-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
The treatment results in patients with lmphoma disease in the orbit
Authors: A. Furdová; Andrea Marková; K. Kapitánová; P. Zahorjanová
Authors place of work: Klinika oftalmológie Lekárskej fakulty Univerzity Komenského a Univerzitná nemocnica, Nemocnica Ružinov, Bratislava, prednosta doc. MUDr. Krásnik Vladimír, PhD.
Published in the journal: Čes. a slov. Oftal., 73, 2017, No. 5-6, p. 211-217
Category: Původní práce
Summary
Introduction:
Lymphoma is a malignant disease that can affect several structures of the orbit and eye adnexa. In the area of orbit the non-Hodgkin‘s lymphoma (NHL) is typical, which may be indolent or aggressive. Indolent subtypes include MALT (mucosa-associated lymphoid tissue), follicular lymphoma (FL), lymphoplasmocytic lymphoma (LPL). Conversely, subtypes such as diffuse large cell lymphoma (DLBCL), mantle cell lymphoma (MCL) and Burkitt lymphoma (BL) are aggressive. The disease can be presented as primary or secondary malignancy of the orbit.Material and methods:
A group of 35 patients from the Department of Ophthalmology, Faculty of Medicine, Comenius University in Bratislava in the period from January 1 2009 to December 31 2016 with diagnosed non-Hodgkin‘s lymphoma located in the area of the orbit. For all patients, the generally valid diagnostic criteria for the NHL in the eye area were met.
We processed the first signs of disease, the proportion of women and men with NHL, the percentage of NHL types in the orbit area. Statistically, we evaluated the age at which NHL occurred in patients and evaluated the incidence of the disease over the reference period. We have statistically processed the forms of the applied therapy, their adverse effects, the recurrence of the disease, the presence of other malignancies in the lymphoma patient.Results:
Of the total number of NHL patients in orbit region 13 (37%) were male and 22 (63%) female. The overall mean age at which lymphoma was diagnosed was 60 years. Median for the total age of patients was 61. In women, a slightly higher average age and median was found. On the other hand, lower values of both parameters were present in men. The modus of both sexes was the same, 70 years.
We have seen various first symptoms in our group. We found that the most common symptom is red eye, and the rarest is the deterioration of the central visual acuity. The longest lasting symptom was swelling of eyelids (on average, up to 10 years) and the shortest described eye itching. Overall, the average duration of symptoms was 28 months, with a median of 13 months.
In our group of patients were 3 % of LPL, 6 % of Burkitt’s lymphoma, 6 % of FL, 8 % of MCL, 17 % of DLBCL, and 60 % of malignant lymphoma. MALT lymphoma occurred in 62 % in orbital and 38 % in conjunctival localization. In 2 patients with MALT lymphoma of the conjunctiva to start with systemic therapy wasn't neccessary.
In 21 patients with MALT lymphoma excisional biopsy or orbitotomy was the first step to diagnose lymphoma disease in 3 cases; in 18 patients the infiltration of the orbit or conjunctiva occured 1 to 3 years after primary diagnose of systemic lymphoma disease.
In general, NHL localization was 29 % in conjunctiva and 71 % in the orbital area. In 9 % of the orbital lymphoma, we observed lymphoma ingrowth to the conjunctiva. Systemic therapy was initiated in patients in II. stage and higher stage of the disease according to the Ann Arbor system. Totally 63 % of the group were treated by systemic therapy. Recurrence occurred in 5 patients, representing 14 % of the observed, but only in one patient with MALT lymphoma.
Preoperative and postoperative (excisional biopsy, orbitotomy) central visual acuity (CVA) stayed unchanged, postoperative swelling did not affect CVA, and CVA didn't change even during long-term follow-up.Conclusion:
Careful differential diagnosis determines the therapy of the disease, since the primary symptoms are usually nonspecific for ocular lymphoma. Significant factors for therapy include tumor grading and clinical staging by AJCC 2009 (American Joint Committee on Cancer, Chicago, Illinois). Correct evaluation of the symptoms is an important step to indicate excisional biopsy or orbitotomy: After histopathological results we can start adequate therapy in the cooperation with oncohematologist.Key words:
conjunctival tumors, orbit, lymfoma, orbitotomyINTRODUCTION
Lymphoma disease affecting the orbital region is a rare pathology, which in recent years has recorded an increasing incidence. It predominantly occurs in patients of more advanced age, but cases diagnosed in patients aged under 30 are not an exception. Lymphoma is a malignant disease which may affect several structures surrounding the orbit and eye adnexa.
In the area of the orbit the typical form is non-Hodgkin's lymphoma (NHL), which may be of an indolent or aggressive character. Indolent subtypes include MALT (mucosa-associated lymphoid tissue) lymphoma, follicular lymphoma (FL) and lymphoplasmocytic lymphoma (LPL). By contrast, subtypes such as diffuse large cell lymphoma (DLBCL), mantle cell lymphoma (MCL) and Burkitt's lymphoma (BL) are of an aggressive character. The disease can be presented as primary or secondary malignancy of the orbit (6).
We can observe manifestations of lymphoma disease also by the naked eye in the case of its localisation on the conjunctiva, or with the aid of imaging methods in the case of its location behind the eyeball (computer tomography – CT, magnetic resonance imaging – MRI). Especially important is differential diagnostics of red eye syndrome, from which the subsequent therapy of the disease is developed, since the initial symptoms are not generally specific to lymphoma disease. Significant factors for therapy are grading of the tumour and clinical staging according to AJCC 2010 (American Joint Committee on Cancer) (2). Correct evaluation of symptoms represents an important step towards determining the correct diagnosis and indication of adequate therapy.
AIM
The primary aim of the observation was to identify the first symptoms stated by patients, which were initially diagnosed and treated as red eye syndrome or edema of the eyelids. After unsuccessful therapy of these symptoms, the patients were sent to an ophthalmological outpatient clinic with suspicion of a tumorous pathology. We examined the frequency of occurrence of the individual symptoms and the period of their duration in the form of a questionnaire. We also focused on the characteristics of the pathology, determining the indication of therapy and subsequent results, as well as adverse effects of treatment.
MATERIAL AND METHODS
The analysis incorporated 35 patients with diagnosed non-Hodgkin's lymphoma in the region of the orbit, who were registered at the Department of Ophthalmology of the Faculty of Medicine, Comenius University and at the University Hospital in Bratislava, covering the period from 1 January 2009 to 31 December 2016. All patients met the generally valid diagnostic criteria for NHL in the orbital region.
We statistically processed the incidence of the first symptoms of the pathology, the proportion of men and women with NHL, the percentage share of types of NHL in the area of the orbit. We statistically evaluated the age at which NHL occurred in the patients and evaluated the incidence of the pathology within the observed period. We subsequently statistically processed the forms of applied therapy, their adverse effects, the incidence of recurrence of the disease and the presence of other malignancy in patients with lymphoma.
RESULTS
In the cohort of patients we recorded various initial symptoms, whose frequency of incidence and average duration is evaluated in the following graphs.
We determined that the symptom most frequently described by patients was red eye, and that the least commonly stated was deterioration of central visual acuity (graph 1). The longest persisting symptom was tumescence of the eyelids (on average as much as 10 years) and the shortest described symptom was a feeling of burning and stinging in the eyes. Overall the mean period of duration of complaints was 28 months, in which the median of this period was 13 months (graph 2).
Graph 1. Subjective symptoms described by patients (incidence of symptoms in cohort of patients in %) 
Graph 2. Average period of duration of complaints in patients before diagnosis of NHL, expressed in months 
The following appeared in the examined cohort of patients: 3% with LPL (lymphoplasmocytic lymphoma), 6% Burkitt's lymphoma, 6% FL, 8% MCL, 17% DLBCL. The most highly represented was MALT lymphoma, with 60% (graph 3). MALT lymphoma occurred in 62% in orbital and 38% in conjunctival localisation.
Graph 3. Proportion of types of B-NHL in cohort of 35 patients 
In general the representation of localisation of NHL was 29% in the conjunctiva and 71% in the orbital region (fig. 1). In 9% of orbital lymphomas we observed an outgrowth of the lymphoma into the conjunctiva.
Fig. 1. Typical image of infiltration of soft tissues of orbit upon lymphoma disease 
Of the total number of patients with NHL in the region of the orbit, 37% were men (13) and 63% were women (22). The total mean age at which lymphoma was diagnosed was 60 years. The median for the total age of patients was 61. In women a slightly higher mean and median age was determined, by contrast in men there were lower values of both parameters in comparison with the whole. The modus was equal in both sexes, 70 years (table 1).
Tab. 1. Age composition of patients with lymphoma disease 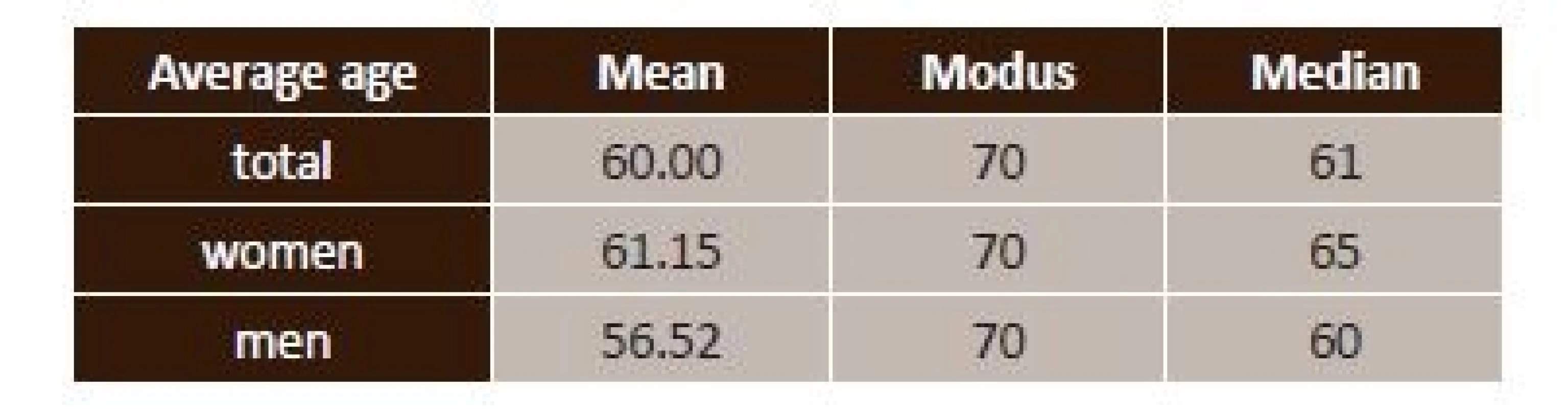
In the period of 2009-2012 we recorded a relatively low number of patients, approximately 1-2 per annum. The number of diagnosed patients significantly increased in 2013 and 2015 (graph 4).
Graph 4. Proportion of incidence of B-NHL in the region of the orbit in individual years 
The disease was confirmed in the observed cohort of patients on the basis of a histopathological examination from a biopsy or excision from the area of the conjunctiva, or following orbitotomy (fig. 2, 3).
Fig. 2. Patient after orbitotomy for lymphoma of the right orbit: a) third day after procedure, before removal of drain – 2014, b) clinical finding 9 months later – 2015, c) clinical find at follow-up examination – 2016 
Fig. 3. Patient with lymphoma of the orbit infiltrating the upper temporal quadrant of the conjunctiva and fornix: a) clinical picture before start of operation, b) perioperative visualisation of tumour deposit, c) deposit beneath tendon of superior oblique muscle, d) drain fitted before completion of procedure 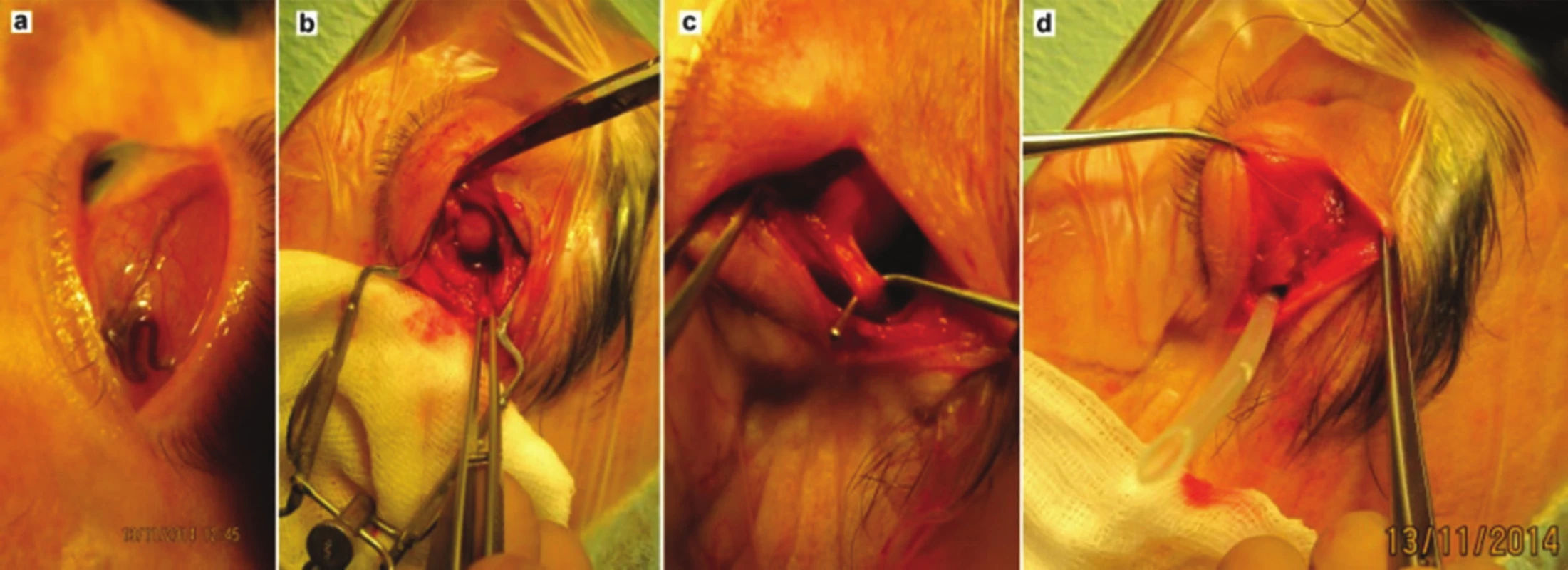
Systemic therapy was commenced in patients in the 2nd and higher stage of the disease according to the Ann Arbor system, and covered 63% of the total number of those treated (graph 5).
Graph 5. Representation of used forms of systemic therapy in cohort of 35 patients 
Radiotherapy of the orbital region was applied on all patients following orbitotomy. It was not indicated in any cases for patients with conjunctival infiltration.
Following the surgical procedure on the conjunctiva, patients described tension in the area of the original sutures. After orbitotomy, pseudoptosis of the upper eyelid and diplopia appeared in the first weeks after surgery (fig. 4).
Fig. 4. Clinical finding at follow-up examination: a) 2 weeks after removal of drain, b) 1 month after procedure, c) 2 months after procedure 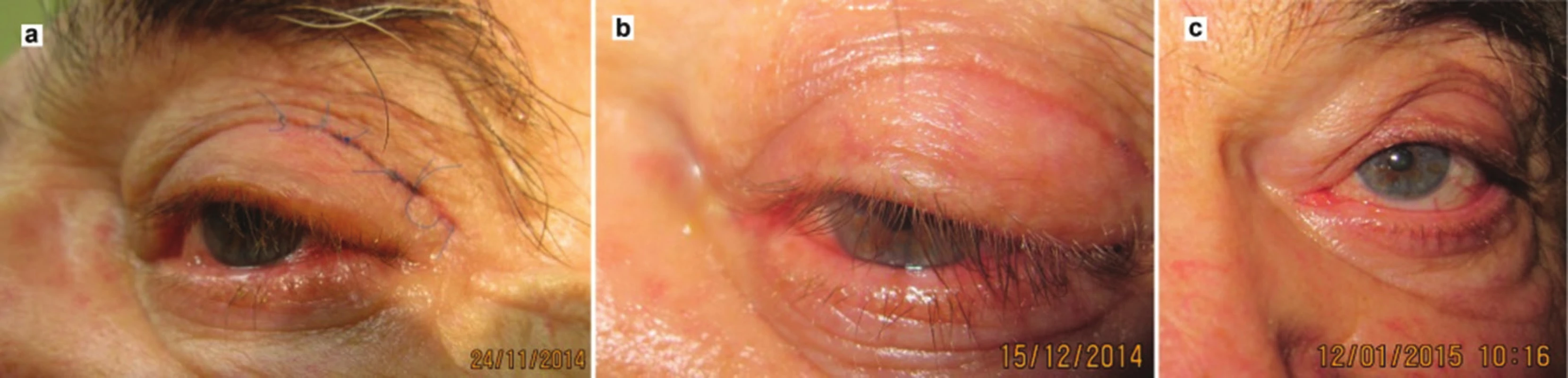
Adverse effects of radiotherapy of an acute character in the sense of post-radiation keratopathy and irritation of the eyeball were present in 1 case.
Recurrences occurred in 5 patients, which represents 14% of those observed (table 2).
Tab. 2. Number of recurrences depending on localisation according to type of lymphoma 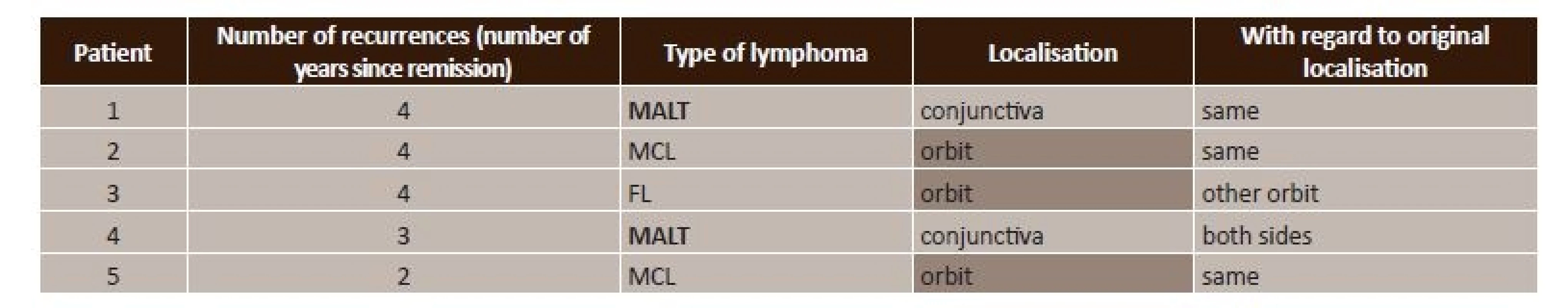
MALT – mucosa-associated lymphoid tissue lymphoma, FL – follicular lymphoma, MCL – mantle cell lymphoma The number of patients affected by autoimmune disorder in the cohort we observed was 2 with Sjögren's syndrome (SS) and 2 patients with rheumatoid arthritis (RA).
During the observed period, 5 patients died as a consequence of severe generalisation of lymphoma disease, their length of survival from the determination of the diagnosis to death was on average 2.4 years. In all patients this concerned secondary infiltration in the region of the orbit following prior treatment of lymphoma disease. Histopathologically this concerned MALT lymphoma in 4 patients and mantle cell lymphoma in 1 patient.
In our cohort we observed another malignancy than lymphoma in two patients (table 3).
Tab. 3. Other malignancies occurring in patients with lymphoma disease 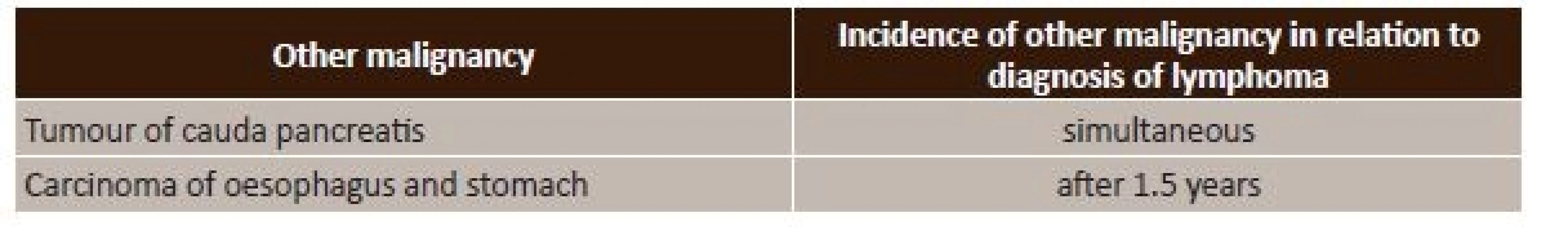
Central visual acuity in the patients before surgery (excision, orbitotomy) and after surgery at the first follow-up examination was unchanged. Neither the scope of infiltration of the orbit nor the surgical procedure had any influence on a change of CVA after surgery, even in long-term observation.
DISCUSSION
Diseases which belong among malignant lymphomas are characterised by diversity of the biological course and difference in therapeutic procedures for each nosological unit. The treatment of lymphoma in the orbital region consists of four main modalities, which are surgical intervention, radiotherapy, chemotherapy and immunotherapy. The choice of therapeutic method depends on the grading and staging of the pathology (1, 4, 5).
Surgical excision of lymphoma in the region of the orbit is a therapeutic and at the same time a diagnostic method. Surgical intervention in monotherapy is not demonstrated to be sufficient, since relapses of the disease frequently occur, the basis of which is a residue of tumour cells in the place of excision. As a consequence of this, e.g. upon lymphoma of the conjunctiva, mitomycin C is applied into the place of excision in the form of drops, which represents chemotherapy with an anti-proliferative effect on rapidly dividing residual tumour cells, which reduces the risk of potential relapse of the disease. In the case of orbital localisation of lymphoma, adjuvant radiotherapy is used with curative potential following the initial surgical intervention (6, 12).
Due to the localisation of the majority of lymphomas of the orbital region, radiotherapy is the regular and preferred therapeutic method, which is recommended for the treatment of the tumour pathology in stage IEA. The entire orbit must be covered within the radiation field, regardless of the degree to which the orbit is infiltrated. This procedure reduces the risk of relapse in places without infiltration. The curative dose for a low-grade tumour is 25-35 Gy, and for a high-grade tumour 30-40 Gy. Upon the use of doses higher than 35 Gy, severe complications such as cataract occur. This can be averted by shielding of the lens, but only in the case when the tumour is not within the envisaged shade (11, 12). In our cohort radiotherapy was indicated in all cases following orbitotomy.
We recorded adverse effects of radiotherapy (post-radiation keratopathy and irritation of the eyeball) in one case in our cohort.
Chemotherapy is usually reserved for tumours in stage II and higher, especially for stages III and IV. Commencement of chemotherapy is possible following a surgical procedure, in combination with radiotherapy or in the form of monotherapy. Chemotherapy applied separately or in combination with radiotherapy represents the therapeutic standard for lymphomas localised extraorbitally. The primary therapeutic modality for aggressive extranodal lymphomas is systemic therapy. Induction aggressive chemotherapy, followed by the transplantation of blood-forming stem cells has been examined in patients with MCL. Autologous or allogenic transplantation of stem cells may produce better results in achieving remission in the case of more aggressive lymphomas. Consultation with an oncologist is important here (3, 7, 8, 10). In our cohort systemic chemotherapy was indicated for 63% of patients.
Immunotherapy is used for tumours expressing a certain antigen, against which an antibody is directed in therapy. The treatment incorporates the use of the rituximab substance, which is used in the case of CD20 positive tumours such as MALT lymphoma. The main disadvantage of rituximab in monotherapy is frequent relapses. An auxiliary therapeutic regime has been added in order to avert relapses, planned for 2 years and administered every 2 months (10).
Similar procedures in therapy were used also on our patients, in which partial to total remission was achieved, depending on the histopathological type of tumour. The patients' condition was subsequently stabilised until it was symptom-free, although relapse occurred in 5 cases.
In foreign studies from 2011 and 2013, intralesionally applied injections of rituximab were demonstrated to be effective in the treatment of primary lymphoma in the area of the orbit. The usability of the given therapy appears to be promising for lesions localised in the anterior part of the orbit, by contrast in the case of lesions in the medial and posterior part of the orbit its effectiveness is lesser, inasmuch as the response is incomplete or completely absent. Treatment by intraorbital injection of rituximab is also a prospective option, thanks to the minimisation of systemic adverse effect in the form of application and the use of a low dose in comparison with high doses administered intravenously (8, 9).
Intralesional injection of rituximab did not take place in our cohort of patients, the standard intravenous form of the substance was applied.
CONCLUSION
In general lymphoma of the orbit is a rare disease, but within the given locality it represents the most common malignancy. The pathology especially affects women in advanced age.
Patients report to ophthalmologists due to persistent complaints of a non-specific character in the sense of red or dry eye, a feeling of a foreign body, diplopia and others. Diagnosis of the disease proceeds from non-invasive to invasive methods, which have a decisive position in determining the final diagnosis. The demand factor of performing differential diagnostics depends on the symptoms of the pathology which cause the patient to seek an ophthalmologist. After confirmation of lymphoma by histopathological examination of the tissue of the lesion by biopsy, it is possible to proceed to the selection of the therapeutic modality suitable for the given type of malignancy. Selection of the correct therapy is the basis of success and a good prognosis for the patient. Therapy is ordered on the basis of the properties of the given tumour, indicated by an onco-haematologist. Even primary orbital localisation of a lymphoma is a manifestation of a general pathology. As a result an ophthalmologist may be the first one to identify this pathology on the basis of correct recognition of the symptoms.
Non-Hodgkin's lymphoma in the region of the orbit is a treatable disease, but not all types are entirely curable. Patients may survive for many years with the given diagnosis following surgical and systemic therapy, and furthermore with good results of CVA.
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company.
Doc. Mgr. MUDr. Alena Furdová, PhD., MPH, FEBO
Klinika oftalmológie LFUK a UNB,
nemocnica Ružinov
Ružinovská 6, 826 06 Bratislava
e-mail: afrf@mail.t-com.sk, alikafurdova@gmail.com
tel: pracovisko +421 2 48234 kl. 607
Zdroje
1. Dunleavy, K. et al.: Low-intensity therapy in adults with Burkitt’s lymphoma. The New England Journal of Medicine. 2013-11-14, vol. 369, no. 20, p. 1915–1925. DOI: 10.1056/NEJMoa1308392.
2. Edge, S. B., Compton, C. C.: The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Annals of Surgical Oncology. 2010-06, vol. 17, no. 6, p. 1471–1474. DOI: 10.1245/s10434-010-0985-4.
3. Giuliari, G. P. et al.: Orbital Burkitt’s Lymphoma: An Aggressive Presentation. Case Reports in Ophthalmological Medicine. 2012, vol. 2012, p. 354043. DOI: 10.1155/2012/354043.
4. Kafková, A.: Folikulový lymfóm. Via practica. 2008, vol. 5, no. 12, p. 514–518.
5. Menon-Mehta, S.: Ocular Lymphoma. Medscape. 2008. URL <http://emedicine.medscape.com/article/1219134-overview>.
6. Mohan, H.: Patológia. 1. Balneotherma, 2011. 976 p. ISBN: 978-80-970156-6-4.
7. Saunders, T. S. et al.: Systemic non-Hodgkin’s lymphoma involving the orbit and leptomeninges. Digital Journal of Ophthalmology. 2010-07-29, vol. 16, no. 3, p. 9–12. DOI: 10.5693/djo.02.2010.06.001.
8. Savino, G. et al.: Evaluation of intraorbital injection of rituximab for treatment of primary ocular adnexal lymphoma: a pilot study. Cancer Science. 2011-08, vol. 102, no. 8, p. 1565–1567. DOI: 10.1111/j.1349-7006.2011.01976.x.
9. Savino, G. et al.: Long-term outcomes of primary ocular adnexal lymphoma treatment with intraorbital rituximab injections. Journal of Cancer Research and Clinical Oncology. 2013-07, vol. 139, no. 7, p. 1251–1255. DOI: 10.1007/s00432-013-1438-9.
10. Sharma, T., Kamath, M.: Diagnosis and Management of Orbital Lymphoma. EyeNet Magazine (American Academy of Ophthalmology). 2015, vol. 6. URL <https://www.aao.org/eyenet/article/diagnosis-management-of-orbital-lymphoma>.
11. Tzekov, C. et al. [Orbital lymphoma]. Khirurgiia. 2009, no. 4–5, p. 19–23.
12. Yahalom, J. et al. Modern radiation therapy for extranodal lymphomas: field and dose guidelines from the International Lymphoma Radiation Oncology Group. International Journal of Radiation Oncology, Biology, Physics. 2015-05-01, vol. 92, no. 1, p. 11–31. DOI: 10.1016/j.ijrobp.2015.01.009.
Štítky
Oftalmológia
Článek Autorský rejstřík
Článok vyšiel v časopiseČeská a slovenská oftalmologie
Najčítanejšie tento týždeň
2017 Číslo 5-6- Cyklosporin A v léčbě suchého oka − systematický přehled a metaanalýza
- Dlouhodobé výsledky lokální léčby cyklosporinem A u těžkého syndromu suchého oka s 10letou dobou sledování
- Účinnost a bezpečnost 0,1% kationtové emulze cyklosporinu A v léčbě těžkého syndromu suchého oka − multicentrická randomizovaná studie
- Pomocné látky v roztoku latanoprostu bez konzervačních látek vyvolávají zánětlivou odpověď a cytotoxicitu u imortalizovaných lidských HCE-2 epitelových buněk rohovky
- Konzervační látka polyquaternium-1 zvyšuje cytotoxicitu a zánět spojený s NF-kappaB u epitelových buněk lidské rohovky
-
Všetky články tohto čísla
- OCT Findings and Long-term Follow-up Results of Vitrectomy in Patients with Optic Disc Pit and Associated Maculopathy
- PERSISTENT HYALOID ARTERY – PERFORM A SURGERY OR NOT?
- Combination of Intravitreal Corticosteroid with Anti-vegf in Macular Edema Secondary to Retinal Vein Occlusion
- Jubileum doc. MUDr. Šárky Pitrové, CSc., FEBO
- Sarkoidosis and its Eye Ocular Manifestation (an Analysis of Six Case Report)
- Results of Treatment of Diabetic Retinopathy by the Laser System PASCAL
- Ciliary body melanoma treatment by stereotactic radiosurgery
- The treatment results in patients with lmphoma disease in the orbit
- The Difference between Ganglion Cell Complex and Nerve Fiber Layer in the Same Altitudinal Halves of the Retina in Hyper-tension and Normal-tension Glaucomas
- Xerosis in Patient with Vitamin A Deficiency – a Case Report
- Recommended procedure for eye examination for infants and children of pre-school age in regular outpatient practice
- Autorský rejstřík
- Česká a slovenská oftalmologie
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Sarkoidosis and its Eye Ocular Manifestation (an Analysis of Six Case Report)
- Recommended procedure for eye examination for infants and children of pre-school age in regular outpatient practice
- PERSISTENT HYALOID ARTERY – PERFORM A SURGERY OR NOT?
- The treatment results in patients with lmphoma disease in the orbit
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy




