-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Vertical Strabismus – Indication of Surgical Techniques on the Inferior Rectus Muscle
Authors: J. Krásný
Authors place of work: Oční klinika FN Královské Vinohrady, Praha, přednosta: doc. MUDr. P. Studený, PhD, MHA
Published in the journal: Čes. a slov. Oftal., 74, 2018, No. 4, p. 132-139
Category: Původní práce
doi: https://doi.org/10.31348/2018/1/2-4-2018Summary
Aid:
Familiarize themselves with the operating techniques in their own modulation to solve hypotropic states with elevation or hypotropic states with depression.
Methods:
Surgery technique “cul-de-sac” is a procedure with fixed adjustable sutures (non-absorbable suture), which are guided in parallel on both peaks original insertion of inferior rectus muscle. The node itself of suture is done in cutting the muscle and through the original insertion only leads arc suture. During „counterclockwise transposition“ procedure sec. Knapp, the horizontal rectus muscles are fixed at the straight inferior rectus muscle level. The author included their graphical diagrams.
Material:
At the Department of Ophthalmology in the Faculty Hospital Královské Vinohrady in Prague (Czech Republic, EU) in the years 1996 - 2014 a release relaxing operation of the inferior rectus musle by the technique “cul-de-sac” on 49 eyes. Indication was double elevator palsy in 31 patients, congenital fibrosis of the extraocular muscles in 15 patients and in 3 cases, it was thyroid eye disease. “Counterclockwise transposition” procedure sec. Knapp was indicated twice for paresis of the inferior rectus muscle in 2015 and 2016. For the first time, it was a congenital form. It was detected histologically atrophy of stripped muscle with hypertrophy collagen. The second traumatic form was formed after an orbital injury.
Results:
We provided adequate relaxation of the inferior rectus muscle and practical restoration of eye elevation by the technique “cul-de-sac“ in 18 preschool children with the double elevator palsy and three adult patients with thyreiod eye disease. We had to restore motility to complete the procedure by classical transposition procedure sec. Knapp of both horizontal rectus muscles to the direct superior rectus muscle in elderly children and adults with the double elevator palsy, as well as in all patients with the congenital fibrosis of the extraocular muscles. Indicate the inclusion of this transposition influenced the degree of fibrotic rectus inferior muscle given by age. “Counterclockwise transposition“ procedure sec. Knapp ensured the practical disappearance hypertropie in both cases of paresis of the inferior rectus muscle. The alignment of the position of the eyes without diplopia in the direct view was ensured by prismatic correction.
Conclusions:
To release the fibrotically altered inferior rectus muscle in the double elevator palsy, the congenital fibrosis of the extraocular muscles and the thyroid eye disease, the operation of adjustable sutures was necessary in accordance with our experience with the technigue “cul-de-sac“ in its own modification. The transposition procedure sec. Knapp, either classical or “”counterclockwise” “ in its own modification, was of paramount importance for the solution of the vertical deviation of a paretic ethiology.
Key words:
adjustable sutures, congenital fibrosis of the extraocular muscles, double elevator palsy, thyroid eye disease, transposition procedure sec. Knapp, vertical strabismus
INTRODUCTION
Vertical strabismus has many clinical pictures and manifestations, vertical deviations are also a component of palsies of the cranial nerves controlling motility of the eyes. Surgical solution is generally not simple, combining a range of operating techniques. In this report we wish to focus on surgical techniques on the inferior rectus muscle, through which it is possible to influence the disorder of elevation and depression of the eye in certain diagnoses, also on the basis of an analysis of previous experiences.
METHOD
Cul-de-sac surgical technique (Fig 1 and 2) – own modification
After spraying the conjunctiva in the lower quadrants of the bulbar conjunctiva with BSS solution, we make an incision of 3-4 mm from the limbus in the shape of an isosceles trapezoid. We insert temporary fixation sutures into the peak of the folded lobe, serving for good orientation in the operating field by folding the bulbar conjunctiva, and at the conclusion of the operation for optimal fixing of the conjunctiva upon its closure. We do not loosen the inferior rectus muscle in its entirety in order to protect the Lockwood ligament. We only place a Daviel spoon beneath the tendon, which enables us to perform precise insertion of sutures made of the non-absorbable suturing material Ethibond 5-0. The sutures are fixed from both edges of the tendon up to 1/8 of its width. We then relax the muscle with a fastened suture by cutting off close to the sclera, up to a maximum of 1/6 of the width of the tendon from both sides, the central part remains firmly fixed in approx. 2/3 of the width of the tendon. We subsequently stitch the original tendon in such a manner that we form a loop of the suture above it, and the suture is then again drawn into the offcut section of the tendon. We repeat this procedure also on the other side. Upon drawing up to the original tendon we measure the loop in calculated mm, in which 1 mm corresponds to 3 pdpt. In this manner we dose the procedure, mostly the indication is within the range of 6 to 8 mm, maximally 9 mm. We firmly knot in the original fixation, also bilaterally. After carefully cutting off the muscle in the central part of the original tendon, the muscle is loosened in depth on this pair of sutures also with the capsules of the Tenon's membrane. Spontaneous movement is aided by the fibrotic property of this muscle within the framework of the basic diagnoses, which enables its fixing at the given distance, and the non-absorbable material of the suture prevents its “slippage” into the depth of the orbit. We close the conjunctiva with two submerged sutures made of the absorbable material Vicryl 7-0.
Fig. 1. Cul-de-sac surgical technique: insertion of Daviel spoon (A), insertion of sutures made of Ethibond 5-0 (B), cutting off of muscle with sutures in close proximity to sclera (C), back stitching into original tendon (D) 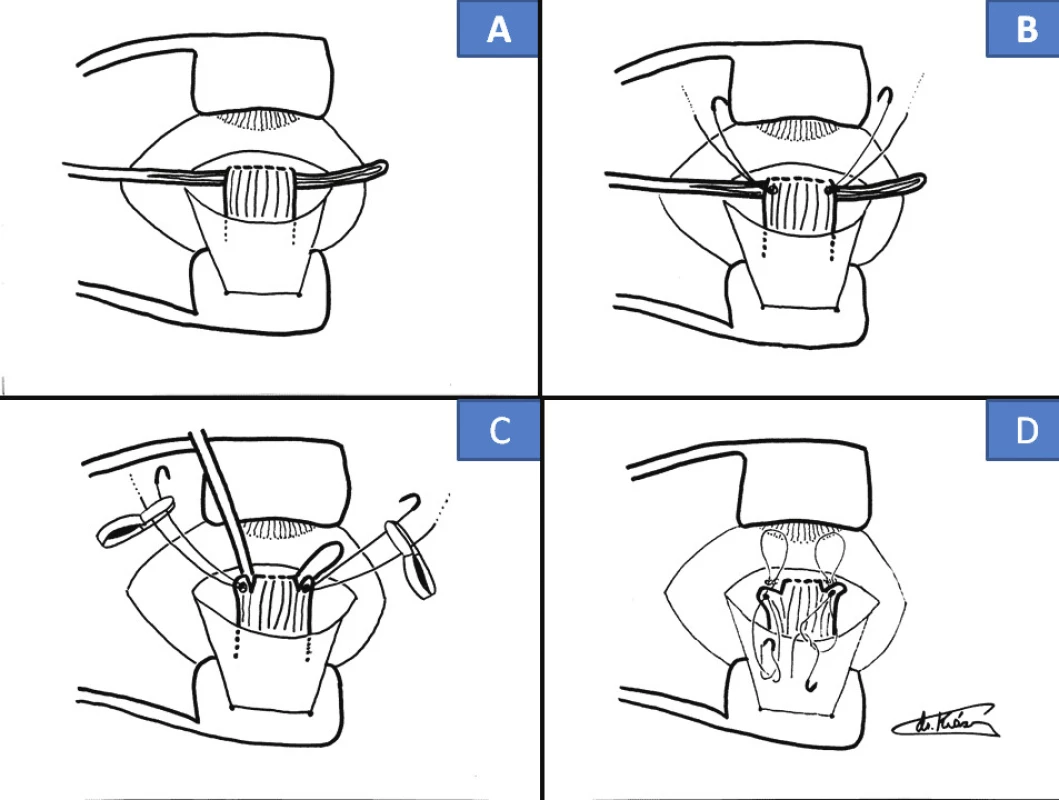
Fig. 2. Cul-de-sac surgical technique: drawing of suture into offcut tendon (E), measurement of loop of suture, fixation thereof (F), cutting off of central part of tendon (G), spontaneous loosening of muscle (H) 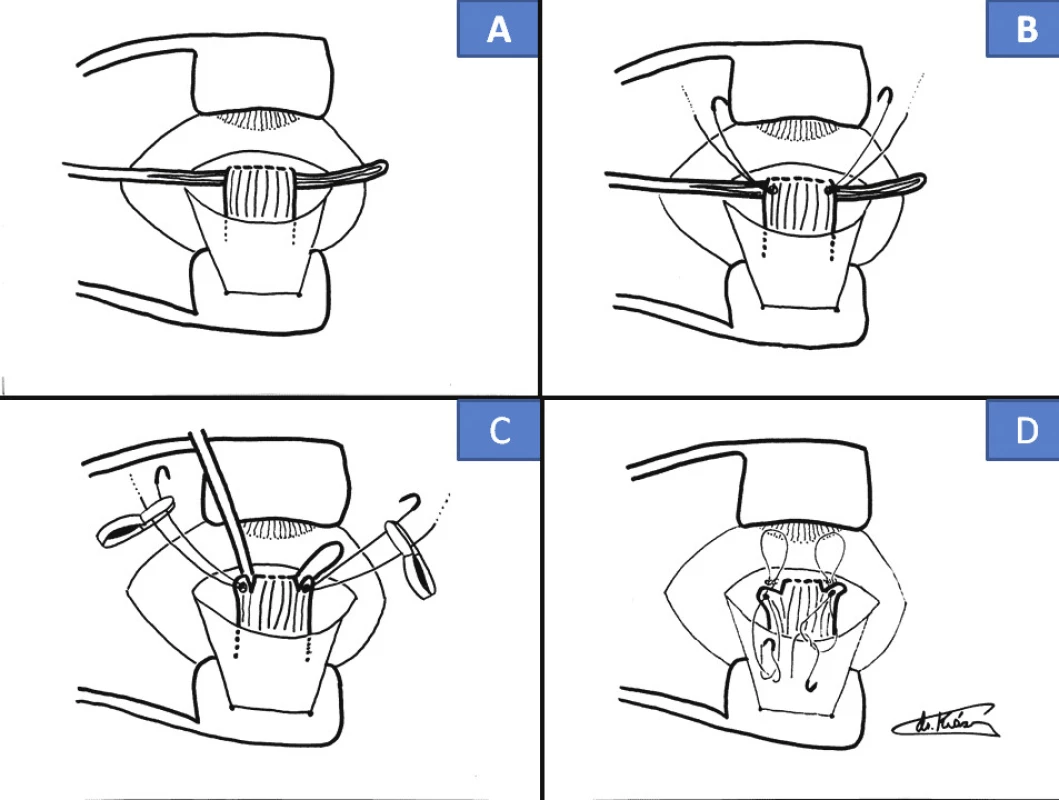
Fig. 3. Surgical technique of “anticlockwise” transposition according to Knapp procedure: scope of incision of bulbar conjunctiva (A), fixation of sutures and cutting off of horizontal rectus muscles (B), fixation of horizontal rectus muscle by tendon of inferior rectus muscle (C), fixing of both horizontal rectus muscles on level of tendon of inferior rectus muscle (D) 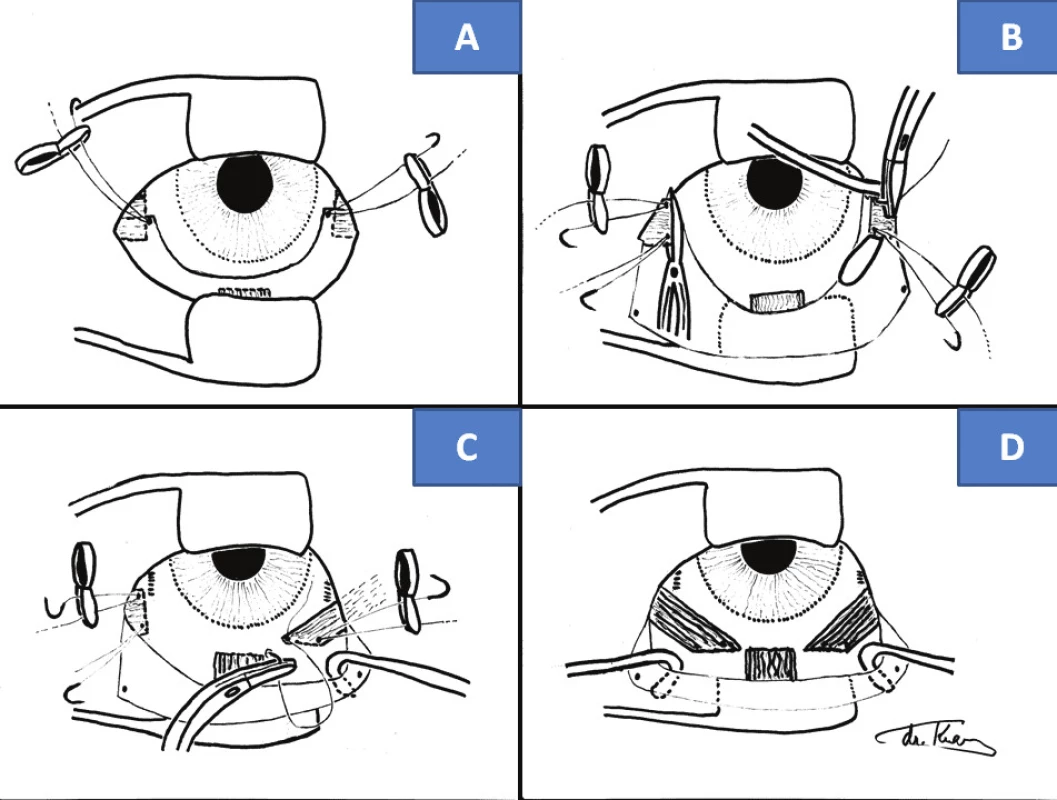
Fig. 4. 3-year-old boy with left-sided elevator palsy: elevation defect in left eye (A), with hypotropia on same side before cul-de-sac operation (B), and bilateral loose elevation (C), with parallel position of eyes two years after surgery (D) 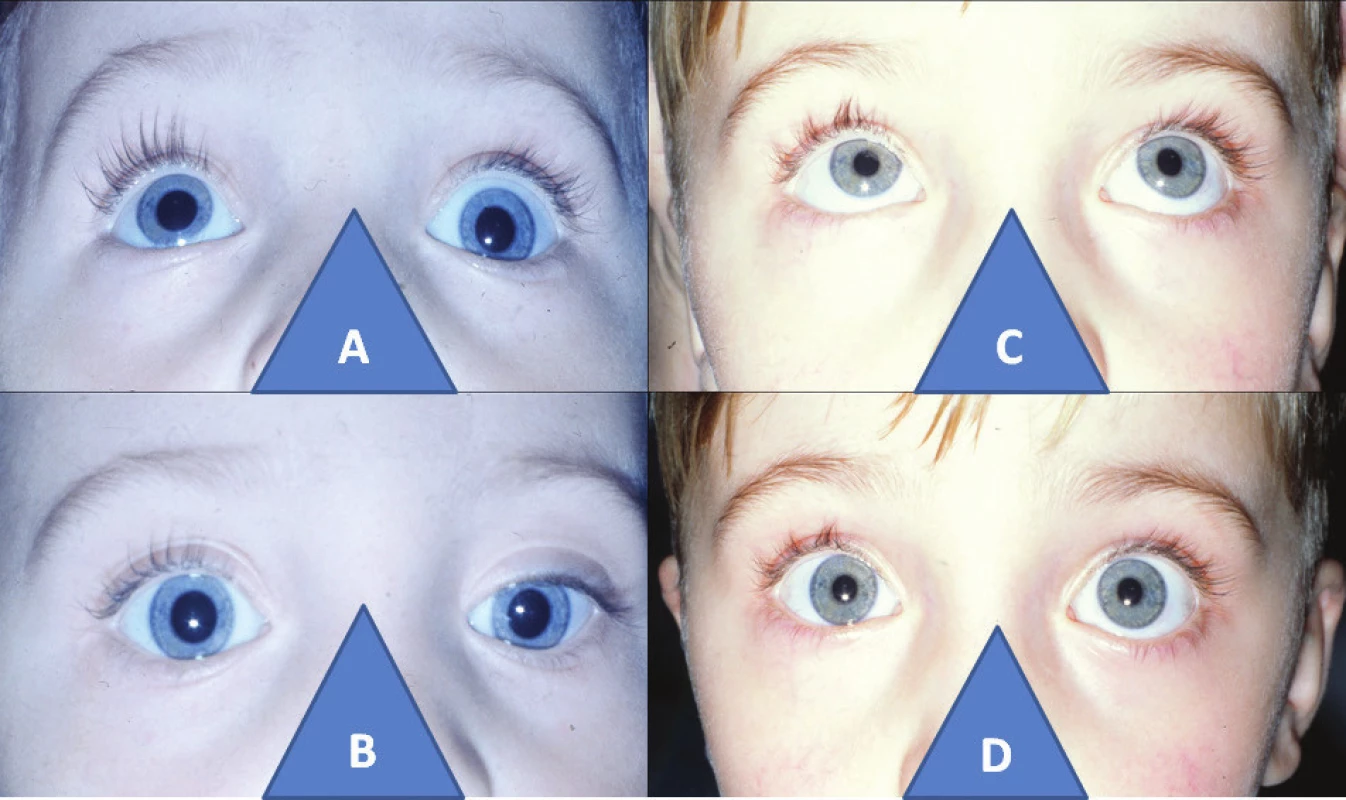
Fig. 5. 11-year-old girl with right-sided congenital fibrosis of extraocular muscles: closed ocular aperture in right eye (A), hypotropia in right eye with passive opening of ocular aperture (B), zero ability to open ocular aperture in right eye upon attempt at elevation (C), position of upper eyelid and eyeball in right eye four years after comprehensive triple surgical procedure according to cul-de-sac, Knapp procedure, according to Fox (D) 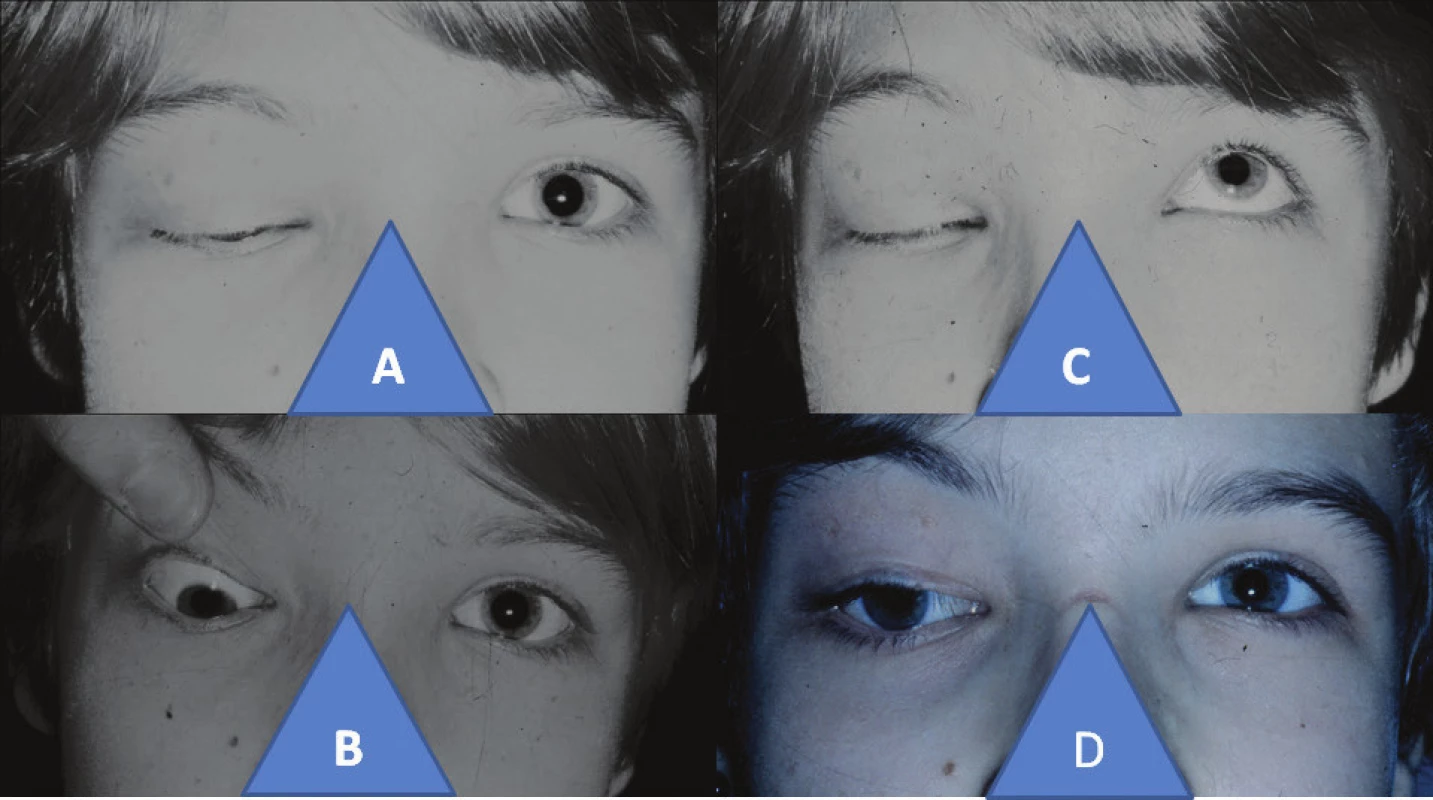
Surgical technique of anticlockwise transposition according to Knapp procedure (Fig. 3) – own modification
After spraying the conjunctiva in both lower quadrants of the bulbar conjunctiva with BSS solution, we make an incision of 3-4 mm from the limbus in the shape of an arc, reaching up to the area before the tendons of the horizontal rectus muscles. There follows a horizontal incision at both ends in the direction above the tendons of these muscles. We then insert temporary fixation sutures into the created peaks of the folded lobe, serving for good orientation in the operating field by folding the bulbar conjunctiva, and at the conclusion of the operation for optimal fixing of the conjunctiva upon its closure. We do not release the inferior rectus muscle in order to protect the Lockwood ligament, and that is why we do not put a hook under the tendon. We prepare the tendons of both horizontal muscles on a hook by the classic method as in their retropositioning, with analogous insertion of Vicryl 6-0 sutures. We cut off the muscles fixed to the sutures, and subsequently stitch them to the sclera by the tendon of the inferior rectus muscle. We first of all, we fix their lower edges 1-2 mm from the relevant edge of this muscle on the same level. We anchor the upper edges of the horizontal muscles peripherally in the horizontal axis via the peak of the tendon of the inferior rectus muscle. We close the conjunctiva with two sutures in the peaks and a further two to three between them with the absorbable suturing material Vicryl 6-0, always by submerged sutures, in order to preserve the continuity of the bulbar conjunctiva.
Own cohort (material)
We used the cul-de-sac surgical technique to relax the inferior rectus muscle in three indications: dual elevator palsy, endocrine orbitopathy and congenital fibrosis of the extraocular muscles.
In the period from 1996-2014 we indicated for surgery 49 eyes of children, youth and adult patients aged from 3 to 47 years, median age 15.5 years. In 18 patients of predominantly pre-school age we used surgery separately in unilateral elevator palsy (Fig. 4).
We also operated on 3 adult patients with endocrine orbitopathy, whose clinical picture included hypotropia due to traction of the inferior rectus muscle. In the remaining 28 eyes with dual elevator palsy we were necessitated to combine the loosening of the inferior rectus muscle with transposition of both superior rectus muscles according to the Knapp procedure. This concerned older children and adults in 13 eyes with dual elevator palsy and 15 operations on eyes of patients with congenital fibrosis of the extraocular muscles in all age groups.
In the case of congenital fibrosis of the extraocular muscles we always supplemented the comprehensive surgical procedure with a suspension operation of ptosis according to Fox (Fig. 5).
We have indicated the surgical technique of anticlockwise Knapp transposition procedure only twice to date, detailed case reports are provided for an analysis of the issue in question.
Case report 1 (Fig. 6)
In May 2011 a three-year-old boy was admitted with a working diagnosis of congenital right-sided strabismus sursoadductorius, weakening the rectus medialis and inferior rectus muscles.
The anamnestic data confirmed a finding of non-inflammatory affliction from birth and injury to the given orbital region. Within the framework of co-operation it was possible only to determine pronounced right-sided sursumadduction (approx. +12 DP and 10 DP hypertropia). We indicated elongation according to Gonin-Hollwich on the rectus medialis muscle of 5 mm, and partial triple myotomy of the inferior rectus muscle by electrocautery according to Romero-Martinez. He was subsequently monitored and in 2013, thus at the age of four years, the boy slightly inclined his head toward the left shoulder. Upon fixation LE, RE was in approx. 30 pdpt hypertropia and indicated microesotropia, in dissociation up to +6 pdpt. In elevation RE was pronouncedly higher, whereas depression was lacking. Examination on a troposcope was not performed due to lack of co-operation, and it was therefore not possible to determine the version component of the deviation. Stereoscope: suppressed perception of RE, without stereopsis according to Randot, VRE 0.8 nat., VLE 1.0 nat. We considered alternating sursumduction or palsy n.IV in the right eye, but the Bielschowsky test was negative. In February 2016 we first decided to use the technique of transposition of both horizontal rectus muscles to the tendon of the inferior rectus muscle. During the operation we detected hypertrophic granulation tissue by the tendon of the inferior rectus muscle, which created an image similar to a double head of the muscle (Fig. 7A). We removed this pathological tissue.
A histological examination detected scarry changes to the fragment of the skeletal muscle, surrounded by a relatively thick layer of dense ligament without manifest inflammatory cellularisation and neovascularisation. The morphological picture corresponded to hyperplastic scarry changes, the etiogenesis of which cannot be unequivocally determined retrospectively from the morphology alone.
After surgery the condition was stabilised, the positioning of the head was aligned, and hypertropia of 6 pdpt persisted with microexotropia – 8 pdpt only in distance vision, which was accented to V-syndrome in elevation. Depression was not restored. Stereoscope demonstrated alternation of perception, but the finding on Randot persisted, therefore still without stereopsis. Prisms were applied which aligned the vertical deviation. VRE 0.9 with 6 pD ax. 270 DP and VLE 1.0 with 6 pD ax. 90 DP. The finding was stable also 3 years later, at the age of 9 years.
Fig. 6. 6-year-old boy with congenital palsy of the inferior rectus muscle in the right eye: increase of elevation in right eye (A), hypertropia in right eye (B), incapacity of depression in right eye (C), practically aligned elevation after surgery with subsequent V-syndrome (D), practically parallel positioning of eyes after surgery (E), finding is identical also three years after surgery (F) 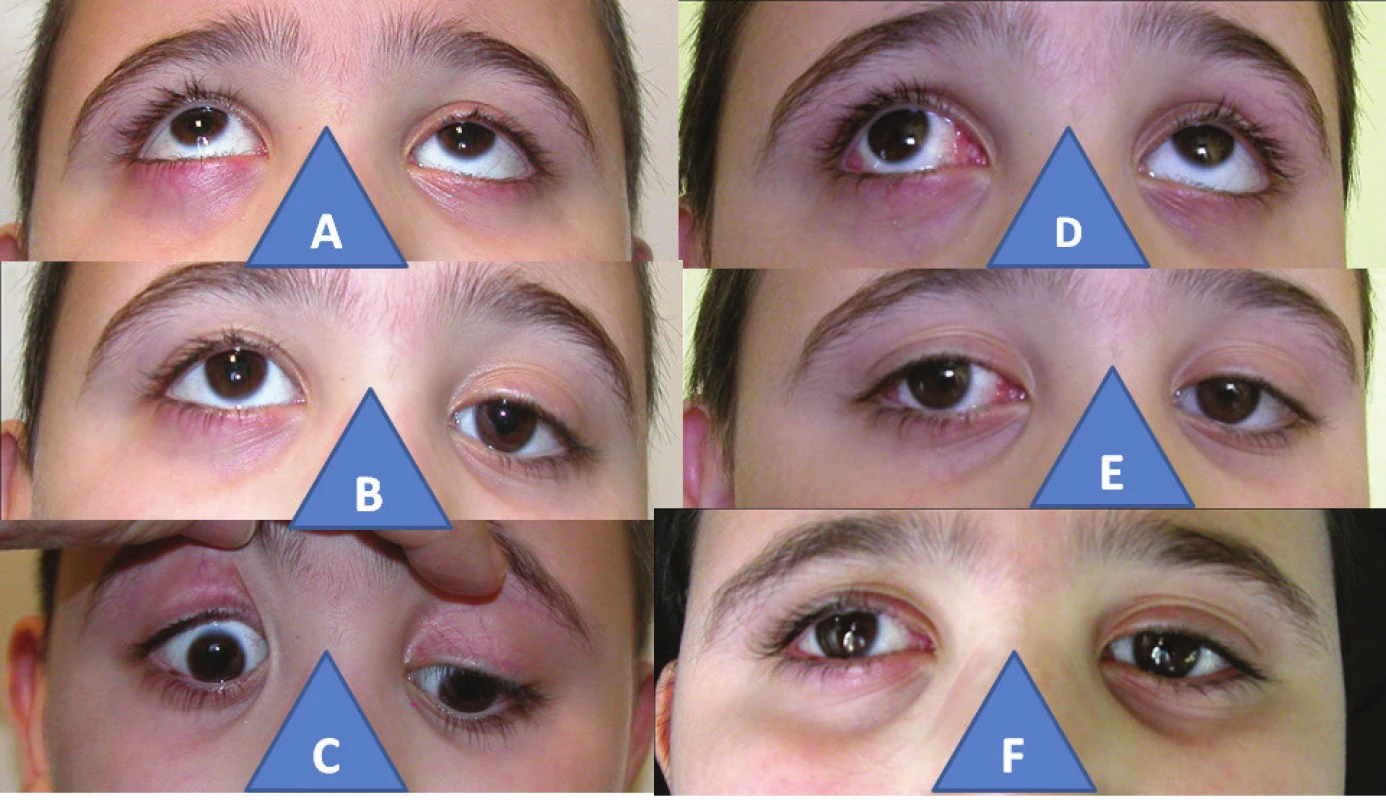
Fig. 7. Diagnostic balance sheet in palsies of inferior rectus muscle: hypertrophic pathological tissue by tendon of inferior rectus muscle – arrow (A), finding on Hess screen – right-sided hypertropia and secondary hypotropia on double surface on left. 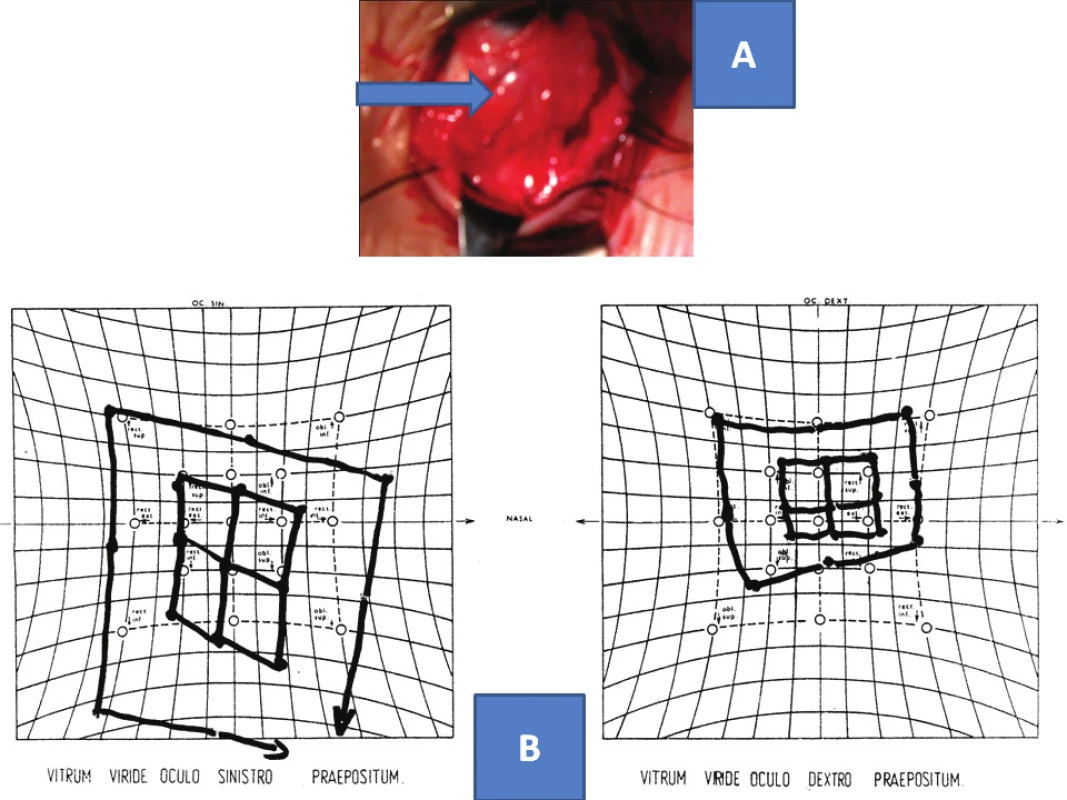
Fig. 8. 67-year-old man with post-traumatic palsy of inferior rectus muscle in right eye: increased elevation in right eye (A), hypetropia in right eye (B), zero depression in right eye (C), normalisation of elevation after surgery (D), parallel position of eyes after surgery (E), only indication of depression after surgery in right eye (F) 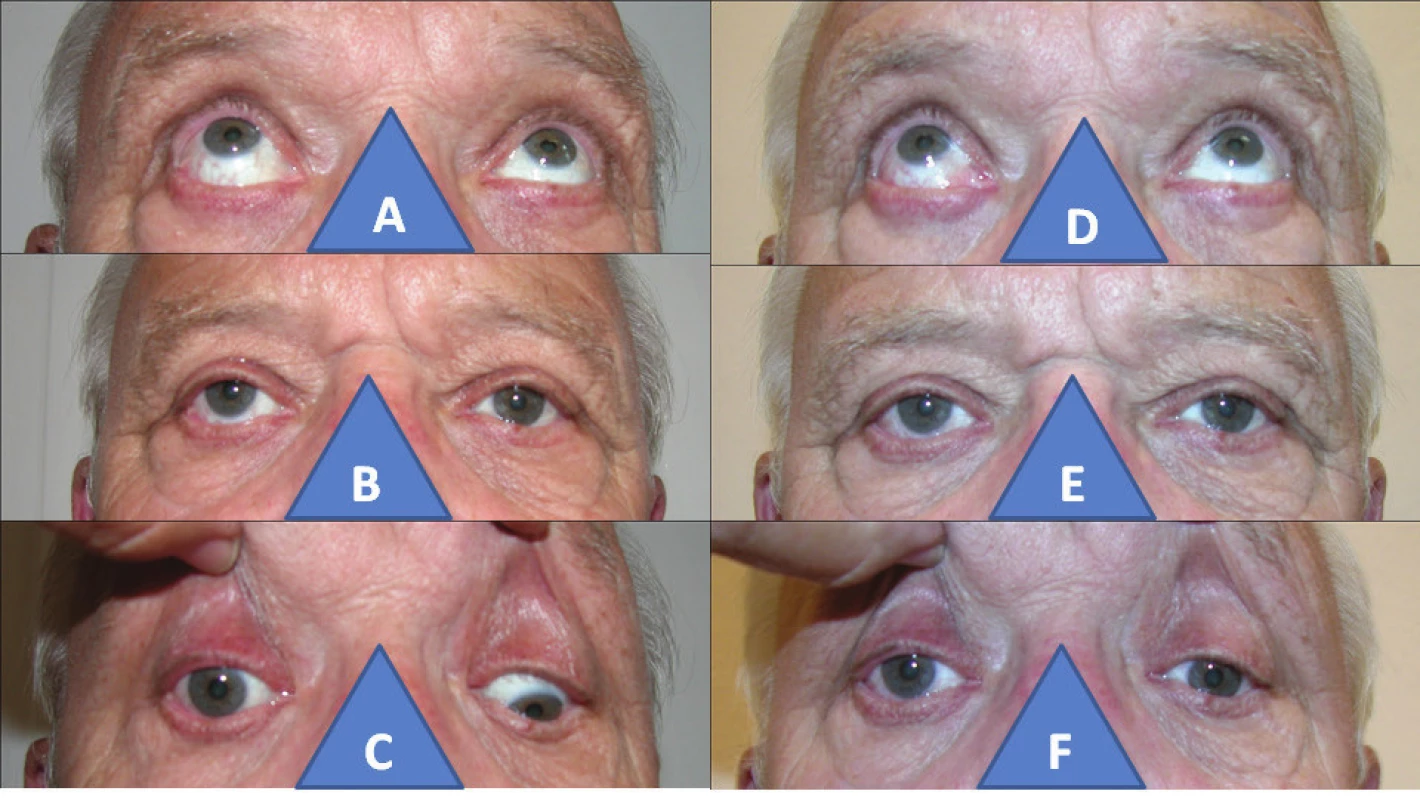
Case report no. 2
In May 2017 we performed the above-stated transposition a second time on a 67-year-old man due to mechanical strabismus in the right eye on the background of the consequences of an injury to the orbit, in which the inferior rectus muscle was torn. At another clinical centre the condition of vertical diplopia was resolved by retropositioning of the superior rectus muscle. Slanting vertical diplopia was stated, fixed permanently by LE, RE from above 8 – 12 pdpt and by convergent micro-movement, in motility RE was pronouncedly higher in elevation, and depression was entirely lacking. Troposcope: obj. angle +3 DP and 4 DP hypertropia RE without torsional component. An orthoptic analysis on Worth four light test, Bagolini striated glasses test and stereoscope confirmed vertical diplopia, and Randot did not confirm stereopsis. Hess screen (Fig. 7 B) demonstrated primary hypertropia with microesotropia in right eye, with smallest squares of both depressors, secondarily left-sided hypotropia of opposite direction with at least double surface. VRE 0.7 with +1.0/+1.0 ax. 160 DP and VLE 1.0 with +1.25/-0.5 ax. 95 DP, prismatic correction did not help. After surgery the condition was adjusted to parallel position without diplopia, but only in direct upward gaze with prismatic correction. VRE 0.8 with +2.0/1.0 ax. 65 with 7 pD ax. 265 DP and RLE 1.0 with +1.0/-0.5 ax. 95 with 8 pD ax. 165 DP. In motility now without hypertropia and depression only slightly improved. In October the same year retinal complications appeared in diagnosis: Foramen maculae lutae, in which we could not exclude the possibility that this condition was a late complication of contusion of the eye within the framework of orbital trauma. Pars plana vitrectomy was performed at our centre. In March 2018, six months after posterior segment surgery, VRE was 0.5-0.66 with the given correction, prismatic correction has absolutely no effect, since the image is undulating due to the loss of photoreceptors.
RESULTS
A highly satisfactory result of the “cul-de-sac” surgical technique was achieved in three adult patients with endocrine orbitopathy, in which the positioning of the eyeballs was aligned in parallel position, and elevation was also practically restored. In the case of elevator palsy it applied that the earlier the age of indication, the more optimal the result, meaning that the elevation defect was conditional primarily upon the block of the inferior rectus muscle and not yet complete affliction of the elevators. This condition pointed to the important function of the inferior rectus muscle, or rather its fibrotic state due to the development within the age factor, which makes a comprehensive contribution to the condition of elevator palsy. As a result we did not need to proceed with a supplementary procedure of Knapp transposition surgery, which applied always for children of pre-school age. In schoolchildren and adults this transposition always restored elevation within a varying scope. In the case of congenital fibrosis of the extraocular muscles, an optimum result was evaluated as restoration of practical alignment of the position of the eyes in the vertical axis, and position of the head without inclining backward in bilateral forms, adjustment of elevation above the horizontal plane even despite the fact that the use of classic transposition operation of the horizontal rectus muscles according to the Knapp procedure was incomplete, since the eyeball minimally drew over the medium line in the horizontal plane.
It is not possible to make a precise and conclusive evaluation of the “anticlockwise” Knapp procedure in a mere two operations, but the positioning of the eyes in the horizontal axis was practically aligned, and pathological elevation was markedly reduced, even if not completely eliminated.
CONCLUSION
The loosening of a fibrotically altered inferior rectus muscle in the case of dual elevator palsy, congenital fibrosis of the extraocular muscles and endocrine orbitopathy required essential surgery using adjustable sutures, according to our experience by the cul-de-sac technique in our own modification. The condition of the inferior rectus muscle determined the supplementary indication of classic transposition technique according to the Knapp procedure.
A Knapp transposition procedure was of fundamental significance for resolving vertical deviation of palsy origin, either classic or “anticlockwise” in our own modification. Both newly introduced surgical techniques extend the range of possible surgical procedures for strabismus.
DISCUSSION
The first mentions of a surgical solution of vertical strabismus in Czechoslovak ophthalmology appeared at the end of the 1950s and beginning of the 1960s (25), before the introduction of transposition surgery according to the Knapp procedure and surgical techniques using adjustable sutures. It was not until the new millennium that vertical strabismus once again became the subject of interest of ophthalmologists within our region, as an issue of resolving dissociated vertical deviation (DVD) (23), which is also the content of a number of paediatric ophthalmological Czech-Slovak discussions, with outputs in supplements of Folia strabologica et neurophthalmologica (5, 24, 30, 32).
Vertical strabismus in its clinical picture has vertical deviations of varying scope and character, which can be divided into three groups and two separate units. The congenital forms cover unilateral and bilateral palsy of the superior oblique muscle on the basis of congenital palsy of the n. trochlearis, as well as dual elevator palsy and palsy of the inferior oblique muscle, which is considered in differential diagnosis with Brown syndrome. Congenital structural changes are also the cause of Brown syndrome, congenital fibrosis of the extraocular muscles, a rare condition is secondary vertical deviation in Duane syndrome, as is the absence of the inferior rectus muscle, which must however be demonstrated on MR. The acquired form of vertical strabismus may be manifested as Brown syndrome or palsy of the superior oblique muscle, and contributes to inflammatory processes in the orbit and palsy of the inferior rectus muscle following orbital trauma. Separate conditions are DVD and hyperfunction of the inferior rectus muscle (IOOA) (1). Vertical deviations conditioned by affliction of the individual oblique muscles are manifested only in the direction of their function. The full extent of affliction of vertical strabismus in all directions of gazes upon elevation or depression pertains to the image of DVD, dual elevator palsy or congenital fibrosis of the extraocular muscles (7, 38), as well as palsy of the inferior rectus muscle on the basis of traumatic affliction (35). The congenital form of palsy of the inferior rectus muscle which we observed, manifested by hypertropia and defect of depression of the eye, is an entirely rare condition, as attested to by the fact that it was not included in the detailed analysis of the above-stated total of 17 vertical deviations (1). Modern extensive foreign monographs also do not mention the condition (7, 38). In addition, the eighteen year old Czech analysis of strabismus operations did not confirm this diagnosis in a total of 2248 operated eyes (14). A mention of the condition, including a proposal for a surgical solution, can be found in the as yet unsurpassed Czech monograph by Dr. Divišová et al. (3), which became the inspiration for our surgical approach. Histological verification confirmed hypertrophic scarry changes to the skeletal muscle in a younger patient (case report 1) (19), in contrast with scarry changes three years after strabismus surgery using the hang-back technique (at another centre), which were manifested by fascicularly aligned collagen ligament without muscle tissue, with slight vascularisation and cellularisation (16). Changes to the structure of the muscle were therefore long-term, and it was not possible to exclude a congenital background. The second of our observations (case report no. 2) concerned post-traumatic unilateral hypertropia with depression disorder and vertical diplopia in connection with post-traumatic damage to the inferior rectus muscle, and is described upon loss, laceration or denervation of this muscle (35), or as its possible post-traumatic palsy (1). This was confirmed by the finding on a Hess screen, primary hypertropia of the afflicted eye with secondary other-sided hypotropia on a larger surface. Depression disorder is further described in posterior fracture of the orbit and myasthenia. Elevation disorder is also linked with endocrine orbitopathy, blow-out fracture and also myasthenia (35).
DVD represents the most common hyperdeviation in children, and its theory is by and large obscure (6). It is necessary to differentiate DVD from IOOA. DVD is of supranuclear origin, and has a concomitant relationship, whereas IOOA is of nuclear origin with an incomitant relationship. DVD was formerly also referred to as alternating sursumduction or dissociated vertical divergence (3), and we may encounter this term in the literature to this day (6). DVD is characterised by spontaneous relaxation of the eye in an upward direction upon covering, and upon fatigue or inattention binocular functions are disrupted. Following repeated fixing the eye returns back to position, secondary deviation is in the same direction (3). The depressed eye is suppressed, thereby averting diplopia (3, 6, 36). IOOA is manifested by increased elevation only in adduction, and is generally present in V-pattern strabismus, which is manifested by hypofunction of the antagonistically acting superior oblique muscle. Both of these clinical units are linked with congenital esotropia and may be mutually combined (34). A highly effective method of limiting DVD is anteriorisation of the inferior oblique muscle. This procedure was first used at the end of the 1980s (20), and is currently used for congenital esotropia and exotropia, in which a prerequisite is co-participation of hyperfunction of this muscle (39). It concerns retropositioning of the muscle by 8-14 mm and antepositioning of the tendon toward the temporal edge of the inferior rectus muscle according to professor Fink (3). This surgical technique substantially strengthens convergent movement, which may be a disadvantage upon residual esotropia. Between 1998 and 2002, 100 eyes were treated for DVD at a clinic in Bratislava. The most frequently used procedure was retropositioning of the superior rectus muscle and anterior transposition of the inferior oblique muscle, or anteriorisation. In total the success rate was evaluated at 75% (5). Out of a total number of 934 vertical deviations in the period from 1985 to 2001, DVD comprised 29% and IOOA 31% (1). Authors from Brno in a number of studies state always a total of 82 eyes operated on for DVD, frequently also connected with IOOA. For comparison they used two surgical techniques of anteriorisation of the inferior oblique muscle and its myectomy (24, 30, 32, 33). Overall they demonstrated the same effectiveness of both surgical techniques, and demonstrated a difference between preoperative and postoperative deviation, the dosing of anteriorisation was more precise and the incidence of secondary IOOA less common in comparison with myectomy (34). Upon solution of DVD we unequivocally preferred procedures on the inferior oblique muscle. Upon solution of congenital esotropia with presence of hyperfunction of the inferior oblique muscle, we weakened the rectus medialis muscles by dosable elongation according to Gonin-Hollwich, in combination with triple partial myotomy of the inferior oblique muscle by electrocautery according to Romero-Martinez under one anaesthesia in 115 eyes out of a total number of 211 operations of strabismus sursoadductorius (12), which blocked the advancement of DVD or it substantial weakening. We have long-term excellent experience with this procedure, since it has no influence on convergence, and furthermore the principle is denervation of the muscle, by which its cyclic component remains extorsion (15). For this reason we applied it also in IOOA, which was manifested more pronouncedly only after surgery for congenital esotropia on a further 96 eyes (12).
Dual elevator paresis is a congenital unilateral disorder, with accompanying paralysis of the superior rectus and inferior oblique muscle in one eye. The terminological synonym of this condition is monocular elevation deficiency (MED) (7). Etiologically it is considered that dual elevator paresis is in fact conditioned only by long-term palsy of the inferior rectus muscle (35), which was confirmed by our analysis of used surgical techniques depending on age, therefore a thus influenced development of changes to the inferior rectus muscle in the sense of progressive fibrotisation. The cause may also be supranuclear paralysis on the basis of retarded automatic and reflexive movements and findings on EMG (22). Patients incline the head backward in an attempt to attain binocular vision. The eyeball does not cross the central line in the attempt at elevation, but Bell's phenomenon is retained, and the upper eyelid has a normal function. Pseudoptosis appears, in which the width of the ocular aperture corresponds to hypotropia of the eye. Retraction of the upper eyelid appears upon the attempt at elevation. Upon undertaking fixation by the paretic eye, a pronounced secondary deviation turned upward is manifested, with eventual limitation of the Bell's phenomenon (22, 23).
Congenital fibrosis of the extraocular muscles is more commonly bilateral than unilateral. It is also indicated as congenital stationary external ophthalmoplegia always in bilateral form on a background of autosomal heredity. It combines elevator palsy, distinguished by hypotropia with excessive convergence and ptosis with a flattened orbitopalpebral fold, and also generally involves hypomimia (23). In the English speaking literature it is abbreviated as CFOEM (29).
The basic choice of surgical procedure is loosening of the inferior rectus muscle, which may be fibrotically altered. The technique of “adjustable sutures” is recommended for vertical strabismus in endocrine orbitopathy (26, 38) or in elevatory palsy (11, 38), and also for overcoming ectasia of the sclera or silicone implants in external operations for retinal detachment (2, 38). Paretic strabismus has also been an indication for this surgical technique: palsy n. IV has been addressed by loosening of the other-sided inferior rectus muscle. Weakening of the inferior rectus muscle has been indicated in Duane syndrome and palsy of n. VI. following Jensen's transposition procedure (4).
“Adjustable sutures” operations were first independently described by Scott (27) and Rosenbaum (26) in 1977. In these operations the sutures were guided through the centre of the tendon at a distance of 2 mm, and fixed here beneath the conjunctiva (4). The development of this surgical technique is also connected with the name of professor Nelson in 1982 in the form of the cul-de-sac technique with parallel sutures guided above the conjunctiva, which enabled later postoperative handling (21). We adjusted our surgical technique in comparison with the classic method (21) in the following details: we used non-absorbable suturing material, and above all we did not fix the sutures via the conjunctiva, but by contrast in the loosened muscle, which enabled the original tendon to remain without a knot. The fundamental conformity was in the parallel guiding of the sutures on the edge of the tendon, guaranteeing the full development of the new tendon. In this the surgical procedure differs significantly from the “hang-back” technique implemented later (38), in which the sutures are guided in the centre of the original tendon, where they are fixed via the conjunctiva, which enables postoperative adjustment. The suspension of the muscle is established via this triangle, and this subsequently increases the contact of the muscle with the sclera, and a flat surface of the new tendon (16). The author of this technique started out from his previous surgical technique of an adjustable suture, using a tractional subconjunctival suture with free adjustability. It was resolved in the fornix of the conjunctiva, which generated a minimal scarry reaction for the patient's comfort after surgery (37). The problem of operating with or without adjustable suture was addressed also in a study on strabismus surgery for endocrine orbitopathy, with confirmation of the advantage of non-absorbable suturing material in comparison with absorbable material (9). We have used this material from the beginning of the introduction of the cul-de-sac technique. We have not confirmed the advantage of freely adjustable sutures in comparison with fixed adjustable sutures (9). On the contrary, the cul-de-sac technique in our modification enables precise dosing of the operation according to the measured deviation, and furthermore develops the new tendon well. The comparison in both studies rests upon small numbers of patients (9, 13), from which it is not possible to draw definitive conclusions due to the possibility of error of small numbers, which does not enable statistical processing.
A Brazilian study evaluated surgery using “freely adjustable” sutures using classic techniques on groups of one hundred cohorts, in comparison with retropositioning and myectomy (“non-adjustable”) for concomitant horizontal strabismus. One week after surgery the effectiveness of adjustable sutures was 90% for esotropia and exotropia, in comparison with 60% for esotropia and only 50% for exotropia in the case of the non-adjustable procedure. One month after surgery both surgical procedures had a success rate of 60% for esotropia, but in exotropia a better result persisted in the case of adjustable sutures, also 60% as against 50% upon the use of the classic procedure. Three months after surgery both procedures were similarly effective for exotropia at almost 50%, whereas in for esotropia the position had improved to 70% in the case of retropositioning or myectomy, while in the case of adjustable sutures the condition did not improve or deteriorate, remaining at 60% (31). This confirms the previous opinion of the authors of the Czech monograph that it is necessary to wait three months for a definitive evaluation of the result of operations on horizontal muscles (3).
After the loosening of the inferior rectus muscle, after an interval there follows the second phase of the surgical procedure to improve elevation of the eye. A 50-year-old surgical procedure was introduced by Knapp (9). The brilliance of the idea consists in the mechanical transfer of the function of both horizontal muscles following the separation from their original insertion and suturing onto each side of the insertion of the paretic superior rectus muscle, as can be seen on the simple diagrams of the basic monographs (3, 8, 35). The function of the horizontal muscles on this axis remains fully preserved by this method. The operation leads to an up to 19 degree correction of the vertical muscle in primary position, and enables 25-45 degrees of mobility in the field of maximum action of the paralysed muscle (10). A detailed description of this surgical technique can be found in basic atlases of strabismus surgery from world leading strabologists (8, 35).
From the perspective of the surgical tonic component of strabismus, in which there is an important contribution of the mechanical role of the muscle and ligament component (Demer, 2007) and the pulley of the extraocular muscles (Miler, 1989) (6), surgery according to the Knapp procedure in both the classic and anticlockwise form is a strengthening operation. The tonic fibres have a fundamental influence here, since the rolling curve of contact is extended. It is necessary to be aware that professor Knapp was not thinking along these lines. The proposed surgical procedure was based on his anatomical knowledge of the anatomy of the orbit. The position of the eyeball within the framework of these transposition operations under general anaesthesia does not change. The position of the eye is adjusted only after the restoration of the tonic component of the muscles following the subsidence of anaesthesia. The tonic component of the heterotropic deviation is more dynamic, e.g. it disappears under general anaesthesia (6), which also applies to unconsciousness on all skeletal muscles. The Faden operation described by Cüpres in 1974 as an alternative weakening operation has the opposite effect. As a consequence of reducing the rolling curve of contact it limits the tonic component, if fixation of the muscle is located in the curve of contact (6).
We did not use the second phase of the surgical procedure for dual elevator palsy in young patients, since fibrosis of the inferior rectus muscle was not of primary importance, but in older children and adults this was essential. Transposition according to the Knapp procedure was necessary in all cases of congenital fibrosis of the extraocular muscles in our patients, regardless of age, together with surgery for ptosis as the third phase of the comprehensive surgical procedure. We resolved drooping of the eyelid with absent function of lifting with the aid of frontotarsal suspension according to Fox, for which preparation of allogenic deeply frozen fascia was developed (16). We have twenty years' successful experience with this surgical procedure; in only 2 patients out of a total number of 124 it was necessary to perform re-operation again with the aid of fascia due to the biodegradation of the implanted material, or in 18 of the patients the procedure was supplemented by tarsosection according to the Fasanella-Servat procedure, predominantly in the case of unilateral congenital fibrosis of the extraocular muscles (17).
“Anticlockwise” transposition of the horizontal muscles according to the Knapp procedure was our own modification of the classic technique. We have not found any observations on this in the available literature (PubMed), and it has not been stated even in the extensive atlases of strabological operations (8, 35). We resolved to perform the procedure after a long period of deliberation, since we had not found any other optimum solution for the condition of hypertropia with restriction of depression. The result documented an improvement of the position and adjustment of the motility of the afflicted eye.
The author of the study declares that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company.
Thanks to Dr. Josef Šach for enabling the publication of the result of the histological examination, which was the content of another of our joint reports in Folia strabologica et neuroophthalmologica.
Presented at the 13th Symposium of Paediatric Ophthalmology in Luhačovice (2017) and the 6th Trends in Paediatric Ophthalmology and Strabology in Litomyšl (2018).
Devoted to the memory of Dr. Lada Hromádková (21.12.1932 – 26.12.2017), co-author of the monograph The Golden Era of Czech Strabology.
Received: 20. 4. 2018
Accepted: 5. 9. 2018
Available online: 18. 3. 2019
MUDr. Jan Krásný
Oční klinika FN Královské Vinohrady
100 34 Praha 10
Zdroje
1. Autrata, R., Unčovská, Hromádková, L. et al.: Vertical deviation in children. Folia strabologica et neuroophthalmologica, 5; 2002 suppl. I.: 39–44.
2. Chang, JH., Hutchinson, AK., Zhang, M. et al.: Strabismus surgery outcomes after scleral bucking procedures for retinal reattachment. Strabismus, 21; 2013 : 235 - 241
3. Divišová, G. et al.: Strabismus, Avicenum, Praha, 1979, 306 p.
4. Docherty, PTC.: Paralytic strabismus correction by adjustable suture technique, Br J Ophtalmol, 68; 1984 : 353 – 359.
5. Dostálek, M., Krejčířová, I.: Chirurgické tonické složky strabismu – teoretické aspekty. Folia strabologica et neuroophthalmologica, 17; 2016 suppl. I.: 35.
6. Fišerová, O.:Disociovaná vertikalna divergencia – charakteristika a liecba. Folia strabologica et neuroophthalmologica, 6; 2003, suppl. I.: 45–47.
7. Gerinec, A.: Detská oftalmológia, Osveta, Martin, 2005, s. 157–196.
8. Helveston, EM.: Surgical Management of Strabismus, 4th ed., St. Louis, Mosby, 1993, 395 p.
9. Karhanová, M., Vláčil, O., Šín, M. et al.: Srovnání metody nastavitelných stehů versus fixační stehy při operaci strabismu u pacientů s endokrinní orbitopatií. Ces Slov Oftal, 68; 2012 : 207–213.
10. Knapp, P.:Vertical transposition of the horizontal rectus musles for the elimination of vertical strabismus, Trans Am Ophthalmol, 67; 1969 : 304–323.
11. Keech, RV., Heckert, RR.: Adjustable suture strabismus surgery for acquired vertical deviation. J Pediatr Ophtalmol Strabismus, 25; 1988 : 159–164.
12. Krásný, J.: Strabismus sursoabductorius (v kontextu osmnáctiletého rozboru strabismu). Ces Slov Oftal, 71; 2015 : 267–277.
13. Krásný, J.: Vertikální strabismus I: Operační technika cul-de-sac. Folia strabologica et neuroophthalmologica, 18; 2017 suppl. I.: 102–104.
14. Krásný J., Brunnerová, R.: Strabismus – konzervativní postupy a chirurgické metodiky. In Rozsíval, P. (ed.) : Trendy v oftalmologii, sv. 6., Galén, 2010, 56–98.
15. Krásný, J., Kubištová, V.: Trojitá parciální myotomie dolního šikmého svalu. Posouzení s retropozicí a volnou myectomií. Cs Oftal, 48; 1992 : 186–190.
16. Krásný, J., Měřička, P.: Možnosti řešení ptózy v dětství a dospělosti. Ces Slov Oftal, 55; 1999 : 145–155.
17. Krásný, J., Měřička, P.: Dvě desetiletí zkušeností s využitím hluboce zmražené fascie u operace neurogenních ptóz v rámci neurooftalmologických diagnóz. Folia strabologica et neuroophthalmologica, 15; 2014, suppl. I.: 45–47.
18. Krásný, J., Šach, J.: Klinicko-patologický stav po operaci „nastavitelnými stehy“. Folia strabologica et neuroophthalmologica, 17; 2016: suppl. I.: 51–53.
19. Krásný, J., Šach, J.: Vertikální strabismus II: Operační technika protisměrné Knappovy transpozice. Folia strabologica et neuroophthalmologica, 19; 2018, suppl. I.: 61–63.
20. Mims, J.L., Wood, R.C.: Bilateral anterior transposition of inferior oblique muscle. Arch Ophthalmol, 107; 1989 : 41 – 44.
21. Nelson, LB., Calhoun, JH., Harley, RD. et al.: Cul-de-sac approach to adjustable strabismus surgery. Arch Ophthalmol, 100; 1982 : 1305–1307.
22. Otradovec, J., Vacek, J.: Jednostranná supranukleární obrna elevátorů. Cs Oftal, 31; 1975 : 241 252
23. Otradovec, J.. Klinická neurooftalmologie. Grada, Praha, 2003, 487 p.
24. Pellarová, H., Autrata, R., Uničovská et. al..: Výsledky operací vertikálních deviací. Folia strabologica et neuroophthalmologica, 13; 2012, suppl. I.: 126–128.
25. Pur, S., Pištělka, Z.: Výsledky chirurgické úpravy vertikálních heterotropií. Cs Oftal, 18; 1962 : 107–111.
26. Rosenbaum, AK., Metz, HS., Carlson, M. et al.: Adjustable rectus muscle recession surgery. Arch Ophthalmol, 95; 1977 : 817–820.
27. Scott, WE., Martin-Casals, A., Jackson, OB.: Adjustables sutures in strabismus surgery. J Pediatr Ophthalmol Strabismus, 14; 1977 : 71–75.
28. Sprague, CE., Moseley, MJ., Fielder, AR. et al.: Dissociated vertical deviation treatment with the Faden-operation of Cuppers. Arch Ophthalmol, 98; 1980 : 465–468.
29. Tawfik, HA., Rashad, MS.: Surgical management of hypotropia in congenital fibrosis of extraocular muscles presented by pseudoptosis. Clin Ophthalmol, 7; 2013 : 1 – .
30. Varadyová, B., Pellarová, H., Autrata, R. et al.: Výsledky operací vertikálních deviací. Folia strabologica et neuroophthalmologica, 14; 2013, suppl. I.: 88–91.
31. Vasconcelos, GC., de Almeida, HC. : Adjustable versus non-adjustables suture technique for concomitant horizontal strabismus: a comparative study. Arq Bras Oftalmol, 78, 2015 : 1–7 .
32. Vodičková, K., Autrata, R., Řehůřek, J.: Anterior transposition and myectomy of the inferior oblique muscle in vertical deviations – long term results. Folia strabologica et neuroophthalmologica, 8; 2007, suppl. I.: 38–41.
33. Vodičková, K., Autrata, R., Řehůřek, J.: Dlouhodobé výsledky anteriorizace a myectomie dolního šikmého svalu u vertikálních deviací. Ces Slov Oftal, 64; 2008 : 157–160.
34. Vodičková, K., Autrata R.: Chirurgická léčba komplikovaných případů strabismu. In Rozsíval, P. (ed.) : Trendy v oftalmologii, sv. 6., Galén, 2010, s. 101 – 123..
35. von Noorden, GK., Helveston, EM.: Strabismus – Rozhodovací postupy. Folia strabologica et neuroophthalmologica, 5, 2002 suppl. II.: 130–133.
36. von Noorden, GK.: Atlas of Strabismus, 4th ed., St. Louis, Mosby, 1995, 223 p.
37. Wright, KW., McVey, JH.: Conjunctival retraction suture for fornix adjustable strabismus surgery. Arch Ophthalmol, 109; 1991 : 138–141.
38. Wright, KW., Hong, P.: Strabismus surgery in Wright, K.W., Spiegel, P.H.: Paediatric Ophthalmology and Strabismus. 2nd ed., New York, Springer, 2003: p. 278–291.
39. Yoo, EJ., Kim, SH.: Modified inferior oblique transposition considering the equator for primary inferior oblique overaction (IOOA) associated with disociated vertical deviation (DVD). Strabismus, 22; 2014 : 13–17.
Štítky
Oftalmológia
Článok vyšiel v časopiseČeská a slovenská oftalmologie
Najčítanejšie tento týždeň
2018 Číslo 4- Cyklosporin A v léčbě suchého oka − systematický přehled a metaanalýza
- Dlouhodobé výsledky lokální léčby cyklosporinem A u těžkého syndromu suchého oka s 10letou dobou sledování
- Účinnost a bezpečnost 0,1% kationtové emulze cyklosporinu A v léčbě těžkého syndromu suchého oka − multicentrická randomizovaná studie
- Pomocné látky v roztoku latanoprostu bez konzervačních látek vyvolávají zánětlivou odpověď a cytotoxicitu u imortalizovaných lidských HCE-2 epitelových buněk rohovky
- Konzervační látka polyquaternium-1 zvyšuje cytotoxicitu a zánět spojený s NF-kappaB u epitelových buněk lidské rohovky
-
Všetky články tohto čísla
- Diagnosis of Familial Hypercholesterolaemia on First Sight? The Role of the Ophthalmologist in Identifying Patients with Familial Hypercholesterolaemia
- Vertical Strabismus – Indication of Surgical Techniques on the Inferior Rectus Muscle
- Keratopigmentation (Corneal Tattoo) – Our First Experience
- Correction of Myopia and Myopic Astigmatism by Implantation of a Phakic Posterior Chamber Implantable Collamer Lens
- Digital Eye Strain in a Population of Young Subjects
- EFFECT OF MULTIPLE VARIABLES ON THE REFRACTIVE ERROR AFTER CATARACT SURGERY
- Česká a slovenská oftalmologie
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Vertical Strabismus – Indication of Surgical Techniques on the Inferior Rectus Muscle
- Keratopigmentation (Corneal Tattoo) – Our First Experience
- Diagnosis of Familial Hypercholesterolaemia on First Sight? The Role of the Ophthalmologist in Identifying Patients with Familial Hypercholesterolaemia
- Correction of Myopia and Myopic Astigmatism by Implantation of a Phakic Posterior Chamber Implantable Collamer Lens
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy




