Endoscopic Third Ventriculostomy to Treat Hydrocephalus in Children with Brain Tumours – a Single Centre Experience
Endoskopická ventrikulostomie III. komory v léčbě hydrocefalu u dětí s mozkovými tumory – zkušenosti jednoho centra
Úvod:
Neuroendoskopie je miniinvazivní alternativou především implantace drenážních systémů. V indikovaných případech od ní lze očekávat výrazné snížení morbidity a zlepšení kvality života dětí s mozkovými nádory. U dětí s tumorem zadní jámy lební může neuroendoskopická. ventrikulostomie III. komory nahradit implantaci vnitřního drenážního systému. U obtížně přístupných nitrokomorových expanzí je možné zpřesnit diagnózu endoskopickým odběrem biopsie a v jedné době provést i definitivní ošetření sekundárního hydrocefalu.
Cíl:
Cílem práce bylo na základě získaných dat posoudit možnosti využití endoskopického přístupu v terapii sekundárního hydrocefalu u dětí s tumorem mozku.
Soubor a metodika:
Do souboru bylo zahrnuto celkem 21 dětí, 16 chlapců a 5 dívek s věkovým rozpětím od 1 do 16 let věku s primárním tumorem mozku a sekundárním obstrukčním hydrocefalem způsobeným tumorem, kteří byli operováni v průběhu období od 1. 1. 2008 do konce listopadu roku 2010.
Výsledky:
Celkem 6 nemocných zůstalo po operaci tumoru mozku bez trvalé drenáže likvoru, 5 má úspěšnou ETV, 10 dětí má trvale implantovaný V-P shunt (2 z nich po neúspěšné ETV). Délka samotného operačního výkonu pro hydrocefalus je srovnatelná pro shunt i ETV, nicméně délka prvotní hospitalizace je zřetelně kratší u nemocných s provedenou ETV. Rovněž komplikací, které si vynutily další operační revize, bylo více u nemocných s implantovaným drenážním systémem.
Závěr:
Na základě zkušeností s uvedeným souborem dětských pacientů byl endoskopický miniinvazivní přístup implementován do terapeutického algoritmu jako metoda první volby v terapii sekundárního hydrocefalu u dětí s tumorem zadní jámy lební. V případě nemožnosti provedení ETV nebo jejího selhání je metodou druhé volby implantace vnitřního drenážního systému.
Klíčová slova:
endoskopická III. ventrikulostomie – hydrocefalus – tumor mozku – dětská onkologie
Authors:
J. Ventruba 1; Z. Mackerle 1; K. Zitterbart 2; J. Sterba 2
Authors‘ workplace:
University Hospital Brno
Department of Pediatric Surgery, Orthopedics and Traumatology
1; University Hospital Brno
Pediatric Oncology Department
2
Published in:
Cesk Slov Neurol N 2012; 75/108(2): 212-217
Category:
Short Communication
Overview
Introduction:
Neuroendoscopy is a mini-invasive alternative to implantation of drainage systems in particular. In indicated cases, this method could lower morbidity and increase the quality of life in children with brain tumours. In children with a tumour of posterior fossa, endoscopic third ventriculostomy (ETV) could be used instead of internal drainage system implantation. In patients with deep-seated intraventricular expansions, the diagnosis may be refined using endoscopic sample biopsy and, simultaneously, definitive treatment can be provided of the secondary hydrocephalus.
Aim:
To obtain short-term outcome data for endoscopic treatment of hydrocephalus in children with brain tumours in a tertiary care centre and to evaluate reliability of this approach.
Patients and method:
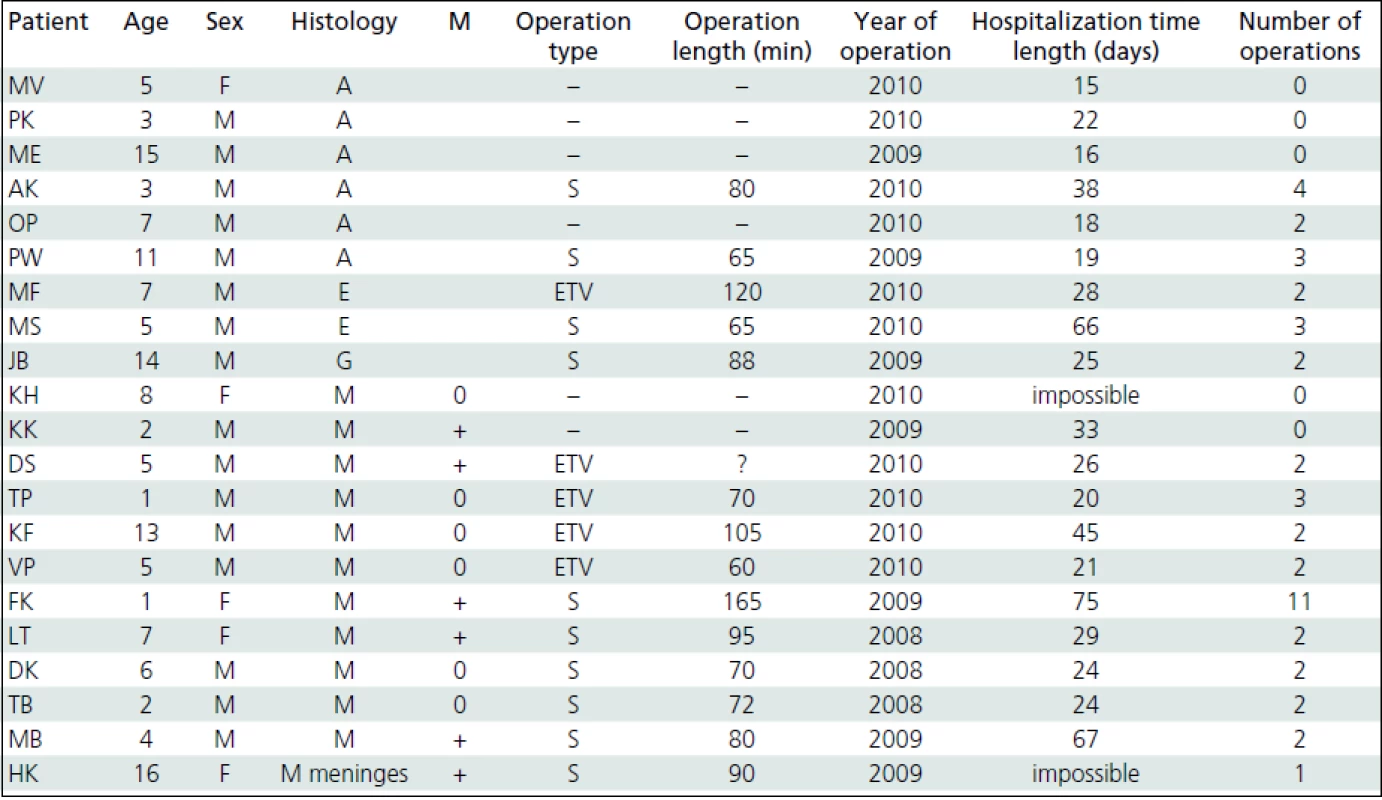
The sample involved 21 children, 16 boys and 5 girls, aged 1 to 16 years with a primary brain tumour and secondary obstructive hydrocephalus caused by the tumour who underwent surgery between 1st January 2008 and the end of November 2010.
Results:
Six patients had no permanent cerebral spinal fluid (CSF) drainage after the brain tumour surgery, other 5 had a successful ETV, 10 children had a permanent ventricular-peritoneal shunt (V-P) implanted (2 of them after an unsuccessful ETV). The length of the procedure for hydrocephalus itself is comparable between shunt and ETV. Nevertheless, the length of primary hospitalization is markedly shorter for the patients with ETV (28 das versus 41 days for patients with V-P shunt). Likewise, complications demanding further surgical revisions were more frequent in patients with implanted drainage system.
Conclusion:
The miniinvasive endoscopic approach was included in our therapeutic algorithm as the method of choice to treat secondary hydrocephalus in children with posterior fossa tumour. Implantation of an internal drainage system is the second line approach in patients in whom ETV cannot be performed or fails.
Key words:
endoscopic third ventriculostomy – hydrocephalus – brain tumour – paediatric oncology
Introduction
Paediatric patients with a brain tumour used to form the saddest spheres of paediatric neurosurgery and oncology. In addition, recent publications show that medulloblastoma continues to be a tumour with severe prognosis with 5-year EFS of about 50–70% [1]. With the development of new surgical techniques, microsurgery, endoscopic methods as well as new chemotherapy and targeted radiotherapy options, the chances for long-term survival and even complete recovery of children with malignant brain tumours significantly increases. In addition, the need to improve the quality of life of the afflicted children is increasingly being stressed as is the need to use minimally invasive surgical techniques as well as the entire therapeutic approach in children whose histological subtype is more favourable (particularly the pilocytic astrocytoma). The care for a paediatric patient should aim not only to cure the patient but also to provide maximum possible comfort, reduce the number of surgeries, their length, number of surgical wounds and stress and pain associated with it. Implanted ventricular-peritoneal shunt very negatively affects the lives of paediatric patients with posterior fossa tumours. There is no doubt that the ventricular-peritoneal (V-P) shunt represents a significant advance in the treatment of hydrocephalus in paediatric patients. However, in spite of indisputable benefits, it bears a risk of numerous mechanical or infectious complications. If it is not necessary, implantation of the shunt should be avoided or replaced with a ’gentler’ and safer method, such as endoscopic third ventriculostomy (ETV) in obstructive hydrocephalus [2,3]. Even though the financial aspects are less important, it needs to be acknowledged that the increasing quality of shunt systems is associated with a steady price increase. In spite of the high purchase costs of endoscopic instrumentarium, endoscopy seems to be a safer and more effective method for the patients as well as a more cost-effective solution for health care providers [4].
At present, obstructive hydrocephalus is the primary diagnosis where endoscopic approach can be applied. In our study, the method is used specifically in patients with posterior fossa tumours [5].
In a small number of patients, endoscopy can be used for a biopsy from intraventricular tumours or during ventricular tumour procedures [6,7]. Endoscopy of the third cerebral ventricle has become a standard, whereas robust anatomical evaluation, such as description of the third ventricle base anatomy in hydrocephalic patients, is required when it is to be performed safely [8].
The aim of the project was to assess the advantages and risks of endoscopic approach for children with brain tumours and secondary obstructive hydrocephalus and its comparison with the traditional method of V-P shunt implantation.
In individual cases there was a secondary aim to examine the feasibility of endoscopy as a diagnostic tool in deep--seated intraventricular brain tumours in children.
Authors attempted to prove that the neuroendoscopy is a mini-invasive alternative to the drainage system implantation in particular and, in indicated cases, a notable decrease in morbidity as well as increased quality of life in children with brain tumours can be expected. It has been assumed that, in children with a posterior fossa tumour, the endoscopic third ventriculostomy could replace external ventricular drainage and, eventually, the permanent V-P shunt. In patients with deep-seated intraventricular expansions, diagnostic refinement is expected using an endoscopic biopsy sample. Eventually, endoscopy can be used for an opening or targeted drainage of a tumour cyst.
Patients and method
The sample included 21 children, 16 boys and 5 girls, aged 1 to 16 years with a primary brain tumour and secondary obstructive hydrocephalus caused by the tumour who underwent surgery between 1st January 2008 and the end of November 2010. Diagnosis of the tumour and of subsequent obstructive hydrocephalus was always made on clinical symptoms and was confirmed by CT or brain MRI scan. All patients were and still are treated at the Paediatric Oncology Department, University Hospital Brno. Neurosurgical drainage surgery was, in the majority of patients, performed at the Department of Paediatric Surgery, Orthopaedics and Traumatology, University Hospital Brno. Three children had the surgery done at another neurosurgical departments. One patient had an initial diffuse tumoural spread across the brain and spinal cord meninges and underwent a biopsy through laminectomy. All other patients were indicated for a resection of the posterior fossa tumour.
Pathology revealed low-grade astrocytoma in 6 children, 1 high-grade brain stem glioma, 2 patients had ependymoma and 12 children had medulloblastoma//PNET. Adjuvant treatments, if indicated, were according to the current protocol by one of the international paediatric oncology cooperative groups, i.e. either the Société Internationale d’Oncologie Pédiatrique (SIOP) or the Children’s Oncology Group (COG). When having symptoms of acute hydrocephalus, the majority of patients were preoperatively secured by a temporary external ventricular drainage. Postoperatively, the need for a definitive CSF drainage was decided according to the clinical outcome. If surgery indicated the endoscopic third ventriculostomy with Ommaya reservoir placement was preferred (Fig. 1–4) [9].




Subsequently, we evaluated a number of surgical complications as well as surgical burden of a particular procedure (numbers of surgical wounds, length of surgery) and compared the duration of primary hospitalization. The aim was also to evaluate the cost of ETV compared to the V-P shunt implantation.
Results
Postoperatively, 6 out of 21 patients did not need permanent CSF drainage, 5 children underwent a successful ETV, 10 patients had the permanent V-P shunt implanted (2 of them after failed ETV). Summary results are shown in the Tab. 1.
The average duration of surgery was 88 minutes including preparation and administration of anaesthesia. Shunt implantation took 87 minutes and ETV 89 minutes. The difference is not statistically significant. Shorter surgical part of ETV procedure (anaesthesia is not included) encourages its use. Considering the age of the treated patients, anaesthesia often represents as much as half of the total surgery time.
The mean duration of primary hospitalization during which the resection and hydrocephalus surgery was performed was 33 days; 21 days for pilocytic astrocytoma and 37 days for medulloblastoma. Patients with ETV spent 28 days (mostly medulloblastomas, does not include histology) and patients with implanted shunt 41 days in a hospital.
As expected, patients with no need for any drainage had the shortest hospitalization, 20 days on average. Complications in patients with successful ETV were only sporadic. One patient experienced a temporary minor CSF fluctuation over the burr hole that healed when a compression bandage was applied and a single shot puncture performed. There were two unsuccessful ETVs (28% of the total number of patients with ETV) that were resolved with shunt implantation. In the first patient, the approach had to be revised due to lasting intracranial hypertension with bulging pseudomeningocele after a posterior fossa tumour surgery. The second failure occurred 6 weeks after the ETV and manifested with intracranial hypertension due to decompensation of hydrocephalus after the endoscopy.
Three out of the 10 children (30%) with V-P shunt had complications related to the implanted shunt. In two patients this meant one surgical revision only to resolve complications linked to over-drainage. Repeated complications in one patient required a total of 11 surgeries. Most frequently these were revisions due to infectious complications at the first of the peritoneal catheters with an inevitable temporary externalization of the whole shunt system. Subsequently, after the shunt replantation, several revisions were required because of wound dehiscence on the head. This dehiscence is expected to have resulted from chronic mitigated infection during complex cancer therapy, including repeated chemotherapy cycles with profound and prolonged episodes of neutropaenia. In patients with a shunt, the total number of surgeries to manage hydrocephalus, including possible preoperational drainages, was 3.2. If we exclude the patient with multiple surgical revisions, the final number of surgeries was 2.3. Patients with ETV had 2.4 surgeries, including the 2 patients who required subsequent V-P shunt implantation.
Patients who were maintained without any drainage continue to be monitored with no symptoms of hydrocephalus or intracranial hypertension. These were predominantly the patients who were diagnosed with pilocytic astrocytoma (4/6).
Two children died, both of the disease progression. One had a histological diagnosis of glioblastoma multiforme and the other of cerebellar medulloblastoma. However, median of follow-up is too short to evaluate long-term survival.
Calculating the cost of investments and expendable supplies, the rate of return of endoscopic instrumentarium is approximately 20 ETV-type surgeries. If more expensive programmable shunts are used, then the rate of return is much faster.
In addition, in terms of economics, the ETV expedience increases in time as there is a lower number of reoperations and, therefore, reduced additional surgery and hospitalization costs. Compared to historical controls, patients with high-grade posterior fossa tumours who required adjuvant therapies – chemotherapy and radiotherapy – experienced improved overall status prior to the commencement of oncology treatments.
In addition to the patients with posterior fossa tumour and hydrocephalus, the endoscopy approach was also used to perform biopsy of intraventricular tumour in 5 paediatric patients. There were 2 craniopharyngiomas, 1 pilocytic astrocytoma, 1 high-grade glioma and 1 malignant embryonal tumour. In all cases, the biopsy was diagnostic in spite of a quite small size of the sample. We did not observe any surgical complications. In neither of the patients was it possible to perform the biopsy concurrently with the initially planned ETV because of size of the tumour. All patients with the third ventricle tumour were treated with endoscopic biopsy approached through frontal horn of lateral ventricle.
Discussion
In the majority neurosurgical departments, neuroendoscopy is presently considered to be the method of choice in therapy of secondary hydrocephalus in children with posterior fossa tumour [3]. It is highly effective (up to 100%) when performed in patients with mesencephalic or tectal tumours and pineal region tumours. Endoscopy is preferred to ventricular-peritoneal shunt implantation in cases with obstructive hydrocephalus evoked by these tumours [10]. Since 1923, when Mixter first published the use of endoscopic third ventriculostomy, the neuroendoscopic surgery technique has evolved and indication spectrum expanded. Nowadays, endoscopic treatment is the most convenient therapeutic procedure in paediatric patients with obstructive hydrocephalus [11]. The benefits of the technique are clearly documented in statistical evaluations of large samples of patients where the bias resulting from diverse primary diagnoses (leading to the obstructive hydrocephalus) is limited [12]. Such studies also show that, in a very short time of several months post-operatively, the risk of ETV failure could be higher than the risk of shunt malfunction. However, in the long-term perspective, ETV is associated with a significantly lower risk of failure than shunts [12]. A functional shunt is probably comparable to ETV [13] when the quality of life is considered. Nevertheless, this needs to be confirmed by further, more detailed studies on larger patient samples.
Even though endoscopic third ventriculostomy does not preclude development of post-surgical hydrocephalus , it contributes to prevention of acute post-surgical hydrocephalus due to postoperative cerebral tissue oedema. ETV also lowers the risk of CSF infection, higher in patients with external ventricular drainage, and minimizes the risk of over-drainage as it constitutes more physiological drainage of CSF than temporary or permanent drainage systems [14]. This can also explain the obviously slower reduction in dilation of cerebral ventricles after ETV than with V-P shunt.
Failure of endoscopic third ventriculostomy (26%) is lower than failure of ventricular-peritoneal shunt (42%) in surgical solution of obstructive hydrocephalus in children with brain tumours [15].
The ETV failed in 2 cases out of 7 patients (28%) in our sample group. Complications of the V-P shunt were recorded in 3 cases out of 10 (30%), in one case even repeatedly in the same patient.
ETV was successful in 3 of the 6 patients with M 0 stage medulloblastomas, and in 1 of the 6, children with a metastatic disease.
In patients with tumours in the dorsal part of the third ventricle, endoscopic biopsy can be very effectively (with 100% successfulness) performed at the same time as endoscopic third ventriculostomy, thus forming an optimal therapeutic single-stage procedure [16]. However, at our neurosurgical department, we did not identify any tumour in which successful ETV could be feasible together with biopsy at the same time. All children with the third ventricle tumour had a radiologically established diagnosis at the time, when the tumour practically blocked the entire third ventricle and it was technically impossible to perform the ETV. Even in these cases, biopsy sampling using neuroendoscope represented a significant contribution to the diagnosis. Likewise, endoscopic biopsy sampling is preferred in patients in whom radical surgical intervention is not practicable, such as in patients with suspected craniopharyngioma [13]. In all endoscopic biopsy cases, the histology was conclusive and enabled diagnosis. Literature suggests somewhat lower proportion of histological diagnosis (70%). At our department, we use a special grasper tool to extract a greater volume of tissue. This might explain the higher efficacy [6].
Authors initially planned to use endoscopic third ventriculostomy at the acute stage, preferably on the day of admission of a diseased child to the hospital and after the diagnosis of a brain tumour and secondary hydrocephalus had been made. However, the majority of our paediatric patients are admitted to the hospital with an advanced hydrocephalus and expressed acute intracranial hypertension symptoms. A simple, fast surgery – placement of a temporary external ventricular drainage – thus seems to be the most desirable and timely solution. ETV is technically a bit more complicated; it requires a well-coordinated neurosurgical team and is thus more suitable as an optional procedure after tumour resection.
The analysis of the ETV procedures at our department provided an interesting outcome associated with the duration of hospitalization; patients with ETV spent an obviously shorter time at the hospital than the patients with an implanted shunt. This was regardless of the fact that 4 out of 5 of them were diagnosed with medulloblastoma that itself essentially extends the time of hospitalization. On the other hand, patients with the shunt had higher diversity of histological diagnoses, including several patients with pilocytic astrocytoma. This prolongation cannot be simply explained by higher occurrence of surgical complications related to the V-P shunt, for these complications usually occurred during subsequent hospitalizations (three patients).
As we expected – hospitalization was the shortest in patients in whom there was no need for any CSF drainage after tumour surgery. In adition, hospitalization in patients with pilocytic astrocytoma was shorter than that in patients with medulloblastoma, regardless of drainage type.
Reduction of the cerebral ventricle width seems quite unreliable for evaluation of the efficacy of the drainage surgery. Especially after the ETV, cerebral ventricles frequently remain dilated in spite of the explicit clinical effect. In addition to the direct measurement of intracranial pressure, clinical condition of the patient continues to be the main parameter for evaluation of the effect of hydrocephalus surgery [13].
At the time of the study, we were unable to perform dynamic MRI scans to assess the CSF flow through the anastomosis. At present, this evaluation is a standard part of postoperative MRI protocol.
Conclusion
Endoscopic mini-invasive approach is a feasible and effective method of choice to manage secondary hydrocephalus in children with posterior fossa tumour. If ETV cannot be performed or it fails, internal drainage system implantation is the method of the second choice. As these patients mostly present with the symptoms of acute hydrocephalus on admission, authors prefer to postpone the definitive drainage surgery along with acute placement of external ventricular drainage.
This research was supported from the grant number IGA MT CR NS 9873-3.
Accepted for review: 13. 6. 2011
Accepted for publication: 28. 6. 2011
Jiri Ventruba, M.D., Ph.D.
Department of Pediatric Surgery, Orthopedics and Traumatology
University Hospital Brno
Jihlavská 20
625 00 Brno
e-mail: jiriventruba@seznam.cz
Sources
1. Fadrus P, Lakomý R, Hübnerová P, Slabý O, Keřkovský M, Svoboda T et al. Intrakraniální nádory – diagnostika a terapie. Interní Med 2010; 12 (7, 8): 376–381.
2. Kulkarni AV, Drake JM, Kestle JRW, Mallucci CL, Sgouros S, Constantini S. Predicting who will benefit from endoscopic third ventriculostomy compared with shunt insertion in childhood hydrocephalus using the ETV Success Score. J Neurosurg Pediatr 2010; 6(4):310–315.
3. Fritsch MJ, Doerner L, Kienke S, Mehdorn HM. Hydrocephalus in children with posterior fossa tumors: role of endoscopic third ventriculostomy. J Neurosurg 2005; 103 (1 Suppl): 40–42.
4. Sacko O, Boetto S, Lauwers-Cances V, Dupuy M, Roux FE. Endoscopic third ventriculostomy: outcome analysis in 368 procedures. J Neurosurg Pediatr 2010; 5(1): 68–74.
5. Sainte-Rose C, Cinalli G, Roux FE, Maixner R, Chumas PD, Mansour M et al. Management of hydrocephalus in pediatric patiens with posterior fossa tumors: the role of endoscopic third ventriculostomy. J Neurosurg 2001; 95(5): 791–797.
6. Ahn ES, Goumnerova L. Endoscopic biopsy of brain tumors in children: diagnostic success and utility in guiding treatment strategies. J Neurosurg Pediatr 2010; 5(3): 255–262.
7. Novák Z, Chrastina J, Feitová V, Lžičařová E, Říha I. Možnosti neuroendoskopie v komplexní terapii kraniofaryngeomů. Onkologie 2009; 3(3): 194–197.
8. Chrastina J, Novák Z, Říha I, Feitová V, Koutková H. Geometrická studie rozměrů III. komory a její spodiny z pohledu neuroendoskopie. Ces Radiol 2008; 62(4): 388–394.
9. Parikh D, Foroughi M, Nannapaneni R, Hatfield RH. Is the routine placement of a CSF reservoir following endoscopic third ventriculostomy justified? Br J Neurosurg 2009; 23(5): 521–523.
10. Ray P, Jallo GI, Kim RY, Kim BS, Wilson S, Kothbauer K et al. Endoscopic third ventriculostomy for tumor-related hydrocephalus in a pediatric population. Neurosurg Focus 2005; 19(6): E8.
11. Hellwig D, Grotenhuis JA, Tirakotai W, Riegel T, Schulte DM, Bauer BL et al. Endoscopic third ventriculostomy for obstructive hydrocephalus. Neurosurgical Review 2005; 28(1): 1–34.
12. Kulkarni, AV, Drake J, Kestle J, Mallucci C, Sgouros S, Constantini S. Endoscopic third ventriculostomy vs cerebrospinal fluid shunt in the treatment of hydrocephalus in children: a propensity score-adjusted analysis. Neurosurgery 2010; 67(3): 588–593.
13. Kulkarni AV, Hui S, Shams I. Quality of life in obstructive hydrocephalus: endoscopic third ventriculostomy compared to cerebrospinal fluid shunt. Childs Nerv Syst 2010; 26(1): 75–79.
14. Ruggiero C, Cinalli G, Spennato P, Alberti F, Cianciulli E, Trischitta V et al. Endoscopic third ventriculostomy in the treatment of hydrocephalus in posterior fossa tumors in children. Childs Nerv Syst 2004; 20(11–12): 828–833.
15. de Ribaupierre S, Rilliet B, Vernet O, Regli L, Villemure JG. Third ventriculostomy vs ventriculoperitoneal shunt in pediatric obstructive hydrocephalus: results from a Swiss series and literature review. Childs Nerv Syst 2007; 23(5): 527–533.
16. Roopesh Kumar SV, Mohany A, Santosh V, Satish S, Devi BI, Praharaj SS et al. Endoscopic options in management of posterior third ventricular tumors. Childs Nerv Syst 2007; 23(10): 1135–1145.
Labels
Paediatric neurology Neurosurgery NeurologyArticle was published in
Czech and Slovak Neurology and Neurosurgery

2012 Issue 2
- Advances in the Treatment of Myasthenia Gravis on the Horizon
- Memantine Eases Daily Life for Patients and Caregivers
- Memantine in Dementia Therapy – Current Findings and Possible Future Applications
-
All articles in this issue
- Postural Instability, Gait Disorders and Falls in Parkinson’s Disease
- Superior Temporal Sulcus and its Functions
- The Algorithm of CSF Examination according to the Reccomendation of the Committee of CSF and Neuroimmunology of the Czech Neurological Society
- The Use of Percutaneous Endoscopic Gastrostomy – Overview of Indications, Description of the Technique and Current Trends in Neurology
- Imaging Techniques to Evaluate Morphological Correlates of Cognitive Dysfunction in Multiple Sclerosis Patients
- Nutritional and Metabolic Disorders in Parkinson’s Disease
- Measuring of Cognitive Deficit after Cerebral Aneurysm Intervention
- Polysomnographic Findings in Children with Attention-Deficit//Hyperactivity Disorder Investigated for Sleep Disturbances
- Treatment of Neurogenic Detrusor Overactivity after Spinal Cord Injury Using Botulinum A Toxin. Comparison of Endoscopic Submucosal and Intramuscular Route of Application
- Our Experience with Lateral Supraorbital Approach in Surgery of Intracranial Aneurysms
- Visual Functions in Premature Children with Perinatal Brain Injury
- Obstructive Sleep Apnoe and CPAP – is it Reasonable to Solve Nasal Patency?
- Therapeutic Options for Prevention of Cerebrovascular Events in Patients with Carotid Stump Syndrome – Case Studies
- Oligosymptomatic Forms of Myotonic Dystrophy Type 2
- Reversal of Traumatic Pentaplegy after Combined C1–C2 Fracture
- Guideline for the Diagnosis and Therapy of Myasthenia Gravis
- Dementia Diagnosis and Treatment in Czech Neurological and Psychiatric Practices
- Endoscopic Third Ventriculostomy to Treat Hydrocephalus in Children with Brain Tumours – a Single Centre Experience
- Detection of Anaplastic Foci within Infiltrative Gliomas with Nonsignificant Contrast Enhancement using 5-aminolevulic Acid – a Report of Five Cases
- Czech and Slovak Neurology and Neurosurgery
- Journal archive
- Current issue
- About the journal
Most read in this issue
- The Use of Percutaneous Endoscopic Gastrostomy – Overview of Indications, Description of the Technique and Current Trends in Neurology
- Postural Instability, Gait Disorders and Falls in Parkinson’s Disease
- The Algorithm of CSF Examination according to the Reccomendation of the Committee of CSF and Neuroimmunology of the Czech Neurological Society
- Obstructive Sleep Apnoe and CPAP – is it Reasonable to Solve Nasal Patency?
