Selective angiography with the possibility of thrombolysis in patients with central retinal artery occlusion
Authors:
P. Kristian 1; D. Cholevík 1; D. Czerný 2,3
Authors place of work:
Gemini oční klinika Ostrava, primář. MUDr. Dalibor Cholevík, Ph. D.
1; Radiodiagnostický ústav, Fakultní nemocnice Ostrava, přednosta: doc. MUDr. Petr Krupa, CSc.
2; Ústav zobrazovacích metod, Lékařská fakulta, Ostravská univerzita
3
Published in the journal:
Čes. a slov. Oftal., 75, 2019, No. 3, p. 152-159
Category:
Kazuistika
doi:
https://doi.org/10.31348/2019/3/6
Summary
Purpose: Describe the clinical finding and course of treatment in patients with a sudden decrease in visual function due to an acute occlusion of the arteria centralis retinae. Patients were primarily indicated for selective angiography with thrombolysis of the ophthalmic artery.
Materials and methods: Medical documentation of two patients with acute central retinal artery occlusion with a time duration of up to 5 hours was evaluated retrospectively. The diagnosis of central retinal artery occlusion was determined on the basis of a detailed ophthalmological examination in arteficial mydriasis. The initial best-corrected visual acuity (BCVA) were hand movement in front of the eye with uncertain light projection in first patient and no light perception in the second patient. In both cases a relative afferent pupillary defect of the 4th degree was present with the onset of the ischemic macular edema and an incipient development of the cherry red spot. After evaluation of the overall condition, laboratory findings, exclusion of cancer and surgery in the last three months, a selective angiography of ophthalmic artery and thrombolysis in collaboration with the intervention radiologist were performed.
Results: First patient with a better initial visual acuity, selective angiography demonstrated a decrease in flow in the central retinal artery with subsequent improvement in haemodynamic ratios after application of 12 ml of recombinant tissue plasminogen activator (Alteplase). The BCVA improved to 1/ 60 after interventional procedure. We did not experience any serious treatment side effects during or after intervention.
In the second patient, selective angiography of the intracranial arteries and internal carotids revealed the presence of an aneurysm before the ophthalmic artery. Due to the normal flow of the contralateral carotid and the filling of the intracranial vessels on the affected side via the circle of Willis, the internal carotid ligation was performed under the aneurysm. Three months after the surgery BCVA was no light perception and patient had no neurological symptomatology.
Conclusion: Selective angiography in combination with thrombolysis appears to be a useful imaging as well as therapeutic method for acute central retinal artery occlusion. This technique allows not only to confirm the diagnosis but it can also solve problem causally and improve the visual acuity of the affected person. Sometimes it also helps to clear the cause of the closure and prevent next potential embolization into the intracranial space and possible fatal consequences of CNS involvement or even death.
Keywords:
Selective angiography – thrombolysis – aneurysm of the internal carotid artery – recombinant tissue plasminogen activator – central retinal artery occlusion – CRAO
INTRODUCTION
Central retinal artery occlusion (CRAO) is an acute condition in which the blood flow is closed off in the central retinal artery. The cause is most frequently thrombosis (60-75%), followed in second place by embolisation into the affected artery (6). It is manifested in a pronounced decrease of visual acuity, which is often irreversible. Similarly as in the case of other vascular disorders, it predominantly affects the older population. The average age of patients is around 60 years. However, cases of the disorder have also been described in younger and even child patients (18). Men are affected slightly more frequently than women. The incidence is approximately 1 per 10000 of the population (10). The majority of patients are affected in one eye, in 1-2% of cases the disorder is bilateral (18). Complete central retinal artery occlusion is manifested in a sudden and severe decrease of visual functions, as a rule to the level of counting fingers in front of the eye and worse (2, 10). The patient is often also capable of determining precisely the moment of onset of the visual malfunction. Upon examination of the anterior segment on a slit lamp there is a perceptible evident relative afferent pupillary defect (RAPD) in the affected eye. A cherry red spot is biomicroscopically indicated in the macula, as well as segmentation of the blood column in the arteries and impaired flow in the veins. On fluorescence angiography (FAG) there is a demonstrable extended arterial transit time. Conservative therapy covers medicamentous reduction of intraocular pressure, paracentesis of the anterior chamber, inhalation of a CO2 rich compound (for inducing vasodilation of blood vessels), massage of the eyeball, vasodilation preparations, haemodilution, corticosteroids, heparin or antiaggregant drugs (3, 11). Of invasive methods, in the acute stage arteriotomy by Nd:YAG laser is possible (if thrombus or embolus is visible on the papilla or its periphery), or systemic or selective thrombolysis of the affected artery (9, 18).
MATERIAL AND METHOD
Healthcare documentation was retrospectively evaluated for two patients with acute central retinal artery occlusion with a duration of less than 5 hours, who were indicated for selective angiography with the possibility of performing local intra-arterial thrombolysis. Thrombolysis is a therapeutic process by which we attempt to achieve pharmacological dissolution of the blood coagulation which is causing a blockage of the blood flow in the vessel. The obstacle is generally a thrombus (coagulation originating in situ) or embolus (coagulation carried into the place of obstruction by blood flow). At present recombinant tissue plasminogen activators (rTPA) are most often used for thrombolysis. These mediators serve for activation of the plasmatic protease plasmin, which acts in the place of fibrin deposits. We distinguish 2 types of thrombolysis, general and local. In general thrombolysis we apply the medication systemically into the venous circulation regardless of the place of occlusion, in contrast with local, in which we apply the active substance directly into the affected artery or vein. The advantage of local thrombolysis is a reduction of the overall dose of the thrombolytic agent and minimisation of systemic adverse effects.
Typical therapeutic indications for thrombolysis include ischemic stroke, acute myocardial infarction and massive pulmonary embolism. In ophthalmological practice, thrombolytic treatment is indicated for patients with acute central retinal artery occlusion and a short medical history of complaints, as a result up to 6 hours from the first symptoms. Contraindications (CI) of thrombolysis include haemorrhagic states, tumorous pathologies and operations in the last three months (thoracic, abdominal or intracranial procedures). Selective angiography with thrombolysis is performed exclusively under conditions of hospitalisation on a monitored bed.
A diagnosis of central retinal artery occlusion was determined on the basis of the anamnestic data and a complex ophthalmological examination, and was subsequently confirmed by an imaging method with a contrast substance.
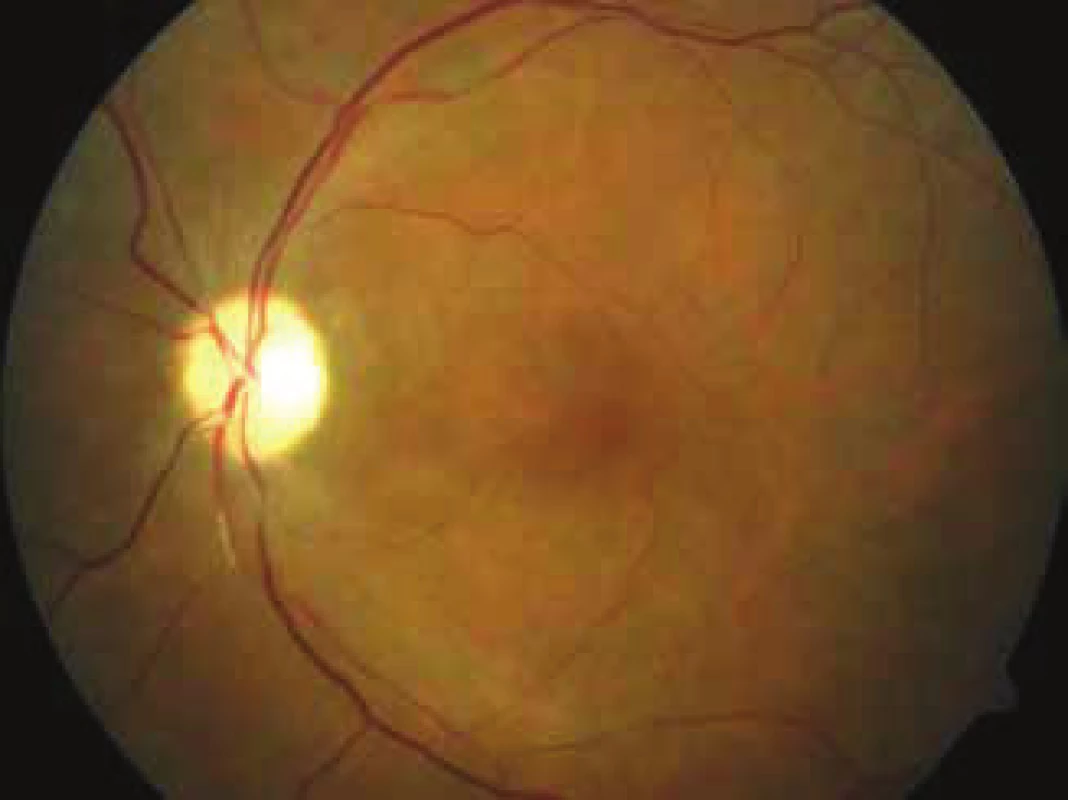
Initial best corrected visual acuity (BCVA) was on the level of blindness in both eyes. In the first patient hand movement in front of the eye with uncertain light projection, in the second patient without light perception. A relative afferent pupillary defect of the 4th degree was present on the anterior segment, biomicroscopically on the ocular fundus incipient ischemic macular edema with incipient development of a central cherry red spot. Due to the urgent nature of the condition, photo-documentation of the retinal finding was obtained with the aid of a mobile telephone and a slit lamp. For the same reason, fluorescence angiography (FAG) was performed the following day.
After an evaluation of the overall condition, the laboratory finding and elimination of CI of thrombolysis, selective angiography of the ophthalmic artery was indicated for both patients and performed with the intervention of a radiologist, with the possibility of local administration of thrombolytic agents. The selected pharmaceutical for thrombolysis was the recombinant tissue plasminogen activator Actilyse (Alteplasum). During hospitalisation further consultancy and paraclinical examinations were conducted as standard after the intervention, such as monitoring of blood pressure values, ultrasonography (SONO) of the carotid artery, transthoracic echocardiography (ECHO) of the heart etc. The observation period for the patients was 1 month after the intervention.
CASE REPORTS
The first referred case report relates to a 58-year-old man, who reported for an urgent eye examination due to sudden loss of vision in the left eye. The patient stated that 5 hours previously his vision had become blurred in the left eye, had then spontaneously corrected itself within minutes, but 2 hours later he lost his vision entirely in that eye. The patient's personal medical history shows that he had suffered a stroke 3 years previously, but did not use and medications long term, and negated other risk factors. The allergological and ocular anamnesis is negative.
Upon the initial examination, best corrected visual acuity was 6/6 in the right eye, and in the left (affected) eye only hand movement in front of the eye, light perception with uncertain light projection, which was not improved by any correction. Intraocular pressure was 16 mmHg in the right eye and 17 mmHg in the left eye.
Examination of the anterior segment revealed a relative afferent pupillary defect of the 4th degree in the left eye. In both eyes there was also an incipient senile nuclear cataract.
On the ocular fundus in the right eye we observed only a 2nd degree hypertonic finding on the arteries. In the left eye cotton wool spots were perceptible by the upper and lower edge of the optic nerve papilla, as well as filiform arteries with an interrupted blood column, in the macula a typical finding of a cherry red spot and pale ischemic edema. In the patient we did not record the presence of a cilioretinal artery either ophthalmoscopically or by fluorescence angiography. Due to the urgent nature of the condition, photo-documentation of the ophthalmoscopic finding was obtained with the aid of a mobile telephone and contact lens on a slit lamp. Fluorescence angiography was performed the following day for the same reason.
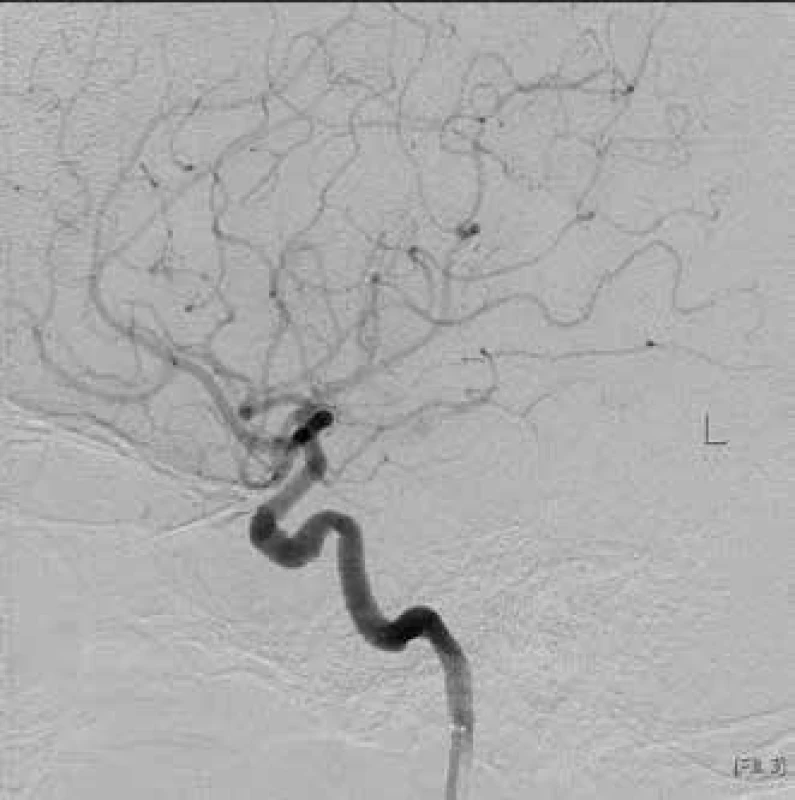
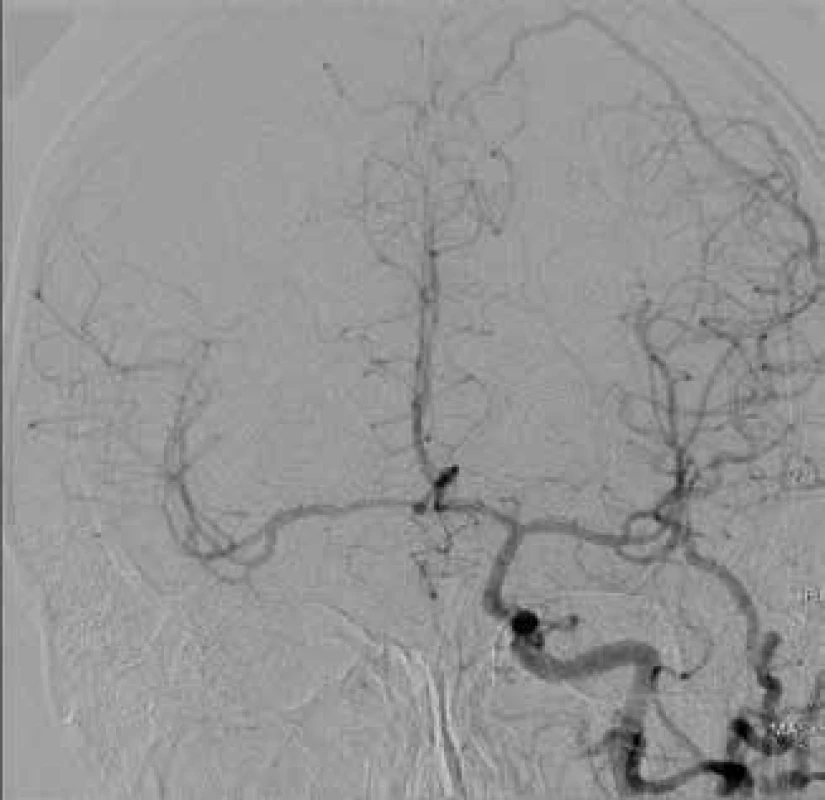
After the initial examination, diagnosis of central retinal artery occlusion and elimination of any contraindications of thrombolysis, we sent the patient, on the basis of a consultation with a radiologist, to the department of intervention radiology. Here a sheath was applied to the patient via the arteria femoralis communis (AFC) I.dx, approx. 4.5 hours after complete loss of sight and under local anaesthesia (Fig. 1). After the application of 5000 units of Heparin intraarterially (i.a.), the catheter continues under X-ray control via the arteria carotis communis (ACC) and arteria carotis interna (ACI) I. sin (Fig. 2).
Upon spray application of the contrast substance, slowed filling of the arteria ophthalmica in the left eye was clearly evident (Fig. 3). Subsequently, during the course of 40 minutes, 12 ml of Alteplasum (recombinant tissue plasminogen activator) was applied therapeutically i.a., after which there was a complete restoration of through passage of the arteria ophthalmica and arteria centralis retinae (Fig. 4).
Significant stenosis remained by the exit of the ophthalmic artery from the ACI even despite peripheral fulfilment. We did not observe any serious adverse effects of treatment either during or after the procedure. On the following day we recorded only a slight laboratory decrease in the level of haemoglobin, which showed a tendency toward spontaneous correction. On the same day best corrected visual acuity (BCVA) improved to 1 metre excentrically. On the retina of the affected eye there was regression of the cotton wool spots. With regard to the persisting stenosis of the exit of the opthalmic artery, we administered dual antiaggregant therapy generally to the patient: Anopyrin 100 mg (acetysalicylic acid) 1x daily and Trombex 75 mg (Clopidogreli sulfas) 1x daily orally. During hospitalisation further consultancy and paraclinical examinations were conducted, such as monitoring of blood pressure values, SONO of carotid, ECHO of heart etc. With regard to the repeated episodes of high arterial pressure, compensation of general pathologies was recommended for the patient before discharge to outpatient care, above all for untreated systemic hypertension.
At a follow-up examination 4 weeks after the intervention, visual acuity in the left eye was 1m naturally, not improved by any correction. On the ocular fundus there was a perceptible finding of a pale optic nerve papilla, constricted retinal capillaries and embolus by the branching of the lower arcade (Fig. 5).



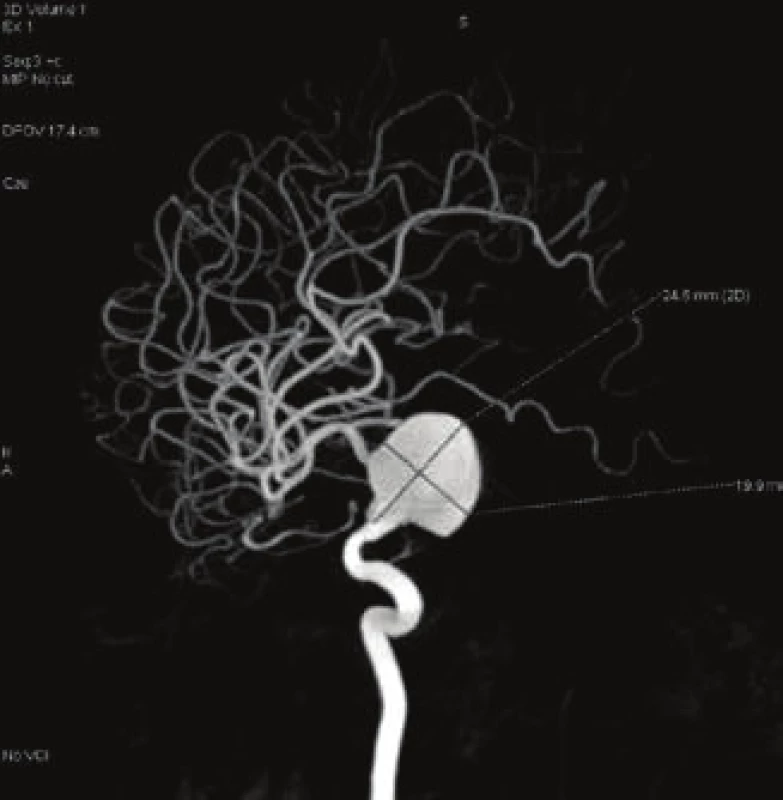

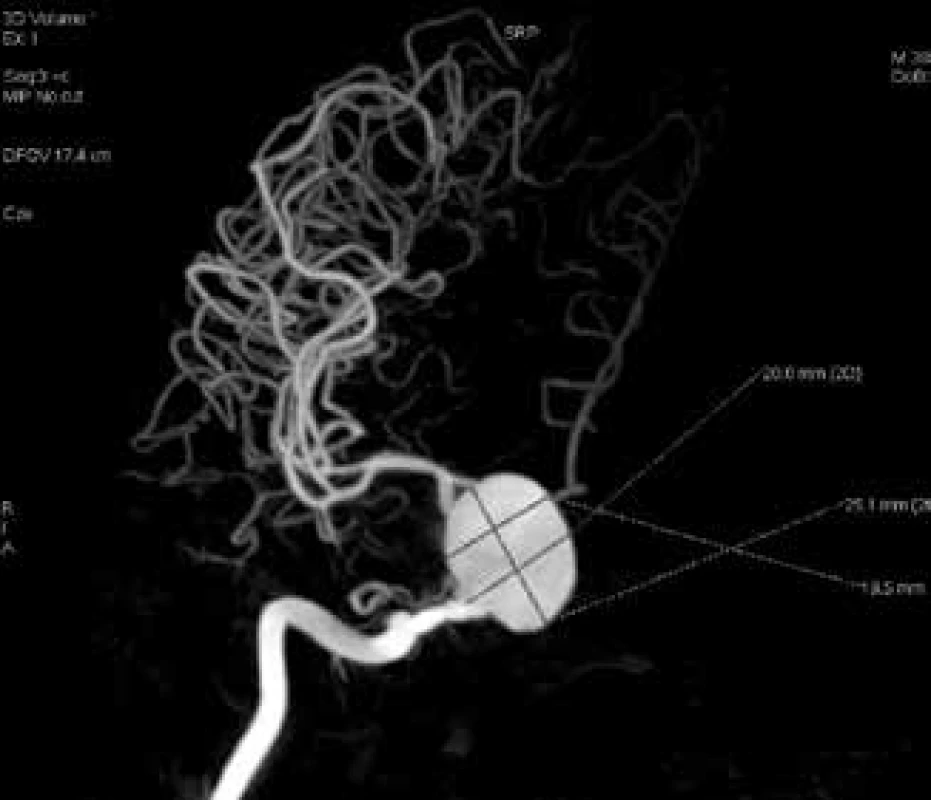
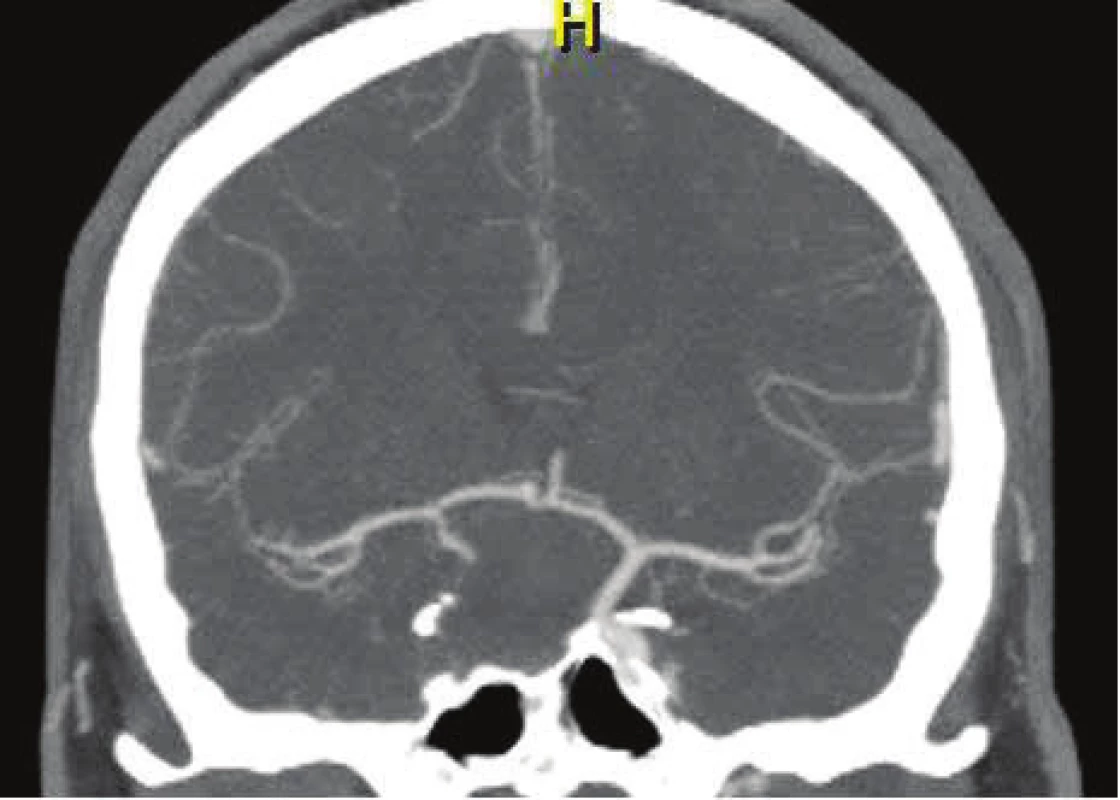
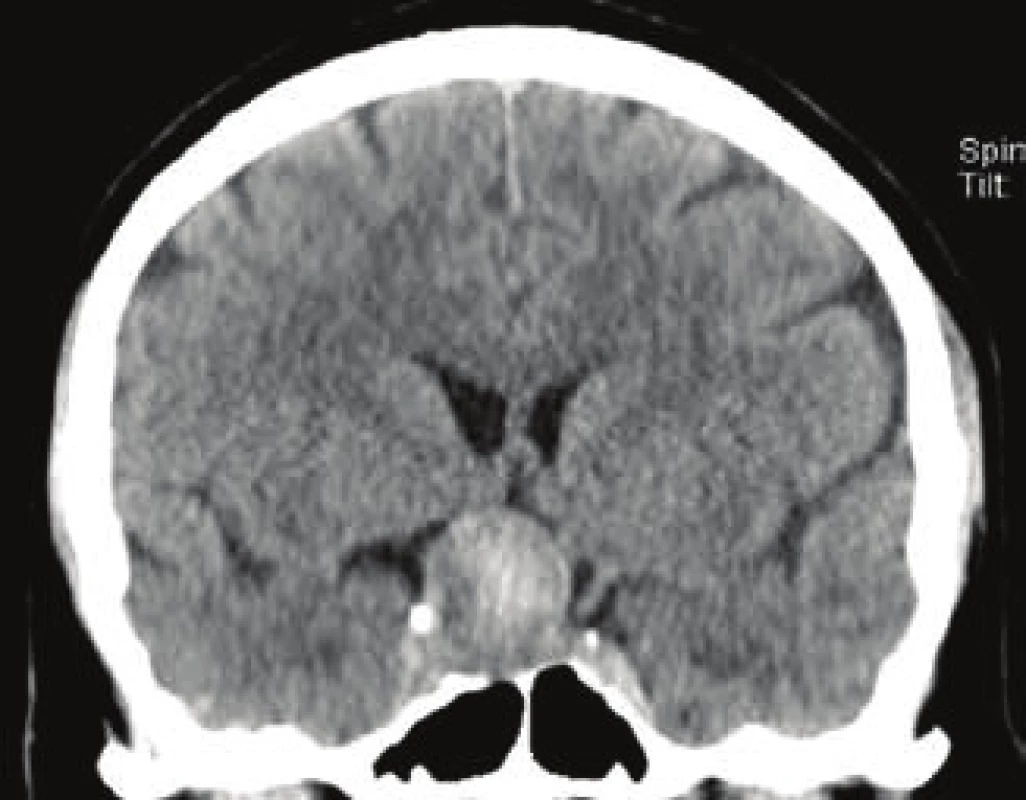
The second referred case was a 36-year-old man, who was brought to the centre by ambulance due to sudden loss of vision in the right eye 2 hours previously. The patient's personal, allergological and ocular anamnesis was negative. The patient did not use any medication long term. The loss of visual acuity in this patient was even more dramatic than in the first case, the affected eye was without light perception. BCVA in the left eye was 6/6. Intraocular pressure was 16 torr in the right eye, 17 torr in the left eye. Upon examination on a slit lamp, RAPD of the 4th degree was expressed on the anterior segment of the affected eye. On the retina biomicroscopically there was a perceptible typical finding of a cherry red spot in the macula, with surrounding pale ischemic edema, confirming a diagnosis of central retinal artery occlusion. With regard to the short history of complaints, after an urgent general and laboratory examination we indicated the patient for the performance of selective angiography with the possibility of targeted administration of a thrombolytic agent. After the insertion of a sheath and spray application of a contrast substance to the arteria carotis interna (in an analogous manner as in the first referred case), a gigantic fusiform aneurysm was discovered, localised by the exit of the arteria ophthalmica in the right eye (Fig. 6). CT angiography was also performed on the patient (Fig. 7). The size of the formation was 20.6 x 25.1 mm (Fig. 8). The cause of occlusion of the ACR appeared to be very probably progression of the sac or embolisation from the sac of the aneurysm. On the basis of the finding of this probable etiology of occlusion, the administration of thrombolytic agents was abandoned due to the large risk of release of further thrombembolisms from the sac of the aneurysm intracranially. Subsequently a CT angiography examination of the contralateral carotid artery was also performed on the patient, with concurrent compression of the affected artery (Fig. 9). During the course of this examination normal through-flow was recorded, as well as filling of the intracranial blood vessels on the affected side of the circle of Willis. The patient tolerated the occlusion well, and was neurologically entirely asymptomatic. With regard to the fact that the aneurysm was a threat to the patient in future due to subsequent embolisations into the intracranial space and potentially also a lethal rupture of the aneurysm with intracranial haemorrhage, ligation of the affected ACI before the aneurysm was indicated and performed following an agreement with the radiologists and neurosurgeons. One month after the procedure, according to a follow-up angiographic examination there was no longer any retrograde filling of the aneurysm (Fig. 10). There was also almost complete thrombotisation of the aneurysm lumen (Fig. 11). Visual acuity of the affected eye is without light perception, and the patient is without lesion neurological symptomatology.
DISCUSSION
The clinical finding upon central retinal artery occlusion was first described by Albrecht von Graefe in 1859 (18). Obliteration occurs in the majority of cases due to atheroma or embolism in the region of the lamina cribrosa (4). The most common cause of embolism is thrombi from the left half of the heart (14). A visible embolism in the central retinal artery is generally linked with a worse prognosis of visual acuity and increased patient mortality (5, 10). However, the embolus may also be infectious, tumorous, fat or air (14). Central retinal artery occlusion may also occur iatrogenically. For example, Oláh et al. published a case of a patient with central retinal artery occlusion following an injection of hydrocortisone into the region of the mandibular joint (14). Park et al. treated a woman with central retinal artery occlusion (CRAO) of the nose after autologous injections of fat tissue into an area of the nose, which she had applied for cosmetic reasons (15). In a further study, Park et al. described 12 patients with vascular occlusions following injections applied to the region of the glabella or nasolabial fold due to a cosmetic indication. Two patients had central retinal artery occlusion, three had branch occlusion. In the other seven patients there was an occlusion of the arteria ophthalmica. In the majority of cases the injected material was autologous fat, hyaluronic acid or collagen. In comparison with other materials, the application of fat was linked with a worse prognosis for resulting visual acuity (16).
Kalvodová et al. described a case report of occlusion of the lower temporal branch of the ACR as an early complication of percutaneous transluminal coronary angioplasty (PTCA) in a man with acute Q-wave infarction of the lower wall and right chamber (8). Mohindra et al. presented a study on the onset of central retinal artery occlusion in a 12-year-old boy following selective embolisation of juvenile nasopharyngeal angiofibroma, supplied only from the arteria maxillaris (12).
In the majority of cases CRAO affects older patients, with an average age around 60 years (10). However, there are case reports of younger patients, such as the case of our second patient. A case of a patient of similar age was published by Mach et al. (11), who observed a 34-year-old man with aortic stenosis on a background of congenital malformation, who had suffered central retinal artery occlusion. The patient's initial vision was 0.5 metres. Approximately 6 hours after the beginning of anamnestic complaints, urokinase was administered by catheter into the inner carotid artery on the same side. In long-term observation, best corrected visual acuity was stabilised at a value of 6/36.
In the acute stage, BCVA is most often within the range of light perception to counting fingers in front of the eye (10, 18). Central visual acuity may also be normal if the present cilioretinal artery ensures sufficient supply to the fovea and maculo-papillary bundle (18). Visual acuity without light perception is less common. If a patient does not even see light, it is necessary to consider an accompanying pathology, mostly abnormalities in the choroidal artery or damage to the optic nerve (5, 18). A further possibility in differential diagnostics may be affliction of the inner carotid artery by an aneurysm, as was the case in our second patient.
A similar case was described also by Haritogla et al. (7). The authors observed central retinal artery occlusion in connection with an aneurysm of the arteria carotis interna in a 41 year old woman. This aneurysm was of smaller dimensions of approx. 17 x 15 mm as opposed to 20.6 x 25.1 mm in our patient. There was a significant difference above all in best corrected visual acuity, which in this patient was far better, specifically 6/15, whereas our patient was without light perception. This fundamental difference was due to the presence of the cilioretinal artery.
The prognosis of CRAO is unfavourable (19). On experimental animal models it has been demonstrated that irreversible changes on the retina take place as soon as within 90-100 minutes of the occurrence (10). For example, the retina of monkeys is capable of tolerating ischemia for a maximum of 100 minutes. However, angiographic findings in humans have demonstrated that occlusion of the ACR is complete only rarely. For this reason selective thrombolysis, commenced within 6 hours of the beginning of the symptoms, may restore the blood supply to the retina (9, 19). In addition to classic options of conservative therapy, which include reduction of intraocular pressure, vasodilation, massage of the eyeball etc., it is possible in indicated cases of a short duration of complaints to use methods of pharmacological thrombolysis of the occlusion. The first attempts at local fibrinolysis of retinal blood vessels appeared at the beginning of the 1960s (11). The most suitable candidates are patients with a medical history of the onset of the complaints of less than 3 hours, less positive results have been described up to 6 hours from the first symptoms (3, 21).
Schmidt et al. (19) described a cohort of 14 patients to whom they applied medication by a micro-catheter inserted into the ophthalmic artery or inner carotid artery. Of these patients, 11 were treated with urokinase, 3 with the aid of recombinant tissue plasminogen activator (rTPA). Vision improved markedly in 4 patients, in 5 patients there was a slight improvement. In five patients visual functions remained unchanged. A cilioretinal artery was not present in any of the patients (19).
Very promising results with rTPA were published by Vulpius et al., who treated 9 patients. In five they achieved an improvement of visual acuity from original hand movement in front of the face to the level of 6/10 (22).
Schumacher et al. evaluated the results of treatment of 23 patients. In 18 cases they used urokinase, in the others rTPA. In six patients visual acuity was improved very significantly to values of 6/15 – 6/6. In six patients BCVA or the scope of the visual field improved only slightly. The worse results were attained by the group of patients treated on average more than 20 hours after the beginning of the symptoms (21).
A large retrospective study was published by Richard et al. The authors used rTPA for local intra-arterial treatment on a total of 53 patients, 46 with CRAO and 7 with branch retinal artery occlusion (BRAO). At the end of the three-month observation period, visual acuity improved in 35 (66%) patients (17).
Aldrich et al. published a study comparing the results of visual acuity in 2 groups of patients with acute CRAO. Twenty one patients were treated by local intra-arterial thrombolysis. The same number received standard conservative therapy. In the first group of patients treated with thrombolysis vision improved by one or more rows of Snellen's optotypes in 76%, in comparison with 33% in the control group. Nonetheless, a disadvantage of this study was the fact that the patients were not randomised, and it was rather patients with a shorter history of complaints who were indicated for thrombolysis (1).
Results of one of the first multicentric prospective randomised studies which set out to evaluate the efficacy and safety of intra-arterial thrombolysis with the aid of rTPA in comparison with conventional therapy were published by Schumacher et al. (20). This study incorporated 84 patients, 40 of whom were treated conservatively, in the remaining 44 patients local thrombolysis was performed. The authors evaluated best corrected visual acuity one month after treatment. Vision improved significantly in both of the observed groups, and no difference was recorded between the two groups. With regard to the comparable effect and the fact that in the group with thrombolysis there was a higher number of complications, the authors of the study did not recommend thrombolysis. However, a shortcoming of this study was the relatively long time interval between the initial symptoms and the commencement of therapy. This period was on average equal to 10.99 ± 5.49 hours in the case of conservative therapy, and 12.78 ± 5.77 hours in the case of thrombolytic strategy of treatment.
Arterial intervention and thrombolysis bring with them a certain risk of complications, which include above all haemorrhage in the place of entry into the central artery, intraretinal and intracranial haemorrhage, transitory ischemic attack (TIA) or stroke. These complications are more frequent in older patients (13). A larger risk of haemorrhage is linked with a higher dose of the thrombolytic agent and longer duration of the procedure (1). However, it has been demonstrated that 39% of patients with CRAO would accept a certain risk of stroke. In the case of affliction of the only seeing eye this rises to more than 80% (2).
On the basis of our observation and the published results, a very important prognostic factor which influences the results of therapy appears to be the length of duration of ischemia. As in the majority of retrospective studies, in our first patient we recorded an improvement of BCVA after the administration of a thrombolytic agent, from original movement in front of the eye and light perception with uncertain light projection to a resulting 1m with correct light projection. The improvement was relatively small, although for the patient this was quite significant. The persisting constriction by the exit of the arteria ophthalmica and relatively longer interval until the commencement of therapy was probably the cause of the limited effect of treatment. In the second referred case, the doctor performing the procedure abandoned the administration of a thrombolytic agent due to the excessive risk of release of further embolisms from the lumen of the aneurysm. After the performance of ligation of the affected artery beneath the sac of the aneurysm, thrombotisation of the aneurysm lumen took place in the patient. By this procedure we averted life threatening complications such as rupture of the sac or subsequent embolisation into the intracranial space.
CONCLUSION
Selective angiography in combination with thrombolysis appears to be a useful imaging and also therapeutic method in the case of acute central retinal artery occlusion. These techniques enable us not only to confirm a working diagnosis, but also to resolve it causally and thus improve the patient's visual acuity, as was the case in our first patient. At the same time, in certain cases it may clarify the etiology of the occlusion and thereby avert potentially life threatening conditions ensuing from further embolisations into the intracranial space.
On the basis of the majority of published studies, the method of local thrombolysis appears to be more effective than classic conservative methods. However, this hypothesis is refuted by the results of the first prospective study, although in this study there is a relatively long interval between the beginning of the complaints and the commencement of therapy. This aspect is demonstrated to be a very important prognostic factor in the majority of the published reports. More randomised prospective studies with a shorter anamnesis and prompt commencement of treatment are required in order to verify the actual effectiveness in comparison with classic strategies.
The authors of the study declare that no conflict of interest exists in the compilation, theme and subsequent publication of this professional communication, and that it is not supported by any pharmaceuticals company.
MUDr. Petr Kristian
Opavská 225,
747 19 Bohuslavice u Hlučína
Received: 14. 2. 2019
Accepted: 1. 6. 2019
Available on-line: 19. 10. 2019
Zdroje
1. Aldrich, EM., Lee, AW., Chen, CS. et al.: Local intraarterial fibrinolysis administered in aliquots for treatment of central retinal artery occlusion: Johns Hopkins Hospital experience. Stroke, 39(6); 2008: 1746-1750.
2. Biousse, V., Calvetti, O., Bruce, BB. et al.: Thrombolysis for central retinal artery occlusion. J Neuro-Ophthalmol, 27(3); 2007: 215-230.
3. Biousse, V.: Thrombolysis for acute central retinal artery occlusion: Is it time?. Am J Ophthalmol, 146(5); 2008: 631-634.
4. Boguszaková, J., Pitrová, Š., Růžičková, E.: Akutní stavy v oftalmologii, Praha, Galén, 2006, 116 s.
5. Brown, GC., Magargal, LE.: Central retinal artery obstruction and visual acuity. Ophthalmology, 89(1); 1982: 14-19.
6. Dostál, O., Dubská, Z., Skalická, L. et al.: Trombolytická terapie akutní okluze a. Centralis retinae. Kardiol Rev Int Med, 12(4); 2010: 175-178.
7. Haritoglou, C., Műller-Schunk, S., Weber, C. et al.: Central retinal artery occlusion in association with an aneurysm of the internal carotid artery. Am J Ophthalmol, 132(2); 2001: 270-271.
8. Kalvodová, B., Aboutable, T., Sedláček, K. et al.: Okluze větve a. centralis retinae jako komplikace koronární angioplastiky pro akutní infarkt myokardu. Cor Vasa, 42(7); 2000: 354-356.
9. Kanski, JJ., Bowling, B.: Clinical Ophthalmology: a systematic approach. 7th ed. Edinburgh, Elsevier Saunders, 2011, 909 s.
10. Kuchynka, P.: Oční lékařství. 1. vyd. Praha, Grada, 2007, 768 s.
11. Mach, R., Kessler, P., Sušický, P. et al.: Trombolýza arteriální sítnicové okluze urokinázou. Čs. Oftal., 48(1), 1992: 42-47.
12. Mohindra, S., Mankoo, RS., Grover, G. et al.: Central retinal artery occlusion: An unusual complication in a case of nasopharyngeal angiofibroma solely supplied by ipsilateral internal maxillary artery. Int J Pediatr Otorhinolaryngol Extra, 6(3); 2011: 111-113.
13. Noble, J., Weizblit, N., Baerlocher, MO. et al.: Intra-arterial thrombolysis for central retinal artery occlusion: a systematic review. Br J Ophthalmol, 92(5); 2008: 588-593.
14. Oláh, Z., Zváč, J.: Uzáver vetiev a. centralis retinae po injekcii hydocortisonu do oblasti mandibulárného zhybu. Čs. Oftal., 28(4); 1972: 193-196.
15. Park, SJ., Woo, SJ., Park, KH. et al.: Partial Recovery after Intraarterial Pharmacomechanical Thrombolysis in Ophthalmic Artery Occlusion following Nasal Autologous Fat Injection. J Vasc Interv Radiol, 22(2); 2011: 251-254.
16. Park, SW., Woo, SJ., Park, KH. et al.: Iatrogenic Retinal Artery Occlusion Caused by Cosmetic Facial Filler Injections. Am J Ophthalmol, 154(4); 2012: 653-662.
17. Richard, G., Lerche, RC., Knospe, V. et al.: Treatment of Retinal Arterial Occlusion with Local Fibrinolysis Using Recombinant Tissue Plasminogen Activator. Ophthalmology, 106(4); 1999: 768-773.
18. Ryan, SJ.: Retina. 5th ed. London: Elsevier Saunders, 2013, 3164 s.
19. Schmidt, D., Schumacher, M., Wakhloo, AK.: Microcatheter urokinase infusion in central retinal artery occlusion. Am J Ophthalmol, 113(4); 1992: 429-434.
20. Schumacher, M., Schmidt, D., Jurklies, B. et al.: Central Retinal Artery Occlusion: Local Intra-arterial Fibrinolysis versus Conservative Treatment, a Multicenter Randomized Trial. Ophthalmology, 117(7); 2010: 1367-1375.
21. Schumacher, M., Schmidt, D., Wakhloo, AK. et al.: Intra-arterial fibrinolytic therapy in central retinal artery occlusion. Neuroradiology, 35(8); 1993: 600-605.
22. Vulpius, K., Hőh, H., Lange, H. et al.: Selektive perkutane transluminale Lysetherapie mit RTPA bei retinolem Zentralarterienverschluβ. Ophthalmologe, 93(2); 1996: 149-153.
Štítky
OftalmológiaČlánok vyšiel v časopise
Česká a slovenská oftalmologie

2019 Číslo 3
- Cyklosporin A v léčbě suchého oka − systematický přehled a metaanalýza
- Myasthenia gravis: kombinace chirurgie a farmakoterapie jako nejefektivnější modalita?
- Pomocné látky v roztoku latanoprostu bez konzervačních látek vyvolávají zánětlivou odpověď a cytotoxicitu u imortalizovaných lidských HCE-2 epitelových buněk rohovky
- Konzervační látka polyquaternium-1 zvyšuje cytotoxicitu a zánět spojený s NF-kappaB u epitelových buněk lidské rohovky
- Dlouhodobé výsledky lokální léčby cyklosporinem A u těžkého syndromu suchého oka s 10letou dobou sledování
Najčítanejšie v tomto čísle
- Pupillary abnormalities in childhood – 2 case presentations
- Influence of cornea on intraocular pressure measurement by ICARE PRO and ORA
- Selective angiography with the possibility of thrombolysis in patients with central retinal artery occlusion
- Methods of improving the quality of life in patients with stable maculopathy-pilot results of a new study
