-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Náhlé příhody břišní u drogově závislých
Acute abdomen in drug abusers
Introduction:
Acute abdomen is one of the most important issues in abdominal surgery. Our study aims to describe the differences in clinical presentation of patients, in the course of their hospitalization, and in morbidity and mortality of patients with drug abuse; another aim is to describe our own experience with drug abusers with acute abdomen.
Method:
Patients with the history of drug abuse and with non-traumatic acute abdomen were included retrospectively to our set. We chose patients hospitalized between 2013 and 2018. We analyzed the demographical data of the patients, types of abused drugs, concordance between the first and final diagnosis, findings of paraclinical examinations, the need of surgical treatment, and the type of surgery. Morbidity, mortality and the length of hospital stay were tracked. All the data was evaluated using descriptive statistics.
Results:
8 patients (4.7 per mille of all the patients hospitalized for acute abdomen) fulfilled the criteria of our study. All the patients were men with median age 32 years. Pervitin (methamphetamine) was the most frequently abused drug (in 50%), followed by heroin, benzodiazepines, tetrahydrocannabinol, subutex, hypnotics and tramadol. Peptic ulcer perforation was the most frequent diagnosis in our set (in 50% of all patients). The other diagnoses included: two cases of upper gastrointestinal tract bleeding, one case of Crohn’s disease relapse with peritonitis and one case of colitis of the ascending colon. Surgical treatment was necessary in 75% patients. 30-day mortality was zero; an early complication (wound dehiscence) developed in one operated patient. Mean length of hospital stay was 9.7 days in our set, with the median of 7 days.
Conclusion:
Drug abusers represent only a marginal part of all patients with acute abdomen. This group is characterized by a significantly lower age, by a considerable predominance of men and by the preference of perforated peptic ulcer.
Key words:
acute abdomen, gastric and duodenal peptic ulcer perforation, drug abuse
Autoři: L. Hána; M. Ryska
Působiště autorů: Surgical Clinic of 2nd Faculty of Medicine of the Charles University and the Military University Hospital Prague
Vyšlo v časopise: Rozhl. Chir., 2019, roč. 98, č. 1, s. 14-17.
Kategorie: Původní práce
Souhrn
Úvod:
Náhlé příhody břišní (NPB) jsou jednou ze základních kapitol břišní chirurgie. Naše práce si klade za cíl popsat odlišnosti v klinickém obrazu, průběhu hospitalizace, v morbiditě a mortalitě u nemocných s NPB závislých na návykových látkách a uvést vlastní zkušenosti u skupiny těchto nemocných.
Metoda:
Do našeho souboru jsme retrospektivně zařadili nemocné z let 2013–2018 hospitalizované pro neúrazovou NPB, u nichž byla uvedena anamnestická informace o abúzu drog. Z dokumentace byla získána demografická data, typ zneužívané drogy, pracovní diagnóza před příjmem, nálezy paraklinických vyšetření, shoda pracovní a definitivní diagnózy, nutnost operačního řešení a typ chirurgického výkonu. Byla sledována morbidita, mortalita a délka hospitalizace. Získané údaje jsme vyhodnotili metodami popisné statistiky.
Výsledky:
Zadaná kritéria splnilo 8 pacientů (4,7 promile ze všech hospitalizovaných nemocných pro NPB). Všichni pacienti v souboru byli muži s mediánem věku 32 let. Nejčastěji zneužívanou látkou (v 50 %) byl pervitin, dále se jednalo o heroin, benzodiazepiny, tetrahydrokanabinol, subutex, kokain, hypnotika a tramadol. Nejčastější diagnózou v souboru (v 50 %) byla perforace peptického vředu, dále ve dvou případech krvácení do horní části trávicí trubice, v jednom případě relaps Crohnovy choroby s peritonitidou a kolitida vzestupného tračníku. Operační řešení bylo nutné u 75 % nemocných. Třicetidenní mortalita byla nulová, časná komplikace se objevila u jednoho operovaného (dehiscence laparotomie). Průměrná délka hospitalizace byla 9,7 dne, její medián činil 7 dní.
Závěr:
Drogově závislí se podílí na skupině pacientů s NPB marginálně. Jedná se o skupinu signifikantně mladší, s výraznou převahou mužské populace a s preferencí perforace peptické léze.
Klíčová slova:
náhlá příhoda břišní, perforace peptického vředu žaludku a duodena, drogová závislost
INTRODUCTION
Acute abdomen is defined as an abdominal disease characterized by a sudden onset and rapid development, often requiring urgent surgical treatment to save the patient’s life. The most common symptoms include abdominal pain, vomiting and blocked bowel passage [1].
The purpose of our study is to describe the relationship between acute abdomen and drug abuse (not quite well documented in available literature), including the differences in clinical presentation, in the course of hospitalization and in morbidity and mortality, and also to share our own experience with acute abdomen in drug abusers.
METHOD
Patients hospitalized at the Department of Surgery of the 2nd Faculty of Medicine and The Military University Hospital Prague between 2013 and 2018, with the diagnosis of acute abdomen according to ICD – 10 [2] with the exception of traumatic aetiology. The existence of any diagnoses referring to information on drug abuse in the history, with the exception of nicotinism and alcohol abuse, was explored in these patients. The following diagnoses were included: Z 72.2 – Drug use, F1 diagnoses – Mental and behavioural disorders due to psychoactive substance use (with the exception of F10 and F17 diagnoses related to nicotinism and alcohol abuse), R78 – Findings of drugs and other substances, not normally found in blood, and Z86.4 – Personal history of psychoactive substance abuse. The selected medical records were used to obtain information about patient age and sex, type of the abused drug, the first diagnosis when assessing the patient before admission to the Department of Surgery, laboratory assessments, findings of imaging examinations, concordance between the first and final diagnosis, need of surgical treatment and type of the surgery. Additionally, we studied patient morbidity, mortality and the length of hospital stay. The obtained data was processed using the methods of descriptive statistics.
RESULTS
Among all 1690 patients hospitalized at the Department of Surgery of the 2nd Faculty of Medicine and The Military University Hospital Prague between 2013 and 2018 for acute abdomen, only 8 patients satisfied the inclusion criteria. They included patients hospitalized for non-traumatic acute abdomen, with the history of hard drug abuse. All the selected patients were men aged 29–71 years, with the mean age 36.4 years and median age 32 years. The representation of individual drugs reported to be abused by the patients is shown in Tab. 1. Two patients reported abuse of only one drug – pervitin. This type of drug was reported by one half of patients. The other most common drugs included heroin in 3 cases, and benzodiazepines, THC (tetrahydrocannabinol) and subutex in 2 cases. Cocaine, hypnotics and tramadol occurred in 1 case each.
Tab. 1. Zastoupení konkrétních drog v souboru pacientů
Tab. 1: Specific drug representation in patients with acute abdomen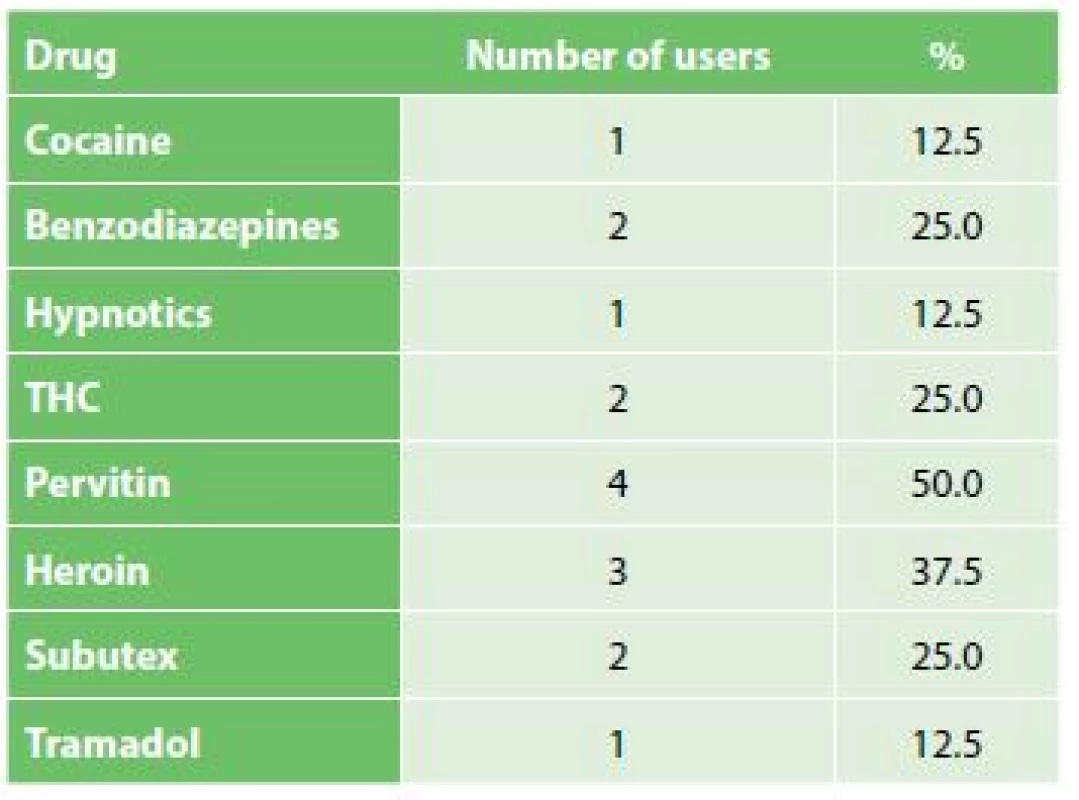
Perforated peptic ulcer was the most common diagnosis in our set. One half of the patients were hospitalized for this diagnosis. Two cases concerned bleeding in the upper gastrointestinal tract; Crohn’s disease relapse with peritonitis and an abscess in the lesser pelvis, and colitis of the ascending colon mimicking acute appendicitis were present in one case each.
Little concordance between the first and final diagnosis was an interesting finding. The concordance was found only in one half of the cases. The first diagnosis of one patient was duodenal ulcer perforation (particularly based on the CT finding) but a lesion at the gastric outlet was found instead in the perioperative period. Severe colitis in the caecum and ascending colon with starting necrosis in the caecum was found in another patient admitted for abdominal pain in the lower right abdomen with clinically suspected acute appendicitis. Bleeding aetiology of one patient admitted with haemorrhagic shock was not determined at admission; gastrofibroscopy with the finding of a Forrest IIa lesion in the duodenal bulb was done only when the patient’s condition had stabilized. However, the disagreement between the first and final diagnosis in the above mentioned patients had no impact on subsequent therapy. In one patient examined for abdominal pain in the epigastrium, the condition was not initially assessed as gastrointestinal perforation; however, the patient’s condition worsened in the course of two hours and subsequent clinical and paraclinical assessments did indicate the diagnosis of perforated peptic ulcer – see Tab. 2.
Tab. 2. Zastoupení příčin NPB v naší sestavě
Tab. 2: Acute abdomen causes in our set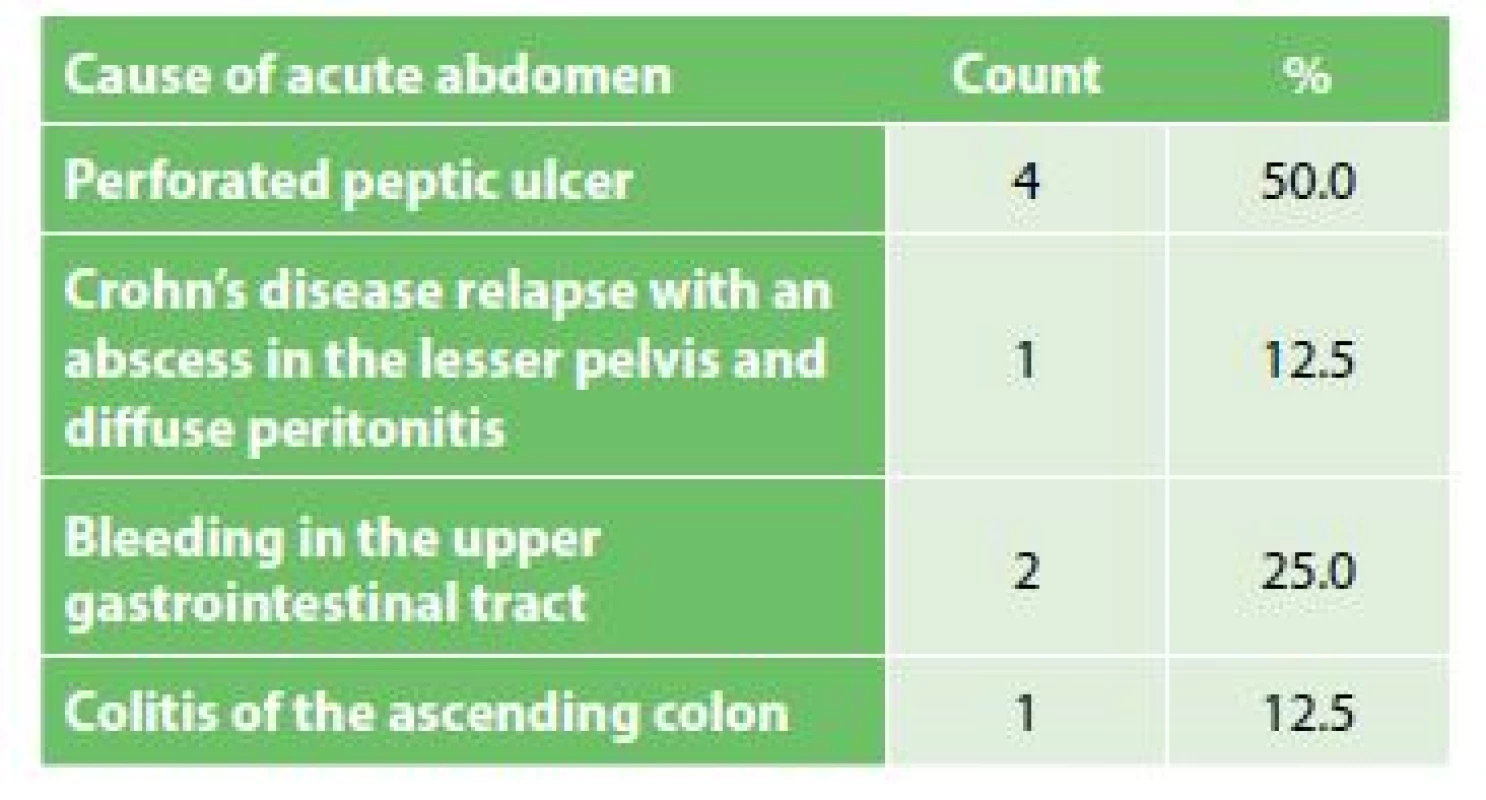
Acute surgery was needed in 75% patients; endoscopic treatment was used in one quarter of the cases (bleeding in the upper gastrointestinal tract).
Considering the above described diagnoses for which the patients were hospitalized, the most common surgeries done in the set of our patients included abdominal revision surgery, suture of a perforated ulcer with omentoplasty and abdominal drainage. This surgery was done in four cases and was laparoscopic in one of these cases. Subtotal colectomy with terminal ileostomy was completed in the patient with Crohn’s disease relapse. Ileocolic resection with primary ileo-ascending colon anastomosis was done in the patient with suspected acute appendicitis with the perioperative finding of typhlitis and starting necrosis of the caecum.
There was zero 30-day mortality in our set, and complications occurring in the early postoperative period were observed in one patient. Laparotomy dehiscence occurred in the patient undergoing ileocolic resection on postoperative day 6. The condition was managed by resuture, securing the wound using the Ventrofil® system. Hepatorenal failure developed in the patient admitted for haemorrhagic shock of unclear aetiology. This condition fully resolved during the hospitalization period.
The length of hospital stay of our patient set ranged from 4 to 21 days, with the mean of 9.1 days and median of 7 days.
DISCUSSION
Acute abdomen events in drug abusers are not documented in detail in the literature. Most publications are conceived as case reports [3−7]. Original studies occur only rarely in the literature, and only for small patient sets [8]. There are no multicentre studies with prospective enrolment of subjects.
Epidemiology
Acute abdomen incidence has been reported as 11–13 patients/1000 inhabitants/year in the Czech Republic (CR); in accordance with our observations, drug abusers with acute abdomen represent a negligible group in the CR [9]. The incidence of acute abdomen as an entire group of diseases is not well documented in Europe and worldwide. This may be due to not quite identical understanding of “acute abdominal pain” and “acute abdomen” [10]. Individual diagnoses are often assessed separately in the international literature; the incidence of acute appendicitis as the most common acute abdomen has been reported as 1 to 1.5 patients/1000 inhabitants/year [11]. The incidence of acute appendicitis in the national literature does not differ [9]. In accordance with the literature, young men aged 32 years predominate in our patient set of drug abusers [8], while in the population with no drug abuse, the median age of patients with perforated peptic ulcer is higher – 55 years [12,13]. The total number of patients enrolled in our set is affected by the relatively older population of Prague 6 compared to other municipal districts [14]. Therefore our study cannot be considered as cross-sectional or representative, although we did choose drug abusers with acute abdomen for the relatively long period of 5.5 years.
The most commonly represented drugs in our set included pervitin and heroin. This distribution corresponds to the nationwide situation in the CR: in 2015, pervitin was the most common hard drug (34 thousand users), and it was followed by heroin with 4.5 thousand users [15].
Causes of acute abdomen in drug abusers
The diagnosis of perforated peptic ulcer was most common in our set of drug abusers, which is at variance with the normal population on the nationwide as well as worldwide scale. Acute appendicitis is the predominant acute abdomen in the normal European population with the incidence of 105–151 patients/100,000 inhabitants/year [9,11,16], while the incidence of perforated peptic ulcer is 3.8 to 14 patients/100,000 inhabitants/year in the normal population [17].
Diagnostic process and treatment of acute abdomen in drug abusers
After clinical examination at emergency departments, patients with suspected acute abdomen undergo standard paraclinical assessments, i.e. blood collections and subsequent imaging examination(s). Abdominal ultrasonography and native abdominal x-ray imaging are essential for the diagnosis of acute abdomen. The utilization rate of CT imaging has been rising in the diagnosis of pneumoperitoneum associated with perforation-related acute abdomen – this imaging method was used in 50% patients of our set in accordance with the literature. This is because CT imaging provides very high sensitivity, up to 99% [18]. Other papers emphasize the importance of ultrasonography also for the diagnosis of perforated peptic ulcer [19]. No significant deviations from the usual course of the tracked diseases in patients without drug abuse were found in our set as regards evaluation of the patients’ clinical condition at the time of their first contact at the emergency department and the evaluation of clinical and paraclinical assessment results performed before admission to the Department of Surgery.
Considering the spectrum of the diagnoses, the most common treatments in our set included abdominal surgical revision, and suture of the perforated ulcer with omentoplasty and abdominal drainage. This surgery was done using the classical method in 75% cases and using laparoscopy in 25% cases. Considering the data found in the literature, which demonstrates advantages of laparoscopy compared to laparotomy [9,12,20], laparoscopy should be preferred to a higher extent in our treatment procedure of perforation-related acute abdomen events [21].
Early morbidity and mortality in drug abusing patients with acute abdomen
The mortality in our set was low, which is in accordance with the literature [22]. Apparently, morbidity is influenced by the low number of enrolled patients. Compared to data in the literature, it is found near the upper limit of the reported range [17,22]. Among the patients operated for perforated peptic ulcer, thus the most common aetiology of acute abdomen in our set, surgical revision was not needed in any patient. Again, this may be influenced by the low number of the subjects because according to the literature, surgical revision is required approximately in one fifth of the cases [23]. The length of hospital stay of our patients shows no significant difference from data in the literature [12].
Weak points of the study
The small patient set is a limitation of the study. There may be flaws in the documentation, resulting in absence of important history data on hard drug abuse and thus in the enrolment of a smaller number of patients. The covered area and regional occurrence of drug abusers may be other problems with a potential impact on representativeness of our patient set.
Further research should focus on a more detailed comparison of drug user groups and patients with no history of drug abuse, examined and hospitalized for acute abdomen, particularly in a larger patient set in multicentre studies.
CONCLUSION
Based on our own observations, we can note that the share of drug abusers in the group of patients with acute abdomen is quite marginal – 4.7 pro mille. Unlike patients with acute abdomen but without any drug abuse, our patients were significantly younger, exclusively male, and exhibited the preference of perforated peptic lesion. The clinical findings do not differ. Our results are in accordance with data in international literature, where case reports are at the centre of attention, in particular.
Supported by MO 1012.
Conflict of interest
The authors declare that there is no conflict of interest regarding the publication of this article and that this article has not been published in any other journal.
MUDr. Luděk Hána
Surgical Clinic of 2nd Faculty of Medicine of the Charles University
and the Military University Hospital Prague
U Vojenské nemocnice 1200
169 02 Praha 6
e-mail: ludek.hana@seznam.cz
Zdroje
-
Ferko A, Šubrt Z, Dědek T. Chirurgie v kostce, Praha, Grada Publishing 2015.
-
Mezinárodní statistická klasifikace nemocí a přidružených zdravotních problémů: MKN-10: desátá revize. Praha, Bonton Agency 2008.
-
Brown CD, Maxwell F, French P, et al. Stercoral perforation of the colon in a heroin addict. BMJ Case Rep 2017.
-
Yahchouchy E, Debet A, Fingerhut A. Crack cocaine-related prepyloric perforation treated laparoscopically. Surg Endosc 2002;16 : 220.
-
Aspirin/paracetamol/caffeine abuse: Duo-denal ulcer and its complications: 3 case reports. Reactions weekly 2018;1693 : 68.
-
Ippolito SF, Spitz WU. Gastrointestinal hemorrhage from an internal jugular abscess in an intravenous drug addict. Am J Forensic Med Pathol 1990;11 : 158−9.
-
Albu E, Parikh V, Abugaida AM, et al. Delayed splenic rupture in a drug addict. Ann Emerg Med 1993;22 : 861−2.
-
Kahrom M, Kahrom H. Perforation of peptic ulcer following abrupt cessation of long-term opiate use. Surg Today 2010;40 : 836−9.
-
Hájek M, Charvátová E, Křepelka P, et al. Náhlé příhody břišní. Praha, Centrum doporučených postupů pro praktické lékaře 2011.
-
Cervellin G, Mora R, Ticinesi A, et al. Epidemiology and outcomes of acute abdominal pain in a large urban Emergency Department: retrospective analysis of 5,340 cases. Ann Transl Med 2016;4 : 36.
-
Ferris M, Quan S, Kaplan BS, et al. The global incidence of appendicitis: A systematic review of population-based studies. Ann Surg 2017;266 : 237−41.
-
Agaba EA, Klair T, Ikedilo O, et al. A 10-year review of surgical management of complicated peptic ulcer disease from a single center: Is laparoscopic approach the future? Surg Laparosc Endosc Percutan Tech 2016;26 : 385−90.
-
Feliciano DV, Ojukwu JC, Rozycki GS, et al. The epidemic of cocaine-related juxtapyloric perforations: with a comment of testing for Helicobacter pylori. Ann Surg 1999;229 : 801−4.
-
Věkové složení obyvatelstva hl. m. Prahy v roce 2011 [on line]. Český statistický úřad 2012. Available fom: https://www.czso.cz/documents/10180/20567029/104003_12.pdf/b4d8a4ce-e779-4a2f-afb7-50d24ae4ce0b.
-
Výroční zpráva o drogách: Češi ve velkém konzumují alkohol a tabák, počet uživatelů nelegálních drog klesá [on line]. Vláda České republiky, 2016. Available from: https://www.vlada.cz/cz/ppov/protidrogova-politika/media/vyrocni-zprava-o-drogach-cesi-ve-velkem-konzumuji-alkohol-a-tabak--pocet-uzivatelu-nelegalnich-drog-klesa--151149/.
-
Menclová K, Traboulsi E, Nikov A, et al. Treatment of acute appendicitis: Retrospective analysis. Rozhl Chir 2016;95 : 317−21.
-
Søreide K, Thorsen K, Søreide JA. Strategies to improve the outcome of emergency surgery for perforated peptic ulcer. Br J Surg 2014;101:e51−64.
-
Thorsen K, Glomsaker TB, von Meer A, et al. Trends in diagnosis and surgical management of patients with perforated peptic ulcer. J Gastrointest Surg 2011;15 : 1329−35.
-
Kuzmich S, Harvey CJ, Fascia DT, et al. Perforated pyloroduodenal peptic ulcer and sonography. AJR Am J Roentgenol 2012;199:W587−94.
-
Vărcuş F, Beuran M, Lica I, et al. Laparoscopic repair for perforated peptic ulcer: A retrospective study. World J Surg 2017;41 : 948−953.
-
Kim MG. Laparoscopic surgery for perforated duodenal ulcer disease: Analysis of 70 consecutive cases from a single surgeon. Surg Laparosc Endosc Percutan Tech 2015;25 : 331−6.
-
Yang YJ, Bang CS, Shin SP, et al. Clinical characteristics of peptic ulcer perforation in Korea. World J Gastroenterol 2017;23 : 2566−74.
-
Wilhelmsen M, Møller MH, Rosenstock S. Surgical complications after open and laparoscopic surgery for perforated peptic ulcer in a nationwide cohort. Br J Surg 2015;102 : 382−7.
Štítky
Chirurgia všeobecná Ortopédia Urgentná medicína
Článek Náhlé příhody břišníČlánek Kolorektální robotický kurz
Článok vyšiel v časopiseRozhledy v chirurgii
Najčítanejšie tento týždeň
2019 Číslo 1- Metamizol jako analgetikum první volby: kdy, pro koho, jak a proč?
- Kombinace metamizol/paracetamol v léčbě pooperační bolesti u zákroků v rámci jednodenní chirurgie
- Antidepresivní efekt kombinovaného analgetika tramadolu s paracetamolem
-
Všetky články tohto čísla
- Timing ERCP u akutní biliární pankreatitidy
- Náhlé příhody břišní u drogově závislých
- Současná léčba difuzních peritonitid – je kvadrantová laváž stále aktuální?
- Spontánní retroperitoneální hematom – naše zkušenosti s aktivním chirurgickým přístupem
- Mezenteriální divertikly tenkého střeva jako příčina náhlé příhody břišní
- Náhlé příhody břišní
- Náhlé příhody břišní u pacientů s Crohnovou chorobou − kazuistiky
- Kolorektální robotický kurz
- Obstrukce tlustého střeva nádorem – co je prioritou léčby?
- Cena profesora Hájka za nejlepší články roku 2018
- Rozhledy v chirurgii
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Spontánní retroperitoneální hematom – naše zkušenosti s aktivním chirurgickým přístupem
- Mezenteriální divertikly tenkého střeva jako příčina náhlé příhody břišní
- Timing ERCP u akutní biliární pankreatitidy
- Současná léčba difuzních peritonitid – je kvadrantová laváž stále aktuální?
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



