-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Ethical Implications of Modifying Lethal Injection Protocols
article has not abstract
Published in the journal: Ethical Implications of Modifying Lethal Injection Protocols. PLoS Med 5(6): e126. doi:10.1371/journal.pmed.0050126
Category: Essay
doi: https://doi.org/10.1371/journal.pmed.0050126Summary
article has not abstract
Courts in the United States have historically judged execution methods against “evolving standards of decency,” and have prohibited punishments that involve “the unnecessary and wanton infliction of pain,” or more recently the “substantial risk of serious harm” [1]. Public repugnance and legal challenges to execution by cyanide gas and electrocution led to the development of lethal injection as an ostensibly more humane method of state killing [2,3]. The intravenous delivery of an anesthetic, a paralytic, and potassium chloride in lethal injection protocols is intended to cause a painless death, which likely accounts for its use in 930 of the 1,100 executions in the United States from the reestablishment of the death penalty in 1976 to May 6, 2008, as well as for its growing use worldwide [4,5].
Despite the procedure's use of drugs and medical personnel and equipment, lethal injection for execution was conceived and implemented by physicians and corrections personnel without adherence to standards now used for developing and testing new clinical procedures. Oklahoma legislators looking for a more humane and less expensive alternative to the electric chair approached the state medical examiner, Jay Chapman, who suggested a protocol that was subsequently approved by the chairman of anesthesiology at the University of Oklahoma and then written into law [2,3,5]. Chapman has since stated that he did no research in choosing the drugs [5]. Moreover, there is no evidence of any directed experimental or clinical research of this protocol being performed prior to the first lethal injection, the 1982 Texas execution of Charlie Brooks. Subsequently, execution data and eyewitness reports from various states indicate that some inmates have suffered during lethal injection, and suggest that others may have suffered without detection [6–8]. Such observations have prompted legal challenges as well as judicially mandated or executive review of states' protocols [9].
Summary
Lethal injection for execution has largely replaced other execution methods, in part due to the appearance of a peaceful death; however, available evidence indicates that some inmates actually suffer extreme pain. This has triggered legal challenges against lethal injection on the grounds that it violates the United States' constitutional prohibition against cruel and unusual punishment. Some jurisdictions collect comprehensive data on executions and outcomes, and some have modified their lethal injection protocols. Recently, jurists and lethal injection advisory panels have recommended specific changes to be instituted for future executions. Such use of biomedical inquiry to evaluate, modify, and “improve” protocols resembles human experimentation and should be scrutinized against accepted norms for ethical conduct of research, particularly given the vulnerable nature of the prisoner population. Although the regulations governing prisoner research vary by jurisdiction, the ethical framework for the modification of lethal injection protocols should be made clear prior to further investigation into how to “improve the process.”
Lethal Injection Investigative Activities
Execution records are unavailable from many jurisdictions, including Texas and Virginia, which together have performed 51.1% of lethal injection executions [4]. However, evidence obtained in litigation and from Freedom of Information Act requests reveals that at least some jurisdictions systematically collect data on executions and outcomes (Table 1). The motivations for the data collections are largely unknown, although in certain cases, the processes suggest a prospective intent to collect data, e.g., assaying thiopental levels in virtually all executed inmates, while in others the stated goal is to assess adequacy of anesthesia in life and post-mortem thiopental changes after death [6]. Moreover, the collection of multiple, timed post-mortem blood samples from individual inmates in Connecticut and North Carolina was clearly intended to address questions regarding thiopental redistribution [10].
Tab. 1. Known Lethal Injection Investigative Activities by Jurisdiction 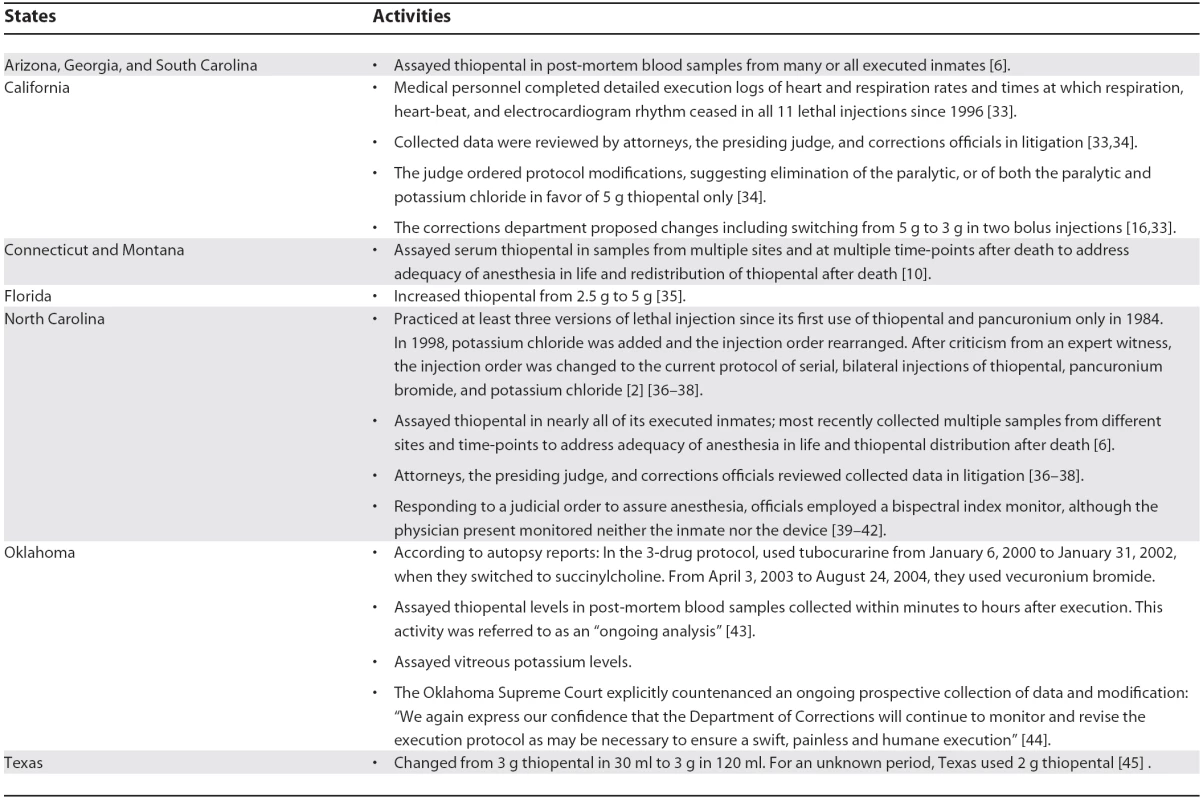
In addition to data collection activities, systematic modifications of lethal injection protocols have been implemented or are planned in several jurisdictions, with the effect of subjecting inmates to different drug doses or injection sequences (Table 1). In certain cases, such as the use of at least three different chemical paralytics in Oklahoma or three different doses of thiopental in Texas, the impetus for change from the standard protocol is unknown. For others, including rearranging the drug injection sequence in North Carolina and increasing the dose of thiopental in Florida, expert testimony, judicial orders, or recommendations from special state panels were involved [8,11–14]. In these latter cases, the jurisdictions were responding directly to charges that the prior process of lethal injection posed an unacceptable risk of pain and suffering.
Many of the methods being used to collect data in executions and modify lethal injection protocols incorporate biomedical research activities. Moreover, processes such as prospective blood and vitreous sample collections, thiopental or potassium assays, bispectral index monitoring with the intent to gauge consciousness in execution, and the systematic alteration of drugs, doses, and order of drug administration in various groups of inmates are invasive activities that carry substantial implications for prisoners. This raises the concern: are corrections officials and judges engaging in human experimentation as they seek to improve lethal injection protocols?
Guidelines for Ethical Conduct of Human Subjects Research
Modern policies, including guidelines and regulations for the ethical conduct of research involving human subjects, such as the Nuremberg Code, the World Medical Association's Declaration of Helsinki, the Council for International Organizations of Medical Sciences, and the Belmont Report, were developed at least partially in response to experimentation on prisoner populations. Together they describe a set of rules designed to guide researchers and reviewers in order to protect the interests of research participants. In the US, federally funded research is regulated by the Federal Policy for the Protection of Human Subjects (also known as the “Common Rule”) [15]. The Common Rule provides protection for research participants by requiring institutional assurance of compliance with federal regulations, institutional review board (IRB) review, approval, and oversight, and informed consent of the participants. Currently the Common Rule categorizes prisoner subjects as a vulnerable population requiring special protections. Although the Common Rule strictly applies only to research conducted or supported by federal departments or agencies, many states, universities, hospitals, and other private enterprises apply its standards uniformly across all research projects, regardless of funding source, and the Common Rule is generally considered an important standard for ethical conduct of human experimentation in the United States.
The Common Rule defines research as “a systematic investigation, including research development, testing and evaluation, designed to develop or contribute to generalizable knowledge”—without explicitly defining “generalizable knowledge.” A human subject is a “living individual about whom an investigator….obtains (1) Data through intervention or interaction with the individual, or (2) Identifiable private information.” Intervention includes both physical procedures by which data are generated and manipulations of the subject or environment performed for research purposes. While the Common Rule is often applied to biomedical research, it covers the range of human experimentation, including education and behavioral studies as well as medical device or drug studies with no beneficial intent.
Lethal Injection Investigations as Human Subjects Research
The evidence displayed in Table 1 indicates that the collective practice of lethal injection has employed invasive testing of different drug protocols and devices, data collection and monitoring, and systematic review with outcome data being used to revise practice. Therefore, it might be argued that certain lethal injection inquiries constitute human subjects research as defined in the Common Rule. Corrections officials and their medical collaborators might contend that their intent is not to produce “generalizable knowledge”, i.e., information for use in other settings, but rather to improve the protocol within a particular jurisdiction. It is important to keep in mind, however, that virtually all US lethal injection protocols derive directly from the initial Oklahoma legislation and Texas experience as communicated by corrections officials [2]. A former executioner for Virginia and Georgia has stated that he both assisted Florida with its electrocution protocol and visited Texas to observe that state's lethal injection protocol prior to the first Virginia lethal injection. More recently, the State of California cited surveys and site visits to other jurisdictions as “invaluable” in making improvements in that state's lethal injection protocol [16]. In addition, the Department of Justice has held at least one execution training session, for corrections personnel from Arizona, California, Florida, Missouri, and Tennessee. Although there have been only three lethal injections under Federal jurisdiction, the session included protocol overviews, facility tours, discussion of current issues, practical exercises, and networking [17]. Given this history, it is conceivable that protocol modifications resulting from activities performed in particular states would likely be communicated to or copied by other jurisdictions, in effect generalizing the conclusions to others.
On the contrary, some might argue that the evaluation and modification of lethal injection protocols has been practiced solely to “improve” lethal injection within jurisdictions and not to contribute to generalizable knowledge, thereby inviting comparison to clinical quality improvement projects. Such a designation falls short of “human subjects research” and its current federal regulatory requirements. Although presently there is a lack of consensus regarding the definition of quality improvement in health care and the requirements for its ethical oversight, the Hastings Center convened a group to address the ethical requirements of quality improvement and their relationship to regulations protecting human subjects of research. In a recently published report, the group defined quality improvement as “systematic, data-guided activities designed to bring about immediate improvements,” that “at its heart is a form of experiential learning that regards improvement to be part of the work process and always involves deliberate actions expected to improve care, guided by data reflecting the effects” [18,19]. They conclude that while quality improvement activities may differ from human subjects research, they are not exempt from ethical requirements, including social or scientific value, scientific validity, fair participant selection, favorable risk–benefit ratios, respect for participants, informed consent, and independent review. Thus in this interpretation, classifying lethal injection investigations as quality improvement activities would not exempt such studies from some type of ethical oversight, even if they do not fall within the purview of traditional IRBs.
If lethal injection data collection and modification activities meet the definition of research or human experimentation, a substantial set of policies become relevant. Collectively, internationally accepted standards for the ethical conduct of research demand that properly conducted human studies:
be founded upon adequate scientific data and animal experimentation,
be conducted by scientifically qualified persons,
be reviewed and supervised by a qualified review board,
be performed with the consent of the participants, and
must minimize risk to human subjects.
Judging lethal injection data collection and protocol modification activities by these standards reveals fundamental flaws. First, none of the current protocols were ever tested in animals; indeed, details of dose and administration actually contradict current veterinary practices [2,5,8]. Thus neither the original protocol nor subsequent modifications are “founded upon adequate scientific data and adequate animal experimentation.” Second, the scientific and medical qualifications of those responsible for evaluating and modifying lethal injection protocols (distinct from those participating in executions) vary from state to state, but are known to range from lay volunteers or prison staff with no medical training to judges and medical experts advising in the courtroom but not present in the execution chamber [3,20–22].
Third, lethal injection research activities have not been subject to expert review. The only known reviews of lethal injection protocols have been retrospective reviews by sometimes secret executive committees convened by governors in California, Tennessee, and Florida [16,23,24]. However, those reviews were focused specifically upon investigating past execution outcomes, rewriting outdated protocol handbooks, and facilitating future executions, but not upon explicitly protecting the interests of the prisoners being executed, which is the intent of guidelines such as the Common Rule [16,24]. Fourth, consent for these activities has not been described. Under all accepted ethical guidelines, including the Common Rule, participation of research subjects must be free and not subjected to undue influence or coercion. Finally, while some lethal injection studies could be considered minimal or no risk (electrocardiogram monitoring, post-mortem sample collection) others, including the addition or omission of drugs and altering of drug doses and sequences, seem to present substantial risk. Indeed, the risk of extreme pain and suffering is at the heart of the current lethal injection debate.
Additional Protections for Prisoner Subjects of Research
Finally, prisoners constitute a vulnerable group that historically has been provided special protections in research in large part because of concerns regarding the difficulty of ensuring voluntary informed consent in this setting. Under current regulations, death row inmates have the same protections as other prisoners; while they may have been stripped of the right to freedom and to life, they maintain the right to bodily integrity and to refuse participation in research [25]. Subpart C of the Common Rule specifies additional protections for prisoner subjects and limits research to minimal risk studies relating directly to incarceration; research on conditions particular to prisoners as a class (but only with approval by the Secretary of Health and Human Services); and research that has the “intent and reasonable probability of improving the health or well-being of the subject.” The Common Rule explicitly prohibits all other biomedical and behavioral studies on prisoners. In its 2006 report, “Ethical Considerations for Research Involving Prisoners,” the Institute of Medicine recommended changes to the Common Rule, including (1) expanding the definition of research, (2) ensuring universal, consistent ethical protection, (3) shifting from categorical to risk–benefit-based research review, (4) employing collaborative responsibility, and (5) enhancing systematic oversight—although these have not yet been employed [26].
State Regulation of Prisoner Research and Implications for Lethal Injection
We have been evaluating lethal injection investigation against the Common Rule, but as recognized by the Institute of Medicine, the Common Rule regulates only a fraction of human experimentation conducted in the United States. In the absence of federal authority, state laws, when they exist, become the only regulatory paradigm [27]. Further, when state laws exist and afford additional protections for research subjects they are to be followed [28]. Virtually all lethal injections and thus lethal injection investigative activities occur in state prisons, where regulation of human subjects research and prisoner protections vary considerably. Arizona allows any research approved by the prison director and chief of inmate health services, while Georgia merely requires research approval by the commissioner of corrections [29]. Oregon law states that “there shall be no medical, psychiatric, or psychological experimentation or research with inmates in Department of Corrections institutions of the State of Oregon,” although it limits the ban to “nontherapeutic” procedures [30]. California law prohibits all “biomedical research” except for participation in investigational new drug research deemed in the best medical interest of the inmate [31]. In Virginia, “nontherapeutic research using institutionalized participants shall be prohibited unless it…will not present greater than minimal risk” [32].
Overall, 30 states require IRB review of prison research studies; therapeutic biomedical research is permissible in 15 of 48 state departments of correction, while only three states permit biomedical studies of a nontherapeutic nature [26]. Thus, because both lethal injection protocols and regulatory authority of individual jurisdictions vary significantly, the legal requirements of such studies ultimately must be decided upon a case-by-case basis. To our knowledge, however, there has been no attempt to apply regulatory standards for human experimentation or IRB review and oversight to lethal injection activities to date.
Conclusions
While lethal injection and the death penalty present a host of ethical questions, the specific, pressing issue now faced by 36 US states, the federal government, and the 3,350 prisoners on death row is the movement to amend lethal injection protocols to comport with Eighth Amendment requirements and to minimize the potential for pain and suffering, in itself a commendable goal. As jurists demand lethal injection protocol changes, however, corrections officials, governors, and their medical collaborators are left in a legal and ethical quandary. In order to comply with the law and carry out their duties, they are employing the tools and methods of biomedical inquiry without its ethical safeguards. Given the current guidelines for human experimentation, it is difficult to conceive of circumstances in which lethal injection research activities could be carried out in a fashion consistent with these ethical norms, and yet those engaged in such research would seem to be required to do so. We submit that the ethical framework, if any, for the modification of lethal injection protocols must be made clear prior to further investigation into how to “improve the process.”
Zdroje
1. 2008
Baze v. Rees, 128 S. Ct. 1520, 1532, 1548, 1568
2. DennoD
2002
When legislatures delegate death: The troubling paradox behind state uses of electrocution and lethal injection and what it says about us.
Ohio State Law J
63
63
260
Available: http://papers.ssrn.com/sol3/papers.cfm?abstract_id=319340. Accessed 5 May 2008
3. DennoDW
2007
The lethal injection quandary: How medicine has dismantled the death penalty.
Fordham Legal Studies Research Paper No. 983732. Available: http://papers.ssrn.com/sol3/papers.cfm?abstract_id=983732. Accessed 5 May 2008
4. Death Penalty Information Center
2008
Searchable database of executions.
Available: http://www.deathpenaltyinfo.org/executions.php. Accessed 5 May 2008
5. FellnerJTofteS
2006
So long as they die: Lethal injection in the United States. Human Rights Watch.
Available: http://hrw.org/reports/2006/us0406/. Accessed 5 May 2008
6. KoniarisLGZimmersTALubarskyDASheldonJP
2005
Inadequate anaesthesia in lethal injection for execution.
Lancet
365
1412
1414
7. WeismanRSBernsteinJN
2005
Inadequate anaesthesia in lethal injection for execution.
Lancet
366
1074
author reply 1074–1076
8. ZimmersTASheldonJLubarskyDALópez-MuñozFWatermanL
2007
Lethal injection for execution: Chemical asphyxiation.
PLoS Med
4
e156
doi:10.1371/journal.pmed.0040156
9. KoniarisLGSheldonJPZimmersTA
2007
Can lethal injection for execution really be “fixed”.
Lancet
369
352
353
10. TuohyL
2005
Ross autopsy stirs execution debate. Hartford Courant.
Available: http://pqasb.pqarchiver.com/courant/access/880781791.html?dids=880781791 : 880781791&FMT=ABS&FMTS=ABS:FT&type=current&date=Aug+11%2C+2005&author=LYNNE+TUOHY&pub=Hartford+Courant&edition=&startpage=A.1&desc=ROSS+AUTOPSY+STIRS+EXECUTION+DEBATE+. Accessed 5 May 2008
11. LiptakAAguayoT
2006
After problem execution, Governor Bush suspends the death penalty in Florida. The New York Times.
Available: http://query.nytimes.com/gst/fullpage.html?res=9A07E2D81231F935A25751C1A9609C8B63. Accessed 5 May 2008
12. KennedyJBellM
2006
Bush halts executions to review procedure: Florida prison staff inserted the killer's needles poorly, a preliminary autopsy finds.
Orlando Sentinel
13. DworkinG
2003
Lethal injection, autonomy, and the proper ends of medicine: A esponse to David Silver.
Bioethics
17
212
214
14. LiangBA
2006
Special doctor's docket. Lethal injection: policy considerations for medicine.
J Clin Anesth
18
466
470
15. United States Department of Health and Human Services
2005
Federal Policy for the Protection of Human Subjects (the “Common Rule”).
Available: http://www.hhs.gov/ohrp/humansubjects/guidance/45cfr46.htm. Accessed 8 May 2008
16. California Department of Corrections and Rehabilitation Lethal Injection Protocol Review Team
2007
State of California lethal injection protocol review.
Available: http://www.cdcr.ca.gov/News/2007_Press_Releases/docs/ReportToCourt.pdf. Accessed 5 May 2008
17. United States Department of Justice Federal Bureau of Prisons
2007
Execution protocol training agenda, April 17, 2007.
Federal Correctional Complex Terre Haute
18. LynnJBailyMABottrellMJenningsBLevineRJ
2007
The ethics of using quality improvement methods in health care.
Ann Intern Med
146
666
673
19. BailyMABottrellMLynnJJenningsBHastingsC
2006
The ethics of using QI methods to improve health care quality and safety.
Hastings Cent Rep
36
S1
S40
20. TruogRDBrennanTA
1993
Participation of physicians in capital punishment.
N Engl J Med
329
1346
1350
21. ZimmersTALubarskyDA
2007
Physician participation in lethal injection executions.
Curr Opin Anaesthesiol
20
147
151
22. GawandeA
2006
When law and ethics collide—Why physicians participate in executions.
N Engl J Med
354
1221
1229
23. Tennessee Department of Correction
2007
Report on administration of death sentences in Tennessee.
Available: http://www.tennessean.com/assets/pdf/DN71684430.PDF. Accessed 5 May 2008
24. Florida Governor's Commission on Administration of Lethal Injection
2007
Final report with findings and recommendations.
Available: http://sentencing.nj.gov/downloads/pdf/articles/2007/Apr2007/document08.pdf. Accessed 5 May 2008
25. 1990
White v. Napoleon, 897 F.2d 103 (3d Cir. 1990). Available: http://biotech.law.lsu.edu/cases/prisons/white_v_napoleon.htm. Accessed 5 May 2008
26. Committee on Ethical Considerations for Revisions to DHHS Regulations for Protection of Prisoners Involved in Research
2006
Ethical considerations for research involving prisoners. National Academies Press.
Available: http://www.nap.edu/catalog.php?record_id=11692. Accessed 5 May 2008
27. SchwartzJ
2007
Oversite of human subject research: The role of the states (research involving human participants V2). Online Ethics Center at the National Academy of Engineering.
Available: http://www.onlineethics.diamax.com/CMS/research/resref/nbacindex/nbachindex/hschwartz.aspx. Accessed 5 May 2008
28. ShahSK
2008
How lethal injection reform constitutes impermissible research on prisoners.
Am Crim Law Rev
45
29. Arizona State Legislature
2005
Prisoner participation in medical research and plasmapheresis and whole blood programs. Arizona Statutes 31-321 to 31-323.
Available: http://www.azleg.gov/ArizonaRevisedStatutes.asp?Title=31. Accessed 5 May 2008
30. Oregon State Legislature
2007
Experimentation on inmates prohibited; inmate's right to judicial restraint of violation; action for damages.
Oregon Statutes 421.085(2) and 421.085(1). Available: http://www.leg.state.or.us/ors/421.html. Accessed 5 May 2008
31. California State Legislature
2007
Biomedical and behavioral research: General provisions and prohibitions.
California Penal Code 3502 and 3502.5. Available: http://law.justia.com/california/codes/pen/3501-3509.5.html. Accessed 5 May 2008
32. Virginia General Assembly
2007
Criminal justice and corrections: Regulations for human subject research.
Virginia Administrative Code Title 6, 15-26-30C. Available: http://leg1.state.va.us/cgi-bin/legp504.exe?000+reg+6VAC15-26-30. Accessed 5 May 2008
33. United States District Court, Northern District of California
2006
Exhibit A to Motion for TRO, Morales v. Hickman.
Case Number 6–219. San Quentin Operational Procedure No. 770
34. United States District Court, Northern District of California
2006
Memorandum of intended decision; Request for response from defendants, Morales v. Tilton.
Case Number C 06-219, C 06-926. Available: http://www.hrw.org/us/morales121506.pdf. Accessed 5 May 2008
35. Florida Department of Corrections
2007
Florida lethal injection protocol to use after August 16, 2006.
Exhibit A. February 15, 2007. Tallahassee, FL. Available: http://lethal-injection-florida.blogspot.com/2007/02/florida-lethal-injection-protocol-to.html. Accessed 5 May 2008
36. United States District Court, Eastern District of North Carolina
2005
Second Heath Affidavit, Page v. Beck.
Case Number 4-04. Document Number 102
37. United States District Court, Eastern District of North Carolina
2004
Affidavit of Dershwitz, Perkins v. Beck.
Case Number 04-643. Document Number 7, pp
22
31
38. United States District Court, Eastern District of North Carolina
2005
Polk Deposition, Page v. Beck.
Case Number 5 : 04-ct-4. Document Number 98
39. SteinbrookR
2006
New technology, old dilemma—Monitoring EEG activity during executions.
N Engl J Med
354
2525
2527
40. WeiglA
2007
Doc's execution role: «Be present». The News & Observer.
Available: http://www.newsobserver.com/1509/story/559110.html. Accessed 5 May 2008
41. North Carolina Office of Administrative Hearings
2007
Conner et al. v. North Carolina Council of State, 07 Gov. 0238 & 0264 at 6
42. United States District Court, Eastern District of North Carolina
2006
Final Order; Brown v. Beck. Case Number 5 : 06-CT-3018-H.
Available: http://www.law.fsu.edu/library/blogdocs/williebrown.pdf. Accessed 5 May 2008
43. HeathMJStanskiDRPounderDJ
2005
Inadequate anaesthesia in lethal injection for execution.
Lancet
366
1073
1074
author reply 1074–1076
44. Oklahoma Court of Criminal Appeals
2006
Order denying request for stay of execution and setting execution date, Malicoat v. State.
Case Number D-1998-151. Available: http://www.oscn.net/applications/oscn/DeliverDocument.asp?CiteID=446506. Accessed 5 May 2008
45. 2007
Response from the Office of General Counsel, Texas Department of Criminal Justice, dated November 5, 2007, to an Open Records Request by Jon Sheldon, dated October 10, 2007
Štítky
Interné lekárstvo
Článok vyšiel v časopisePLOS Medicine
Najčítanejšie tento týždeň
2008 Číslo 6- Parazitičtí červi v terapii Crohnovy choroby a dalších zánětlivých autoimunitních onemocnění
- Nech brouka žít… Ať žije astma!
- Intermitentní hladovění v prevenci a léčbě chorob
- Co dělat při intoleranci statinů?
- Monoklonální protilátky v léčbě hyperlipidemií
-
Všetky články tohto čísla
- Melanoma: What Are the Gaps in Our Knowledge?
- Adapting the DOTS Framework for Tuberculosis Control to the Management of Non-Communicable Diseases in Sub-Saharan Africa
- Ethical Implications of Modifying Lethal Injection Protocols
- How Might Cocaine Interfere with Brain Development?
- New Medicines for Tropical Diseases in Pregnancy: Catch-22
- Severe Vivax Malaria: Newly Recognised or Rediscovered?
- Subnational Burden of Disease Studies: Mexico Leads the Way
- Guidelines for Reporting Health Research: The EQUATOR Network's Survey of Guideline Authors
- Drug Development for Maternal Health Cannot Be Left to the Whims of the Market
- PLOS Medicine
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Guidelines for Reporting Health Research: The EQUATOR Network's Survey of Guideline Authors
- Ethical Implications of Modifying Lethal Injection Protocols
- Subnational Burden of Disease Studies: Mexico Leads the Way
- Adapting the DOTS Framework for Tuberculosis Control to the Management of Non-Communicable Diseases in Sub-Saharan Africa
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



