Fractional CO2 laser therapy of hypertrophic scars – evaluation of efficacy and treatment protocol optimization
Authors:
Klosová H. 1; Zálešák B. 1; Xinopulos P. 1; Langová K. 2
Authors‘ workplace:
Department of Plastic and Esthetic Surgery, University Hospital Olomouc, Czech Republic
1; Department of Medical Biophysics, Faculty of Medicine and Dentistry, Palacky University Olomouc, Czech Republic
2
Published in:
ACTA CHIRURGIAE PLASTICAE, 63, 4, 2021, pp. 171-180
doi:
https://doi.org/10.48095/ccachp2021171
Introduction
Hypertrophic scars are defined as scars above the level of healthy surrounding tissue. They are an undesirable consequence of injury or surgery with prolonged healing. They can be linear, extensive or widespreading, causing various mental and physical difficulties to patients.
Extensive hypertrophic scars most often occur in the areas after dermoepidermal autotransplatation due to a burn injury. The prevalence of scar hypertrophy reported in the literature ranges from 30 to 70%. In fact, the prevalence is purely documented and remains unknown [2,3]. Significant interindividual variability in the onset of scar hypertrophy is based on many factors [4].
The predisposing factors are: childhood and younger age, prolonged healing, infection, widespread deep destruction of the dermis during burns or extensive decollement, dermoepidermal autotransplantation and meshed grafts, genetic factors, increased hormonal activity during adolescence, somatization of fears and untreated mental tension in injuries, especially in hypersensitive and anxious individuals [5,6]. The scars after autotransplantation of meshed grafts present a specific problem. The regular geometric appearance is striking and esthetically disturbing.
Successful treatment must be complex with active patient’s cooperation. An integral part of modern treatment of hypertrophic scars is laser therapy. Its effectiveness has been proven in numerous clinical studies [7–9].
In principle, the treatment of hypertrophic scars is divided into the treatment of immature scars and the treatment of mature scars. Pulsed-Dye Lasers (PDLs), CO2 laser, Erb: YAG laser and Q-switched Nd: YAG lasers are most frequenly used in the treatment. Vascular laser treatment causes selective photothermolysis of small vessels, so it is especially suitable for the treatment of immature scars [10].
Ablation fractional CO2 and Erb-YAG lasers are suitable for the treatment of mature scars, which significantly reduce the height and hypertonus of both mature and immature scars by evaporating scar tissue [10]. Fractional lasers act non-selectively in the epidermis and dermis and lead to the formation of microscopic cylindrical zones of thermal destruction (microscopic thermal damage zones, MTZs) [11–13]. Lateral thermal destruction zones are immediately adjacent to the cylindrical zones of thermal destruction as thermal damage to the immediate vicinity of the borehole. Among the vaporized canals is preserved tiny net of healthy, laser-untouched tissue, from which regeneration and epithelialization occurs. Subsequent retraction of the zone of thermal damage is responsible for volumetric reduction of the scar. Repeated fractional laser therapy reduce gradually the thickness of the scar [14]. Ideally, the relief is smoothed into healthy surrounding.
The scars after 12–18 months are generally considered to be matured [15–18].
They are usually stable and are not a subject to further changes. Stability is a basic requirement for quantifying the effect of laser therapy both clinically and with objective methods to eliminate the changes caused by spontaneous regression. Generally, hypertrophic scars have a tendency to spontaneous regression which vary individualy between few and several months. Thus, in unstable scars, the effectiveness of laser therapy is always combined with the changes that accompany spontaneous scar regression over time. These changes show significant individual variability and therefore the effectiveness of laser therapy in immature scars cannot be precisely estimated [19].
To evaluate the effectiveness of laser therapy in everyday medical practice, clinical evaluation and specifically designed evaluation tools and scoring scales, such as Vancouver Scar Scale (VSS), Patient and Observer Scar Assessment Scale (POSAS), Visual Analog Scale (VAS), and Manchester Scar Scale (MSS) are most frequently used with VSS being the most commonly used and generally accepted rating scale for scar hypertrophy [20]. Although clinical evaluation of scars using the above scales is always subjective [21], it is a practical and affordable tool with satisfactory informative value. The limiting factor is that none of the above scales was designed directly to evaluate the response of scars to laser therapy, so it fails to capture the spectrum of changes in its complexity.
For this reason, it is necessary to create new evaluation protocols that can more accurately capture the changes in scars and evaluate the effects of laser therapy. The creation of such an evaluation tool was a secondary goal of our study focused on the optimization of the treatment protocol of fractional CO2 laser therapy (fr-CO2-LT).
The primary goal of the project was to optimize fr-CO2-LT parameters that will lead to the smoothing of prominent areas of the scar to the level of healthy surrounding skin and a significant reduction of scar hypertonus with a minimum number of laser therapy sessions possible.
Methods
Patients with hypertrophic scars who required more than one fr-CO2-LT session to achieve significant improvement were included in the study. These scars, with their texture, appearance, height, color, pigmentation and pliability, differed significantly from the surrounding healthy tissue. Stiff, contracting scars and scars limiting the range of motion in the joints were evaluated as functionally deficient. Contracting scars accounted for 44% of the intervention group, and mobility-limiting scars accounted for 28% of the group (Tab. 1).
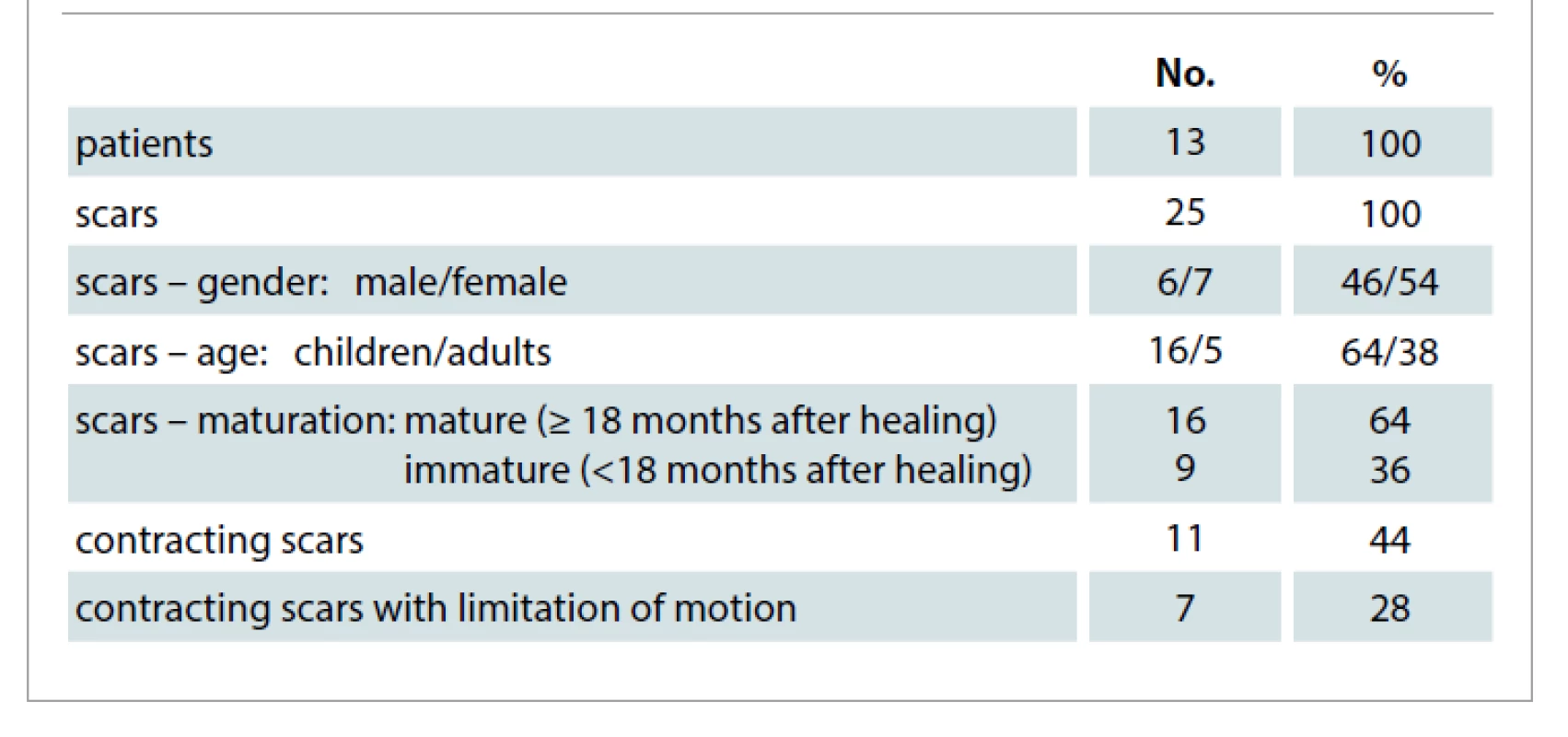
There were 25 hypertrophic scars in 13 patients (6 men and 7 women). Eight children were indicated for fr-CO2-LT (Tab. 1). The vast majority of scars occurred after healing of deep burn; one of the patients developed scar hypertrophy after the excision of a giant nevocellular naevus followed by cutaneous dermoepidermal autotransplantation.
The treatment of fr-CO2-LT scars was performed in all patients under topical anesthesia by applying lidocaine 5% gel (Lidocaine 5% gel, magistraliter according to the Czech Pharmacopoeia, Olomouc University Hospital) under an occlusion of 1–1.5 hours prior to the procedure. In patients (23%) who experienced pain of VAS 3–4 intensity, the analgesia was supplemented by local cooling with gel pads (Mediflex Duo, Medicalflox, Czech Republic). In one case, treatment under general anaesthesia was required. The interval between the first and second fr-CO2-LT (L1–L2) was in agreement with a median of 11 weeks.
Fractional CO2 laser therapy was performed with a Microsys 40W high powerCO2 laser (Daeshin Enterprise (D.S.E), 0476 ISO 13485) using a pulse fractional mode with a fraction scanner. This mode generates short, high-energy pulses suitable for tissue vaporization.
The CO2 laser operates at the wavelength λ = 10 600 nm. It is a vaporization laser, its target chromophore is water and the radiation is non-selectively absorbed by tissue fluid [22]. Reduction in the mass of the scar tissue is achieved by vaporization.
The following parameters can be optionally set for fractional CO2 laser therapy with the Microsys 40W device:
• fluence: laser output energy per dot of the scanned area, 5–300 mJ / 1 point;
• repeat time: the length of delay (repeat interval) between laser pulses, 0.5–2.5 s or SINGLE = OFF;
• density level: the density of points in the scanned area per cm2, 1–23;
• depth level: laser depth, level 1–5;
• scan area: scan size, from 2 x 2 mm to max 20 x 20 mm, max 4,489 fraction points (dots)
• scan shape: square, hexagon, triangle, circle;
• shape rendering: line – ARRAY, diagonal – GRID, random – RANDOM.
The treatment strategy and parameters of fractional CO2 laser therapy – fluence, density level, depth – were set according to the current clinical findings and the intended power of treatment in order to reduce scar height, release hypertonic, contracting scars and improve the homogeneity of relief and texture of scars. Medical photography was obtained for all patients before and after laser therapy, and the parameters of laser therapy were recorded in a special protocol. The areas before and after the treatment were disinfected with Octenisept (Schülke & Mayr, GmbH, Germany); after the treatment, they were covered with Flamigel (Dahlhausen, Czech Republic), greasy tulle (Lomatuell, Lohmann & Rauscher, GmbH, Germany), and mule; thereafter, they were gently fixed with Fixa crep bandage (Batist Medical as, CR).
The scars were clinically evaluated shortly before fr-CO2-LT (rating 1, H1) and, in average, 11 weeks following the first fr-CO2-LT (rating 2, H2), using two assessment tools – Vancouver Scar Scale (VSS) and HTT protocol.
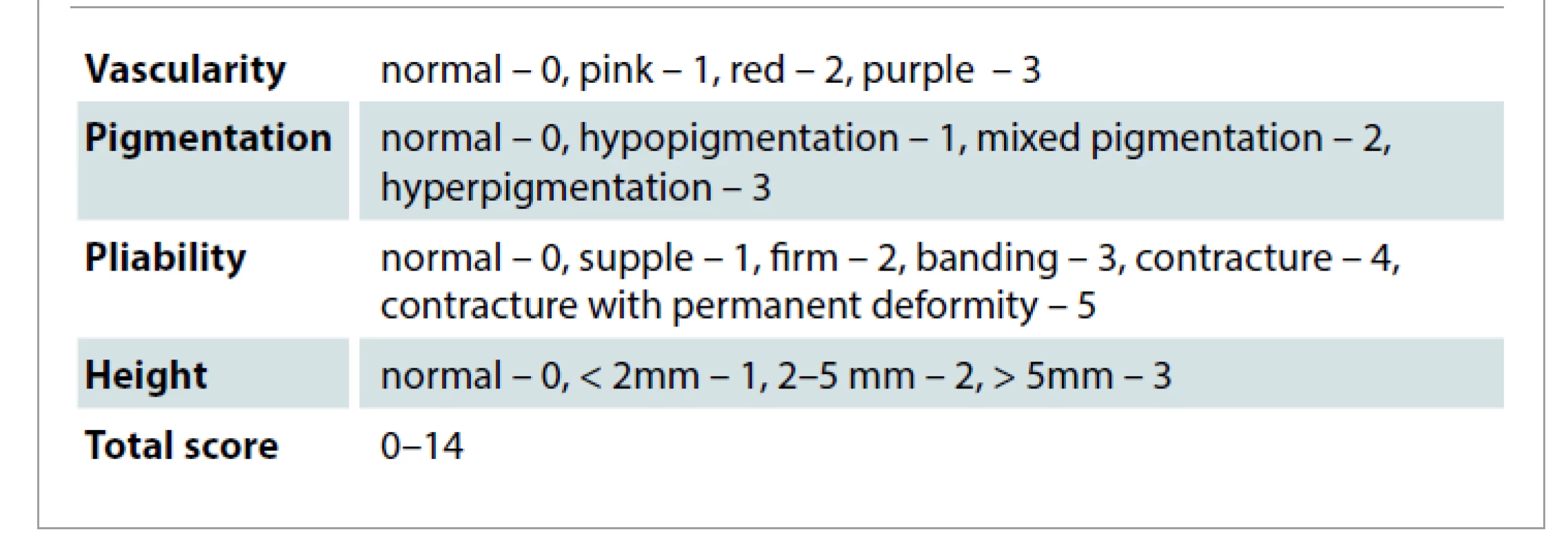
In accordance with the VSS, four scar qualities were monitored clinically, by inspection and palpation: vascularity, pigmentation, pliability, and height. The resulting VSS is the sum of individual scores; its value ranges from 0 to a maximum of 14 points. The zero value corresponds to healthy skin (Tab. 2).
Scar vascularity and pigmentation were assessed visually on a four-point scoring scale (Tab. 2). The vascularity and pigmentation were considered normal if the entire area of the scar with its color or pigmentation corresponded to healthy surrounding tissue. If any part of the scar had other than normal vascularity or pigmentation, an appropriate rating was recorded in the protocol. Flexibility was assessed by palpation, on a six-point scale as normal (0), scar elastic, flexible with minimal resistance (1), scar flexible, flexible under pressure (2), scar firm, inflexible, resistant to hand pressure, immobile (3), scar cords and patchy scars that whiten when the scar is extended (4), scarring contracture or permanent shortening of the scar causing deformity (5). The height of the scar was assessed by inspection and qualified clinical estimate on a four-point scale (Tab. 2). It is typical that the height of the scar is heterogeneous in the majority of extensive hypertrophic scars. The areas within, above or below the level alternate. The most prominent area of the scar was always decisive for the classification of a scar in the relevant VSS subcategory. Qualified height estimation of the most prominent part was made and recorded in the VSS protocol.
VSS is a generally accepted and most frequently used scar rating scale in studies [19]. Clinical practice of laser therapy shows that VSS is not a sufficiently sensitive and esthetically sensitive tool for the purposes of evaluating the effects of laser therapy, because some of the changing qualities of the scars occurring after laser therapy are not part of the evaluation protocol. Therefore, VSS is a less specific tool for the evaluation of the effectiveness of laser therapy. In order to describe a spectrum of changes in scars after laser therapy, the researchers designed their own evaluation protocol, the so-called HTT protocol. The name of the protocol was derived from the names of evaluated parameters (Tab. 3).
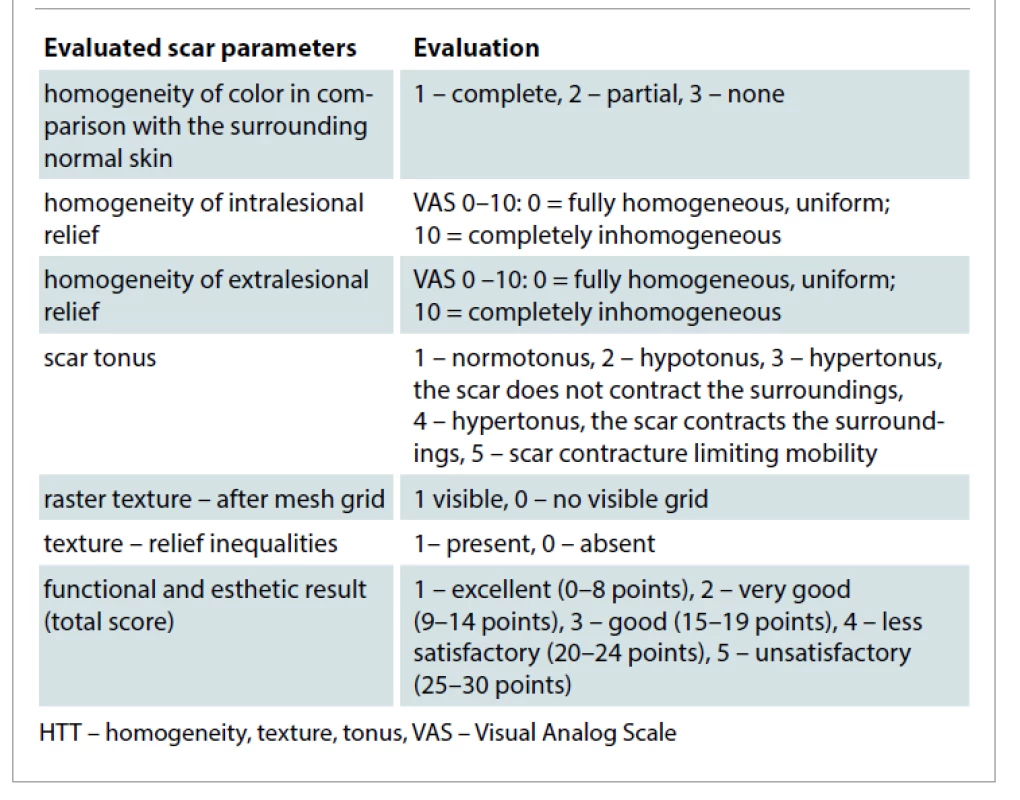
The following parameters were evaluated for each of the treated scars:
• homogeneity of the color (H-C) of the scar in comparison with the surrounding normal skin;
• homogeneity of intralesional relief
(H-IL) within the scar area;
• homogeneity of extralesional relief (H-EL) in comparison with healthy surrounding skin;
• scar tonus – scar tension in comparison with healthy surrounding skin;
• raster texture – raster visibility across the mesh;
• texture – the presence pf textural irregularities.
The overall functional and esthetic result is the sum of the scores of the individual evaluated parameters.
After-mesh raster and relief inequalities were rated on a dichotomous scale. Other monitored qualities include ordinal quantities; they were evaluated using scoring scales. The homogeneity of the color with surrounding normal skin was evaluated on a three-point scale and the tone of the scar in comparison with healthy surrounding skin was evaluated on a five-point scale (Tab. 3).
Intralesional homogeneity of relief (H-IL) and homogeneity of relief with surrounding healthy skin (H-EL) were evaluated using VAS in the range 0–10 (Tab. 3). Intralesional homogeneity assessed the extent to which the surface of the scar is uniform in its various parts. According to the VAS, the homogeneity of the relief to the surroundings assessed the extent to which the appearance of the scar surface was in accordance with surrounding healthy skin.
The characteristics of the scars were recorded in the H1 and H2 clinical trials by a physician performing laser therapy in both the VSS and HTT protocols. Visually evaluable scar qualities (color, pigmentation, intralesional homogeneity of relief, homogeneity of relief to surroundings, raster after mesh and area of scar hypertrophy within the area of intervened scar) were evaluated by visual analysis of medical photography by an independent evaluator, experienced plastic surgeon not performing fr-CO2-LT intervening scars. The numerical data recorded in the H1 and H2 clinical trials were subjected to statistical analysis using IBM SPSS Statistics for Windows statistical software, Version 23.0. Armonk, NY: IBM Corp. Quantitative data were presented using median, minimum and maximum values, means, and standard deviations (SD). Qualitative data were evaluated using absolute and relative frequencies. It was verified by Shapiro-Wilk normality tests that quantitative quantities do not have a normal distribution. The McNemar test was used to determine the differences between the dependent selections in qualitative dichotomous quantities, and the non-parametric serial Wilcoxon test was used for ordinal quantities. The correlation of quantitative and ordinal quantities was verified using Spearman's correlation coefficient. The differences between the two independent selections were verified using the Mann-Whitney U-test. All tests were performed at the level of statistical significance α = 0.05. The results with P-values < 0.05 were considered statistically significant.
Results
Source data from VSS and HTT protocols were subjected to statistical analysis. There was a statistically significant improvement in the height of scars, a decrease in their hypertonus and an improvement in the overall functional and esthetic outcome between H1 and H2, P < 0.05 (Tab. 4, 5).
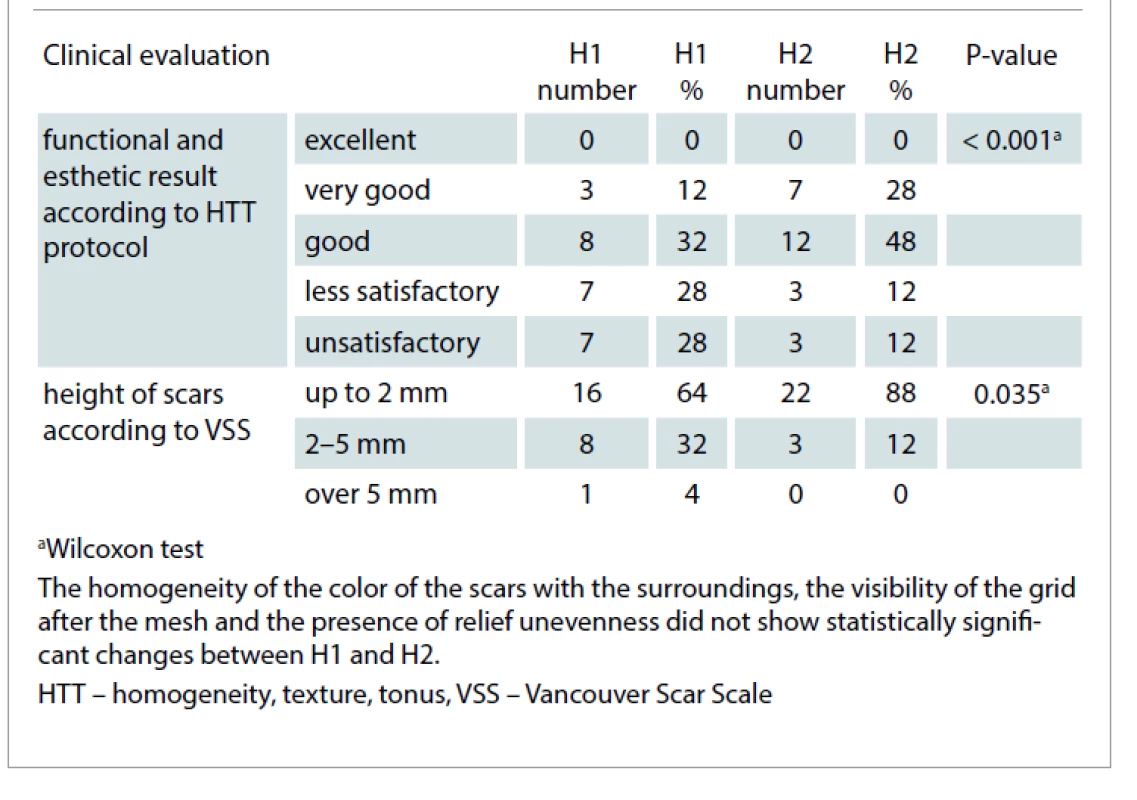
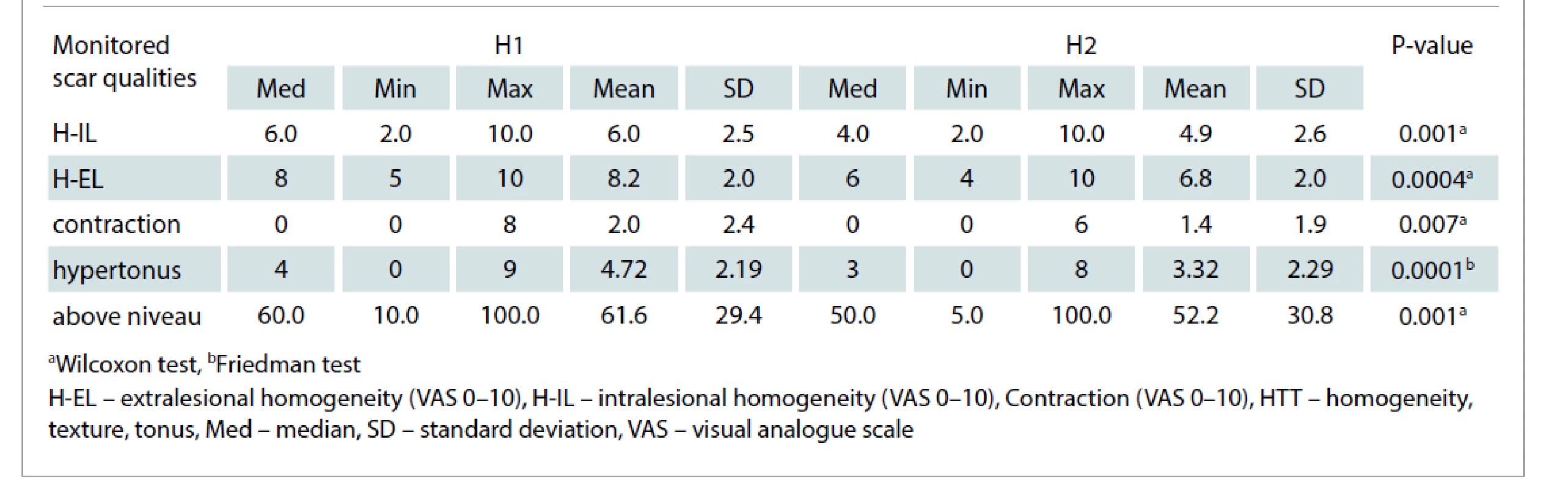
The reduction in scar height achieved after the first laser therapy in 24% of treated scars was statistically significant (Tab. 4). The median hypertonus assessed by VAS decreased between H1 and H2 from 4 to 3; this decrease was statistically significant. Functional and esthetic outcome (FEV) showed a statistically significant improvement – a decrease in the categories of less satisfactory and unsatisfactory and an increase in the categories of good and very good FEV; P = 0.001 (Tab. 4). The greatest contribution was made by the improvement of the homogeneity of the intralesional texture and the improvement of the homogeneity of the relief of the scar towards healthy surroundings (Graph 1, Fig. 1, 2). For other parameters (vascularity, pigmentation, pliability, total VSS) no statistically significant changes between H1 and H2 were demonstrated, P > 0.05.



The homogeneity of the color of scars with the surroundings, the visibility of the grid after the mesh and the presence of relief unevenness did not show statistically significant changes between H1 and H2.
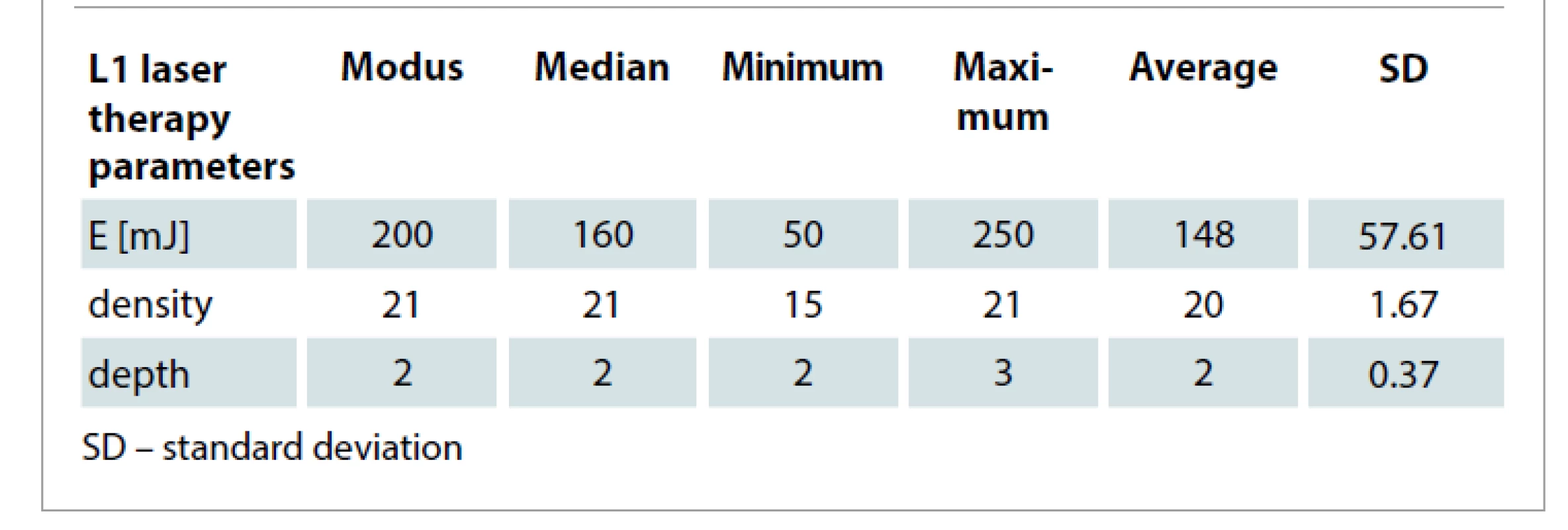
The key parameters of the fr-CO2-LT treatment were recorded in the protocol and subsequently subjected to descriptive statistical analysis (Tab. 6). Scars with fr-CO2-LT were most often treated with the energy 200 mJ, density 21, and depth 2.
The scar changes evident in the H1 and H2 clinical trials were subjected to the correlation analysis in relation to fr-CO2-LT parameters. The correlation analysis revealed a statistically significant positive correlation between the energy of the laser beam and the change in the extent of the areas elevated above the level of healthy surroundings. Areas treated with higher energy showed a greater area reduction in height. Furthermore, a statistically significant negative correlation was detected between the density of fractional points (density of points in the scanned area per cm2) and the change in contraction. In scars treated with a lower density of fractional points per cm2 of treated scar area, less tissue contraction or less tendency to shrink the scar was clinically evident (Tab. 7).
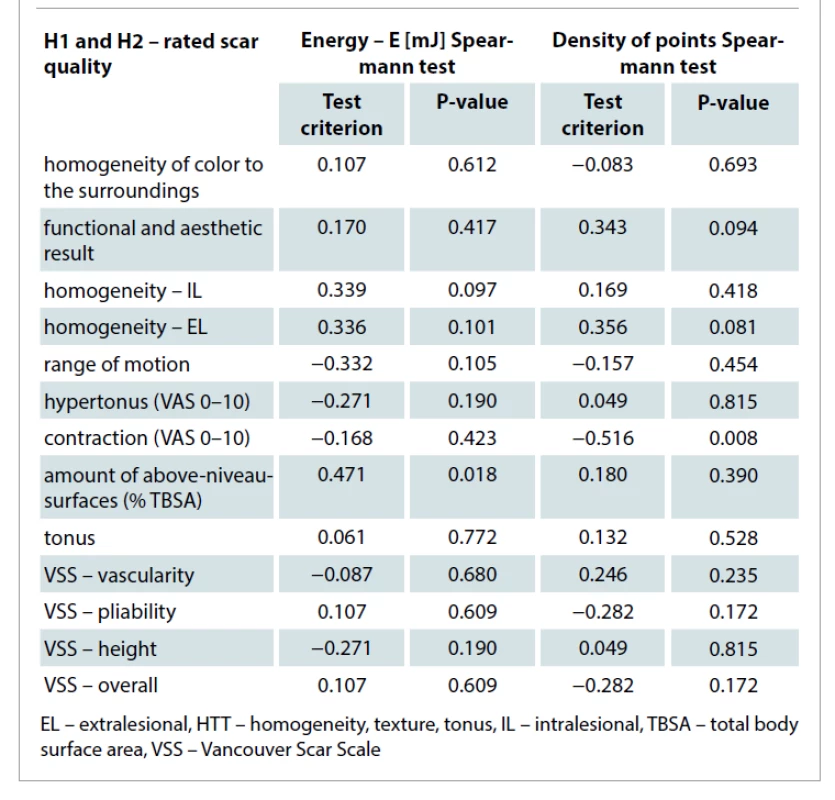
We consider the results of the correlation analysis to be the fundamental outcomes of our work.
Discussion
The efficiency of fr-CO2-LT is given by a combination of the setting of optional parameters of the fractional CO2 laser. We select the parameters based on clinical experience and published data, according to the current clinical findings and the intended severity of treatment, which is given by the level of laser output energy (fluence) in combination with setting the density of points in the scanned area (density level) and laser depth (depth level). The power of fr-CO2-LT
must be well tolerated by the patient, especially the pain during the treatment must not exceed VAS 2. The experience of the physician performing laser therapy and feedback based on long-term systematic continuous analysis of laser therapy results in relation to treatment parameters are very important for setting appropriate treatment parameters. To achieve a good effect, laser therapy must be sufficient, but not excessively aggressive. Excessive aggressive laser therapy alters normal healing, causing unwanted scarring and recurrence of scar hypertrophy [10]. If we choose a high laser output energy (> 200 mJ) for laser therapy, it is necessary to adequately reduce the density of points of the treated area to minimize the risk of complicated healing and subsequent unwanted scarring [10].
In CO2 ablation laser therapy, a beam emerges from the laser and impinges on the skin surface. The beam is solid, unsplit, and the tissue is evaporated throughout the area, without leaving the islands of healthy tissue untouched by the laser. Full-format ablation is associated with the risk of deep thermal destruction of the dermis, resulting in prolonged healing and the occurrence of side effects – permanent dystrophy, infection and scar hypertrophy [23]. Due to the high degree of complications, widespread ablation treatment has not found routine application in clinical practice.
Fractional laser therapy, introduced into clinical practice in 2004 [11], works on the principle of splitting the laser beam into many micro-beams, which cause limited thermal microtrauma at the point of impact with the formation of so-called microscopic thermal zones (MTZ), among which there is a net of healthy tissue [8]. Depending on the set value of the energy, MTZ laser pulses with a diameter of < 400 μm penetrate to different depths of the skin, with the maximum up 1,300 μm. The essence of the effectiveness of fractional ablation laser therapy is the application of a laser beam with high energy and short duration of action.
The introduction of fractional lasers into clinical practice has significantly increased the safety of esthetic and therapeutic applications of these lasers. There is a general agreement that the effect of the therapy depends on the energy used, the treatment density and its depth [8].
There is no consensus on what the specific settings should be for each clinical application [24]. Literature data regarding laser therapy parameters vary considerably from author to author, depending on the type of the laser device used and the scars treated. Therefore, the evaluation, optimization and comparison of the effectiveness of laser therapy in individual studies and for individual types of lasers is problematic. One of the clues for optimizing treatment effectiveness and reaching general consensus could be the works by Bowen [25] and Levi et al [26], where a significant improvement in hypertrophic scars was achieved by adjusting the laser energy to values that led to spot bleeding from at least 50% of the fractional channels. Many authors recommend higher laser energy settings to achieve the best effects [10,27]. At the same time, at higher laser energies, some recommend reducing the treatment density to minimize the risk of complicated healing and unwanted scarring [10]. These general recommendations are in full agreement with our clinical experience.
There is no study that would accurately and objectively compare different specific laser settings and their results. If we compare our clinical experience with the fractional CO2 and Erb:YAG lasers, we find approximately the same effectiveness of both of them in esthetic indications, where the treatment is performed more gently than in the treatment of hypertrophic scars. The experience with the treatment of hypertrophic scars based on a comparison of the work with both types of lasers in our clinical practice has clearly shown benefits of the fractional CO2 laser compared to the Erb:YAG laser. The CO2 laser works significantly faster in rapid fractional laser therapy. For the same depth of ablation that the CO2 laser reaches with one pulse, the Erb:YAG fractional laser requires several pulses; the fractional Erb:YAG laser therapy is thus less vigorous in a single pulse and the individual treatment lasts considerably longer. The fractional CO2 laser has better coagulation effects on surrounding tissue, with better potential for spontaneous hemostasis and good patient tolerance. Our experience is in full agreement with published data [10,28]. In favor of the erbium laser, the literature reports a lower risk of side effects, less edema after surgery and shorter healing times [29].
After initial treatment with fr-CO2-LT, changes in vascularity were clinically evident: red, purple and normally colored scars decreased; on the contrary, pink scars were increased. These clinically apparent changes were not detected as statistically significant. Due to the fact that the scars fade over time with a maturation process with very different rates and intensities individually, the evaluation of the changes in vascularity after fr-CO2-LT is clinically unfavorable.
In response to the initial fr-CO2-LT, there were no clinically apparent changes in scar pigmentation in the intervention scars. Pigmentation can be removed by laser on the principle of selective photothermolysis, the target chromophore of which is melanin at the laser wavelengths 630–110 nm and the pulse length < 1 µs [30,31]. Q-switched type lasers predominantly serve to removing unwanted pigmentations, in particular Q-switched Nd:YAG (532 nm), Q-switched ruby (694 nm), Q-switched alexandrite (755 nm) and also intense pulsed light [22]. The wavelength of the CO2 laser we use (λ = 10,600 nm) does not reach the target chromophore melanin and therefore no regression by pigmentation can be expected after fr-CO2-LT. Our results on the sides of pigmentation and its influence are thus fully in line with available literature sources.
The height of the scars was assessed by a qualified clinical estimation. In 24% of the scars initially assessed by a qualified clinical estimation as higher than 2 mm, the height was reduced below 2 mm after the first treatment with fr-CO2-LT. According to the statistical analysis of clinical data, these changes were detected as statistically significant. In routine clinical practice, the possibilities of the objective measurement of changes in the height of scars after laser therapy are limited by the availability of specific equipment. The clinical evaluation of scar height is most often visual; it is a simple qualified estimate before and after the laser therapy. It is certainly partly subjective and biased by the evaluator, but it is fully sufficient for routine medical practice. If the doctor and the patient perceive the changes as an improvement, it can be assumed that the "evaluators" around the patient in his daily life will be perceived similarly. We consider the improvement perceived by the doctor and the patient to be the primary goals of fr-CO2-LT. Conversely, if the improvement were objectively measured after fr-CO2-LT and at the same time no changes were evident in the clinical trial before and after fr-CO2-LT, the changes would be invisible to the naked eye. In our opinion and experience, such laser therapy cannot be considered clinically beneficial.
The fact that as early as after the first treatment, there was a statistically significant reduction in the height of the scars below 2 mm, can be attributed in our group to the fact that the entry height of these scars was most often 2.5–3 mm. The achieved reduction in the height is in accordance with our clinical practice where we routinely reduce the scar by 0.5–1 mm in one treatment. A greater height reduction in a single treatment is not desirable, as it is associated with prolonged healing and the risk of unwanted scarring and recurrence of hypertrophy [32,33].
The pliability, vascularity, pigmentation and height are usually heterogeneous within the surface of hypertrophic scars after burns or dermoepidermal autotransplantation; individual areas of the scars differ in these qualities and have different proportions. After the treatment with fr-CO2-LT, the individual monitored qualities and their relative representation within the scar area change. This fact cannot be affected by VSS, which can be considered a significant limitation when evaluating the response to fr-CO2-LT. Thus, VSS can be considered for the needs of clinical monitoring of the response to laser therapy as a less robust evaluation tool, with suboptimal informative value, rather suitable for dichotomously evaluated characteristics only [34]. Thus, finding new assessment tools that better capture the qualitative and quantitative specters of scar changes after laser therapy is highly desirable. The HTT protocol designed by the authors of the project is a promising evaluation tool from this point of view, but it must be verified by further studies.
The changes evident in the area of the intervened scars are much better recorded by the evaluation, which focuses on the proportional representation of these changes in the area of the scar. An important quality of the scar perceived very sensitively by the patient and his surroundings is its color and color homogeneity within the scar (intralesional) and towards the surroundings (extralesional). It is referred to in English literature as the so-called "patch appearance". Due to the fact that scars gradually fade over time with different interindividual variability even without treatment, improving scar color in the sense of hyperemia regression accelerates spontaneous scar fading and improves the esthetic appearance of the scar that can be expected after further laser application.
In our group, there was a noticeable increase in the color homogeneity of the scars with the respect to the surroundings, given mainly by the improvement in the scars colors that were at the start of the treatment completely inhomogeneous with the surroundings. The statistical analysis found these changes statistically insignificant, but clinically evident and the patients perceived better color harmony of the scars with the surroundings very favorably.
The reduction in hypertonus of intervened scars was also clinically evident and significant, although it was not detected as statistically significant. The clinical significance of hypertonus reduction lies in the release of scar tension, thanks to which we can gradually release incipient or mild scarring contractures [35–37] and reduce the risk of functional consequences without the need for rapid indication of surgical treatment, which is another surgical burden for the patient with all its risks, including recurrence of hypertrophy [14].
Conclusion
Properly performed fractional scar laser therapy is an effective treatment modality for the treatment of functionally insufficient and esthetically unsightly extensive hypertrophic scars. Individual treatment of scars with fractional CO2 laser therapy brings clinically evident and statistically significant improvement – reduction of scar height, decrease of its tension, improvement of homogeneity of scar relief intra - and extra-lesionally and reduction of the area of scar hypertrophy. This initial improvement positively motivates the patient for good cooperation and repetition of laser therapy, which is a necessary prerequisite for achieving an esthetically and functionally satisfactory result. By optimizing the parameters of fr-CO2-LT, it is possible to achieve effective and safe flattening of the scar relief and release of its hypertonus with a minimum number of treatment sessions. To assess the effectiveness of laser therapy, a sufficiently specific and sensitive evaluation tool is necessary, which can more accurately identify the effect of fractional laser therapy. The HTT protocol proposed by the authors shows a very promising potential in this respect. Further studies of its possible use in clinical practice to evaluate the effectiveness of laser therapy are necessary.
Roles of authors: All authors contributed extensively to the work presented in this paper. H.K. performed fractional CO2laser treatment of hypertrophic scars and enrolled changes of the scars in the subsequent course. B.Z. visually analyzed photos before and after fractional CO2 laser treatment and enrolled it. P.X. provide translation and stylistic corrections. All authors contributed equally in discussed the results and implications and commented on the manuscript at all stages.
Authors’ contributions: All authors contributed to the contents and approved the final version of this manuscript.
Disclosure: The authors declare no conflict of interest. All procedures performed in this study involving human participants were in accordance with ethical standards of the institutional and/or national research committee and with the Helsinki declaration and its later amendments or comparable ethical standards.
Acknowledgements: Supported by the Ministry of Health of the Czech Republic – DRO (FNOl, 00098892).
Bohumil Zálešák, M.D., Ph.D.
Department of Plastic and Esthetic Surgery
University Hospital Olomouc
I. P. Pavlova 185/6
779 00 Olomouc
Czech Republic
e-mail: bzalesak@gmail.com
Submitted: 3.6.2021
Accepted: 1.12.2021
Sources
1. Carniol PJ., Hamilton MM.,Carniol ET. Current status of fractional laser resurfacing. JAMA facial plast. surg. 2015,17(5): 360–366.
2. Bombaro KM., Engrav LH., Carrougher GJ., et al. What is the prevalence of hypertrophic scarring following burns? Burns. 2003, 29(4): 299–302.
3. Gangemi EN.,Gregori D.,Berchialla P., et al. Epidemiology and risk factors for pathologic scarring after burn wounds. Arch Facial Plast Surg. 2008, 10(2): 93–102.
4. Finnerty CC., Jeschke MG., Branski LK., et al. Hypertrophic scarring: the greatest unmet challenge after burn injury. Lancet. 2016, 388(10052): 1427–1436.
5. Königová R., Bláha J. Komplexní léčba popáleninového traumatu. Karolinum; 2010.
6. Ogawa R. Keloid and hypertrophic scars are the result of chronic inflammation in the reticular dermis. Int J Mol Sci. 2017, 18(3): 606.
7. Issler-Fisher AC., Fisher OM., Smialkowski AO., et al. Ablative fractional CO2 laser for burn scar reconstruction: an extensive subjective and objective short-term outcome analysis of a prospective treatment cohort. Burns. 2017, 43(3): 573–582.
8. Issler-Fisher AC., Waibel JS., Donelan MB. Laser modulation of hypertrophic scars: technique and practice. Clin Plast Surg. 2017, 44(4): 757–766.
9. Azzam OA., Bassiouny DA., El-Hawary MS., et al. Treatment of hypertrophic scars and keloids by fractional carbon dioxide laser: a clinical, histological, and immunohistochemical study. Lasers Med. Sci. 2016, 31(1): 9–18.
10. Anderson RR., Donelan MB., Hivnor C., et al. Laser treatment of traumatic scars with an emphasis on ablative fractional laser resurfacing: consensus report. JAMA dermatology. 2014,150(2): 187–193.
11. Manstein D., Herron GS., Sink RK., et al. Fractional photothermolysis: a new concept for cutaneous remodeling using microscopic patterns of thermal injury. Lasers Surg Med. 2004, 34(5): 426–438.
12. Hantash BM., Bedi VP., Kapadia B., et al. In vivo histological evaluation of a novel ablative fractional resurfacing device. Lasers Surg Med. 2007, 39(2): 96–107.
13. Wind BS., Meesters AA., Kroon MW., et al. Formation of fibrosis after nonablative and ablative fractional laser therapy. Dermatol Surg. 2012, 38(3): 437–442.
14. Klifto KM., Asif M., Hultman CS. Laser management of hypertrophic burn scars: a comprehensive review. Burns & Trauma, 2020, 8: tkz002.
15. Smith MA., Munster AM., Spence RJ. Burns of the hand and upper limb—a review. Burns. 1998, 24(6): 493–505.
16. Motamed S., Hasanpoor SE., Moosavizadeh SM., et al. Treatment of flexion contractures following burns in extremities. Burns. 2006, 32(8): 1017–1021.
17. Wainwright DJ. Burn reconstruction: the problems, the techniques, and the applications. Clin Plast Surg. 2009, 36(4): 687–700.
18. Goel A., Shrivastava P. Post-burn scars and scar contractures. Indian J Plast Surg. 2010, 43 (Suppl): S63–S71.
19. Karmisholt KE., Haerskjold A., Karlsmark T., et al. Early laser intervention to reduce scar formation–a systematic review. J Eur Acad Dermatol Venereol. 2018, 32(7): 1099–1110.
20. Draaijers LJ., Tempelman FR., Botman YA., et al. The patient and observer scar assessment scale: a reliable and feasible tool for scar evaluation. Plast Reconstr Surg. 2004, 113(7): 1960–1965.
21. Fearmonti R., Bond J., Erdmann D., et al. A review of scar scales and scar measuring devices. ePlasty. 2010, 10: e43.
22. Chaloupecká J. Možnosti využití laserů v dermatologii. Dermatol. praxi. 2008, 2(2): 96–99.
23. Katsambas AD., Lotti TM., Dessinioti C., et al. European handbook of dermatological treatments. Heidelberg: Springer-Verlag 2015 : 1313–1324
24. Żądkowski T., Nachulewicz P., Mazgaj M., et al. A new CO2 laser technique for the treatment of pediatric hypertrophic burn scars: An observational study. Medicine. 2016, 95(42).
25. Bowen RE. A novel approach to ablative fractional treatment of mature thermal burn scars. J Drugs Dermatol. 2010, 9(4): 389–392.
26. Levi B., Ibrahim A., Mathews K., et al. The use of CO2 fractional photothermolysis for the treatment of burn scars. J Burn Care Res. 2016, 37(2): 106–114.
27. Jung JY., Lee JH., Ryu DJ., et al. Lower‐fluence, higher‐density versus higher‐fluence, lower‐density treatment with a 10,600‐nm carbon dioxide fractional laser system: A split‐face, evaluator‐blinded study. Dermatologic surgery. 2010, 36(12): 2022–2029.
28. Alster T., Zaulyanov-Scanlon L. Laser scar revision: a review. Dermatologic Surgery. 2007, 33(2): 131–140.
29. Newman JB., Lord JL., Ash K., et al. Variable pulse erbium:YAG laser skin resurfacing of perioral rhytides and side-by-side comparison with carbon dioxide laser. Lasers Surg Med. 2000, 26(2): 208–214.
30. Stratigos AJ., Dover JS., Arndt KA. Laser treatment of pigmented lesions-2000: how far have we gone? Arch Dermatol. 2000; 136(7):
915–921.
31. Arora P., Sarkar R., Garg VK., et al. Lasers for treatment of melasma and post-inflammatory hyperpigmentation. J Cutan Aesthet Surg. 2012, 5(2): 93.
32. Lonie S., Baker P., Teixeira RP. Healing time and incidence of hypertrophic scarring in paediatric scalds. Burns. 2017, 43(3):
509–513.
33. Chipp E., Charles L., Thomas C., et al. A prospective study of time to healing and hypertrophic scarring in paediatric burns: every day counts. Burns & trauma. 2017, 5 : 3.
34. Thompson CM., Sood RF., Honari S., et al. What score on the Vancouver Scar Scale constitutes a hypertrophic scar? Results from a survey of North American burn-care providers. Burns. 2015, 41(7): 1442–1448.
35. Willows BM., Ilyas M., Sharma A. Laser in the management of burn scars. Burns. 2017, 43(7): 1379–1389.
36. Fang H., Kaiyang LV., Zhang F., et al. Improvement of scar contractures with ablative fractional CO2 laser treatments: a case report. Clin Surg. 2017, 2 : 1604.
37. Uebelhoer NS., Ross EV., Shumaker PR. Ablative fractional resurfacing for the treatment of traumatic scars and contractures. Semin Cutan Med Surg. 2012, 31(2):110–120.
Labels
Plastic surgery Orthopaedics Burns medicine TraumatologyArticle was published in
Acta chirurgiae plasticae

2021 Issue 4
- Possibilities of Using Metamizole in the Treatment of Acute Primary Headaches
- Metamizole at a Glance and in Practice – Effective Non-Opioid Analgesic for All Ages
- Metamizole vs. Tramadol in Postoperative Analgesia
- Spasmolytic Effect of Metamizole
- Safety and Tolerance of Metamizole in Postoperative Analgesia in Children
-
All articles in this issue
- Editorial
- Moriarty's sign – predictor of skin graft take
- Fractional CO2 laser therapy of hypertrophic scars – evaluation of efficacy and treatment protocol optimization
- Anterior open bite – diagnostics and therapy
- Cyanide poisoning in patients with inhalation injury – the phantom menace
- Cooperation of the maxillofacial and plastic surgeon in reconstructive surgical procedures in gunshot injury – a case report
- Surgical treatment and management of cutaneous squamous cell carcinoma in patients with dystrophic epidermolysis bullosa – a case report
- Combined fungal and bacterial infection in deep burns of the lower limb – a case report
- Celebrating the career and retirement of Dr Hana Řihová
- Acta chirurgiae plasticae
- Journal archive
- Current issue
- About the journal
Most read in this issue
- Anterior open bite – diagnostics and therapy
- Fractional CO2 laser therapy of hypertrophic scars – evaluation of efficacy and treatment protocol optimization
- Cyanide poisoning in patients with inhalation injury – the phantom menace
- Moriarty's sign – predictor of skin graft take