-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Women's Access and Provider Practices for the Case Management of Malaria during Pregnancy: A Systematic Review and Meta-Analysis
Background:
WHO recommends prompt diagnosis and quinine plus clindamycin for treatment of uncomplicated malaria in the first trimester and artemisinin-based combination therapies in subsequent trimesters. We undertook a systematic review of women's access to and healthcare provider adherence to WHO case management policy for malaria in pregnant women.Methods and Findings:
We searched the Malaria in Pregnancy Library, the Global Health Database, and the International Network for the Rational Use of Drugs Bibliography from 1 January 2006 to 3 April 2014, without language restriction. Data were appraised for quality and content. Frequencies of women's and healthcare providers' practices were explored using narrative synthesis and random effect meta-analysis. Barriers to women's access and providers' adherence to policy were explored by content analysis using NVivo. Determinants of women's access and providers' case management practices were extracted and compared across studies. We did not perform a meta-ethnography. Thirty-seven studies were included, conducted in Africa (30), Asia (4), Yemen (1), and Brazil (2). One - to three-quarters of women reported malaria episodes during pregnancy, of whom treatment was sought by >85%. Barriers to access among women included poor knowledge of drug safety, prohibitive costs, and self-treatment practices, used by 5%–40% of women. Determinants of women's treatment-seeking behaviour were education and previous experience of miscarriage and antenatal care. Healthcare provider reliance on clinical diagnosis and poor adherence to treatment policy, especially in first versus other trimesters (28%, 95% CI 14%–47%, versus 72%, 95% CI 39%–91%, p = 0.02), was consistently reported. Prescribing practices were driven by concerns over side effects and drug safety, patient preference, drug availability, and cost. Determinants of provider practices were access to training and facility type (public versus private). Findings were limited by the availability, quality, scope, and methodological inconsistencies of the included studies.Conclusions:
A systematic assessment of the extent of substandard case management practices of malaria in pregnancy is required, as well as quality improvement interventions that reach all providers administering antimalarial drugs in the community. Pregnant women need access to information on which anti-malarial drugs are safe to use at different stages of pregnancy.
Please see later in the article for the Editors' Summary
Published in the journal: Women's Access and Provider Practices for the Case Management of Malaria during Pregnancy: A Systematic Review and Meta-Analysis. PLoS Med 11(8): e32767. doi:10.1371/journal.pmed.1001688
Category: Research Article
doi: https://doi.org/10.1371/journal.pmed.1001688Summary
Background:
WHO recommends prompt diagnosis and quinine plus clindamycin for treatment of uncomplicated malaria in the first trimester and artemisinin-based combination therapies in subsequent trimesters. We undertook a systematic review of women's access to and healthcare provider adherence to WHO case management policy for malaria in pregnant women.Methods and Findings:
We searched the Malaria in Pregnancy Library, the Global Health Database, and the International Network for the Rational Use of Drugs Bibliography from 1 January 2006 to 3 April 2014, without language restriction. Data were appraised for quality and content. Frequencies of women's and healthcare providers' practices were explored using narrative synthesis and random effect meta-analysis. Barriers to women's access and providers' adherence to policy were explored by content analysis using NVivo. Determinants of women's access and providers' case management practices were extracted and compared across studies. We did not perform a meta-ethnography. Thirty-seven studies were included, conducted in Africa (30), Asia (4), Yemen (1), and Brazil (2). One - to three-quarters of women reported malaria episodes during pregnancy, of whom treatment was sought by >85%. Barriers to access among women included poor knowledge of drug safety, prohibitive costs, and self-treatment practices, used by 5%–40% of women. Determinants of women's treatment-seeking behaviour were education and previous experience of miscarriage and antenatal care. Healthcare provider reliance on clinical diagnosis and poor adherence to treatment policy, especially in first versus other trimesters (28%, 95% CI 14%–47%, versus 72%, 95% CI 39%–91%, p = 0.02), was consistently reported. Prescribing practices were driven by concerns over side effects and drug safety, patient preference, drug availability, and cost. Determinants of provider practices were access to training and facility type (public versus private). Findings were limited by the availability, quality, scope, and methodological inconsistencies of the included studies.Conclusions:
A systematic assessment of the extent of substandard case management practices of malaria in pregnancy is required, as well as quality improvement interventions that reach all providers administering antimalarial drugs in the community. Pregnant women need access to information on which anti-malarial drugs are safe to use at different stages of pregnancy.
Please see later in the article for the Editors' SummaryIntroduction
Malaria in pregnancy is an important public health problem for both maternal and neonatal health programmes. The manifestation of maternal infection with malaria depends on transmission intensity, and prompt diagnosis and treatment of malaria illness in pregnancy is important in all malaria endemic regions. Since 2006, WHO recommends quinine plus clindamycin for the treatment of uncomplicated malaria in the first trimester, and artesunate (AS) plus clindamycin for treatment failures. Artemisinin-based combination therapies (ACTs) known to be effective in the country/region, or AS plus clindamycin, are the recommended combinations for case management of uncomplicated malaria in the second and third trimesters [1],[2]. Use of the artemisinin class of compounds, alone or in combination therapies, is not recommended in the first trimester of pregnancy because of insufficient safety data in early pregnancy in humans [3], unless this is the only treatment immediately available [1].
Many countries in high transmission settings have made ACTs available free of charge to pregnant women in efforts to achieve universal coverage [4]. Despite increasing availability of ACTs and new diagnostic tools, such as rapid diagnostic tests (RDTs), very little is known about women's access to these interventions and about the diagnosis and treatment practices of healthcare providers. National malaria indicator surveys focus on access to case management among children, the other important risk group for malaria. Similarly, research on uptake of new diagnostics and ACTs has to date focussed on children and non-pregnant adult populations, whereas research on uptake of interventions in pregnancy has predominantly focussed on progress and challenges to the delivery and uptake of preventive interventions, namely, intermittent preventive treatment in pregnancy (IPTp) and insecticide-treated nets [5]. Information on access to and delivery of effective case management of malaria in pregnancy has not yet received the attention it deserves.
We undertook a systematic review of the factors affecting pregnant women's access to and health provider adherence to the 2006 WHO policy [2] on the treatment of malaria in pregnancy globally. Among pregnant women we reviewed treatment-seeking practices for malaria illness—the range of providers visited, the antimalarials used, and the factors affecting their choice of healthcare provider and medicines. We explored adherence to policy among the range of healthcare providers administering antimalarials to pregnant women, the type and quality of diagnostic and case management services offered at the point of care (including consideration of gestational age), and the health system or other factors that affect quality of care.
Methods
Search Strategy
Studies investigating treatment-seeking practices for malaria among pregnant women and healthcare provider case management practices for malaria in pregnancy were identified by searching the Malaria in Pregnancy Library [6], the Global Health Database [7], and the International Network for the Rational Use of Drugs (INRUD) Bibliography [8] from 1 January 2006 to 3 April 2014. The Malaria in Pregnancy Library (http://library.mip-consortium.org) is a comprehensive bibliographic database created by the Malaria in Pregnancy Consortium that is updated every 4 mo using a standardised protocol to search over 40 sources, including PubMed, Web of Knowledge, and Google Scholar. Searches were run separately for “pregnant women” and “health providers” (see Table S1 for search terms), without language restrictions, and both peer-reviewed and grey literature were retrieved.
Study Selection
Titles and abstracts were reviewed independently for inclusion by two reviewers (J. Hill and L. D′M-G/J. Hoyt). Studies were included if they met the following criteria: (1) study contained data on treatment seeking among women and/or case management practices for malaria in pregnancy, (2) study population included pregnant women and/or healthcare providers, (3) study reported original research data, and (4) study was conducted following the introduction of ACTs for the treatment of uncomplicated malaria in pregnancy in the study country. No restrictions were placed on study design (i.e., quantitative, qualitative, and mixed methods studies), or quality of reporting. Studies limited to knowledge of malaria in pregnancy amongst pregnant women, i.e., without information on practices, were excluded. The Kappa (K) statistic was used as a measure of the inter-rater agreement on study eligibility between reviewers. Discrepancies between reviewers were resolved through discussions with a third reviewer (J. W.) until consensus was reached.
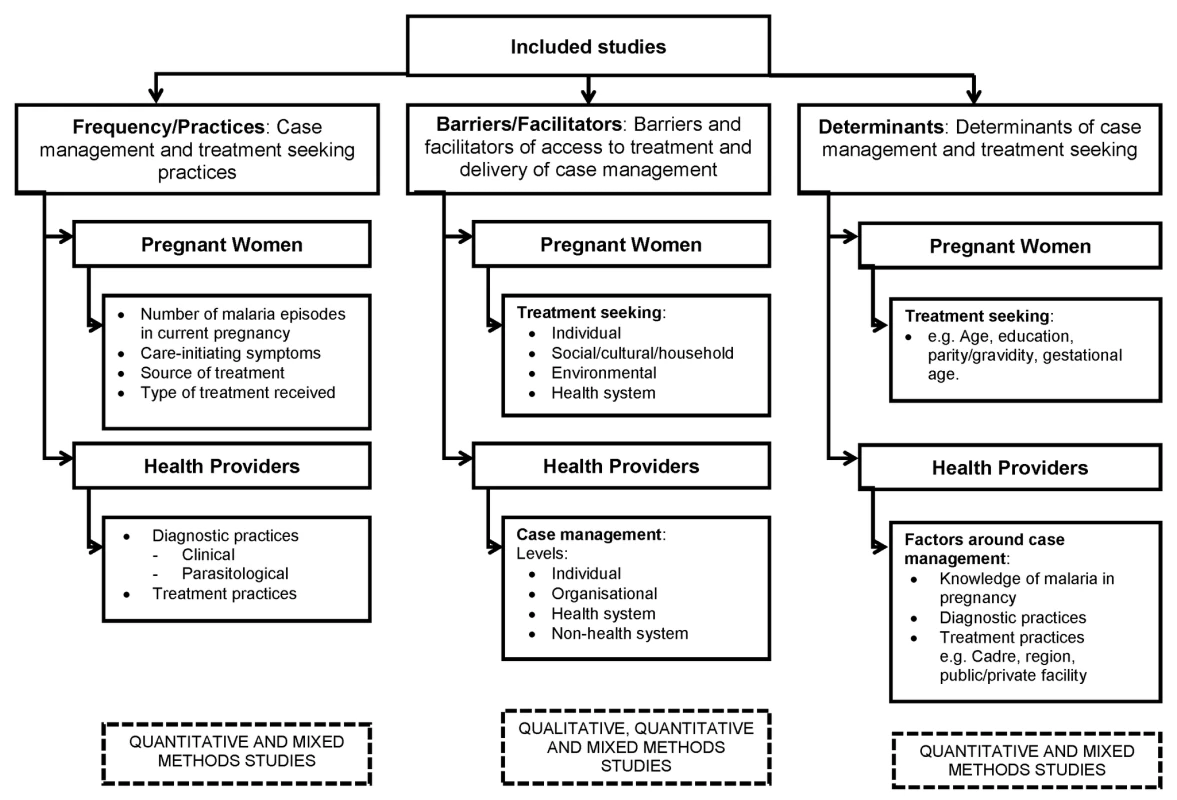
Studies meeting the inclusion criteria were assessed and grouped according to content. Among pregnant women primary outcomes included (1) treatment-seeking practices for malaria, (2) barriers to accessing malaria treatment, and (3) determinants of treatment seeking for malaria. Among healthcare providers primary outcomes were (1) case management practices for malaria in pregnancy, (2) factors affecting malaria case management practices, and (3) determinants of knowledge, diagnosis, and treatment of malaria.
Data Extraction
Two authors extracted data and appraised the quality and content of included studies. Data for pregnant women or healthcare providers were extracted and analysed separately for description and frequency of practices, barriers/facilitators, and determinants (Figure 1). Two authors (J. Hill and L. D′M-G/A. M. v. E/J. Hoyt) extracted quantitative data on the type and frequency of practices from quantitative and mixed methods studies. For pregnant women these quantitative data included the frequency of malaria episodes, sources of treatment, and the resultant treatment achieved, and for healthcare providers the quantitative data included the type and frequency of diagnostic and treatment practices in relation to national drug policy at the time of publication. J. Hill and L. D′M-G/J. Hoyt extracted qualitative and quantitative data on the barriers and facilitators to treatment seeking among pregnant women and case management practices among healthcare providers from qualitative and mixed methods studies. J. Hill and L. D′M-G/J. Hoyt extracted quantitative data on the determinants of treatment seeking and case management practices among pregnant women and healthcare providers, respectively, from quantitative and mixed methods studies. For healthcare providers, determinants of knowledge and practice, and of diagnosis and treatment, were extracted separately. Two authors (J. Hill and L. D′M-G/J. Hoyt) assessed the quality of reporting of individual studies using a checklist of criteria developed a priori based on criteria and methods described in the literature, described previously [5].
Data Synthesis and Analysis
Narrative synthesis was used to summarise, compare, and contrast the type, range, and frequency of practices from each study evaluating treatment seeking among pregnant women and case management practices among healthcare providers. To make a comparison between national policy and healthcare provider practices by country and region, we used the national or global malaria policy cited in the included studies.
Barriers and facilitators were explored using content analysis with a previously defined thematic framework for pregnant women and healthcare providers [5]. NVivo version 9.2 (QSR International) was used to generate an index of codes, which identified each of the recurring barriers amongst pregnant women and healthcare providers. The themes emerged as all the data were analysed, working cyclically through the studies. Data from the women's perspective were categorised into individual, social/cultural/household, environmental, and health system levels. Data from providers were synthesised into a matrix that combined operational levels of individual, organisational, health system, and non-health system levels, together with the six health systems levels of the WHO Health Systems Framework, which include governance/leadership, service delivery, health workforce/human resources, health information systems, finance, and medical products/technologies [9]–[11].
We appraised the quality of reporting of each study using a checklist of criteria based on methods described in a previous review [5], as described and reported in Tables S2–S4.
Statistical Analysis
We pooled the frequency data for source of treatment among pregnant women and adherence to treatment policy among healthcare providers across different types of providers using random effect meta-analysis in Stata version 12 (StataCorp) and Comprehensive Meta-Analysis (Biostat; http://www.meta-analysis.com/), which was also used for sub-group analysis. We used forest plots to visualise the extent of heterogeneity between studies. For studies that reported source of treatment for more than one episode of fever, we included the response to the first episode [12]. For source of treatment among pregnant women, we conducted sub-group analysis within each category for the following: whether the question involved practice (i.e., women with fever) or attitude (i.e., a hypothetical question, “if they had fever…”); health facility – or population-based enrolment; urban or rural populations; and country of study (Nigeria, the country contributing the majority of studies, versus other countries). For adherence to treatment policy, we conducted sub-group analysis for the following: trimester treated, the effect of staff cadre (medical doctor versus others), and method of data collection (self-administered questionnaire, interview, or record review). I2 was used to quantify heterogeneity [13].
Results
Of 2,047 records retrieved from the database searches, 37 studies met the inclusion criteria (Figure 2)—13 studies in pregnant women, 18 studies in healthcare providers, and six studies in both pregnant women and healthcare providers; only one study evaluated interventions. There was close agreement between the reviewers on the review of full text articles (K = 0.84). The majority of studies were conducted in Africa (30), with only four studies conducted in Asia (two in India [14],[15] and two in Cambodia [16],[17]), one in Yemen [18], and two in Brazil [19],[20]. Of the studies conducted in Africa, 17 were in west and central Africa and 12 in east and southern Africa, and one study had sites in east, west and southern Africa [21]. All but three studies were cross-sectional surveys at the population or facility level. The remaining studies included two longitudinal qualitative studies [21],[22] and a randomised controlled trial [23]. The study characteristics are provided in Tables 1–3.
Fig. 2. PRISMA chart of studies included in the review. 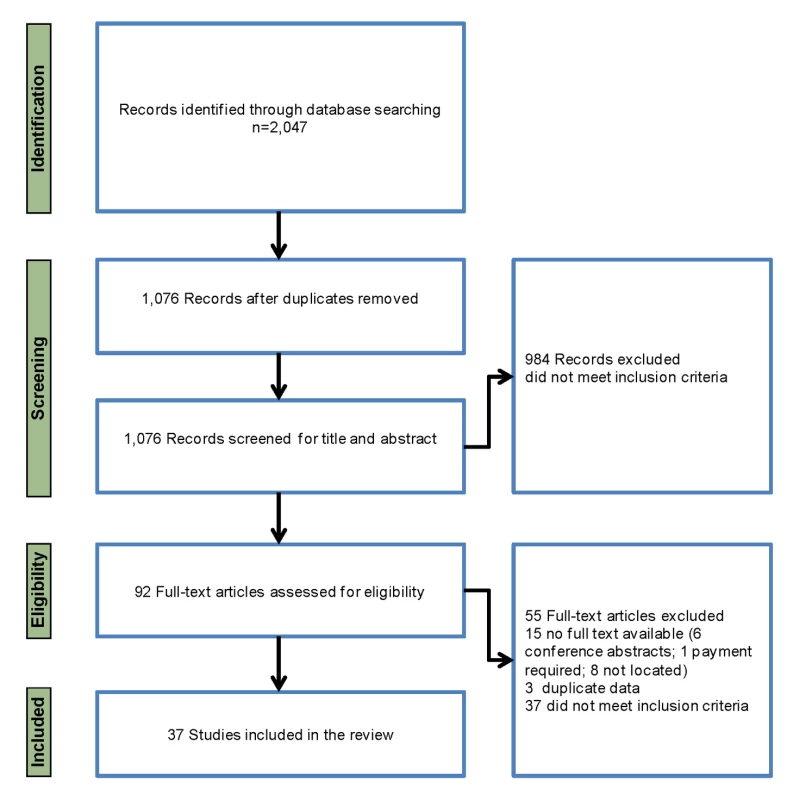
Tab. 1. Characteristics of studies reporting outcomes, barriers, and determinants for treatment-seeking practices among pregnant women (13 studies). 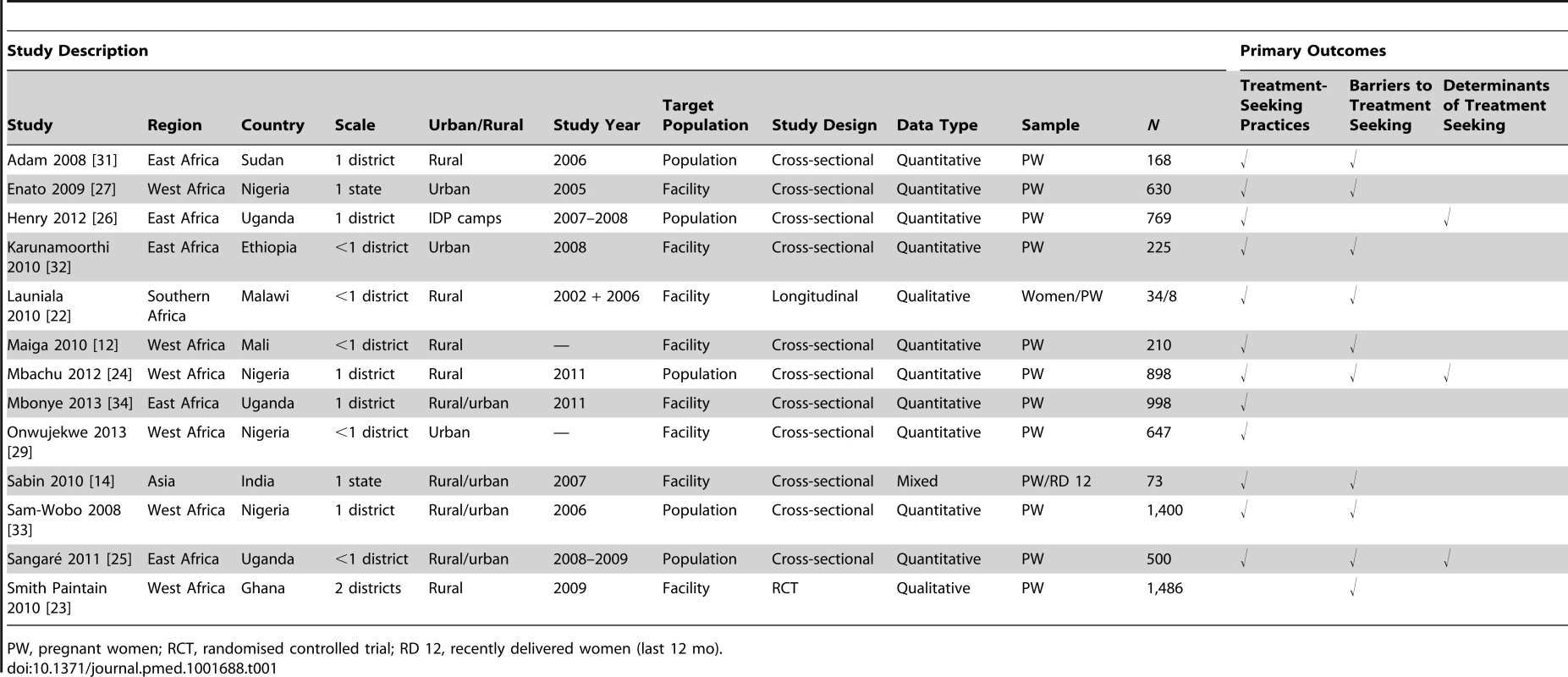
PW, pregnant women; RCT, randomised controlled trial; RD 12, recently delivered women (last 12 mo). Tab. 2. Characteristics of studies reporting outcomes, barriers, and determinants for case management practices among healthcare providers (18 studies). 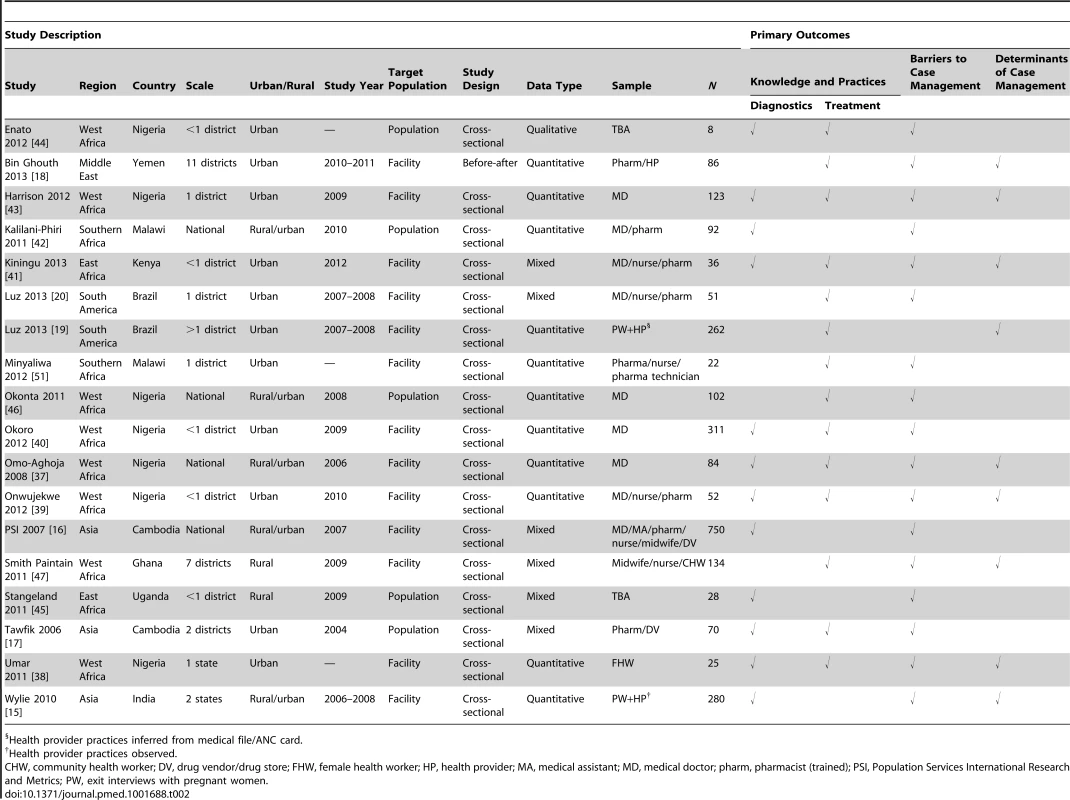
Health provider practices inferred from medical file/ANC card. Tab. 3. Characteristics of studies reporting outcomes for both pregnant women and health providers (six studies). 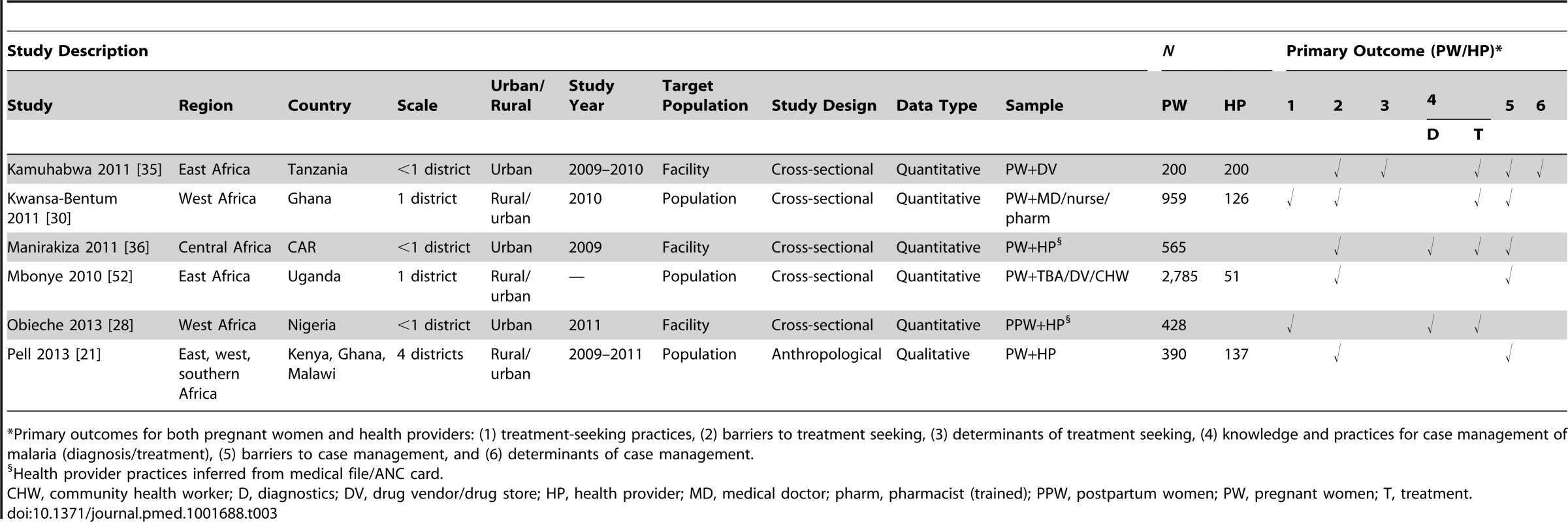
*Primary outcomes for both pregnant women and health providers: (1) treatment-seeking practices, (2) barriers to treatment seeking, (3) determinants of treatment seeking, (4) knowledge and practices for case management of malaria (diagnosis/treatment), (5) barriers to case management, and (6) determinants of case management. Quality of about half (14/27) of the quantitative studies was assessed to be moderate-high (scored 6–8/10), with ten low-moderate-quality studies (4–5/10) and three high-quality studies (9–10/10) (Table S2). The quality criterion least often met among these studies was the use of multivariate analysis. The four qualitative studies were assessed as moderate-high quality (4–7/8), with only one of the studies reporting saturation of themes (Table S3). All six mixed methods studies were assessed as high quality (9–10/11), though only one study reported use of multivariate analysis (Table S4). Data on frequencies of practices, barriers/facilitators, and determinants of access among women were extracted from 13, 15, and four studies, respectively, and of policy adherence among healthcare providers, from 24, 22, and ten studies, respectively (Table 4).
Tab. 4. Data extracted for frequencies, barriers, and determinants by survey type. 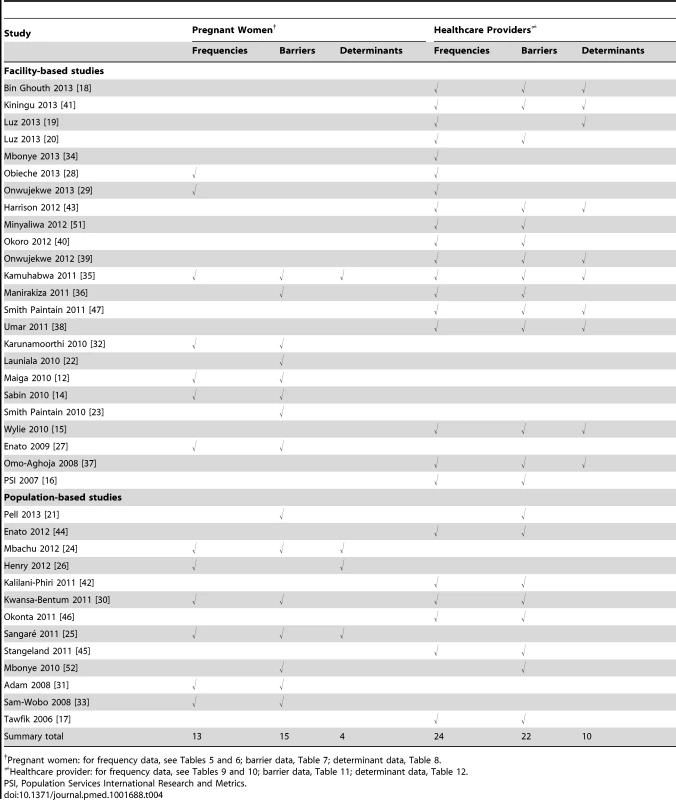
Pregnant women: for frequency data, see Tables 5 and 6; barrier data, Table 7; determinant data, Table 8. Pregnant Women Perspectives
The 19 studies that contributed data on the treatment-seeking practices of pregnant women were undertaken in ten countries across Africa (seven studies in east Africa, eight in west Africa, one in southern Africa, one in central Africa, and one with sites in east, west, and southern Africa) and in one country in Asia (Tables 1 and 3).
Description and frequency of practices among pregnant women
The proportion of women reporting at least one episode of malaria during their current or recent pregnancy ranged from 25% to 75% of respondents in three population-based [24]–[26] and three facility-based [14],[27],[28] studies in Africa and Asia, with between 30% and 46% of women reporting two or more episodes in Africa [25],[27],[28] (Tables 5 and 6). Of one population-based [25] and three facility-based [14],[28],[29] studies, a high proportion (>85%) of women with a reported episode of malaria during pregnancy sought some form of treatment.
Tab. 5. Symptoms and number of episodes of malaria in pregnancy, and percentage who sought treatment by source, reported by pregnant women: population-based studies. 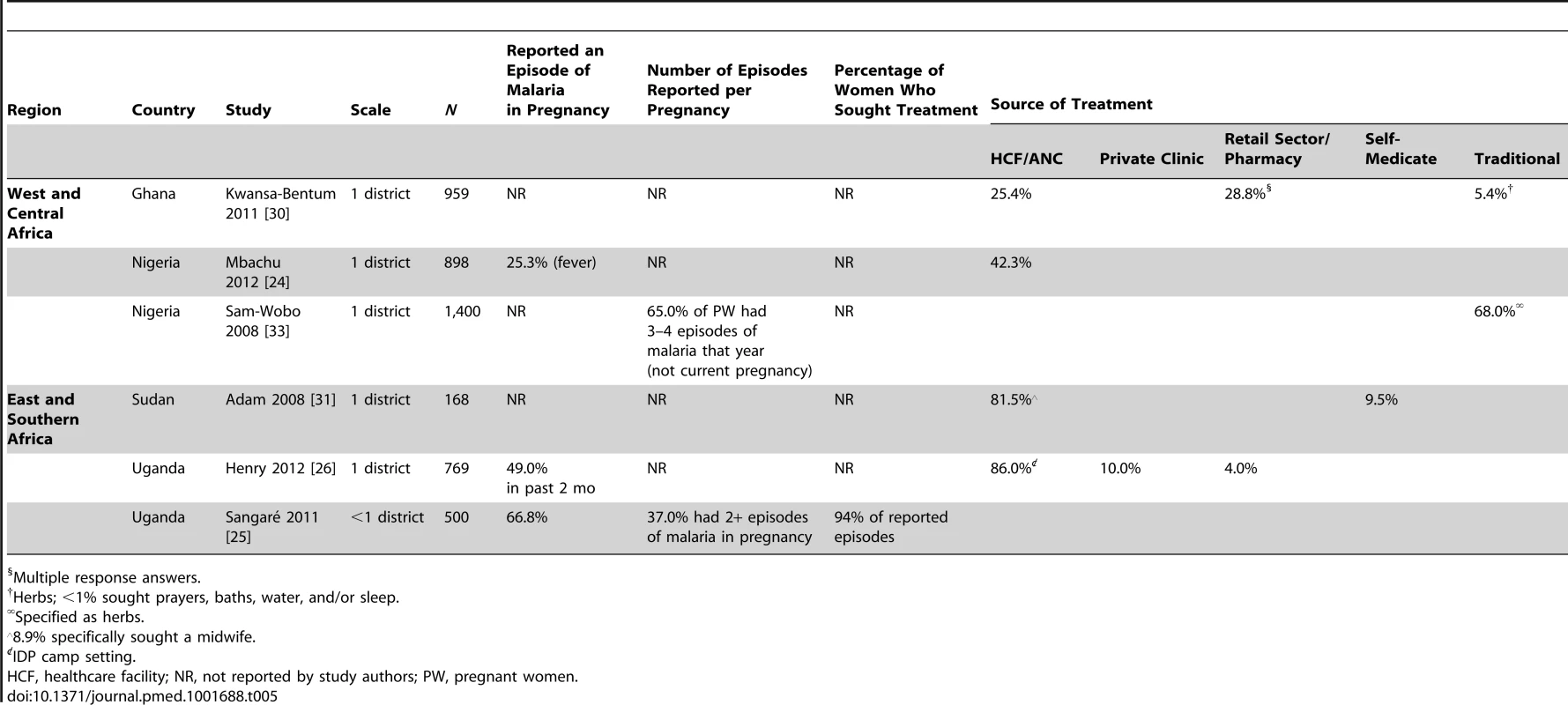
Multiple response answers. Tab. 6. Symptoms and number of episodes of malaria in pregnancy, and percentage who sought treatment by source, reported by pregnant women: facility-based studies. 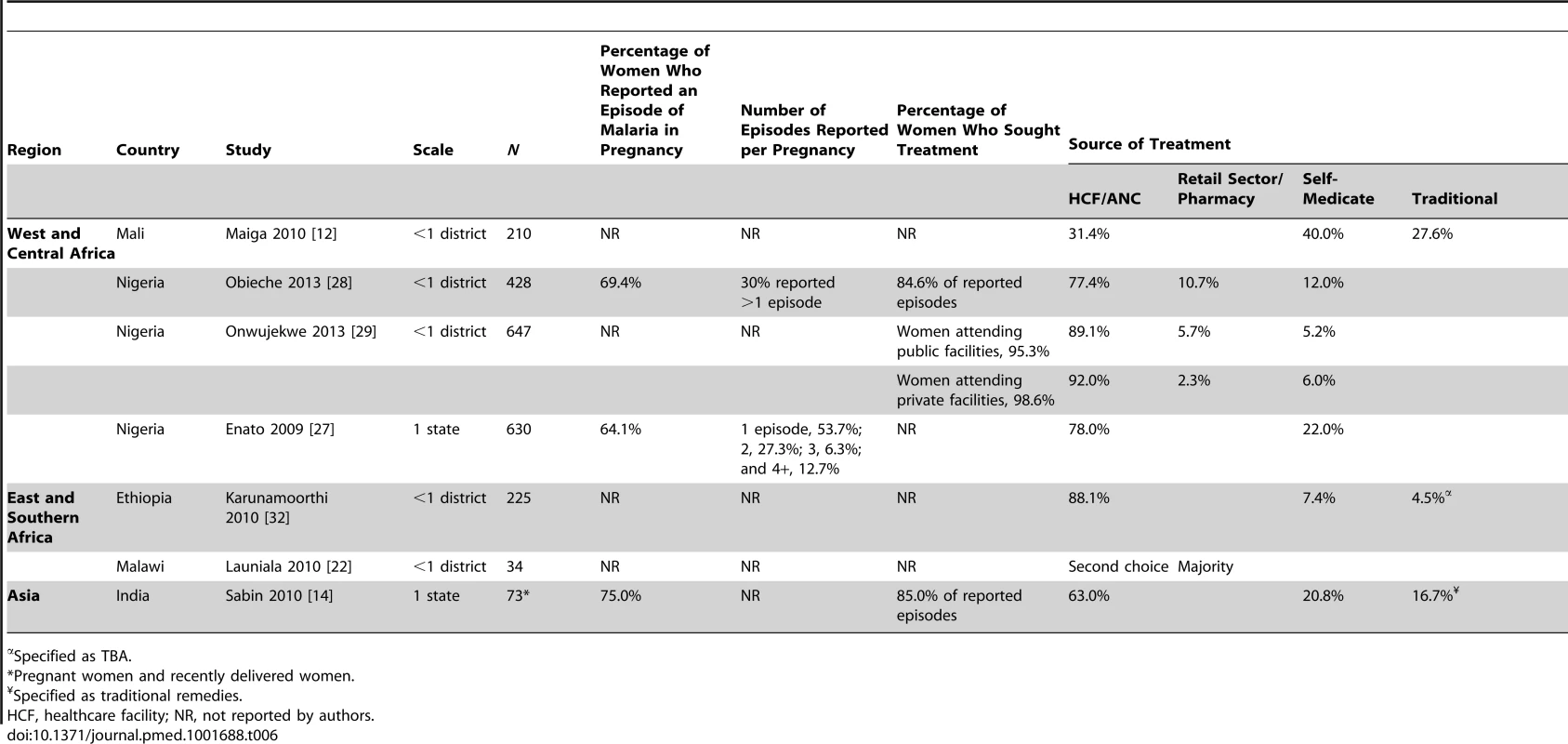
Specified as TBA. Pregnant women in three population-based [26],[30],[31] and seven facility-based [12],[14],[22],[27]–[29],[32] studies in Africa reported self-medication or treatment at a pharmacy/drug store at the onset of fever (range 5%–40%), and attended a health facility only if their fever did not respond to this treatment [12],[30] (Tables 5 and 6). In southern Ghana, women seeking treatment at a pharmacy or drug vendor without a clinic prescription reported that the antimalarials were selected by either the shop attendant (21% and 26% in rural and urban areas, respectively) or themselves (8% and 10%, respectively) [30]. Use of local herbs was a first resort among pregnant women in a population-based study in Nigeria [33]. Pregnant women in urban settings were likely to seek care from antenatal care (ANC) or health facilities as a first resort, as observed in three population-based studies in Nigeria (42%) [24], Sudan (82%) [31], and internally displaced person (IDP) camps in Uganda (86%) [26], and five facility-based studies (range 63%–92%) in Ethiopia [32], Nigeria [27]–[29], and India [14].
Data on sources of treatment extracted from nine studies showed high heterogeneity across studies (I2 ranging from 60% to 99%) (Figure 3), and all but one study [12] were of moderate to high quality. Site of enrolment (health facility – versus population-based), country (Nigeria versus other countries), and type of question (practice versus attitude) had no effect within each category (Table S5). Compared to urban women, rural women were more likely to make use of a traditional healer or herbs (2%, 95% CI 0%–7%, three studies, versus 21%, 95% CI 6%–52%, four studies, respectively, p = 0.008), whereas urban women made more use of health facilities (84%, 95% CI 71%–91%, two studies, versus 38%, 95% CI 14%–70%, four studies, p = 0.006).
Fig. 3. Prevalence of source of malaria treatment during pregnancy assessed in 18 studies with quantitative data. 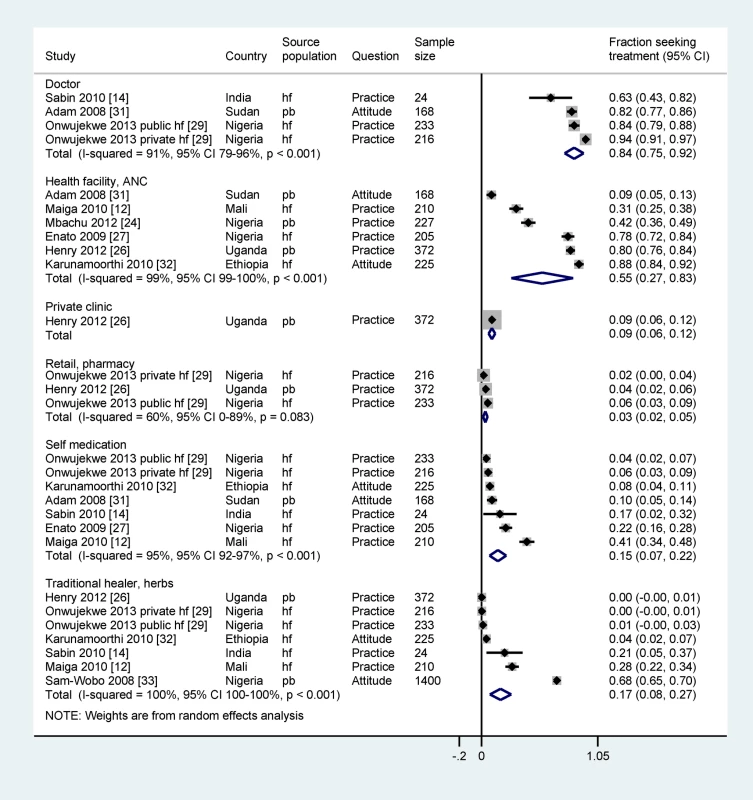
hf, health facility–based survey; pb, population-based survey. Only six of the 14 studies among pregnant women with treatment-seeking practice as a primary outcome included quantitative data on use of ACTs, and of these, only four stratified use by trimester. In a household survey in Uganda, among first trimester episodes, quinine was used in only 6% of first trimester cases, with >80% of episodes treated with drugs not recommended for use in the first trimester either because they are contraindicated (sulphadoxine-pyrimethamine [SP] and artemether-lumefantrine [AL]) or because of high-grade drug resistance (chloroquine [CQ]) [25]. Only 30% of second and third trimester cases adhered to national guidelines (AL or quinine) [25]. Another study conducted in 2011 in Uganda reported appropriate treatment in only 36% of febrile cases, defined as parasite-positive pregnant women given AL (Coartem) and parasite-negative women given no antimalarial drug [34]. Of pregnant women interviewed at a public hospital in Tanzania, 31% had used AL for an episode of malaria in the index pregnancy, 27% SP, 23% quinine, 16% sulphalene-pyrimethamine, and 3% amodiaquine (AQ) [35]. The majority (82%) of women said they were asked about gestational age before being given AL by drug dispensers; however, only 17% of pregnant women were aware that AL should not be taken in the first trimester, and only 22% knew that quinine was recommended. In a population-based study in Ghana, drug sellers said some women requested artemisinin combinations for treatment in the first trimester [30].
A household survey in southeast Nigeria found that 42% of pregnant women who had a fever within the last month had visited a health facility, of which 46% were treated with ACTs, 34% with SP, and 4% with artemisinin monotherapy; however, trimester was not specified [24]. In an earlier population-based study in Nigeria, women reported a high preference for SP for case management in the second and third trimesters of pregnancy, whereas the national treatment policy in second and third trimesters was to use AL; the study was, however, done only a year after the new policy was introduced [33]. A more recent facility-based study in a teaching hospital reported that quinine was used in only 12% of first trimester episodes, with artemisinin-containing compounds, SP, and CQ used in 35%, 39%, and 14% of cases, respectively [28]. In a comparative study of treatment practices of second and third trimester episodes in public and private health facilities, quinine was used in 4% of episodes in both types of facility, with artemisinin monotherapy constituting the most frequently prescribed drug (36%–39%) [29].
Barriers to care seeking for malaria among pregnant women
The factors affecting treatment seeking for malaria most frequently cited in the content analysis related to the following: women's knowledge and perceptions of risk, perceptions and experience of drug safety, cost, and perceptions and experience of healthcare provider and health facility factors (Table 7). Women in one facility-based study [14] perceived malaria during pregnancy as not especially dangerous, and the first response in two population-based [30],[31] and four facility-based [12],[14],[22],[32] studies was to rely on self-medication or herbal treatments, and to seek medical advice only if the illness did not improve. Over 50% of women in a facility-based study reported delaying >2 d after first noticing symptoms before seeking care [27]. The choice of treatment was influenced by women's perceptions of the safety of drugs used during pregnancy, as reported by three population-based studies [30],[31],[33] and one facility-based study [35]. Fear and/or prior experience of side effects to drugs also influenced treatment choices and adherence, as reported by one population-based [21] and three facility-based [14],[23],[35] studies. In northern Ghana, pregnant women identified contradictions between messages provided in health facilities and their own experiences of malaria [21].
Tab. 7. Content analysis of factors that affect treatment seeking for malaria among pregnant women. 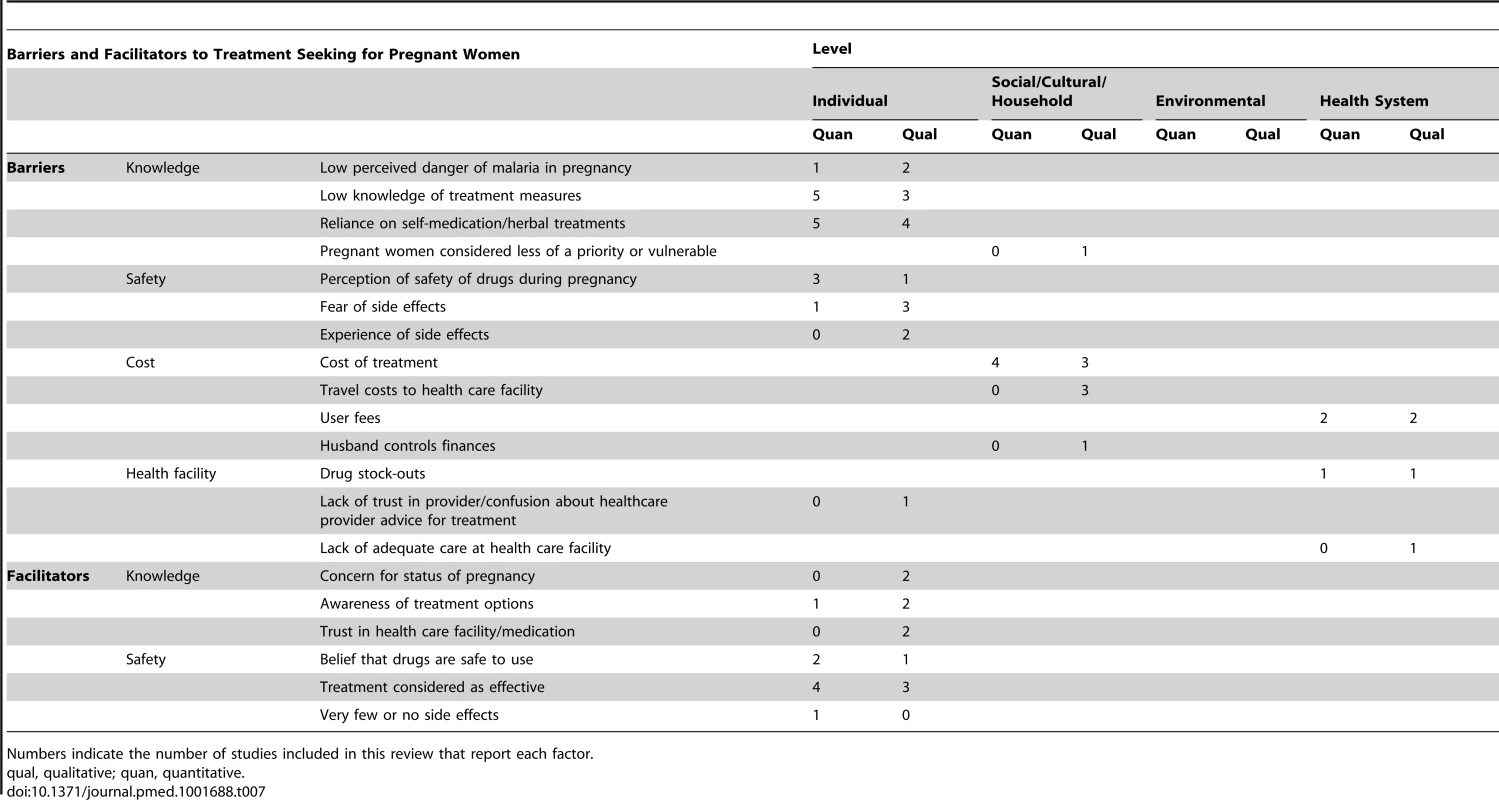
Numbers indicate the number of studies included in this review that report each factor. The high cost of treatment prevented pregnant women from using the formal health sector in rural population-based surveys in Ghana [21],[30], Kenya [21], and Nigeria [24]. Poverty was said to be why women resorted to herbal remedies in Kenya and Ghana, to avoid costs of both transport and medical care [21]. Other barriers cited were user fees at formal health services [33] or the cost of treatment in urban areas in population-based surveys in Ghana [30] and facility-based studies in the Central African Republic (CAR) [36] and India [14]. Lack of adequate care at health facilities [23] was an additional deterrent to using the health facilities. Women in one study reported that they did not understand the instructions given by dispensers regarding (AL) dosage and duration of use [35]. On the other hand, women who were concerned for their pregnancy status, who were aware of the treatment options [22],[23],[30] and considered the drugs safe and effective [14],[25],[30],[35], and who trusted the health facility staff [21],[23] were more likely to seek treatment at health facilities. Women in Ghana and Kenya generally valued diagnostic tests for malaria (and other diseases) and associated testing with more effective treatment [21].
Determinants of care seeking for malaria among pregnant women
The range of determinants of treatment seeking among pregnant women explored across the included studies included education, prior experience of miscarriage, and ANC use. The key findings are highlighted in Table 8; insufficient data and lack of consistency in the indicators used prevented us from performing a meta-analysis of pooled data. A higher level of education was associated with correct knowledge of AL use in pregnancy in Tanzania [35]. Prior use of ANC services and previous experience of miscarriage were associated with increased treatment seeking for malaria in IDP camps in Uganda [26].
Tab. 8. Data on the determinants of treatment-seeking behaviours for malaria in pregnancy by pregnant women. 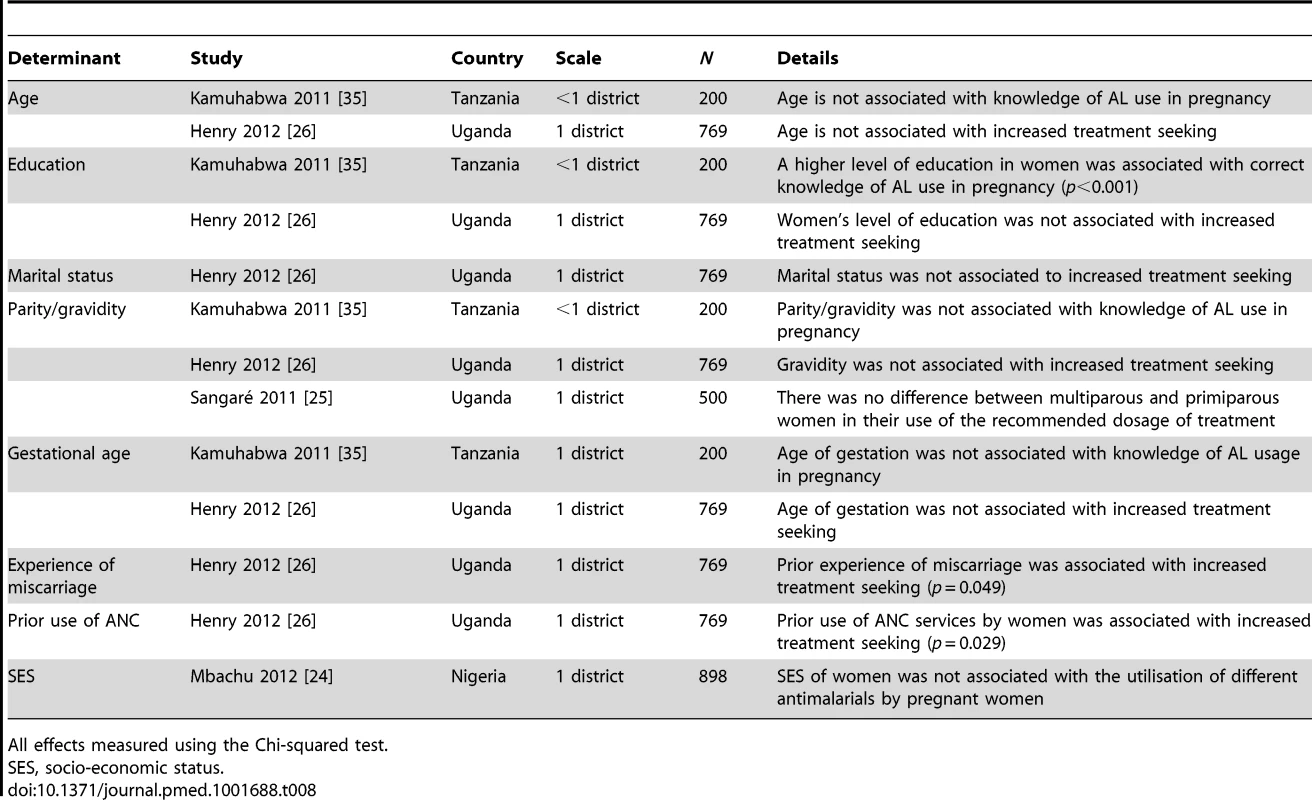
All effects measured using the Chi-squared test. Healthcare Provider Perspectives
The 24 studies that contributed data on the diagnosis and treatment practices of healthcare providers were undertaken in ten countries, involving a range of cadres, including medical doctors and nurses, pharmacists, drug vendors, traditional birth attendants (TBAs), and community health workers (CHWs) (Tables 2 and 3).
Description and frequency of diagnostic practices
Malaria diagnosis in pregnancy by public healthcare providers in the studies conducted in Africa was predominantly performed on the basis of clinical symptoms, as reported by one population-based study in Ghana [30] and five facility-based studies in CAR [36] and Nigeria [37]–[40]. The exceptions to this were microscopy use by private sector providers in Nigeria [39] and by a provincial hospital in Kenya [41] (Table 9). One population-based study in Malawi [42] and three facility-based studies in Nigeria [37],[38],[43] reported a combination of clinical and parasitological diagnosis by microscopy. Providers at the community level in three population-based studies, including private providers in Cambodia [17] and TBAs in Africa [44],[45], relied exclusively on clinical symptoms unless women could produce prescriptions issued from clinics. Globally, few studies reported healthcare providers using RDTs. In Africa, reports of RDT use have been relatively recent (2011 in Malawi [42] and 2012 in Nigeria [39]), compared to in Asia (2007 in Cambodia [16]), and only a fraction of providers reported using RDTs (range 22%–34%) [16],[39],[42]. In a population-based survey of medical doctors and pharmacists in Malawi, availability of tests, patient symptoms, and cost were the main factors affecting choice of diagnostic test [42]. In an observational study of ANC visits in eastern India, blood tests were typically obtained if a patient complained of fever, though enquiries into presence of fever in patients were made in only a minority of patients [15].
Tab. 9. Healthcare provider practices: diagnosis. 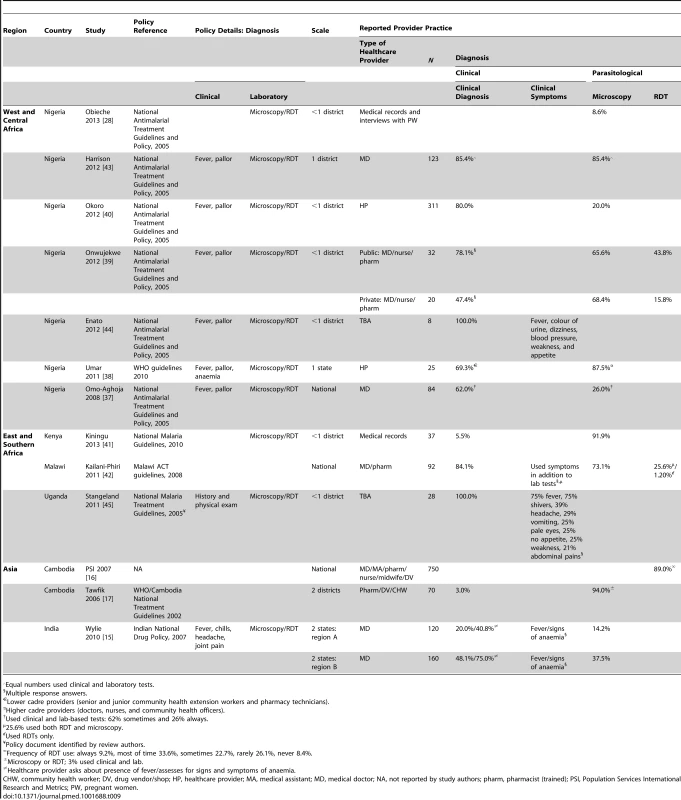
Equal numbers used clinical and laboratory tests. Description and frequency of treatment knowledge and practices
In west and central Africa, 11 studies on health providers were conducted in Nigeria (eight studies), Ghana (two), and CAR (one), where the national antimalarial treatment guidelines stipulate quinine for treatment of uncomplicated malaria in the first trimester and an ACT in the second and third trimesters [30],[36],[39] (Table 10). Only two of the eight studies in Nigeria [28],[37]–[40],[43],[44],[46] reported a relatively high proportion of providers adhering to treatment policy. Onwujekwe et al. found that more doctors, pharmacists, and nurses providing ANC services in public than private sector hospitals adhered to the national policy of prescribing ACTs in the second and third trimesters (69% versus 5%); private hospitals predominantly prescribed SP (70%) [39]. More public than private sector providers prescribed quinine in the first trimester (35% versus 15%); private sector providers predominantly prescribed SP (65%). Okonta found that whilst 56% of doctors had prescribed quinine during the first trimester, the fear of quinine causing miscarriage was a significant consideration, with all but one physician prescribing quinine at lower than the recommended dose, and showing a preference for CQ [46]. Similarly, Okoro and Nwambu found very low prescription of quinine in the first trimester (2.5%), and ACTs constituted 51% and 29% of antimalarial drugs prescribed in the second and third trimesters, respectively [40]. Two studies did not stratify treatment drug by trimester [37],[43]. Up until 2012, SP continued to be used widely for case management of clinical malaria in pregnancy in Ghana [30],[47] and Nigeria [28],[37]–[40],[43], as well as CQ, despite its known resistance [37],[39],[43], and artemisinin monotherapies [37],[43],[46].
Tab. 10. Healthcare provider practices: antimalarials prescribed. 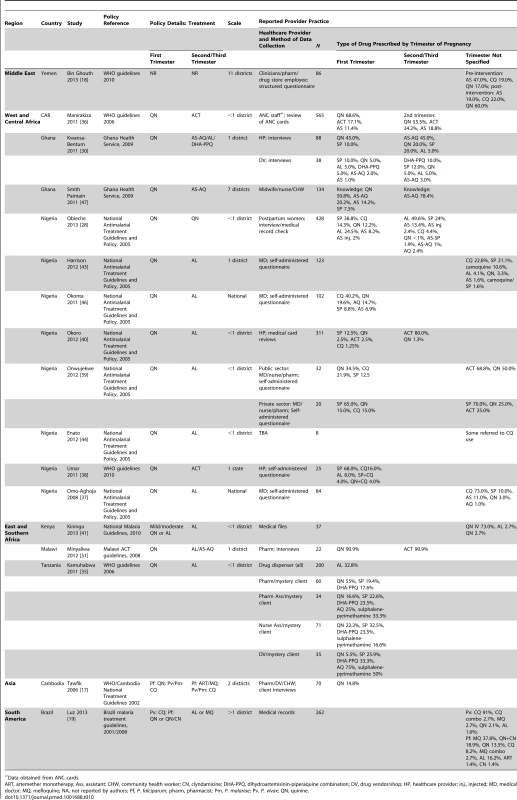
Data obtained from ANC cards. In Ghana, Kwansa-Bentum et al. found clinicians prescribing quinine for malaria treatment in the first trimester of pregnancy, per policy, but also SP, and predominantly ACTs were prescribed in the second and third trimesters, though SP and quinine were also prescribed [30]. In the same study, drug sellers reported pregnant women requesting, in order of preference, SP, ACTs, or quinine, with no difference by trimester. Smith Paintain et al. found that few ANC providers (20%) demonstrated good knowledge of the dosing regimen for treatment in the first trimester, though knowledge that AS-AQ should be prescribed in subsequent trimesters was better (42%), with preference for AS-AQ over quinine due to the side effects and long regimen duration (7 d) of quinine [47]. In CAR, 29% of ANC cards of women who had delivered in a maternity unit contained at least one antimalarial prescription, of which 57% were for quinine, 27% for ACTs, and 14% for artemisinin monotherapies; 11% and 13% of ACTs and artemisinin monotherapies, respectively, were for treatment in the first trimester [36].
In east and southern Africa, six studies were conducted in Kenya (one study), Malawi (two), Tanzania (one), and Uganda (two), where, again, the national malaria treatment policies recommend quinine in the first trimester, with an ACT (AS-AQ or AL) for the second/third trimester [48]–[50]. In Kenya, while 83% of staff at a provincial hospital stated that they used the national guidelines, guidelines were available at only 25% of points of use, and 73% of pregnant patients received parenteral quinine [41]. In Malawi, Kalilani-Phiri et al. found that only 40% of medical doctors and pharmacists knew the treatment guidelines for uncomplicated malaria in pregnant women, compared to 83% for severe malaria [42]. In contrast, Minyaliwa et al. reported that a high proportion (91%) of providers were cognisant of the appropriate drugs to use in each trimester, though specific drug names were not reported [51]. A study of dispensing practices among private pharmacies in urban Tanzania found low knowledge of appropriate antimalarial drugs, with 33% of providers willing to dispense AL for use in the first trimester and 36% indicating it could not be used in pregnancy. Nevertheless, 82% of women reported that they were asked about gestational age before they were given AL. Pharmacists and nurse assistants had better AL knowledge than pharmaceutical technicians and sales persons [35]. In Uganda, Mbonye and Magnussen found that 38% of pregnant women with reported fever but negative blood smears received an antimalarial (drug not specified) in addition to IPTp [52].
The remaining studies were conducted in Cambodia (one study) and Brazil (two studies). In Cambodia, only 4/27 pregnant women surveyed received the recommended drug, quinine, in the first trimester, and knowledge amongst private providers about first line treatment for malaria in pregnancy was poor [17]. In Brazil, while 93% of patients received the recommended first line therapy for Plasmodium vivax malaria, only 45% of patients received the recommended first line therapy for P. falciparum malaria, with 7% and 18% of prescriptions, respectively, not sanctioned by national guidelines [20].
Meta-analysis of adherence to treatment policy
Frequency data on adherence among healthcare providers to treatment policy by trimester, extracted from 12 studies, showed wide heterogeneity (overall I2 98.6%) (Figure 4), and all but one study [51] were of moderate to high quality. There was lower adherence to treatment policy in the first trimester (28%, 95% CI 14%–47%, nine entries from seven studies) than in the other trimesters (72%, 95% CI 39%–91%, five entries from three studies), and this difference was significant in the sub-group analysis (p = 0.02) (Table S6). Studies describing practices among doctors (three entries from Nigeria, 269 doctors in total as defined by the local researchers, all self-administered questionnaires) found that these healthcare providers were significantly less likely to prescribe correctly (11%, 95% CI 4%–23%) than healthcare providers in studies describing practices among other staff or mixed cadres (18 entries, 52%, 95% CI 35%–67%, p<0.001). Studies conducted by self-administered questionnaires showed a significantly lower proportion of adherence to treatment policy (14%, 95% CI 7%–28%, six entries) than studies using interviews (50%, 95% CI 27%–73%, seven entries) or record reviews (66%, 95% CI 39%–86%, eight entries, p = 0.001), and studies describing practices in Nigeria were significantly less likely to report correct treatment (25%, 95% CI 12%–46%, ten entries from eight studies) than studies in all other countries combined (58%, 95% CI 40%–75%, 11 entries from eight countries, p = 0.018).
Fig. 4. Prevalence of adherence to treatment policy for malaria in pregnancy assessed in 15 studies with quantitative data. 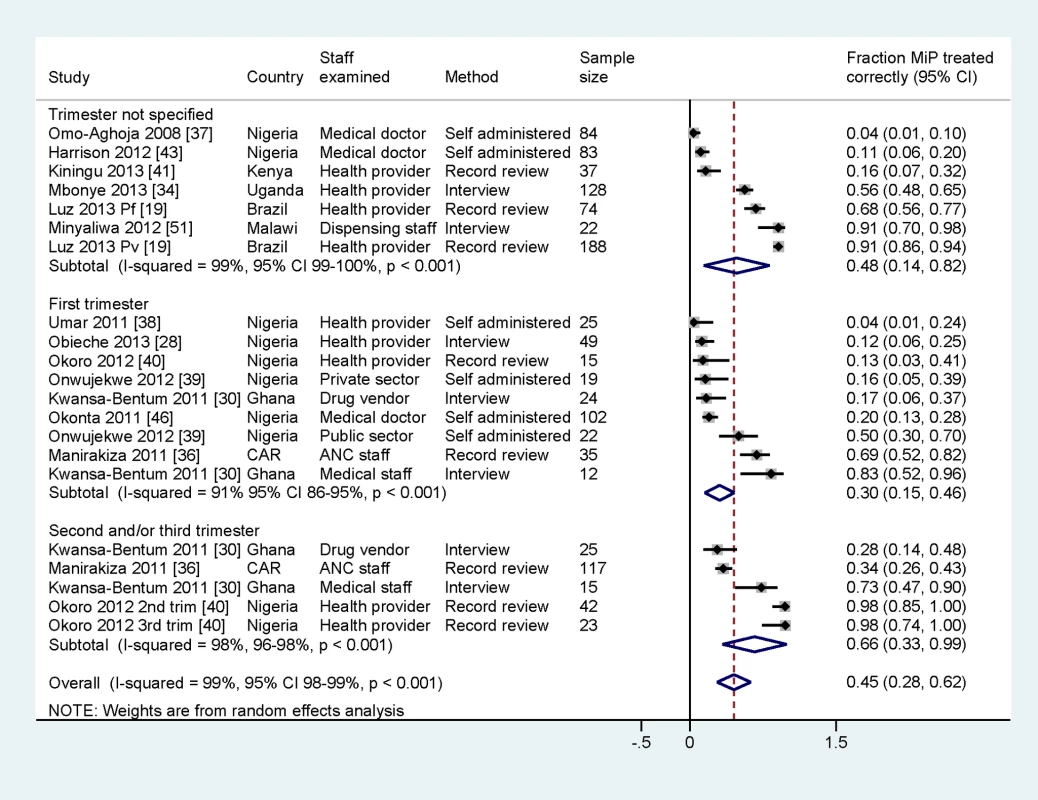
Pf, P. falciparum; Pv, P. vivax; self-administered, self-administered questionnaire; MiP, malaria in pregnancy. Barriers to effective case management practices for malaria in pregnancy among healthcare providers
Factors affecting diagnostic and case management practices occurred at all levels of the health system and across all of the health system building blocks (Table 11). Reliance on clinical diagnosis in the absence of parasitological confirmation by microscopy or RDT is a major weakness to effective management of malaria in pregnancy in many study settings. Parasitological diagnosis was not always possible because of inadequate or lack of diagnostic facilities [15],[17],[21],[42],[43],[47] or prohibitive costs to women [17],[42]. One study noted concerns among providers about the poor predictive value of microscopy, with providers administering treatment to women with negative blood smears [52]. In Cambodia, monovalent RDTs that detected only P. falciparum were available at the village level; hence, people with a negative result were reported to self-treat for P. vivax [17].
Tab. 11. Content analysis of barriers to effective case management practices among healthcare providers. 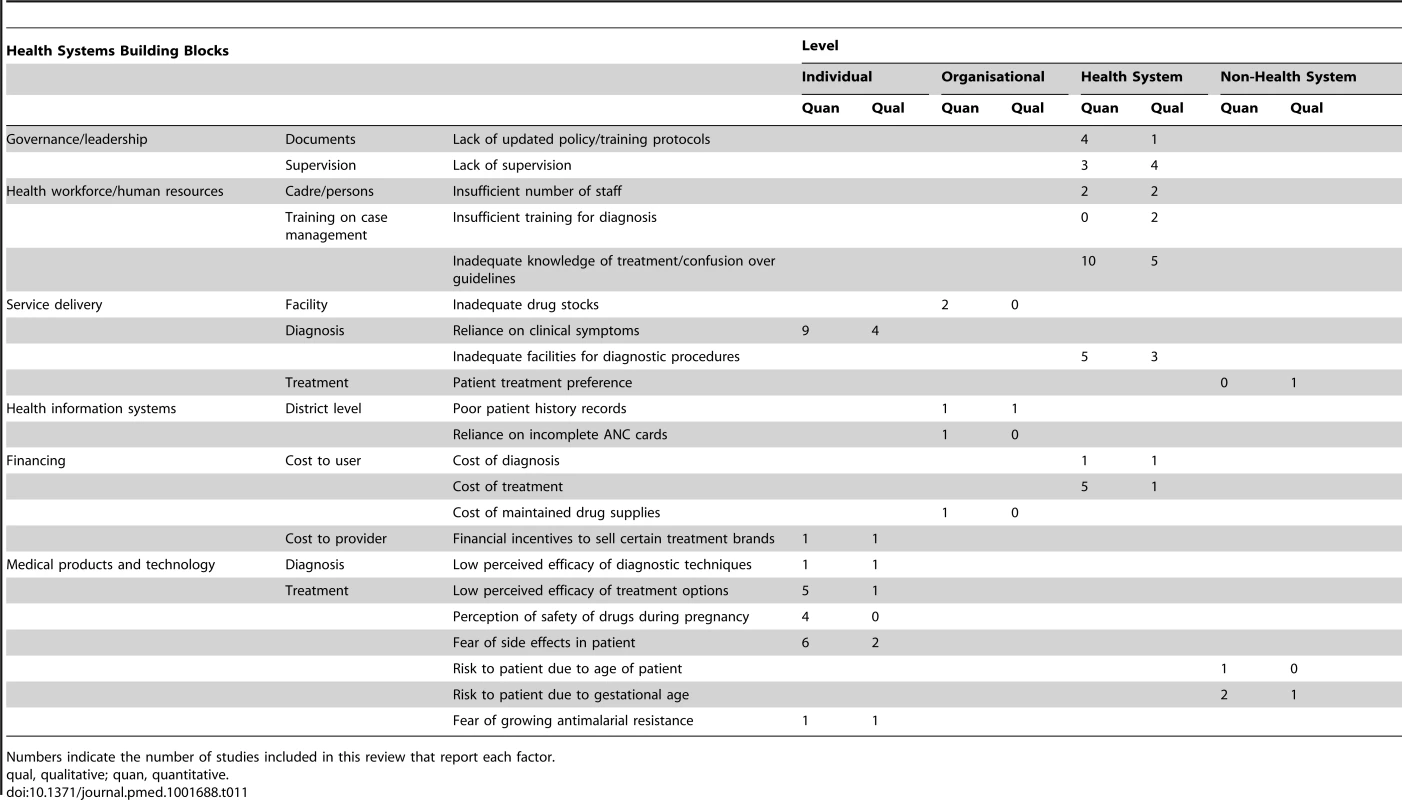
Numbers indicate the number of studies included in this review that report each factor. Poor knowledge of and adherence to national treatment policy guidelines among healthcare providers was a consistent finding across countries in east [42],[51] and west Africa [21],[30],[37],[38],[40],[43],[44],[46],[47], Asia [16],[17], the Middle East [18], and Latin America [20], and knowledge was particularly poor among private providers [35],[39]. In Ghana, healthcare providers asserted that pregnant women were exceptions to the policy of testing prior to treatment, and provided treatment even when a malaria test was negative. This practice was a misinterpretation of the guidelines, which state that in the absence of a laboratory, pregnant women with clinical symptoms of malaria should be treated [21]. Financial incentives and client demand have been reported to motivate private practitioners to sell medicines, even inappropriate medicines or more expensive brands [40], without parasitological testing [17]. Prescription practices were influenced by perceptions of low drug efficacy [20],[37],[38],[46], perceptions of increasing drug resistance [17],[38], concerns about drug safety [35],[37],[46], inadequate understanding and fear of potential side effects of drugs in pregnancy [17],[35],[40],[46],[47],[51], and the influence of patient preference [17], each contributing to poor quality of care. Many of the substandard practices reported are a consequence of factors operating at higher levels of the health system. Lack of national guidelines in India led to healthcare provider confusion about treatment policy [15]. Elsewhere, lack of training for diagnosis [16],[20] and/or treatment [18],[20],[41]–[43],[51] and lack of supervision [16],[41],[47] contributed to poor service delivery. Poor provider knowledge was exacerbated by weak organisation at the level of the health facility, such as inadequate drug stocks [15], and poor record-keeping practices such as providing written prescriptions and infrequent recording of vital information [20] and clinical findings and diagnoses [36] in both in-patient and out-patient records. Health system policies on fees for diagnosis [17],[42] and prescription drugs [17],[30],[38],[41],[42],[46] and human resource constraints [41],[47] also constitute important barriers.
Determinants of knowledge and diagnostic and treatment practices among healthcare providers
Determinants of healthcare provider knowledge, diagnostic practices, and treatment practices explored across the different studies included the following: individual healthcare provider factors (cadre, training), type of facility (public or private; primary or tertiary), and region/location (Table 12). There was insufficient uniformity of indicators and determinants to perform a meta-analysis of pooled data. Cadre of healthcare provider was associated with correct treatment knowledge [47] and diagnostic practices [38]. Public sector providers were more likely to use clinical diagnosis or parasitological diagnosis with RDTs and to adhere to national guidelines than private providers in Nigeria [39]. Two studies assessed the impact of training on provider knowledge, finding a significant positive association between provider knowledge and recent training on malaria treatment guidelines [18],[47].
Tab. 12. Determinants affecting provider knowledge of malaria in pregnancy, diagnostic practices, and treatment practices. 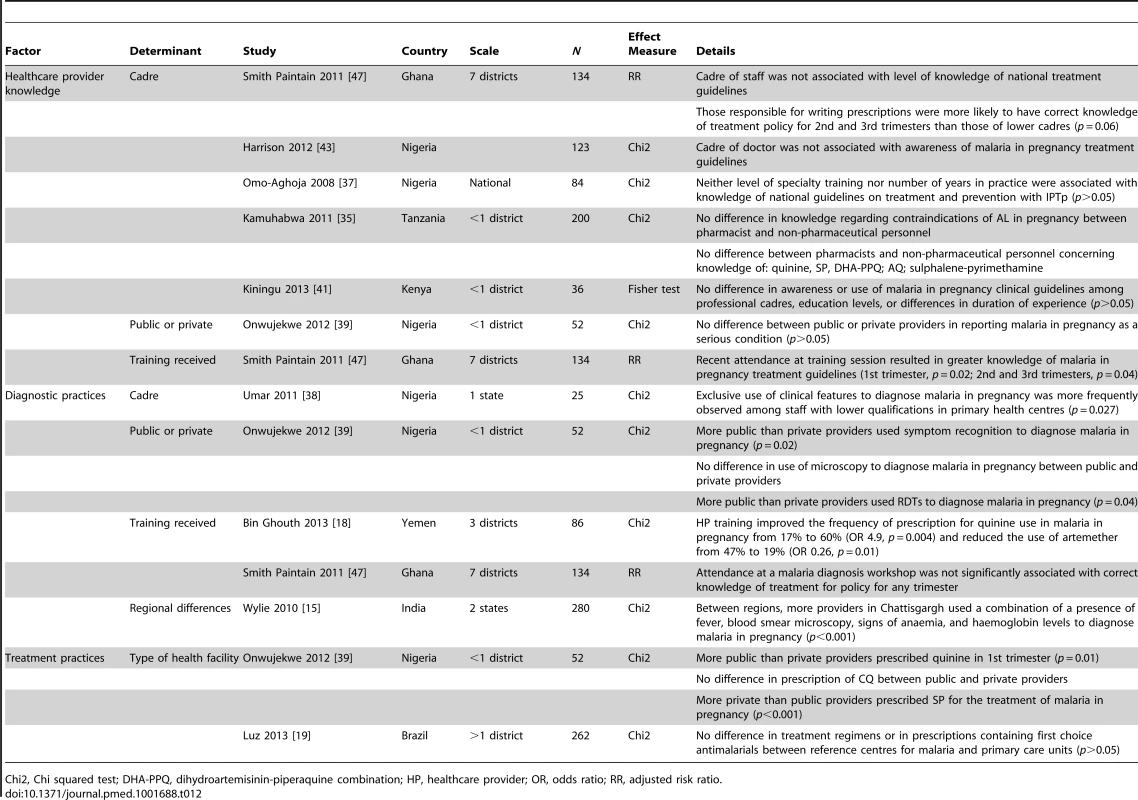
Chi2, Chi squared test; DHA-PPQ, dihydroartemisinin-piperaquine combination; HP, healthcare provider; OR, odds ratio; RR, adjusted risk ratio. Intervention studies
Only one intervention study was identified, which evaluated the effect of in-service training of clinicians and pharmacists in the private sector in three governorates in Yemen on malaria treatment in pregnant women [18]. The post-training assessment showed improved knowledge of correct dosing, from 17% to 60%, still far short of 100%.
Discussion
To our knowledge this review draws together for the first time findings from disparate studies on the treatment-seeking practices for malaria in pregnant women and the case management practices of a range of healthcare providers globally. The key emerging themes are relatively consistent across a range of study settings in terms of local cultural, socio-economic, health system, and non–health system contexts, and geographical locations. One - to three-quarters of women reported malaria illness during pregnancy, of whom treatment was sought by >85%. Self-medication and traditional healers were reportedly used by 5% to 40% of women, alongside care from the formal health sector (range 42%–92%). Knowledge of drug safety, cost, and perceptions of healthcare services affected treatment choices. Determinants of treatment seeking were education and prior experience of miscarriage or ANC use. Healthcare providers' reliance on clinical diagnosis and poor adherence to treatment guidelines by trimester were consistently reported. Prescribing practices were driven by poor knowledge of national guidelines and concerns over side effects and drug safety, patient preference, drug availability, and cost. Determinants of provider practices were individual provider factors (cadre, training), facility type (public or private; primary or tertiary), and sub-national region.
The review highlights important limitations in the implementation of the WHO policy on treatment of malaria in pregnancy [1],[2]. There is an apparent disconnect between the theories that underpin WHO policy and the beliefs and attitudes of women, in addition to which there is dissonance between the principles of delivery of quality care, and the experiences and practices of pregnant women and healthcare providers (Figure 5). Importantly, women do not uniformly seek care within the formal health system, and when they do, they may not access appropriate diagnosis and treatment, because of poor healthcare provider skills or inadequate resources or because they cannot afford to pay for the services.
Fig. 5. Integration of findings in relation to WHO case management policy [1]. ![Integration of findings in relation to WHO case management policy <em class="ref">[1]</em>.](https://www.prelekara.sk/media/cache/resolve/media_object_image_small/media/image/0fb4d4f68a0ece74e81cd599c6e51928.png)
LBW, low birth weight. Barriers to access among women—in particular, poor knowledge of drug safety, prohibitive costs, and self-treatment practices—suggest ministries of health need to improve women's access to information so that they can make informed choices. Educating women about the risks of malaria in pregnancy will be important, especially as the manifestation of malaria illness in pregnancy may be confused with pregnancy-related symptoms [53]. Even when women think they have malaria, a series of socio-cultural factors impede women's ability to act, such as not wishing to disclose their pregnancy status and other factors operating at the household level that restrict women's autonomy to seek care, as reported by others [17],[53],[54]. The finding that pregnant women may self-treat for malaria was partly attributed by the reviewed studies to the irregular and inadequate supply of drugs at health facilities. Given that alternative care providers include shop vendors (who are poorly informed or otherwise incentivised to give more expensive and sometimes inappropriate drugs) and TBAs (who practice and promote herbal remedies and traditional herbs as healthier or less risky to the developing foetus) [45], women need appropriate information about which antimalarials are recommended and safe to use for the treatment of malaria at different stages of pregnancy. Advertising provides an opportunity for governments to add messages about safety and use of antimalarials in pregnancy, and information pamphlets could be given to women at ANC facilities. One of the main barriers to women seeking treatment for malaria at formal health facilities is cost, both direct costs such as user fees and indirect costs, as has been reported in studies on antenatal care seeking more broadly [55],[56]. The economic barriers to accessing expensive diagnostic tests and treatment for malaria among pregnant women have been reported previously [57] and warrant a review of strategies to reach pregnant women with safe and affordable treatment options.
Diagnosis of malaria in pregnancy in many settings is challenging. In stable and high transmission settings, parasitological diagnosis based on microscopy or RDTs potentially reduces the unnecessary use of antimalarials in pregnancy, particularly in areas of high HIV prevalence, where HIV-infected patients have a high incidence of febrile illness [2]. As our review shows, the reality in resource-constrained public health facilities and among community providers is that diagnosis is frequently restricted to clinical symptoms. As observed in a clinical study among pregnant women in Mozambique, the positive predictive values of the three most common malaria symptoms—headache, arthromyalgias, and history of fever—for malaria parasitaemia were low (28%, 29%, and 33%, respectively) [58]. Even where diagnostic tests are available, studies reported that providers sometimes choose to ignore negative test results and prescribe antimalarials when malaria is suspected. The reasons for ignoring diagnostic test results are likely to be a combination of factors related to user preferences and demand, suspected insensitivity or inferiority of the tests, inferior reagents, or lack of trust in the accuracy of slide reading by laboratory staff. Efforts are needed to scale up the availability of RDTs at points of care used by pregnant women and to improve provider proficiency in their application.
Healthcare providers from a range of countries and continents and across a variety of cadres in the private and public sectors, and formal and informal sectors, demonstrated poor knowledge of and adherence to national treatment policy guidelines. Poor knowledge of and availability of treatment guidelines, and concerns over side effects and drug safety suggest the need for refresher training, job aids, and improved supervision. The finding that doctors were less likely to prescribe correctly may reflect personal judgements based on knowledge or individual client needs, as noted in a study in Zimbabwe where many practitioners felt that guidelines would limit their personal flexibility in caring for patients [59]. Health system strengthening is needed to improve drug availability, as well as legislation to promote rational drug use to eliminate the use of monotherapies and other non-recommended antimalarials across all service providers. Efforts by ministries of health to incorporate private sector providers into centralised training and dissemination activities on national treatment policy are needed. In addition, a licensing system to regulate which antimalarials are sold at the community level is needed to prohibit the use of monotherapies and to reduce women's exposure to ineffective drugs and the potential risks of ACT use in the first trimester.
With the advent of the 2006 WHO policy [2], inadvertent exposure to ACTs among pregnant women in the first trimester has been a considerable public health concern [3],[60]. Few studies in our review stratified antimalarial use by trimester; of those that did, prescription of ACTs in the first trimester was reported in Ghana, CAR, and Nigeria. This is a very real concern, and research by the Malaria in Pregnancy Consortium is ongoing to develop pharmacovigilance systems that can be implemented in resource-poor countries to monitor the safety of antimalarials in pregnancy, including inadvertent exposures in the early first trimester [61]. The continued use of drugs that are no longer recommended in national treatment policies, such as SP (recommended for IPTp only) in Ghana and Nigeria, and CQ in Nigeria (because of known high levels of parasite resistance to CQ) [62], is another area for concern. The use of artemisinin monotherapies is a major threat for the development of artemisinin resistance in the Africa region, as occurred in parts of Asia [63],[64].
The dearth of implementation research on interventions to improve the quality of case management of malaria in pregnancy underscores the fact that this is a neglected area of research, despite case management constituting one of the three key strategies for controlling malaria in pregnancy in sub-Saharan Africa, and a lifesaving intervention for both mother and child in lower transmission settings in Asia and Latin America. Research using standardised methodologies is needed to systematically document treatment seeking in pregnant women and healthcare provider practices across a range of countries and settings. Implementation research is needed to evaluate the impact of strengthened public sector practices on pregnant women's access to malaria treatment in the public sector, as well as strategies that target private drug sellers, such as better information, communication, and legislation for rational drug use.
Strengths and Limitations
The review uses data from quantitative, qualitative, and mixed methods studies to increase the comprehensiveness of the review; studies with quantitative data provided frequencies of practices, the qualitative data provided important explanatory factors driving those behaviours, and the content analysis was useful to determine the frequency of reporting of the different factors associated with case management of malaria in pregnancy across studies. We did not attempt a meta-ethnography, as has been done by others [53]. The primary geographic scope of the review is Africa, since this is where the majority of the included studies were undertaken, with few available studies in Asia and Latin America. Whilst no restrictions were placed on the language, and no studies were excluded on the basis of language, the focus of the Malaria in Pregnancy Library (the primary source of studies) to date has been the European family of languages, predominantly English. Reviewer bias was limited by the use of two reviewers to independently assess inclusion criteria. The reporting of the included studies was assessed for quality, and reporting quality for the majority of studies was assessed to be moderate to high. Findings from five studies [12],[35],[44],[51],[52] assessed to be of low quality (meeting <50% of the quality criteria) were consistent with the other studies. Inconsistency in study methodologies and end points precluded a meta-analysis of pooled data of the determinants of women's access to treatment or healthcare provider case management practices. In the meta-analysis for source of treatment, there may have been overlap between sources of treatment reported, e.g., a doctor may practice in a health facility, antenatal clinic, or private clinic.
The majority of studies of women were undertaken at sub-district, district, or state level, which limits the generalisability of the individual studies. There was reasonable consistency of findings across different studies in the same country and across studies in different countries. The studies of healthcare providers had greater geographic scope, with eight of 18 studies undertaken in more than one district or state, three of which were done at national level.
Conclusions
Our review highlights the poor quality of case management practices for malaria in pregnancy across many parts of Africa, Asia, and Latin America. These practices not only threaten the health outcomes for mothers and their infants, but endanger the prospective useful life of several therapeutic drugs, in particular the artemisinins, through the continued use of monotherapies. The challenge for ministries of health will be the deployment of legislative and quality improvement interventions to reach the broad range of healthcare providers that administer antimalarial drugs in the community, in the private and public sectors as well as in the formal and informal sectors. Further implementation research using standardised methodologies is needed to systematically assess the extent of substandard case management practices at the national scale, to review how policies are implemented and disseminated by countries, and to assess practitioner and patient adherence. Research to evaluate targeted or multifaceted interventions aimed to improve the delivery of and access to quality case management services for pregnant women should be a priority.
Supporting Information
Zdroje
1. World Health Organization (2010) Guidelines for the treatment of malaria, second edition. Geneva: World Health Organization.
2. World Health Organization (2006) Guidelines for the treatment of malaria. Geneva: World Health Organization.
3. WardSA, SeveneEJ, HastingsIM, NostenF, McGreadyR (2007) Antimalarial drugs and pregnancy: safety, pharmacokinetics, and pharmacovigilance. Lancet Infect Dis 7 : 136–144.
4. Roll Back Malaria (2014) Global malaria action plan for a malaria-free world: Part II: the global strategy. 2. Overcoming malaria. Available: http://www.rollbackmalaria.org/gmap/2-2.html#. Accessed 20 May 2014.
5. HillJ, HoytJ, van EijkAM, D'Mello-GuyettL, Ter KuileFO, et al. (2013) Factors affecting the delivery, access, and use of interventions to prevent malaria in pregnancy in sub-Saharan Africa: a systematic review and meta-analysis. PLoS Med 10: e1001488.
6. van EijkAM, HillJ, PovallS, ReynoldsA, WongH, et al. (2013) The Malaria in Pregnancy Library: a bibliometric review. Malar J 11 : 362.
7. EBSCO Information Services (2014) Global Health Database [database]. Available: http://www.ebscohost.com/corporate-research/global-health. Accessed 15 April 2014.
8. International Network for the Rational Use of Drugs (2014) INRUD Bibliography [database]. Available: http://www.inrud.org/Bibliographies/INRUD-Bibliography.cfm. Accessed 7 April 2014.
9. AdamT, HsuJ, de SavignyD, LavisJN, RottingenJA, et al. (2012) Evaluating health systems strengthening interventions in low-income and middle-income countries: are we asking the right questions? Health Policy Plan 27 (Suppl 4)iv9–iv19.
10. de SavignyD, WebsterJ, AgyepongIA, MwitaA, Bart-PlangeC, et al. (2012) Introducing vouchers for malaria prevention in Ghana and Tanzania: context and adoption of innovation in health systems. Health Policy Plan 27 (Suppl 4)iv32–iv43.
11. World Health Organization (2009) Systems thinking for health systems strengthening. Geneva: World Health Organization.
12. MaigaAS, DiakiteM, DiawareA, SangoHA, CoulibalyCO (2010) [Pharmacovigilance and impact of intermittent preventive treatment with sulfadoxine-pyrimethamine for pregnant women in Selingue in Mali.]. Mali Med 25 : 41–48.
13. Deeks JJ, Higgins JPT, Altman DG, editors (2009) Analysing data and undertaking meta-analyses. In: Higgins JPT, Green S, editors. Cochrane handbook for systematic reviews of interventions. Chichester (UK): The Cochrane Collaboration.
14. SabinLL, RizalA, BrooksMI, SinghMP, TuchmanJ, et al. (2010) Attitudes, knowledge, and practices regarding malaria prevention and treatment among pregnant women in Eastern India. Am J Trop Med Hyg 82 : 1010–1016.
15. WylieBJ, HashmiAH, SinghN, SinghMP, TuchmanJ, et al. (2010) Availability and utilization of malaria prevention strategies in pregnancy in eastern India. BMC Public Health 10 : 557.
16. Population Services International Research and Metrics (2007) Cambodia 2007: TRaC study exploring the determinants of malaria health care provision among private providers in malaria endemic areas—first round. Washington (District of Columbia): Population Services International.
17. Tawfik L (2006) Mosquitoes, malaria and malarine: a qualitative study on malaria drug use in Cambodia. Arlington (Virginia): US Agency for International Development.
18. Bin GhouthAS (2013) Availability and prescription practice of anti-malaria drugs in the private health sector in Yemen. J Infect Dev Ctries 7 : 404–412.
19. LuzTCB, MirandaES, FreitasLF, Osorio-de-CastroCGS (2013) Prescriptions for uncomplicated malaria treatment among pregnant women in the Brazilian Amazon: evidences from the Mafalda Project. Rev Bras Epidemiol 16 : 409–419.
20. LuzTC, Suarez-MutisC, MirandaS, MoritzF, FreitasF, et al. (2013) Uncomplicated malaria among pregnant women in the Brazilian Amazon: local barriers to prompt and effective case management. Acta Trop 125 : 137–142.
21. PellC, MeñacaA, AfrahNA, Manda-TaylorL, ChatioS, et al. (2013) Prevention and management of malaria during pregnancy: findings from a comparative qualitative study in Ghana, Kenya and Malawi. Malar J 12 : 427.
22. LaunialaA, HonkasaloML (2010) Malaria, danger, and risk perceptions among the Yao in rural Malawi. Med Anthropol Q 24 : 399–420.
23. Smith PaintainLA, JonesC, AdjeiRO, AntwiGD, AfrahNA, et al. (2010) Intermittent screening and treatment versus intermittent preventive treatment of malaria in pregnancy: user acceptability. Malar J 9 : 18.
24. MbachuCO, OnwujekweOE, UzochukwuBS, UchegbuE, OranubaJ, et al. (2012) Examining equity in access to long-lasting insecticide nets and artemisinin-based combination therapy in Anambra state, Nigeria. BMC Public Health 12 : 315.
25. SangaréLR, WeissNS, BrentlingerPE, RichardsonBA, StaedkeSG, et al. (2011) Patterns of anti-malarial drug treatment among pregnant women in Uganda. Malar J 10 : 152.
26. HenryOJ, LagoroKD, OrachCG (2012) Prevalence of malaria and treatment seeking behaviours among pregnant women in postconflict internally displaced persons' camps in Gulu District. ISRN Public Health 2012 : 164935 doi:10.5402/2012/164935
27. EnatoEF, MensPF, OkhamafeAO, OkpereEE, PogosonE, et al. (2009) Plasmodium falciparum malaria in pregnancy: prevalence of peripheral parasitaemia, anaemia and malaria care-seeking behaviour among pregnant women attending two antenatal clinics in Edo State, Nigeria. J Obstet Gynaecol 29 : 301–306.
28. ObiecheAO, EnatoEF, AndeAB (2013) Patterns of treatment of reported malaria cases during pregnancy in a Nigerian hospital. Scand J Infect Dis 45 : 849–854.
29. OnwujekweO, OnwujekweOO, SoremekunR (2013) Chemotherapy and chemoprophylaxis of malaria in pregnancy in private and public facilities: perceptions and use by pregnant women in Enugu State, Nigeria. Gend Behav 11 : 5688–5697.
30. Kwansa-BentumB, AyiI, SuzukiT, OtchereJ, KumagaiT, et al. (2011) Administrative practices of health professionals and use of artesunate-amodiaquine by community members for treating uncomplicated malaria in southern Ghana: implications for artemisinin-based combination therapy deployment. Trop Med Int Health 16 : 1215–1224.
31. AdamI, OmerEsM, SalihA, KhamisA, MalikEM (2008) Perceptions of the causes of malaria and its complications, treatment and prevention among midwives and pregnant women of Eastern Sudan. J Public Health 16 : 129–132.
32. KarunamoorthiK, DebochB, TafereY (2010) Knowledge and practice concerning malaria, insecticide-treated net (ITN) utilization and antimalarial treatment among pregnant women attending specialist antenatal clinics. J Public Health 18 : 559–566.
33. Sam-WoboSO, AkinboroyeT, AnosikeJC, AdewaleB (2008) Knowledge and practices on malaria treatment measures among pregnant women in Abeokuta, Nigeria. Tanzan J Health Res 10 : 226–231.
34. MbonyeAK, BirungiJ, YanowS, MagnussenP (2013) Prescription patterns and drug use among pregnant women with febrile Illnesses in Uganda: a survey in out-patient clinics. BMC Infect Dis 13 : 237.
35. KamuhabwaAR, MnyusiwallaF (2011) Rational dispensing and use of artemether-lumefantrine during pregnancy in Dar es Salaam, Tanzania. Tanzan J Health Res 13.
36. ManirakizaA, SoulaG, LaganierR, KlementE, DjalleD, et al. (2011) Pattern of the antimalarials prescription during pregnancy in Bangui, Central African Republic. Malar Res Treat 2011 : 414510.
37. Omo-AghojaLO, AghojaCO, OghagbonK, Omo-AghojaVW, EsumeC (2008) Prevention and treatment of malaria in pregnancy in Nigeria: obstetrician's knowledge of guidelines and policy changes-a call for action. J Chin Clin Med 3 : 114–120.
38. UmarMT, ChikaA, JimohAO (2011) Compliance of primary health care providers to recommendation of artemesinin-based combination therapy in the treatment of uncomplicated malaria in selected primary health care centres in Sokoto, north western Nigeria. Int J Trop Med 6 : 70–72.
39. OnwujekweOC, SoremekunRO, UzochukwuB, ShuE, OnwujekweO (2012) Patterns of case management and chemoprevention for malaria-in-pregnancy by public and private sector health providers in Enugu state, Nigeria. BMC Res Notes 5 : 211.
40. OkoroRN, NwambuJO (2012) Evaluation of physicians' prescribing patterns of antimalarial drugs during pregnancy at the obstetrics and gynaecology department of a teaching hospital in Maduguri, Borno State, Nigeria. Int J Pharm Biomed Sci 3 : 39–46.
41. Kiningu DK (2013) Factors influencing the use of evidence based guidelines in the management of malaria in pregnancy among health workers at Garissa Provincial Hospital, Kenya [Master's thesis]. Nairobi: School of Public Health, University of Nairobi. Available: http://erepository.uonbi.ac.ke:8080/xmlui/bitstream/handle/11295/59598/Factors%20Influencing%20The%20Use%20Of%20Evidence%20Based%20Guidelines%20in%20the%20Management%20of%20Malaria%20in%20Pregnancy%20Among%20Health%20Workers%20at%20Garissa%20Provincial%20Hospital%20Kenya.pdf?sequence=3. Accessed 7 July 2014
42. Kalilani-PhiriLV, LunguD, CoghlanR (2011) Knowledge and malaria treatment practices using artemisinin combination therapy (ACT) in Malawi: survey of health professionals. Malar J 10 : 279.
43. HarrisonN, OlufunlayoT, AgomoC (2012) Utilization of the current national antimalarial treatment guidelines among doctors in army hospitals in Lagos, Nigeria. Open J Prev Med 2 : 390–393.
44. EnatoEFO, ErihriRE (2012) Knowledge, perception and management of malaria in pregnancy by traditional birth attendants in Benin City. J Pharm Allied Sci 8 : 1292–1297.
45. StangelandT, AlelePE, KatuuraE, LyeKA (2011) Plants used to treat malaria in Nyakayojo sub-county, western Uganda. J Ethnopharmacol 137 : 154–166.
46. OkontaPI (2011) How many physicians prescribe quinine for the treatment of malaria in the first trimester of pregnancy? Ebonyi Med J 10 : 105–111.
47. Smith PaintainL, AntwiGD, JonesC, AmoakoE, AdjeiRO, et al. (2011) Intermittent screening and treatment versus intermittent preventive treatment of malaria in pregnancy: provider knowledge and acceptability. PLoS ONE 6: e24035.
48. Malawi Ministry of Health (2008) Republic of Malawi Ministry of Health national malaria control program supervision report for monitoring ACT and malaria control activities. Lilongwe: Malawi Ministry of Health.
49. Uganda Ministry of Health (2005) National policy on malaria treatment 2005. Kampala: Uganda Ministry of Health.
50. Tanzania Ministry of Health and Social Welfare (2006) National guidelines for malaria diagnosis and treatment 2005. Dar es Salaam: Tanzania Ministry of Health and Social Welfare.
51. MinyaliwaC, BandaweC, MwaleRJ (2012) How much do Blantyre dispensers in hospital and community pharmacies know about the new malaria treatment guidelines? Malawi Med J 24 : 1–4.
52. MbonyeAK, MagnussenP (2010) Symptom-based diagnosis of malaria and its implication on antimalarial drug use in pregnancy in central Uganda: results from a community trial. Int J Adolesc Med Health 22 : 257–262.
53. PellC, StrausL, AndrewEVW, MeñacaA, PoolR (2011) Social and cultural factors affecting uptake of interventions for malaria in pregnancy in Africa: a systematic review of the qualitative research. PLoS ONE 6: e22452.
54. FinlaysonK, DowneS (2013) Why do women not use antenatal services in low - and middle-income countries? A meta-synthesis of qualitative studies. PLoS Med 10: e1001373.
55. JohnsonA, GossA, BeckermanJ, CastroA (2012) Hidden costs: the direct and indirect impact of user fees on access to malaria treatment and primary care in Mali. Soc Sci Med 75 : 1786–1792.
56. PerkinsM, BrazierE, ThemmenE, BassaneB, DialloD, et al. (2009) Out-of-pocket costs for facility-based maternity care in three African countries. Health Policy Plan 24 : 289–300.
57. WorrallE, MorelC, YeungS, BorghiJ, WebsterJ, et al. (2007) The economics of malaria in pregnancy—a review of the evidence and research priorities. Lancet Infect Dis 7 : 156–168.
58. BardajiA, SigauqueB, BruniL, RomagosaC, SanzS, et al. (2008) Clinical malaria in African pregnant women. Malar J 7 : 27.
59. BhagatK, NyazemaN (2001) General practitioners and clinical guidelines. East Afr Med J 78 : 30–34.
60. CrawleyJ, HillJ, YarteyJ, RobaloM, SerufiliraA, et al. (2007) From evidence to action? Challenges to policy change and programme delivery for malaria in pregnancy. Lancet Infect Dis 7 : 145–155.
61. DellicourS, ter KuileFO, StergachisA (2008) Pregnancy exposure registries for assessing antimalarial drug safety in pregnancy in malaria-endemic countries. PLoS Med 5: e187.
62. Bloland P (2001) Drug resistance in malaria. WHO/CDS/CSR/DRS/2001.4. Geneva: World Health Organization.
63. World Health Organization (2005.) Global report on antimalarial drug efficacy and drug resistance: 2000–2010. Geneva: World Health Organization.
64. FairhurstRM, NayyarGM, BremanJG, HallettR, VennerstromJL, et al. (2012) Artemisinin-resistant malaria: research challenges, opportunities, and public health implications. Am J Trop Med Hyg 87 : 231–241.
Štítky
Interné lekárstvo
Článok vyšiel v časopisePLOS Medicine
Najčítanejšie tento týždeň
2014 Číslo 8- Parazitičtí červi v terapii Crohnovy choroby a dalších zánětlivých autoimunitních onemocnění
- Intermitentní hladovění v prevenci a léčbě chorob
- Statinová intolerance
- Co dělat při intoleranci statinů?
- Monoklonální protilátky v léčbě hyperlipidemií
-
Všetky články tohto čísla
- Observational Studies: Getting Clear about Transparency
- Scaling up Rural Sanitation in India
- Intervention Synthesis: A Missing Link between a Systematic Review and Practical Treatment(s)
- From Intense Rejection to Advocacy: How Muslim Clerics Were Engaged in a Polio Eradication Initiative in Northern Nigeria
- Ethics, Economics, and the Use of Primaquine to Reduce Falciparum Malaria Transmission in Asymptomatic Populations
- Hand Sanitiser Provision for Reducing Illness Absences in Primary School Children: A Cluster Randomised Trial
- Protective Efficacy and Safety of Three Antimalarial Regimens for the Prevention of Malaria in Young Ugandan Children: A Randomized Controlled Trial
- Heart Failure: Gaps in Knowledge and Failures in Treatment
- Staffing of Healthcare Workers and Patient Mortality: Randomized Trials Needed
- Associations between Stroke Mortality and Weekend Working by Stroke Specialist Physicians and Registered Nurses: Prospective Multicentre Cohort Study
- Women's Access and Provider Practices for the Case Management of Malaria during Pregnancy: A Systematic Review and Meta-Analysis
- Stress Hyperglycaemia in Hospitalised Patients and Their 3-Year Risk of Diabetes: A Scottish Retrospective Cohort Study
- The Effect of India's Total Sanitation Campaign on Defecation Behaviors and Child Health in Rural Madhya Pradesh: A Cluster Randomized Controlled Trial
- Heart Failure Care in Low- and Middle-Income Countries: A Systematic Review and Meta-Analysis
- PLOS Medicine
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Women's Access and Provider Practices for the Case Management of Malaria during Pregnancy: A Systematic Review and Meta-Analysis
- Observational Studies: Getting Clear about Transparency
- Heart Failure Care in Low- and Middle-Income Countries: A Systematic Review and Meta-Analysis
- Scaling up Rural Sanitation in India
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy