-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Monitoring and Evaluating Progress towards Universal Health Coverage in Chile
article has not abstract
Published in the journal: Monitoring and Evaluating Progress towards Universal Health Coverage in Chile. PLoS Med 11(9): e32767. doi:10.1371/journal.pmed.1001676
Category: Collection Review
doi: https://doi.org/10.1371/journal.pmed.1001676Summary
article has not abstract
This paper is part of the PLOS Universal Health Coverage Collection. This is the summary of the Chile country case study. The full paper is available as Supporting Information file Text S1.
Background
With the establishment of the social security system in 1924, Chile started the path towards UHC. A key milestone was the creation of the National Health System in 1952, which offered public subsidized coverage for the poor [1]. Currently, after the partial privatization of social security in 1981 the health system is mixed, both in insurance and in service provision [2], and health insurance reaches 98% of the population, with 77% of this coverage by the public health insurance [3]. Regardless of this encouraging figure and a relatively good health situation, a significant burden of out-of-pocket (OOP) payment exists and the access to care has been described as noticeably inequitable between the public and private sectors [4],[5],[6],[7].
Defining UHC as a situation where all people obtain the health services they need without risking financial hardship from unaffordable out - of-pocket payments [8], this article reviews the case of Chile, with the aim of identifying indicators to monitor and evaluate UHC.
Universal Health Coverage: The Policy Context
Since 2013, Chile has been ranked among high-income economies; life expectancy is 79 years [9]; poverty has fallen [10]; and education attainment has increased [11]. Despite all these positive trends, inequality still remains as one of the main challenges faced by the country [12].
In an attempt to tackle health inequities and to increase financial protection, in 2005 the Chilean government implemented an innovative health reform, with the central focus of the recognition of the right to health. This focus lead to the establishment of “explicit guarantees” for 80 prioritized health problems. The legal binding guarantee gives equal rights to the beneficiaries of the public and private sectors in four key aspects: access to health care (eligibility), timeliness of care (maximum waiting times), financial protection (maximum co-payments and deductibles), and quality of care (accreditation of facilities and professional certification) [13].
Monitoring and Evaluation of UHC
Following main components of the UHC definition, we estimated or compiled two sets of indicators reflecting coverage of health services and financial protection coverage, set in a larger health services results framework [14]. Two priority groups were included for intervention coverage: Millennium Development Goals (MDGs) diseases and non-communicable diseases (NCDs). OOP health expenditure, as percentage of total household expenditure/income and as percentage of households facing catastrophic health expenditure, was used to reflect financial protection (FP) coverage. Household income, education, gender, and residence were used for equity disaggregation, adding ascription to public/private health insurance.
Progress towards UHC in Chile
Coverage of health insurance is high, but there are still some gaps in needed health services and the quality is not sufficient to have effective treatments.
NCDs are the leading causes of burden of diseases; however, their coverage is lower compared to MDGs diseases (infectious diseases, and maternal and child care, such as in antenatal care, family planning and skilled birth attendance), especially when measuring effective coverage (Figure 1). Additionally, prevalence of risk factors denotes minimum impact of preventive interventions. Equity disaggregation tends to show lower coverage for males, low-income quintiles, less-educated people, residents in rural areas, and people with ascription to public health insurance. Finally, some increasingly important diseases, such as dementias and others with catastrophic cost (like inherited metabolic disorders), are not adequately covered.
Fig. 1. Coverage of interventions: tracer indicators for MDGs diseases and NCDs. 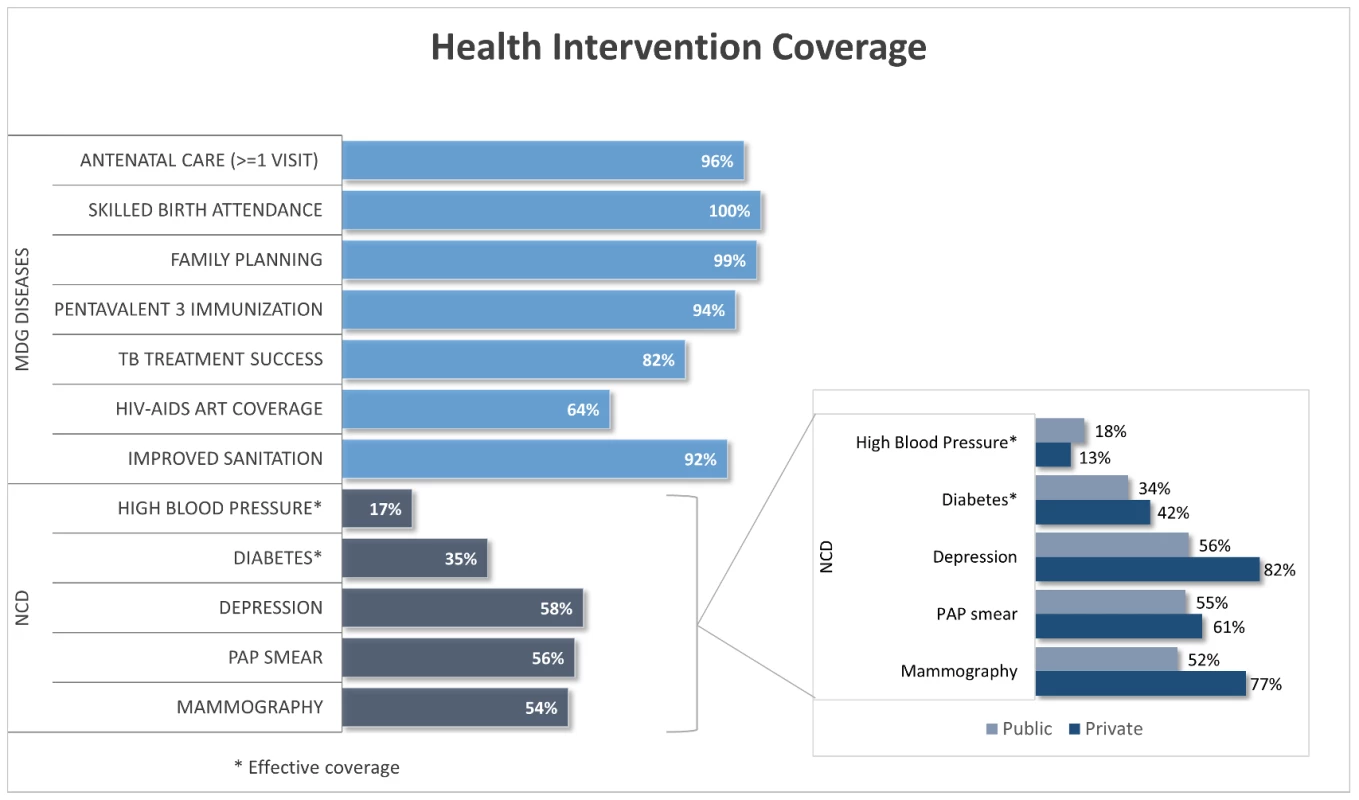
Source: Based on Ministry of Health, National Health Survey 2009-10[15], and CASEN Survey 2011 [16]. About 5% of the total expenditure at household level is devoted to paying for healthcare services and 1.9% of households face catastrophic health expenditures, with a 40% threshold (3.6% using 30% threshold), although both are progressive (Figure 2). Higher catastrophic costs among richer families could be related to the exemption of co-payment for the poorest quintiles, but also to equity gaps in complex services utilization.
Fig. 2. Financial protection tracer indicators. Source: Based on <em class="ref">[17]</em>. ![Financial protection tracer indicators. Source: Based on <em class="ref">[17]</em>.](https://www.prelekara.sk/media/cache/resolve/media_object_image_small/media/image/a21ce53a2e18410497b8009084bbaf06.png)
Conclusions and Recommendations
Over the last 90 years, the Chilean health system has moved towards UHC; however, structural constraints prevent further advancement and create gaps and inequities in terms of services coverage, which impact on health results [18],[19]. Moreover, it is observed that OOP payments have increased and the population still is not totally protected from the risk of facing catastrophic health expenditures.
Public spending is one of the lowest among OECD countries and OOP payments are the highest [20]. System fragmentation, at health insurance and provision levels, results in two realities: an underfunded and overwhelmed public sector and an elitist and increasingly expensive private sector.
UHC monitoring through indicators is feasible in Chile but requires a more robust information system. The Chilean health information system provides data for the required aspects. However, there are missing data for some priority health interventions and for equity disaggregation; at the same time, the consistency and periodicity of health surveys is not guaranteed. Additionally, FP figures only represent the city of Santiago. Overall, Chile has relevant and useful information that allows measuring and monitoring the path towards UHC.
Increasing resources available for healthcare, establishing solidarity among public and private sectors, and improving quality of care to expand effective coverage are key components towards achieving UHC in Chile.
Supporting Information
Zdroje
1. Mardones-RestarF, AzevedoA (2006) The essential health reform in Chile: a reflection on the 1952 process. Salud Pública de Mex 48(6): 504–511.
2. Berrecil-MontekioV, ReyesJD, ManuelA (2011) Sistema de Salud de Chile. Salud Pública Mex 53 supl 2SI 32–SI 43.
3. FONASA (2013) Estadísticas FONASA 2009: Demografía. Available: http://www.fonasa.cl/wps/wcm/connect/03c92fb1-3e3d-4171-bcb5-15d69d868686/01+ - Demograf %C3%ADa_pagina_web_%2822-08 - 011%29JAV.xls?MOD = AJPERES&atta chment = true&id = 1313788185537l. Accessed 23 September 2013.
4. ArteagaO, AstorgaI, PintoAM (2002) Inequalities in Public Health Care Provision in Chile. Cad Saúde Pública 18(4): 1053–66 Available: http://www.ncbi.nlm.nih.gov/pubmed/12118310 Accessed 15 November 2013..
5. Frenz P, Delgado I, Kaufman JS, Harper S (2013) Achieving Effective Universal Health Coverage with Equity: Evidence from Chile. Health Policy Plan. Epub ahead of print. Available: http://www.ncbi.nlm.nih.gov/pubmed/23921988. Accessed 15 November 2013.
6. NúñezA, ChiCh (2013) Equity in health care utilization in Chile. Int J Equity Health 12(1): 58 Available: http://www.ncbi.nlm.nih.gov/pubmed/23937894 Accessed 11 September 2013..
7. ParajeG, VásquezF (2012) Health equity in an unequal country: the use of medical services in Chile. Int J Equity Health 11 : 81 Available: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3544610&tool=pmcentrez&rendertype=abstract Accessed 15 November 2013..
8. WHO (2005) Sustainable health financing, universal coverage and social health insurance. World Health Assembly Resolution 58.33, 2005.
9. World Bank. Statistics (2013) Available: http://data.worldbank.org/indicator?display=default. Accessed 13 August 2013.
10. MDS - Ministry of Social Development (2012a) Poverty Results CASEN 2011. Available: http://observatorio.ministeriodesarrollosocial.gob.cl/layout/doc/casen/pobreza_casen_2011.pdf. Accessed 11 August 2013.
11. MDS - Ministry of Social Development (2012b) Education Results CASEN 2011. Available: http://observatorio.ministeriodesarrollosocial.gob.cl/layout/doc/casen/2013_04_01_Educacion_CASEN_2011.pdf. Accessed 11 August 2013.
12. MDS - Ministry of Social Development (2012c) Income Distribution Results CASEN 2011. Available: http://observatorio.ministeriodesarrollosocial.gob.cl/layout/doc/casen/001_ingreso_2011.pdf. Accessed 11 August 2013.
13. Library of Congress (2004) History of Law N°19.966: Establishes the Explicit Health Guarantees Regime. Ministry of Health. Chilean Government. Document in Spanish.
14. Evans D, Saksena P, Elovainio R, Boerma T (2012) Measuring Progress towards Universal Coverage. July 2012. Geneva, WHO.
15. MoH – Ministry of Health (2010) National Health Survey 2009-10. Database.
16. MDS – Ministry of Social Development (2011) Socioeconomic Characterization Survey 2011. Database.
17. CidC, PrietoL (2012) El gasto de bolsillo en salud: el caso de Chile, 1997 y 2007. Rev Panam Salud Publica 31(4): 310–316.
18. Chilean Government (2011) National Health Strategy 2011–2020 (Estrategia Nacional de Salud para el Cumplimiento de los Objetivos Sanitarios de la Década 2011–2020).
19. MoH – Ministry of Health (2010) Evaluación de Los Objetivos Sanitarios para la Década 2000–2010. 1st ed. ed. Claudia Gonzalez. Ministerio de Salud de Chile.
20. OECD Statistics (2013) OECD Health Data 2013. Frequently Requested Data. Available: http://www.oecd.org/health/health-systems/oecdhealthdata2013-frequentlyrequesteddata.htm. Accessed 11 September 2013.
Štítky
Interné lekárstvo
Článok vyšiel v časopisePLOS Medicine
Najčítanejšie tento týždeň
2014 Číslo 9- Parazitičtí červi v terapii Crohnovy choroby a dalších zánětlivých autoimunitních onemocnění
- Nech brouka žít… Ať žije astma!
- Intermitentní hladovění v prevenci a léčbě chorob
- Co dělat při intoleranci statinů?
- Monoklonální protilátky v léčbě hyperlipidemií
-
Všetky články tohto čísla
- Monitoring and Evaluating Progress towards Universal Health Coverage in Ghana
- Sorting Reality from What We Think We Know About Breast Cancer in Africa
- The PLOS “Monitoring Universal Health Coverage” Collection: Managing Expectations
- Monitoring and Evaluating Progress towards Universal Health Coverage in India
- Monitoring and Evaluating Progress towards Universal Health Coverage in Tanzania
- Monitoring and Evaluating Progress towards Universal Health Coverage in Brazil
- Monitoring and Evaluating Progress towards Universal Health Coverage in Thailand
- Monitoring and Evaluating Progress towards Universal Health Coverage in Estonia
- Monitoring and Evaluating Progress towards Universal Health Coverage in Chile
- Prioritizing Pregnant Women for Long-Lasting Insecticide Treated Nets through Antenatal Care Clinics
- Financial Risk Protection and Universal Health Coverage: Evidence and Measurement Challenges
- Convergence of Mortality Rates among Patients on Antiretroviral Therapy in South Africa and North America
- Malaria Prevention during Pregnancy—Is There a Next Step Forward?
- Beyond UHC: Monitoring Health and Social Protection Coverage in the Context of Tuberculosis Care and Prevention
- Intimate Partner Violence and Reproductive Coercion: Global Barriers to Women's Reproductive Control
- Genetic Predisposition to Increased Blood Cholesterol and Triglyceride Lipid Levels and Risk of Alzheimer Disease: A Mendelian Randomization Analysis
- Readmissions after Hospitalization for Heart Failure, Acute Myocardial Infarction, or Pneumonia among Young and Middle-Aged Adults: A Retrospective Observational Cohort Study
- Intermittent Preventive Treatment of Malaria in Pregnancy with Mefloquine in HIV-Infected Women Receiving Cotrimoxazole Prophylaxis: A Multicenter Randomized Placebo-Controlled Trial
- Equity-Oriented Monitoring in the Context of Universal Health Coverage
- The Clinical and Economic Impact of Point-of-Care CD4 Testing in Mozambique and Other Resource-Limited Settings: A Cost-Effectiveness Analysis
- Effective Coverage: A Metric for Monitoring Universal Health Coverage
- Mortality in Patients with HIV-1 Infection Starting Antiretroviral Therapy in South Africa, Europe, or North America: A Collaborative Analysis of Prospective Studies
- Global Financing and Long-Term Technical Assistance for Multidrug-Resistant Tuberculosis: Scaling Up Access to Treatment
- Oral Cholera Vaccine Development and Use in Vietnam
- Monitoring and Evaluating Progress towards Universal Health Coverage in Bangladesh
- Monitoring and Evaluating Progress towards Universal Health Coverage in South Africa
- Monitoring and Evaluating Progress towards Universal Health Coverage in Ethiopia
- Preventing Acute Malnutrition in Young Children: Improving the Evidence for Current and Future Practice
- Monitoring and Evaluating Progress towards Universal Health Coverage in Singapore
- Monitoring and Evaluating Progress towards Universal Health Coverage in China
- Monitoring and Evaluating Progress towards Universal Health Coverage in Tunisia
- Receptor-Defined Subtypes of Breast Cancer in Indigenous Populations in Africa: A Systematic Review and Meta-Analysis
- WHO Essential Medicines Policies and Use in Developing and Transitional Countries: An Analysis of Reported Policy Implementation and Medicines Use Surveys
- Intermittent Preventive Treatment of Malaria in Pregnancy with Mefloquine in HIV-Negative Women: A Multicentre Randomized Controlled Trial
- Preventing Acute Malnutrition among Young Children in Crises: A Prospective Intervention Study in Niger
- Monitoring Progress towards Universal Health Coverage at Country and Global Levels
- Monitoring Intervention Coverage in the Context of Universal Health Coverage
- Regular Breakfast Consumption and Type 2 Diabetes Risk Markers in 9- to 10-Year-Old Children in the Child Heart and Health Study in England (CHASE): A Cross-Sectional Analysis
- Proton Pump Inhibitors and Hospitalization with Hypomagnesemia: A Population-Based Case-Control Study
- PLOS Medicine
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Proton Pump Inhibitors and Hospitalization with Hypomagnesemia: A Population-Based Case-Control Study
- Monitoring and Evaluating Progress towards Universal Health Coverage in Chile
- Malaria Prevention during Pregnancy—Is There a Next Step Forward?
- Financial Risk Protection and Universal Health Coverage: Evidence and Measurement Challenges
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



