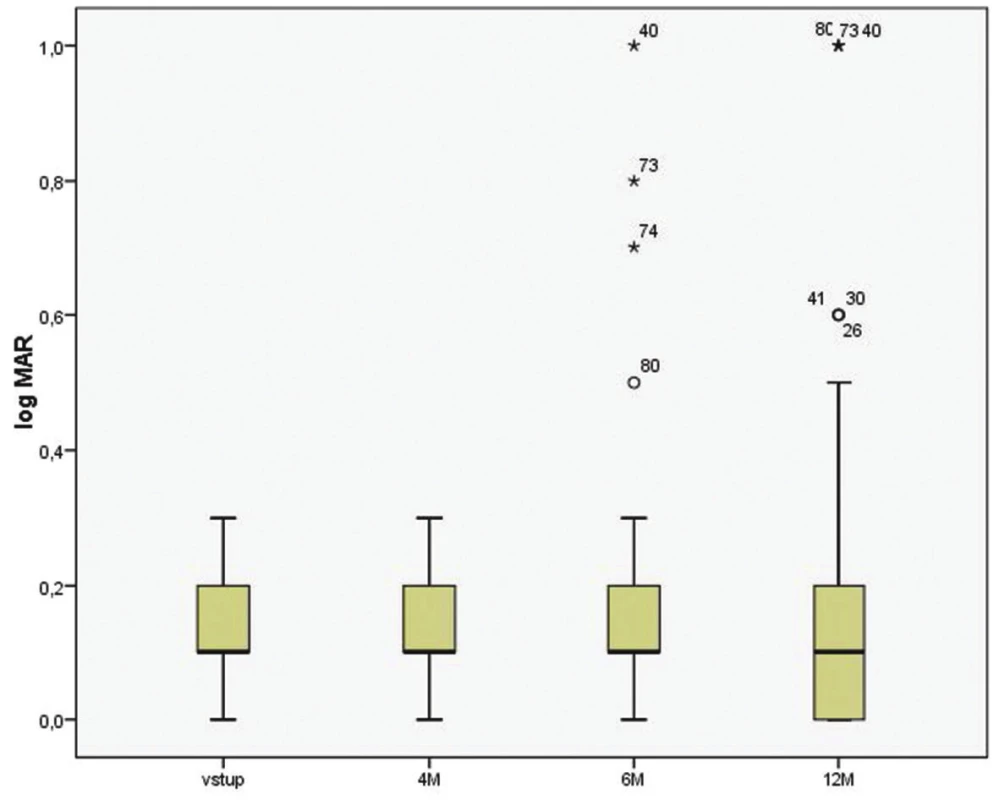
Tab. 3. Distribution of BCVA in individual categories 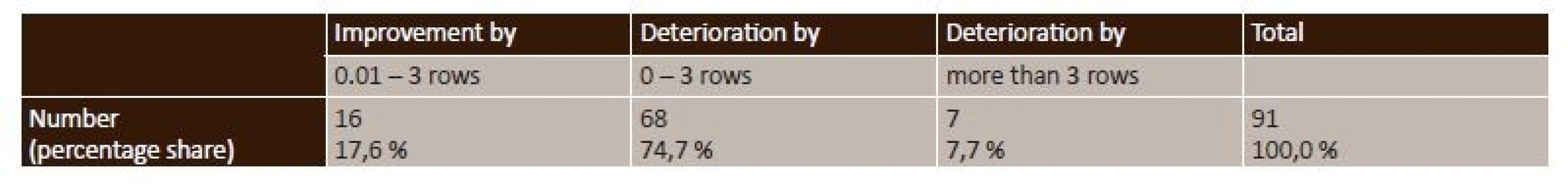
Central retinal thickness
The initial mean CRT was 259 µm, at subsequent follow-up examinations in the 4th month 259 µm, in the 6th month 260 µm and in the 12th month 256 µm. The development of CRT, including the median and the 1st and 3rd quartile is illustrated graphically in fig. 3 and 4.
Fig. 3. Development of mean CRT in individual intervals (M – month) 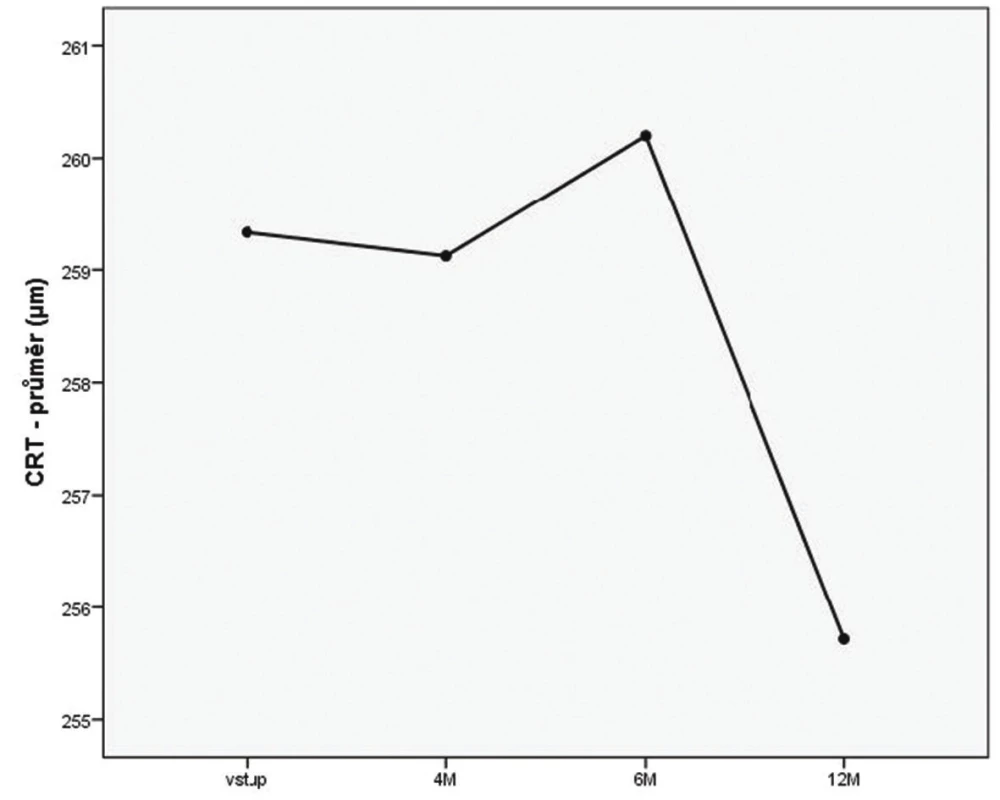
Fig. 4. Values of CRT at initial visit and in individual intervals (M – month) 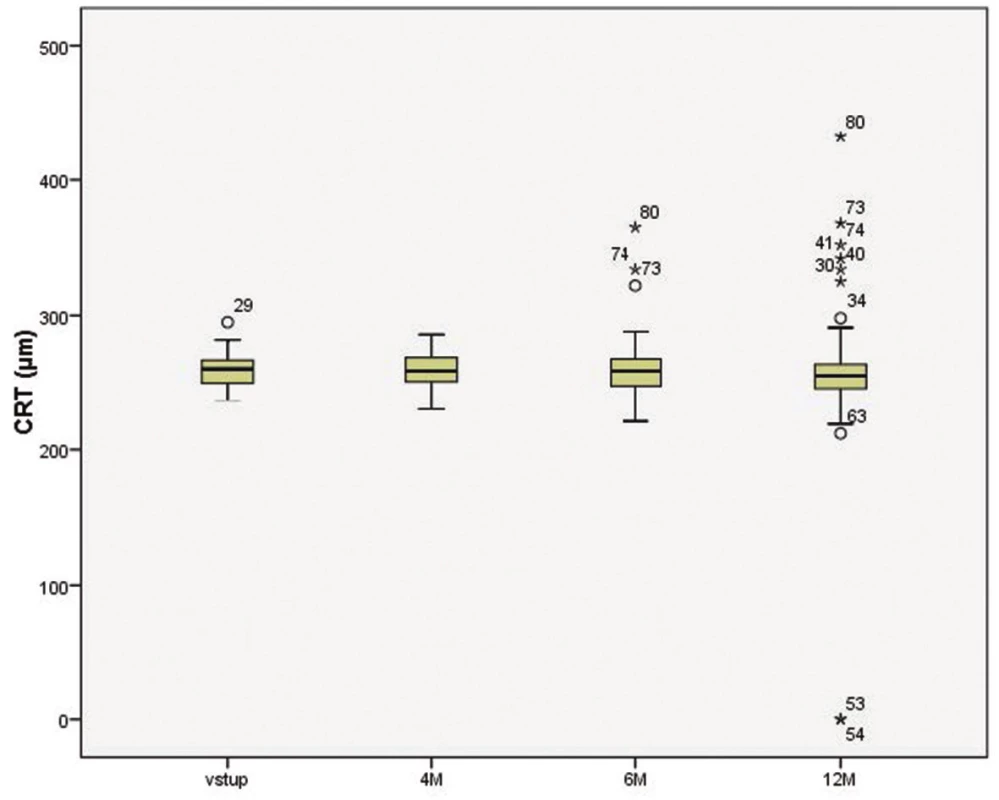
Parametric and non-parametric statistical tests further demonstrated that both the initial values of BCVA and CRT and the values observed observed during the observation period were statistically significantly comparable. In a number of patients we observed statistically significant deviations from the 95% confidence interval in the 6th and 12th month. This concerned patients in whom progression of the pathology occurred (see below).
Effectiveness of treatment and complications
In the period up to 6 months from the beginning of the observation period, stabilisation of the clinical finding was observed in all the patients included in the cohort. In the period between the 6th and 12th month of the observation, progression of the pathology occurred in 5 eyes. Table 4 illustrates the numbers of eyes and an evaluation of the effectiveness of treatment in the individual observation intervals, and the proportion of stabilisation, progression and failure of treatment. The clinical effect of treatment in all eyes during the course of the entire observation period is shown by the graph in fig. 5. Within 12 months of the observation period, no complications were observed.
Tab. 4. Effectiveness of treatment in individual intervals (N – number of eyes; M – month of observation) 
Fig. 5. Clinical effect of treatment (N = 91) 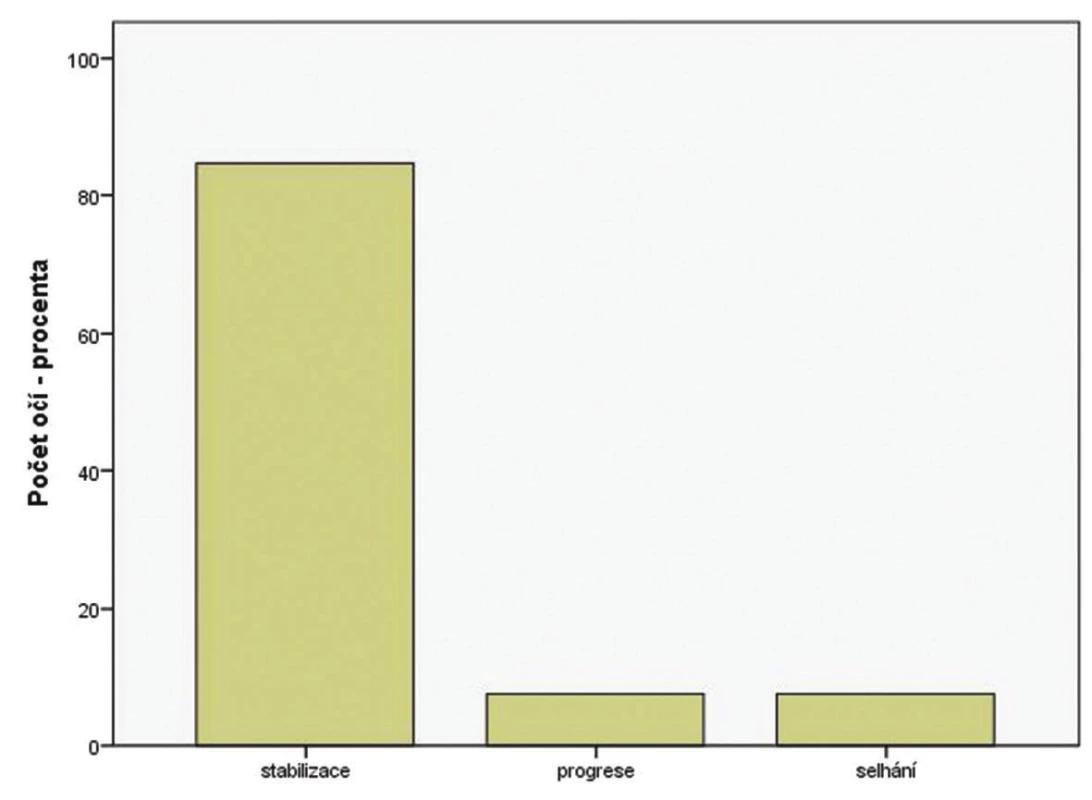
DISCUSSION
Our study evaluates the results of treatment by laser photocoagulation of the retina with low impulse times and using patterns in eyes of patients with diabetic retinopathy, indicated for panretinal photocoagulation of the retina. In indications of PRP and in the treatment itself we took as our basis the DRS and ETDRS studies, and performed “full scatter PRP” (5). Some authors mention and recommend also other methods of laser photocoagulation of the retina, such as focal treatment, “mild scatter PRP”, quadrant treatment in DR, technique of photocoagulation of the supplying blood vessel, bordering of tractional retinal detachment and others (10, 18). We intentionally did not use these techniques, since these concern procedures which are not unequivocally supported by studies meeting the most stringent requirements (degree A, I) of evidence based medicine.
From the analysis of BCVA it is possible to judge that stabilisation of BCVA was significant in all the patients in our cohort. Little demonstrated that 75% of patients after PRP maintained visual acuity of 20/100 and better after 5-12 years of observation, and as many as 60% of patients had visual acuity of 20/50 and better (10). In our cohort, 97% of patients retained BCVA of 20/100 and better, and 92% of patients BCVA of 20/50 and better. We recorded a deterioration of visual acuity in patients who at the outset had BCVA on the borderline of 0.3 in units of logMAR. A deterioration of vision by 3 and more rows occurred in 7 eyes (7.7%), in all cases this concerned patients in whom the pathology progressed and vitreous haemorrhage occurred. All this data is comparable with the values observed in the DRS study (21).
In our cohort, stabilisation of the clinical finding was achieved in all the observed eyes in the period of 6 months after the beginning of LPC. In the ETDRS study there was a progression to high risk PDR in eyes in which early full PRP was performed in 5-18% of cases after 3 years, and in 10-30% after 7 years of observation (4). In the DRS study, after 1 year of observation and following the performance of PRP, 78.8% of treated eyes were without neovascularisation (NV). NVD developed in 7.5% (3.8% mild NVD and 3.8% medium or severe NVD). In eyes with mild NVE there was a progression of NV in 22.8% of all treated eyes. In eyes with medium or severe NVE there was a progression in 16.6% of treated eyes. In eyes with mild NVD there was a progression in 19.8% of eyes (21). In long-term assessment, the clinical finding remained stable in 84.6% of patients in our cohort.
One of the fears upon performance of PRP treatment in one session is the quantity of energy supplied to the retina at once during a short treatment time, and the capacity of the retina to sustain this energy while retaining circulatory parameters, primarily within the region of the posterior pole of the retina. We may consider CRT to represent an indirect parameter of these relations. Muqit et al. in their cohort did not observe an increase of CRT after treatment in one session, by contrast this occurred after classic treatment performed in four sessions (12). We consider the above data to be comparable with our results. Yamakawa et al. (24) and Danielescu and Chiseliţă (3) reached a similar conclusion. On the contrary, Kim et al. recorded an increase in central retinal thickness 1 month after treatment, which then did not change during the observation period of 1 year (9). In the study by Oho et al., macular edema occurred in 11 eyes out of 129 following the performance of PRP in one session 1 month after the performance of the treatment, whilst 3 months after treatment macular edema spontaneously regressed in 5 of these 11 eyes (17). Nagpal et al. did not identify any change of central retinal thickness in their cohort following laser treatment (13). From the perspective of development of macular thickness after the performed treatments, we consider our results to be comparable with the studies published to date.
The complications that are described in the literature and which may have a correlation with aggressive conventional laser photocoagulation performed in a single session are choroidal ablation, ablation of the ciliary body, exudative retinal detachment or occlusion of the chamber angle. A rare complication observed after PRP performed in two sessions using a Pascal laser is central serous chorioretinopathy (25). Sheth et al. observed 2x retinal haemorrhage and 2x choroidal ablation in 666 PRP treatments performed using a Pascal system (17). Velez-Montoya et al. published data in which they retrospectively evaluated over 1301 laser procedures, in 2 eyes (0.17%) they observed choroidal ablation and in 1 eye (0.07%) serous retinal detachment, both complications corrected themselves spontaneously (23). A further complication they encountered was retinal haemorrhage (17 eyes, 1.3%). This complication was observed also by Modi et al. (11). In our cohort no complications of laser treatment were observed.
In the future we see potential for a comparison of the effectiveness of treatment of innovative types of lasers also with other therapeutic modalities, in particular in combination with anti-VEGF preparations administered intraocularly (14). New experiences demonstrate that the application of anti-VEGF agents separately or in combination with PRP has an unequivocally positive influence on eyes which are resistant or refractive to PRP, in aggressive forms of PDR or in newly diagnosed PDR (2, 20, 22).
CONCLUSIONS
The study presents a complex processing of the issue of laser photocoagulation with the use of technical innovations of lasers in a unique cohort of patients with diabetic retinopathy.
The performance of panretinal laser photocoagulation of the retina with the use of patterns and impulses of fundamentally shorter times during one to two therapeutic episodes in cases of severe advanced NPDR and PDR achieved both stabilisation of BCVA, and in 85% of eyes also stabilisation of the clinical finding. Change of BCVA after this intervention was insignificant during the observation period of 4-12 months. Central retinal thickness was stable during the observation, and no complications were observed.
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company.
MUDr. Alexandr Stepanov, Ph.D., FEBO
Oční klinika
Fakultní nemocnice Hradec Králové
Sokolská 581, 500 05 Hradec Králové
stepanov.doctor@gmail.com
Zdroje
1. Blumenkranz, M. S., Yellachich, D., Andersen, D. E., et al.: Semiautomated patterned scanning laser for retinal photocoagulation. Retina, 26(3); 2006 : 370–376.
2. Bressler, SB., Qin, H., Melia, M., et al.: Diabetic Retinopathy Clinical Research Network. Exploratory analysis of the effect of intravitreal ranibizumab or triamcinolone on worsening of diabetic retinopathy in a randomized clinical trial. JAMA Ophthalmol. 131(8); 2013 : 1033–40.
3. Danielescu, C., Chiseliţă, D.: Panretinal photocoagulation with or without focal photocoagulation - the effect on central retinal thickness. Oftalmologia, 54(2); 2010 : 99–103.
4. Early Treatment Diabetic Retinopathy Study Research Group. Early photocoagulation for diabetic retinopathy. ETDRS report number 9. Ophthalmology, 98(5); 1991b: 766–85.
5. Early Treatment Diabetic Retinopathy Study Research Group: Techniques for scatter and local photocoagulation treatment of diabetic retinopathy: Early Treatment Diabetic Retinopathy Study Report no. 3. Int Ophthalmol Clin, 27(4); 1987b: 54–264.
6. Early Treatment Diabetic Retinopathy Study Research Group: Treatment techniques and clinical guidelines for photocoagulation of diabetic macular edema: Early Treatment Diabetic Retinopathy Study Report Number 2. Ophthalmology, 94(7); 1987a: 761–774.
7. Jain, A., Blumenkranz, MS., Paulus, Y., et al.: Effect of pulse duration on size and character of the lesion in retinal photocoagulation. Arch Ophthalmol, 126(1); 2008 : 78-85.
8. Kalvodová, B., Sosna, T., Ernest, J., et al: Doporučené postupy pro diagnostiku a léčbu diabetické retinopatie. Čes. a slov. Oftal. 72(6); 2016 : 226–233.
9. Kim, J.J., Im, J.C., Shin, J.P., et al.: One-year follow-up of macular ganglion cell layer and peripapillary retinal nerve fibre layer thickness changes after panretinal photocoagulation. Br J Ophthalmol, 98(2); 2014 : 213–7.
10. Little, H. L.: Treatment of proliferative diabetic retinopathy. Long-term results of argon laser photocoagulation. Ophthalmology, 92(2); 1985 : 279–83.
11. Modi, D., Chiranand, P., Akduman, L.: Efficacy of patterned scan laser in treatment of macular edema and retinal neovascularization. Clin Ophthalmol, 3; 2009 : 465–70.
12. Muqit, M.M., Marcellino, G.R., Henson, D.B. et al.: Pascal panretinal laser ablation and regression analysis in proliferative diabetic retinopathy: Manchester Pascal Study Report 4. Eye (Lond), 25(11); 2011 : 1447–56.
13. Nagpal, M., Marlecha, S., Nagpal, K.: Comparison of laser photocoagulation for diabetic retinopathy using 532-nm standard laser versus multispot pattern scan laser. Retina, 30(3); 2010 : 452–8.
14. Nicholson, B.P., Schachat, A.P.: A review of clinical trials of anti-VEGF agents for diabetic retinopathy. Graefes Arch Clin Exp Ophthalmol, 248(7); 2010 : 915–30.
15. Oh, J.H., Kim, S.W., Kwon, S.S., et al.: The change of macular thickness following single-session pattern scan laser panretinal photocoagulation for diabetic retinopathy. Graefes Arch Clin Exp Ophthalmol, 253(1); 2015 : 57–63.
16. Palanker, D., Lavinsky, D., Blumenkranz, MS., et al.: The impact of pulse duration and burn grade on size of retinal photocoagulation lesion: implications for pattern density. Retina, 31(8); 2011 : 1664–9.
17. Sheth, S., Lanzetta, P., Veritti, D., et al.: Experience with the Pascal® photocoagulator: an analysis of over 1,200 laser procedures with regard to parameter refinement. Indian J Ophthalmol, 59(2); 2011 : 87–91.
18. Sosna, T. a kol: Diabetická retinopatie. Axonite, Praha, 2016, 280 p.
19. Sosna, T., Švancarová, R., Netuková, M., Studnička, J.: Současný pohled na diabetický makulární edém. Čes. a slov. Oftal. 68(3); 2012 : 91–97.
20. Studnička, J.: Aflibercept v léčbě diabetického makulárního edému, Čes. a slov. Oftal. 71(5); 2015 : 243–246.
21. The Diabetic Retinopathy Study Research Group. Design, methods, and baseline results. Diabetic Retinopathy Study (DRS) Report Number 6. Invest Ophthalmol Vis Sci, 2; 1981a: 210–226.
22. Tremolada, G., Del Turco, C., Lattanzio, R., et al.: The role of angiogenesis in the development of proliferative diabetic retinopathy: impact of intravitreal anti-VEGF treatment. Exp Diabetes Res, Epub 2012 : 728325; doi: 10.1155/2012/728325.
23. Velez-Montoya, R., Guerrero-Naranjo, J.L., Gonzalez-Mijares, C.C.: Pattern scan laser photocoagulation: safety and complications, experience after 1301 consecutive cases. Br J Ophthalmol, 94(6); 2010 : 720–4.
24. Yamakawa, M., Nozaki, M., Sato, R., et al.: Comparison of outcomes of conventional laser versus pascal laser for diabetic retinopathy. Nihon Ganka Gakkai Zasshi, 118(4); 2014 : 362–7.
25. Yang, H.S., Park, S.H.: Exacerbation of central serous chorioretinopathy following PASCAL photocoagulation. Can J Ophthalmol, 48(3); 2013: e 42–3.
Štítky
Oftalmológia
Článek Autorský rejstřík
Článok vyšiel v časopiseČeská a slovenská oftalmologie
Najčítanejšie tento týždeň
2017 Číslo 5-6- Dlouhodobé výsledky lokální léčby cyklosporinem A u těžkého syndromu suchého oka s 10letou dobou sledování
- Cyklosporin A v léčbě suchého oka − systematický přehled a metaanalýza
- Účinnost a bezpečnost 0,1% kationtové emulze cyklosporinu A v léčbě těžkého syndromu suchého oka − multicentrická randomizovaná studie
- Pomocné látky v roztoku latanoprostu bez konzervačních látek vyvolávají zánětlivou odpověď a cytotoxicitu u imortalizovaných lidských HCE-2 epitelových buněk rohovky
- Konzervační látka polyquaternium-1 zvyšuje cytotoxicitu a zánět spojený s NF-kappaB u epitelových buněk lidské rohovky
-
Všetky články tohto čísla
- OCT Findings and Long-term Follow-up Results of Vitrectomy in Patients with Optic Disc Pit and Associated Maculopathy
- PERSISTENT HYALOID ARTERY – PERFORM A SURGERY OR NOT?
- Combination of Intravitreal Corticosteroid with Anti-vegf in Macular Edema Secondary to Retinal Vein Occlusion
- Jubileum doc. MUDr. Šárky Pitrové, CSc., FEBO
- Sarkoidosis and its Eye Ocular Manifestation (an Analysis of Six Case Report)
- Results of Treatment of Diabetic Retinopathy by the Laser System PASCAL
- Ciliary body melanoma treatment by stereotactic radiosurgery
- The treatment results in patients with lmphoma disease in the orbit
- The Difference between Ganglion Cell Complex and Nerve Fiber Layer in the Same Altitudinal Halves of the Retina in Hyper-tension and Normal-tension Glaucomas
- Xerosis in Patient with Vitamin A Deficiency – a Case Report
- Recommended procedure for eye examination for infants and children of pre-school age in regular outpatient practice
- Autorský rejstřík
- Česká a slovenská oftalmologie
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Sarkoidosis and its Eye Ocular Manifestation (an Analysis of Six Case Report)
- Recommended procedure for eye examination for infants and children of pre-school age in regular outpatient practice
- PERSISTENT HYALOID ARTERY – PERFORM A SURGERY OR NOT?
- The treatment results in patients with lmphoma disease in the orbit
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy




