-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Hand Sanitiser Provision for Reducing Illness Absences in Primary School Children: A Cluster Randomised Trial
Background:
The potential for transmission of infectious diseases offered by the school environment are likely to be an important contributor to the rates of infectious disease experienced by children. This study aimed to test whether the addition of hand sanitiser in primary school classrooms compared with usual hand hygiene would reduce illness absences in primary school children in New Zealand.Methods and Findings:
This parallel-group cluster randomised trial took place in 68 primary schools, where schools were allocated using restricted randomisation (1∶1 ratio) to the intervention or control group. All children (aged 5 to 11 y) in attendance at participating schools received an in-class hand hygiene education session. Schools in the intervention group were provided with alcohol-based hand sanitiser dispensers in classrooms for the winter school terms (27 April to 25 September 2009). Control schools received only the hand hygiene education session. The primary outcome was the number of absence episodes due to any illness among 2,443 follow-up children whose caregivers were telephoned after each absence from school. Secondary outcomes measured among follow-up children were the number of absence episodes due to specific illness (respiratory or gastrointestinal), length of illness and illness absence episodes, and number of episodes where at least one other member of the household became ill subsequently (child or adult). We also examined whether provision of sanitiser was associated with experience of a skin reaction. The number of absences for any reason and the length of the absence episode were measured in all primary school children enrolled at the schools. Children, school administrative staff, and the school liaison research assistants were not blind to group allocation. Outcome assessors of follow-up children were blind to group allocation. Of the 1,301 and 1,142 follow-up children in the hand sanitiser and control groups, respectively, the rate of absence episodes due to illness per 100 child-days was similar (1.21 and 1.16, respectively, incidence rate ratio 1.06, 95% CI 0.94 to 1.18). The provision of an alcohol-based hand sanitiser dispenser in classrooms was not effective in reducing rates of absence episodes due to respiratory or gastrointestinal illness, the length of illness or illness absence episodes, or the rate of subsequent infection for other members of the household in these children. The percentage of children experiencing a skin reaction was similar (10.4% hand sanitiser versus 10.3% control, risk ratio 1.01, 95% CI 0.78 to 1.30). The rate or length of absence episodes for any reason measured for all children also did not differ between groups. Limitations of the study include that the study was conducted during an influenza pandemic, with associated public health messaging about hand hygiene, which may have increased hand hygiene among all children and thereby reduced any additional effectiveness of sanitiser provision. We did not quite achieve the planned sample size of 1,350 follow-up children per group, although we still obtained precise estimates of the intervention effects. Also, it is possible that follow-up children were healthier than non-participating eligible children, with therefore less to gain from improved hand hygiene. However, lack of effectiveness of hand sanitiser provision on the rate of absences among all children suggests that this may not be the explanation.Conclusions:
The provision of hand sanitiser in addition to usual hand hygiene in primary schools in New Zealand did not prevent disease of severity sufficient to cause school absence.Trial registration:
Australian New Zealand Clinical Trials Registry ACTRN12609000478213
Please see later in the article for the Editors' Summary
Published in the journal: Hand Sanitiser Provision for Reducing Illness Absences in Primary School Children: A Cluster Randomised Trial. PLoS Med 11(8): e32767. doi:10.1371/journal.pmed.1001700
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1001700Summary
Background:
The potential for transmission of infectious diseases offered by the school environment are likely to be an important contributor to the rates of infectious disease experienced by children. This study aimed to test whether the addition of hand sanitiser in primary school classrooms compared with usual hand hygiene would reduce illness absences in primary school children in New Zealand.Methods and Findings:
This parallel-group cluster randomised trial took place in 68 primary schools, where schools were allocated using restricted randomisation (1∶1 ratio) to the intervention or control group. All children (aged 5 to 11 y) in attendance at participating schools received an in-class hand hygiene education session. Schools in the intervention group were provided with alcohol-based hand sanitiser dispensers in classrooms for the winter school terms (27 April to 25 September 2009). Control schools received only the hand hygiene education session. The primary outcome was the number of absence episodes due to any illness among 2,443 follow-up children whose caregivers were telephoned after each absence from school. Secondary outcomes measured among follow-up children were the number of absence episodes due to specific illness (respiratory or gastrointestinal), length of illness and illness absence episodes, and number of episodes where at least one other member of the household became ill subsequently (child or adult). We also examined whether provision of sanitiser was associated with experience of a skin reaction. The number of absences for any reason and the length of the absence episode were measured in all primary school children enrolled at the schools. Children, school administrative staff, and the school liaison research assistants were not blind to group allocation. Outcome assessors of follow-up children were blind to group allocation. Of the 1,301 and 1,142 follow-up children in the hand sanitiser and control groups, respectively, the rate of absence episodes due to illness per 100 child-days was similar (1.21 and 1.16, respectively, incidence rate ratio 1.06, 95% CI 0.94 to 1.18). The provision of an alcohol-based hand sanitiser dispenser in classrooms was not effective in reducing rates of absence episodes due to respiratory or gastrointestinal illness, the length of illness or illness absence episodes, or the rate of subsequent infection for other members of the household in these children. The percentage of children experiencing a skin reaction was similar (10.4% hand sanitiser versus 10.3% control, risk ratio 1.01, 95% CI 0.78 to 1.30). The rate or length of absence episodes for any reason measured for all children also did not differ between groups. Limitations of the study include that the study was conducted during an influenza pandemic, with associated public health messaging about hand hygiene, which may have increased hand hygiene among all children and thereby reduced any additional effectiveness of sanitiser provision. We did not quite achieve the planned sample size of 1,350 follow-up children per group, although we still obtained precise estimates of the intervention effects. Also, it is possible that follow-up children were healthier than non-participating eligible children, with therefore less to gain from improved hand hygiene. However, lack of effectiveness of hand sanitiser provision on the rate of absences among all children suggests that this may not be the explanation.Conclusions:
The provision of hand sanitiser in addition to usual hand hygiene in primary schools in New Zealand did not prevent disease of severity sufficient to cause school absence.Trial registration:
Australian New Zealand Clinical Trials Registry ACTRN12609000478213
Please see later in the article for the Editors' SummaryIntroduction
While the global impact of infectious diseases on death and disability is outweighed by that of non-communicable disease [1], infectious diseases continue to cause ill health in high-income countries [2], and management of the risk of influenza or other pandemics remains important. Children are important in community disease transmission [3] because they have high rates of infectious disease and tend to have more physical contact with peers and adults than other age groups. In addition, when children are unable to attend school because of illness, family members may have to stay home from work to care for them [3]. Therefore, reducing infectious disease among children has the potential for wide-ranging benefits to society.
Reduction of the incidence of many infectious respiratory and gastrointestinal diseases requires interruption of person-to-person transmission, and the school environment is likely to be an important setting for the transmission of infectious diseases because children are in close contact over long periods. Given that it is not feasible to require all infectious children to stay away from school (because of asymptomatic carriage, high incidence, and often mild symptoms), reduction of transmission between children at school could be an effective way of reducing the incidence of infectious disease among children. Hand hygiene is recognised as a key measure to reduce infectious disease transmission in health care settings [4], and interventions that aim to improve hand hygiene compared with usual practice have been shown to reduce infectious disease risk in the community [5], with typically larger effects observed for gastrointestinal [6] than for respiratory [7] diseases. The study settings have varied, but a number of studies have been conducted in schools [8]–[14]. A review of school-based studies noted that they have generally found beneficial effects of hand hygiene interventions; however, reporting of the methodological characteristics of these studies (which may affect the validity of the results) was generally poor, and the analyses were generally inappropriate (without adjustment for the clustered nature of the design) [15]. Additionally, there is a dearth of large pragmatic trials [7]. A range of different hand hygiene interventions have been tested in primary schools, often in combination with hand-washing education, including mandatory hand-washing [12], providing soap for school basins [8], and providing hand sanitiser [9]–[11],[13],[14]. Studies of providing hand sanitiser in schools have tended to be small or to involve rather intense interventions (e.g., daily wiping of all classroom surfaces at lunchtime [13]) that may not be widely feasible.
We aimed to test whether the addition of hand sanitiser in primary school classrooms compared with usual hand hygiene (use of soap and water, mainly in school bathrooms) would reduce illness absences in primary school children in New Zealand. We chose to use hand sanitiser as our hand hygiene modality in preference to increasing use of existing facilities because school bathroom hand-washing facilities are of variable quality [16],[17], which might be a barrier to attempts to increase hand-washing. Improving and maintaining bathroom facilities in a large number of schools would be a major undertaking, and hand sanitiser is an acceptable alternative to hand-washing with soap and water for children [18]. We provided hand sanitiser in classrooms rather than in the bathroom facilities to promote extra hand cleaning in additional to that usually undertaken, and to ensure that use was largely supervised.
Objectives
Our primary objective was to assess whether the provision of hand sanitiser in primary school classrooms in the South Island of New Zealand reduced the incidence rate of absence episodes due to any illness in children, during the winter terms.
Secondary objectives included assessing whether hand sanitiser was effective in reducing the (i) incidence rate of respiratory illness absence episodes, (ii) incidence rate of gastrointestinal illness absence episodes, (iii) incidence rate of absence for any reason, (iv) length of illness episode, (v) length of illness absence episode, and (vi) incidence rate of subsequent illness among other children or adults in the household. We also examined whether the use of hand sanitiser was associated with an increased risk of any skin reactions during the intervention period.
Methods
The protocol for this trial has been published [19], and a brief description of the methods follows.
Ethics Statement
The New Zealand Multi-Region Health and Disability Ethics Committee provided approval for the trial on 13 March 2009 (MEC/09/01/005). School principals gave permission for their school to take part in the study. Parents/guardians (henceforth “caregivers”) of follow-up children gave written consent to be telephoned following their children's absences from school.
Setting and Participants
The study took place in the three cities within the regions covered by the New Zealand Ministry of Health Public Health Units of investigators (M. P. and C. B.). Only city schools were eligible for inclusion because of the increased cost associated with weekly visits to schools more widely distributed within the regions.
We evaluated the effectiveness of the intervention over the winter school terms (27 April to 25 September 2009) by measuring the absence rates of all children enrolled at the participating schools at any time during the study period, and by collecting more detailed information on the absences of a subgroup of these children, the follow-up group, whose caregivers were contacted via telephone when the child had been absent from school. We aimed to recruit 50 children from each school into the follow-up group. At the beginning of March 2009, letters inviting participation in the study (including a consent form and baseline questionnaire) were distributed by the school to students who had been randomly selected from the school roll.
All eligible schools were invited to take part in the study. The study sample comprised primary schools that met the inclusion criteria below and whose principal consented for the school to participate in the trial, be randomised, and potentially receive the hand sanitiser.
Inclusion Criteria
All schools (i) with at least 100 children in school years one to six (aged 5 to 11 y) enrolled at the school in November 2008; (ii) located within the city boundaries of Christchurch, Dunedin, or Invercargill, in the South Island of New Zealand; (iii) not “special schools” (e.g., schools for children with deafness or disability); and (iv) either not currently using hand sanitiser products or willing to not use hand sanitiser products for the period of the trial if they were randomised to the control group were eligible to participate in the trial.
Children were eligible to participate in the follow-up group, for whom more detailed information on absences was collected, if they attended a school year 1 to 6 class in one of the included schools at the beginning of the second school term in 2009 (the end of April), and their caregivers completed the consent form indicating that they were willing to be telephoned following their child's absences and that they were able to take part in telephone interviews in English.
Exclusion Criteria
Potentially eligible follow-up children were excluded if a caregiver was an investigator or study personnel of the trial, or if the principal of the school directed us not to approach their family.
Intervention
Children in intervention schools received an approximately 30-min in-class hand hygiene education session and were also instructed in the use of hand sanitiser and asked to use it after coughing/sneezing, and on the way out of the classroom for morning break and for lunch. Caregivers of children at intervention schools were sent a letter home with the school newsletter explaining the study and asking them to let their child's teacher know if they did not wish their child to use the hand sanitiser, or if during the study they wished their child to stop using the sanitiser for any reason.
During the school holidays in April 2009, “no touch” dispensers, which dispensed approximately 0.45-ml of alcohol-based sanitiser (>60% ethanol) when hands were placed under an infrared sensor, were fitted in all classrooms in intervention schools. School liaison research assistants subsequently visited each classroom weekly to top up the sanitiser during the course of the study, which continued from 27 April to 25 September 2009 (20 school weeks). The quantity used in each classroom was recorded.
Control
Children in the control schools received the same in-class hand hygiene education sessions as the intervention schools (minus the instructions on classroom hand sanitiser use), to ensure that the children in the two study groups were equivalent in their exposure to hand hygiene education prior to the study.
Outcome
Table 1 shows the outcome measures that were planned and collected. The primary outcome was the number of absence episodes due to any illness among follow-up children.
Tab. 1. Planned outcomes from protocol [19] and outcomes actually measured. ![Planned outcomes from protocol <em class="ref">[19]</em> and outcomes actually measured.](https://www.prelekara.sk/media/cache/resolve/media_object_image_small/media/image/0e1b6c61b43d70a04dffa65702fe1d7e.png)
Follow-up children only. Sample Size
The primary outcome was the number of absence episodes due to illness. Monitoring by the Public Health Unit of absences among primary school children in Dunedin and Invercargill in 2006 and 2007 found an average of 11 absences reported as due to illness per 100 pupil-weeks, equivalent to 2.2 absences per pupil over 20 wk (M. Poore, personal communication). The trial was powered at 80% to detect a 20% reduction in the incidence rate of absence episodes due to illness (from 2.2 to 1.76 episodes per pupil over 20 wk) [5]. Assuming recruitment of 50 follow-up children per school and an intra-cluster correlation of 0.15, 27 schools (1,350 follow-up children) per group would be sufficient to detect a 20% reduction in rates with 80% power (two-sided significance level of 5%). Allowing for 20% attrition in the participation of schools, we aimed to recruit 34 schools per group.
Randomisation and Allocation Concealment
Schools were randomly allocated to either the hand sanitiser or control group using restricted randomisation. Three strata were defined by geographical area (cities of Christchurch, Dunedin, or Invercargill), and within each stratum schools were randomly allocated with equal probability (1∶1 randomisation ratio) to the hand sanitiser or control group (i.e., 34 schools per group). City was chosen as a stratification variable because outbreaks of gastrointestinal illness or flu may be restricted to an area, and could therefore confound the estimated intervention effect if the intervention groups were not equally distributed within cities.
The study statistician (J. E. M.) was provided with only a numeric school code and its area, and randomised schools to “A” or “B” using random numbers generated by Stata/MP version 10.1 for Windows (StataCorp). Independently, and prior to receiving the allocation list, P. P. randomly allocated “A” and “B” to intervention or control. Randomisation of all schools was undertaken at one time, and the randomisation list was held by P. P. until analysis was complete.
Blinding
Due to the nature of the intervention, it was not possible to blind the children, school administrative staff, or the school liaison research assistants. The investigators not involved in running the trial (J. E. M., R. A., M. P., and C. B.), the telephone interviewers (outcome assessors), and the statistician (J. E. M.) were blinded to the group allocation until after the analysis was complete.
Data Collection
The baseline questionnaire sent to the caregivers of follow-up children collected self-reported information on household composition, socio-demographic variables (ethnicity, education, occupation, income, ages of children), paid and unpaid work, family health, and hand hygiene practices.
During the study period, school liaison research assistants visited all schools weekly and collected absence information from the school's records for the previous week for all children in the school. When a follow-up child had been absent and the reason for the absence was recorded as “medical”, “illness”, or “unknown”, the caregiver of the child was telephoned. Contact occurred approximately 9 d after the absence, and the caregiver was asked about the reason for the absence. In cases of illness, further questions were asked about the child's symptoms and their duration, whether others in the family had had the same symptoms, how the child had been cared for during the absence, and the cost of any health care sought because of the illness.
Schools provided information on the total number of children enrolled at the beginning of the study, halfway through the study (when there was a holiday), and at the end of the study period. At the end of the study, the total amount of hand sanitiser used by each classroom in the intervention schools was measured. In addition, we attempted to contact each follow-up child's caregiver, irrespective of whether the child had been absent, to ask about possible adverse effects (skin reactions).
Analyses
Estimates of intervention effectiveness (incidence rate ratios [IRRs] or odds ratios [ORs]) for follow-up children were calculated from marginal models using generalised estimating equations (GEEs), with robust variance estimation, to account for correlation of responses of children within schools. An exchangeable correlation structure was specified, whereby responses from the same school were assumed to be equally correlated. If the estimated intra-cluster correlation (ICC) from the GEE was negative, the model was refitted assuming an independent correlation structure, i.e., an ICC of zero. This approach yields conservative estimates of standard errors and follows the recommendations of others in assuming that in this context, the likely explanation for a negative ICC is sampling variability and not a true negative ICC [20],[21]. Confidence limits for ICCs were calculated through bootstrapping, using a combination of the bootstrap and xtgee commands in Stata. Bootstrapping allowed for clustering of responses within schools. Bias-corrected 95% bootstrap confidence intervals were calculated from 5,000 replicates.
Models were adjusted for the stratification variable, which represented city (Christchurch, Dunedin, or Invercargill). As part of the pre-specified secondary analyses, we also fitted models adjusting for the potential confounder school-level deprivation (in addition to city). School-level deprivation reflects the proportion of students who live in more or less advantaged communities, using information from the census on household income, occupation, household crowding, educational qualifications, and income support [22].
For the primary outcome (number of absence episodes due to any illness) we undertook a pre-specified per-protocol analysis that included only intervention and control schools that complied with the protocol. Protocol compliance for the intervention schools was defined as dispensing a volume equivalent to at least 45 ml per child of hand sanitiser solution over the trial period, and for the control schools, not introducing hand sanitisers. Marginal logistic and negative binomial regression models were employed for binary and count outcomes, respectively. The negative binomial heterogeneity parameter used in the marginal models was first estimated from fitting a generalised negative binomial model.
Estimates of the intervention effectiveness for all children were calculated from models fitted on data aggregated to the level of the school. We were unable to analyse absence data from the school rolls at the level of the child, since we could not uniquely identify children (e.g., when they changed class rooms). Negative binomial regression was used to estimate the effectiveness of the intervention, adjusting for the stratification and confounding variables described above.
No adjustment for multiple testing was undertaken. All models were fitted using the statistical package Stata version 12 (StataCorp).
Deviations from Published Protocol
Some changes were made to the protocol following its publication [19]. All changes were made prior to the commencement of analysis and are summarised in Table 2 (a detailed explanation is available in Deviations S1).
Tab. 2. Summary of protocol deviations. 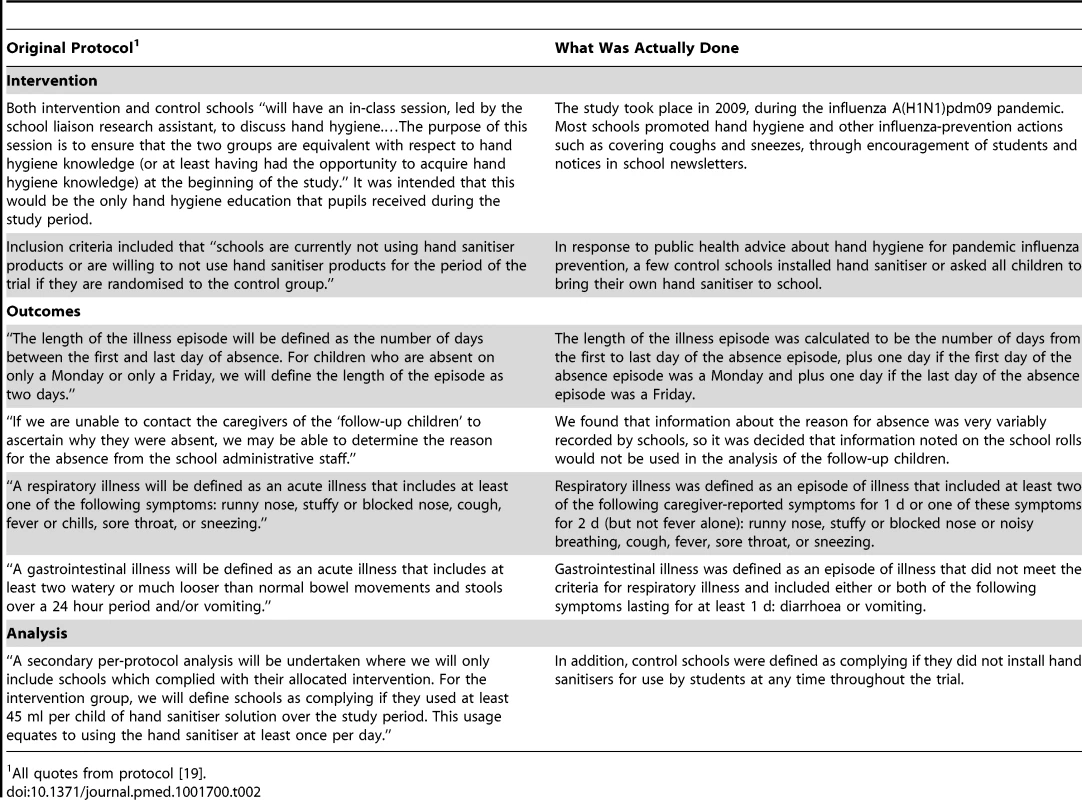
All quotes from protocol [19]. Trial Registration
The trial was registered with the Australian New Zealand Clinical Trials Registry (ACTRN12609000478213). The trial is recorded as “retrospectively registered”. Many aspects of the intervention (e.g., the specifics of the education session) and data collection processes (e.g., frequency with which the absence data would be collected) were negotiated with the schools to ensure they were acceptable. These negotiations necessarily took place in the school term immediately prior to the roll-out of the intervention. The trial was not registered until these details had been confirmed, which occurred just before the commencement of the trial. Trial registration was first submitted to the registry on 11 March 2009, the same week that we first wrote to caregivers of children asking them whether they would be willing to have a telephone interview following any absences of their children. After some delay the registry asked for some clarification and further details, which were provided, and the trial was registered on 12 June 2009. Data collection had begun on 27 April, but no changes were required by the registry, or made by the investigators, to the methods and measures of the study following the initial registration submission in March.
Results
Participants
Sixty-eight schools took part in the study; 34 were randomly allocated to each arm of the trial. Figure 1 shows the progress of schools and children through the trial. Participation was higher among smaller schools (64% of schools with a roll size of 100–199 students versus 28% of schools with a roll size of >300 students) and among schools in Dunedin (74%, versus 41% in Christchurch and 50% in Invercargill). Invitations to take part in follow-up telephone interviews if children were absent from school (i.e., follow-up children) were sent to the caregivers of a total of 6,720 children (up to 100 per school; three children were not approached at the instruction of the school principal), and the caregivers of 2,443 (36.4%) children consented. Consent was higher among caregivers of children from schools in Dunedin (40%, versus 35% in Christchurch and 30% in Invercargill) and in less disadvantaged schools (45% in the least disadvantaged schools, versus 19% in the most disadvantaged schools).
Fig. 1. Flow diagram of the progress of schools and children through the trial. 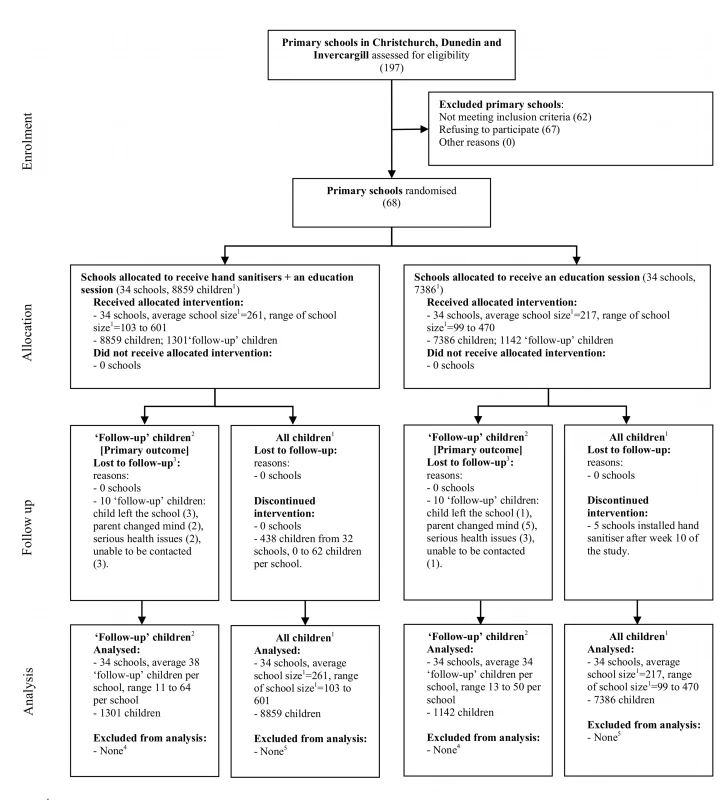
1Includes all children in school years 1 to 6 (generally aged from 5 to 11 y). The number given here is the average roll over the period of the trial. 2Follow-up children were a randomly selected sample of all children attending the participating schools, whose caregivers were followed up for detailed information about their illness absences. The primary outcome, absence episodes due to illness, is measured only in this group of children. 3We may not have been informed about all children who left the schools. 4All follow-up children were included in the analysis. The period of time that each child was in the trial (the exposure period) was adjusted for through the statistical model. 5All children who had an absence (for any reason) were included in the analysis, even if they were lost to follow-up at some point (e.g., moved schools). The exposure period was calculated as the average of the school roll over the period of the trial (multiplied by 100; the number of school days that were encompassed by the trial period). Figure adapted from [29]. Baseline Characteristics
Caregivers of children in intervention schools were more likely to agree to have their children participate as follow-up children than those in control schools (39% versus 34%). Table 3 summarises the school and follow-up children socio-demographic characteristics. Control schools were less advantaged than intervention schools, but otherwise the groups were well balanced.
Tab. 3. Baseline characteristics. 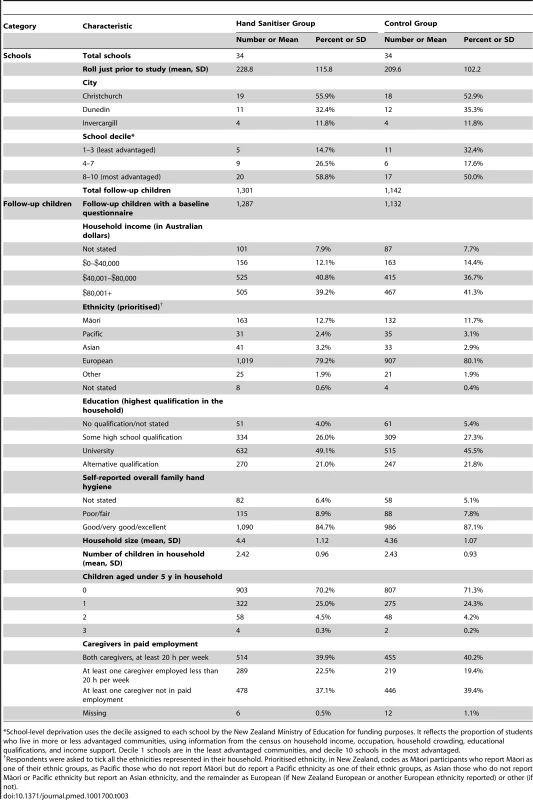
*School-level deprivation uses the decile assigned to each school by the New Zealand Ministry of Education for funding purposes. It reflects the proportion of students who live in more or less advantaged communities, using information from the census on household income, occupation, household crowding, educational qualifications, and income support. Decile 1 schools are in the least advantaged communities, and decile 10 schools in the most advantaged. Absences
Among the 2,443 follow-up children there were 5,766 absences identified from the school rolls, 5,134 of which were recorded as “medical”, “illness”, or “unknown”. Post-absence phone calls resulted in establishing an absence reason for 3,846 absences (74.9%), of which 2,833 were identified as being due to illness (Figure 2). There were 608 absences (13.4%) that should have resulted in a call but did not, 284 in the intervention group and 324 in the control group. Reasons for post-absence calls not being made included errors in identifying that a new absence episode had occurred (i.e., miscounting the gap between the end of one absence episode and the beginning of another) and, for one school in the control group, an administrative error that meant that some follow-up children were not identified as such in the database of absences.
Fig. 2. Flow diagram outlining process for identifying the reason for school absences. 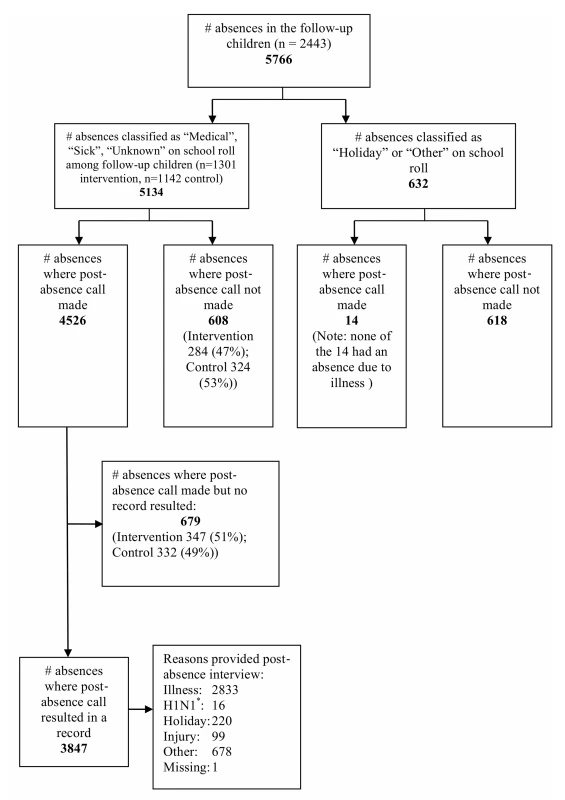
“H1N1” absences (asterisk) were absences where the child had been asked to stay at home because of possible contact with a known case of H1N1, rather than because they were sick themselves. Intervention Fidelity
A change to the hand sanitiser solution was made in 41 of 396 classrooms (in 9 of 34 schools) halfway through the trial (after 10 wk). Some children had become reluctant to use the initial hand sanitiser product before eating their lunch, because they reported tasting the sanitiser on their fingers and food. We identified a product that did not have a “flavour” and provided that to classes where this complaint had been made. Both brands of sanitiser contained >60% ethanol. Following this change to the product, the median classroom difference in sanitiser usage between the first 10 wk and the second 10 wk among classes that switched products was −220 ml; the inter-quartile range of the usage difference was −420 ml to 645 ml.
All schools in the intervention group complied with the protocol of dispensing a volume equivalent to at least 45 ml per child of hand sanitiser solution over the trial period. The average hand sanitiser solution dispensed per child over the 34 schools was 94 ml (standard deviation = 19). We had not anticipated that control schools would install hand sanitiser, because the inclusion criteria for the study required that they agree not to. However, in view of the pandemic of influenza A(H1N1)pdm09 during the study period, five control schools did install hand sanitiser in response to public health advice. Most schools also provided additional education or reminders about hand hygiene.
Effectiveness of Intervention
Follow-up children
The rate of absence episodes due to any illness (primary outcome) was similar in the hand sanitiser (1.21 per 100 child-days) and control (1.16 per 100 child-days) groups, and the confidence interval for the IRR (IRR 1.06, 95% CI 0.94 to 1.18) excluded a clinically important difference (Table 4). Furthermore, there was no evidence that hand sanitiser was effective in reducing rates of respiratory or gastrointestinal illness episodes, or the length of the illness or illness absence episodes, to any clinically important degree. Nor did the rate of occurrence of the same illness among other members of the household subsequent to an illness in a follow-up child differ between groups. The percentage of children who had experienced a skin reaction over the period of the trial was similar between groups (10.4% hand sanitiser versus 10.3% control, OR 1.01, 95% CI 0.78 to 1.30). Pre-specified secondary analyses that adjusted for school disadvantage, in addition to city (design strata), yielded intervention effectiveness estimates that did not change appreciably compared with models that adjusted only for the design strata (Analysis S1).
Tab. 4. Estimates of effectiveness of hand sanitiser on outcome measures. 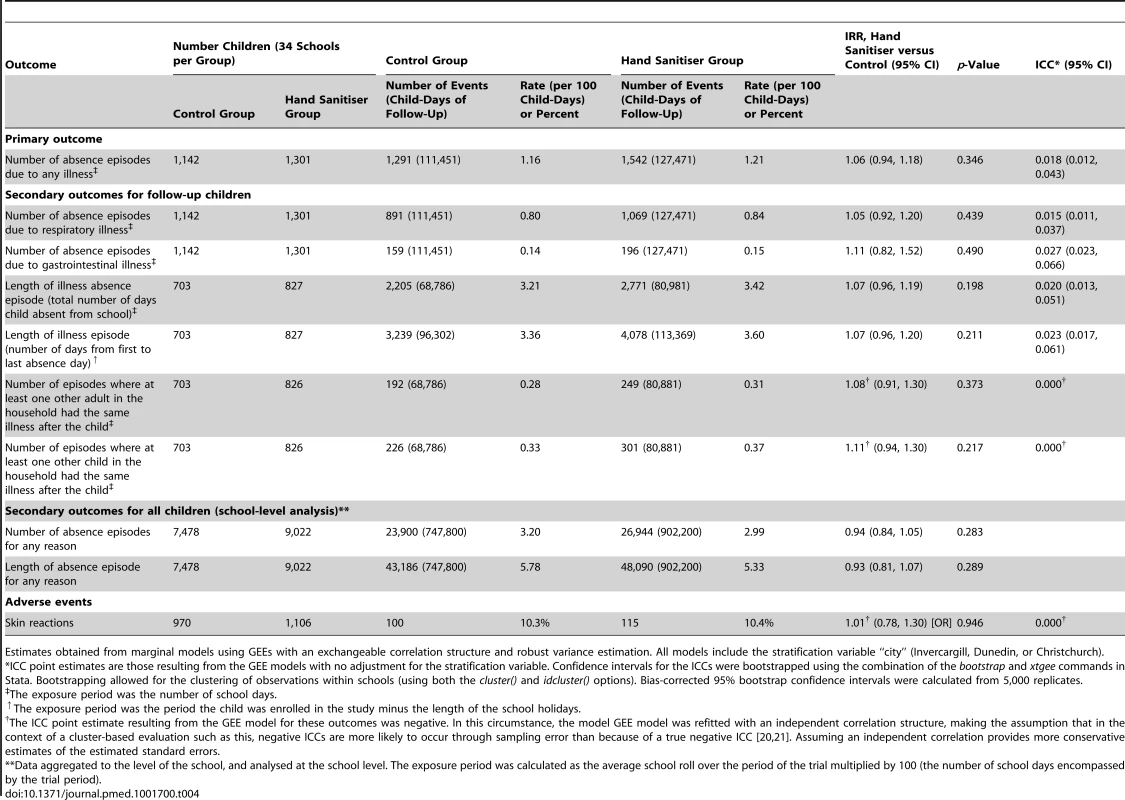
Estimates obtained from marginal models using GEEs with an exchangeable correlation structure and robust variance estimation. All models include the stratification variable “city” (Invercargill, Dunedin, or Christchurch). All children
The rate of episodes of absence for any reason, and the length of episodes, calculated from absence data collected in the school rolls, did not differ importantly between the intervention and control groups (Table 4).
Per-protocol analysis
The per-protocol analysis, with the five control schools removed that did not comply with the protocol (i.e., introduced hand sanitiser), did not modify the intervention effectiveness for the primary outcome, rate of absence episodes due to any illness, in an important way (per-protocol intervention effectiveness estimate 1.03, 95% CI 0.93 to 1.14, p = 0.582).
Intra-cluster correlations
Estimated ICCs for all outcomes were very small (Table 4), with point estimates ranging from 0.000 to 0.027.
Discussion
Main Findings
We undertook a cluster randomised trial to estimate the effectiveness of hand sanitiser in reducing illness absence episodes in children in primary schools. The trial did not demonstrate that hand sanitiser reduced school absences due to illness, school absences due to respiratory or gastrointestinal illness, length of illness or of illness absence episode, or the number of times other members of the household became sick, in children followed up with post-absence interviews. In addition, skin problems were not found to be more common among children at schools where hand sanitiser was provided. The rates of absences for any reason, and of lengths of absence episodes, calculated from absence information collected in school rolls, were also similar between the intervention and control groups.
Strengths
The trial was designed to minimise bias arising from design elements. While cluster trials are less efficient compared with individually randomised trials (although the estimated ICCs in this trial were small), this design reduces contamination that would arise if children within the same classroom or school were allocated randomly to the intervention and control groups. Furthermore, it evaluates the intervention as it would be implemented in the real world (i.e., provided to schools rather than individuals). There was adequate allocation concealment of the randomisation sequence (reducing the possibility of selection bias). Confounding by variability in viral incidence [7] was minimised through stratification by city. Outcome assessors were blind to group allocation (reducing the possibility of detection bias). Participants were not blinded to their allocation, but the use of school absences as an outcome reduces the likelihood of bias that can occur when self-reported illness is the outcome—participants' beliefs about the intervention may affect their threshold for reporting mild and non-specific symptoms such as coughs and colds, whereas caregivers' decisions to keep children at home are not likely to be so affected. A high proportion of absences were followed up with a telephone call to establish the cause of the absence, and absences that did not result in a call or where the call did not result in a record (i.e., the caregiver could not be contacted) were evenly distributed between intervention and control children (Figure 2). A further strength is the collection of absence data from school rolls, which was measured on all children and was unlikely to be affected by selection, detection, or performance biases.
Limitations
Potential limitations of the study can be classified as issues of selection, measurement, and implementation. A higher proportion of schools in the control group were disadvantaged. We did not stratify by school disadvantage because we could not find good evidence that school disadvantage is associated with absence rates in New Zealand, so it would be unlikely to confound the effectiveness of the intervention. Pre-specified secondary analyses that adjusted for school disadvantage, in addition to city (design strata), yielded intervention effectiveness estimates that did not change appreciably compared with models that adjusted only for the design strata (Analysis S1). In fact, if school disadvantage was associated with more absences (which would be the expected direction of association, given known patterns of disease and disadvantage), it would bias the estimated intervention effect in the direction of showing greater effectiveness of hand sanitiser use than actually exists.
Another selection issue is that, as often occurs in cluster trials [23], individual participants (follow-up children) were recruited after the clusters had been randomised and the caregivers knew the allocation of the cluster. The rate of consent to be followed up after absences was not high overall (36.4%), and was lower among more disadvantaged schools. However, the effectiveness of the intervention in the analysis controlling for school disadvantage was essentially unchanged. We are unable to determine in detail whether follow-up children differed from those who did not agree to be followed up. However, despite the higher proportion of disadvantaged schools in the control group, the income and education of follow-up children's families was well balanced between the intervention and control groups, suggesting that the follow-up children in either the intervention or control group may not have been representative of their school populations. The rate of absence due to illness among controls was lower than the rate observed in data collected by the public health unit in previous years, on which our sample size calculations were based. It is possible that caregivers of follow-up children had a particular interest in hygiene and that their children were already practising good hand hygiene, and so no further benefit was possible for them. Nonetheless, the lack of effectiveness of the intervention on absences among all children suggests that our findings for illness absences are valid.
While we did not quite achieve the planned sample size of 1,350 follow-up children per group, we still obtained precise estimates of the intervention effects. This occurred because the ICCs observed in the trial (point estimates ranging from 0.000 to 0.027) were much smaller than the conservative estimate we had used in the sample size calculation (0.15).
We used telephone interviews to collect information on reasons for absence. This is less accurate than, for example, physically examining absent children, but is the only practicable way of collecting these data on the scale necessary for this study. Because our resources allowed for only a weekly visit to each school to collect data, and because of the processing time for identifying absences for follow-up children, these interviews were conducted approximately 9 d following the absences. This may have led to some inaccurate recall, but this is unlikely to have differed by group. Information on reasons for absence was incomplete, because of the failure to identify some follow-up children's absences and the inability to contact caregivers in some cases. However, these issues occurred with similar frequency in the intervention and control groups, and we do not expect the lack of a telephone call to be associated with the reason for absence, so we do not believe that these factors would have introduced meaningful bias.
Despite a pilot study that did not identify the taste of the sanitiser as a barrier to use, this did become an issue in some schools, and we changed the product in 10% of classrooms halfway through the study period. However, the quantity of sanitiser used by these classrooms following the change, which varied widely and in many cases decreased, does not support the idea that if a tasteless sanitiser had been used throughout the study, it would have been used more and would therefore have been more likely to be effective in reducing illness. The education sessions provided to intervention schools emphasised that washing hands after a number of activities is important, and that the hand sanitiser was for additional hand cleaning, reducing the likelihood of intervention children substituting hand sanitiser for use of school bathroom facilities and not actually increasing hand hygiene overall.
Performing large prospective studies of hand hygiene with reasonably long follow-up in schools is a major undertaking, and external events that may affect the purity of the design cannot be prevented [24]. The 2009 influenza A(H1N1)pdm09 pandemic began shortly after this study commenced, and by half-way through the study, there was considerable effort by government agencies to encourage the public, including schools, to practice good hand hygiene, including reminders of its importance with all media releases about the pandemic both nationally and by local health services. Poster reminders about hand hygiene, and in some cases hand sanitiser, were provided in many places such as public venues, shopping centres, and hospitals. Most schools in this study responded by encouraging better hand hygiene and social distancing via school newsletters and reminders to children, and some control schools installed hand sanitiser (we do not have information for children in the study about the individual use of hand sanitiser provided by caregivers). While having contemporaneous controls should deal appropriately with changes that occur over time that are unrelated to the intervention (and this provides a good example of why controlled trials are necessary), there are two potential consequences of the schools' actions that may have affected the intervention effectiveness. First, although children in intervention schools could be argued to have had better opportunities than control children to respond to hand hygiene messaging by using sanitiser, the more intensive hand hygiene education that may have ensued as a result of the pandemic may have increased hand hygiene behaviours in all schools, decreasing the measurable impact of the intervention. Second, the introduction of hand sanitisers in some control schools introduced contamination across groups, potentially biasing the intervention effect. However, the per-protocol analysis did not modify the intervention effectiveness for the primary outcome in an important way.
Generalisability
The participation rate among eligible schools (50%) was not high; however, in a randomised controlled trial this is an issue of generalisability (external validity) rather than bias in the measured intervention effect (internal validity). Participating schools tended to be smaller, but all had at least 100 pupils, and it seems unlikely that the effectiveness of hand hygiene would differ depending on school size within this range, suggesting that our findings are generalisable to primary school children in high-income countries.
These Results in the Context of Other Studies
A systematic review and meta-analysis published by Aiello et al. in 2008 included a number of studies of the effect of hand hygiene interventions on gastrointestinal, respiratory, and combined illnesses in community settings, many of which were schools [5]. They report a rate ratio of “combined illnesses” of 0.74 (95% CI 0.59 to 0.93) for interventions involving alcohol-based hand sanitiser compared with control, based on two studies [11],[25]. Both these studies were set in primary schools, and both were funded by manufacturers of hand sanitiser. One appears to be a non-randomised comparison of sanitiser provision with usual practice [11]; the other was a cross-over study that compared an education session with sanitiser provision plus an enhanced education session, undertaken in a single school with 5 wk of follow-up in each intervention period [25]. Aiello et al. note in their review that studies that did not randomise and those with shorter follow-up found stronger effects on combined illnesses, and this may partly explain why our results differ from those of these two previous studies. Aiello et al. identified no studies that compared intervention with an alcohol-based hand sanitiser with control and measured respiratory or gastrointestinal illnesses separately. However, there were a number of studies that compared provision of alcohol-based hand sanitiser plus hand hygiene education with a control group (this is not the same as our study since we provided hand hygiene education to both the intervention and control groups). For these studies, rate ratios for the intervention group were 0.77 (95% CI 0.52 to 1.13; five studies) for gastrointestinal illness, 0.93 (95% CI 0.84 to 1.03; six studies) for respiratory illness, and 0.79 (95% CI 0.67 to 0.93; three studies) for combined illnesses. Since this systematic review, the results of two cluster randomised controlled trials conducted in primary schools in the US have been reported [9],[13]. One, a trial that randomised ten schools, found a reduction in laboratory-confirmed influenza A infections in the intervention group, but there was no difference in the study's pre-specified primary outcome of all influenza infections (adjusted IRR 0.81, 95% CI 0.54 to 1.23) [9]. The other, which randomised six “teams” of classes either to an intervention that included hand sanitiser and daily surface cleaning or to usual practice, and followed up for 8 wk, found a reduction in school absences due to gastrointestinal illness (adjusted IRR 0.91, 95% CI 0.87 to 0.94) but not absences due to respiratory illness (adjusted IRR 1.10, 95% CI 0.97 to 1.24) [13].
Implications
This study shows that adding hand sanitiser to usual school hand hygiene practices in New Zealand does not prevent disease of a severity to warrant school absence. In particular, we found that during an influenza pandemic [26],[27], when any impact of hand sanitiser would be particularly important, providing hand sanitiser was not an effective mechanism for reducing illness absence. Our study does not address the effectiveness of hand sanitiser for reducing specific infections such as influenza, and we have not shown that hand hygiene itself is not important, nor that hand sanitiser as a method of hand hygiene is not useful. Where clean water is scarce, hand sanitiser could be a useful alternative [28]. However, our results suggest that in a high-income country, putting resources into extra hand hygiene by providing hand sanitiser in classrooms may not be effective in reducing illness absences.
We undertook this trial because school absence due to illness is common in New Zealand, and an intervention that could halve it, as some trials suggested at the time we designed the study, or even reduce it by 25%, as suggested by the meta-analysis by Aiello et al. [5], would be important and useful. However, good-quality and more recent studies in schools in high-income countries, including ours, show that the addition of hand sanitiser to existing hand hygiene facilities does not result in important benefits. An updated systematic review of the impact of different hand hygiene interventions for reducing school absence in high-income countries should be a high priority before further such trials are carried out.
Supporting Information
Zdroje
1. MurrayCJ, VosT, LozanoR, NaghaviM, FlaxmanAD, et al. (2012) Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380 : 2197–2223.
2. BakerMG, BarnardLT, KvalsvigA, VerrallA, ZhangJ, et al. (2012) Increasing incidence of serious infectious diseases and inequalities in New Zealand: a national epidemiological study. Lancet 379 : 1112–1119.
3. NeuzilKM, HohlbeinC, ZhuY (2002) Illness among schoolchildren during influenza season: effect on school absenteeism, parental absenteeism from work, and secondary illness in families. Arch Pediatr Adolesc Med 156 : 986–991.
4. PittetD (2005) Clean care is safer care: the first global challenge of the WHO World Alliance for Patient Safety. Infect Control Hosp Epidemiol 26 : 891–894.
5. AielloAE, CoulbornRM, PerezV, LarsonEL (2008) Effect of hand hygiene on infectious disease risk in the community setting: a meta-analysis. Am J Public Health 98 : 1372–1381.
6. EjemotRI, EhiriJE, MeremikwuMM, CritchleyJA (2008) Hand washing for preventing diarrhoea. Cochrane Database Syst Rev 2008: CD004265.
7. JeffersonT, Del MarCB, DooleyL, FerroniE, Al-AnsaryLA, et al. (2011) Physical interventions to interrupt or reduce the spread of respiratory viruses. Cochrane Database Syst Rev 2011: CD006207.
8. BowenA, MaH, OuJ, BillhimerW, LongT, et al. (2007) A cluster-randomized controlled trial evaluating the effect of a handwashing-promotion program in Chinese primary schools. Am J Trop Med Hyg 76 : 1166–1173.
9. StebbinsS, CummingsDA, StarkJH, VukotichC, MitrukaK, et al. (2011) Reduction in the incidence of influenza a but not influenza b associated with use of hand sanitizer and cough hygiene in schools: a randomized controlled trial. Pediatr Infect Dis J 30 : 921–926.
10. GuinanM, McGuckinM, AliY (2002) The effect of a comprehensive handwashing program on absenteeism in elementary schools. Am J Infect Control 30 : 217–220.
11. HammondB, AliY, FendlerE, DolanM, DonovanS (2000) Effect of hand sanitizer use on elementary school absenteeism. Am J Infect Control 28 : 340–346.
12. Nandrup-BusI (2009) Mandatory handwashing in elementary schools reduces absenteeism due to infectious illness among pupils: a pilot intervention study. Am J Infect Control 37 : 820–826.
13. SandoraTJ, ShihMC, GoldmannDA (2008) Reducing absenteeism from gastrointestinal and respiratory illness in elementary school students: a randomized, controlled trial of an infection-control intervention. Pediatrics 121: e1555–e1562.
14. WhiteCG, ShinderFS, ShinderAL, DyerDL (2001) Reduction of illness absenteeism in elementary schools using an alcohol-free instant hand sanitizer. J Sch Nurs 17 : 258–265.
15. MeadowsE, Le SauxN (2004) A systematic review of the effectiveness of antimicrobial rinse-free hand sanitizers for prevention of illness-related absenteeism in elementary school children. BMC Public Health 4 : 50.
16. ReevesLM, PriestPC, PooreMR (2012) School toilets: facilitating hand hygiene? A review of primary school hygiene facilities in a developed country. J Public Health 34 : 483–488.
17. JewkesRK, O'ConnorBH (1990) Crisis in our schools: survey of sanitation facilities in schools in Bloomsbury health district. BMJ 301 : 1085–1087.
18. VesseyJA, SherwoodJJ, WarnerD, ClarkD (2007) Comparing hand washing to hand sanitizers in reducing elementary school students' absenteeism. Pediatr Nurs 33 : 368–372.
19. McKenzieJ, PriestP, AudasR, PooreM, BruntonC, et al. (2010) Hand sanitisers for reducing illness absences in primary school children in New Zealand: a cluster randomised controlled trial study protocol. Trials 11 : 7.
20. EldridgeSM, UkoumunneOC, CarlinJB (2009) The intra-cluster correlation coefficient in cluster randomized trials: a review of definitions. Int Stat Rev 77 : 378–394.
21. UkoumunneOC, GullifordMC, ChinnS, SterneJA, BurneyPG (1999) Methods for evaluating area-wide and organisation-based interventions in health and health care: a systematic review. Health Technol Assess 3: iii–92.
22. New Zealand Ministry of Education (2009) How the decile is calculated. Available: http://www.minedu.govt.nz/NZEducation/EducationPolicies/Schools/SchoolOperations/Resourcing/OperationalFunding/Deciles/HowTheDecileIsCalculated.aspx. Accessed 23 March 2014.
23. EldridgeS, KerryS, TorgersonDJ (2009) Bias in identifying and recruiting participants in cluster randomised trials: what can be done? BMJ 339: b4006.
24. GeraldLB, GeraldJK, McClureLA, HarringtonK, ErwinS, et al. (2011) Redesigning a large school-based clinical trial in response to changes in community practice. Clin Trials 8 : 311–319.
25. MortonJ, SchultzA (2004) Healthy hands: use of alcohol gel as an adjunct to handwashing in elementary school children. J Sch Nurs 20 : 161–167.
26. Lopez L, Huang QS (2010) Influenza in New Zealand 2009. Wellington: Institute of Environmental Science and Research.
27. Bandaranayake D, Huang QS, Bissielo A, Wood T (2010) Seroprevalence of the 2009 influenza A (H1N1) pandemic in New Zealand. Wellington: Institute of Environmental Science and Research.
28. LubySP, KadirMA, Yushuf SharkerMA, YeasminF, UnicombL, et al. (2010) A community-randomised controlled trial promoting waterless hand sanitizer and handwashing with soap, Dhaka, Bangladesh. Trop Med Int Health 15 : 1508–1516.
29. CampbellMK, ElbourneDR, AltmanDG (2004) CONSORT statement: extension to cluster randomised trials. BMJ 328 : 702–708.
Štítky
Interné lekárstvo
Článok vyšiel v časopisePLOS Medicine
Najčítanejšie tento týždeň
2014 Číslo 8- Parazitičtí červi v terapii Crohnovy choroby a dalších zánětlivých autoimunitních onemocnění
- Intermitentní hladovění v prevenci a léčbě chorob
- Statinová intolerance
- Co dělat při intoleranci statinů?
- Monoklonální protilátky v léčbě hyperlipidemií
-
Všetky články tohto čísla
- Observational Studies: Getting Clear about Transparency
- Scaling up Rural Sanitation in India
- Intervention Synthesis: A Missing Link between a Systematic Review and Practical Treatment(s)
- From Intense Rejection to Advocacy: How Muslim Clerics Were Engaged in a Polio Eradication Initiative in Northern Nigeria
- Ethics, Economics, and the Use of Primaquine to Reduce Falciparum Malaria Transmission in Asymptomatic Populations
- Hand Sanitiser Provision for Reducing Illness Absences in Primary School Children: A Cluster Randomised Trial
- Protective Efficacy and Safety of Three Antimalarial Regimens for the Prevention of Malaria in Young Ugandan Children: A Randomized Controlled Trial
- Heart Failure: Gaps in Knowledge and Failures in Treatment
- Staffing of Healthcare Workers and Patient Mortality: Randomized Trials Needed
- Associations between Stroke Mortality and Weekend Working by Stroke Specialist Physicians and Registered Nurses: Prospective Multicentre Cohort Study
- Women's Access and Provider Practices for the Case Management of Malaria during Pregnancy: A Systematic Review and Meta-Analysis
- Stress Hyperglycaemia in Hospitalised Patients and Their 3-Year Risk of Diabetes: A Scottish Retrospective Cohort Study
- The Effect of India's Total Sanitation Campaign on Defecation Behaviors and Child Health in Rural Madhya Pradesh: A Cluster Randomized Controlled Trial
- Heart Failure Care in Low- and Middle-Income Countries: A Systematic Review and Meta-Analysis
- PLOS Medicine
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Women's Access and Provider Practices for the Case Management of Malaria during Pregnancy: A Systematic Review and Meta-Analysis
- Observational Studies: Getting Clear about Transparency
- Heart Failure Care in Low- and Middle-Income Countries: A Systematic Review and Meta-Analysis
- Scaling up Rural Sanitation in India
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



