Data Sources for Monitoring of Non-healing Wounds in a National Health Information System – Epidemiology of Non-healing Wounds – Analysis of the National Register of Hospitalized Patients in 2007– 2015
Datové zdroje pro sledování nehojících se ran v Národním zdravotnickém informačním systému – epidemiologie nehojících se ran v České republice – analýza Národního registru hospitalizovaných v letech 2007 – 2015
Cíl:
Cílem studie bylo posoudit možnost využití datových zdrojů Národního informačního zdravotnického systému k posouzení epidemiologie nehojících se ran. Analyzovány byly hospitalizační případy s diagnózou související s nehojící se ránou dle MKN-10 a hodnoceny výkony a příčiny úmrtí u pacientů se sledovanou diagnózou.
Metodika a soubor:
Retrospektivní observační průřezová studie s využitím dat z Národního registru hospitalizovaných v České republice (2007 – 2015) a z informačního systému zemřelých (IS ZEM). Sledované diagnózy (MKN-10): I70.2, E10.5, E11.5, L89, L97, I83.0, I83.2, L03.0, L03.1, L02.3, L02.4.
Výsledky:
Z 19 979 081 záznamů bylo ročně identifikováno 35 824 (50,7 %) s vybranou diagnózou související s nehojící se ránou jako hlavní hospitalizační diagnózou a 34 785 (49,3 %) hospitalizací ročně jako vedlejší diagnózy.
Závěr:
Ateroskleróza končetinových tepen byla vykázána nejčastěji ze sledovaných diagnóz (I70.2). Nejméně často vykazovanou diagnózou byl vřed dolní končetiny (L97). Nejčastěji vykazovaný výkon za hospitalizace se lišil dle typu hospitalizační diagnózy. Chirurgické výkony byly vykazovány častěji u hospitalizací s diagnózami E10.5, E11.5, dekubitální vřed (L89), absces a flegmóna (L02.3, L02.4). Konzervativní postupy byly vykazovány u hospitalizací s diagnózou varikózní vřed (I83.0, I83.2) a vřed dolní končetiny (L97). Úmrtí za hospitalizace bylo vykázáno častěji u pacientů s dekubitem (L89), ale pro jinou diagnózu.
Klíčová slova:
epidemiologie – nehojící se rána – hospitalizace – monitorování – národní registry – výkony – úmrtí
Autoři deklarují, že v souvislosti s předmětem studie nemají žádné komerční zájmy.
Redakční rada potvrzuje, že rukopis práce splnil ICMJE kritéria pro publikace zasílané do biomedicínských časopisů.
Authors:
A. Pokorná 1,2; K. Benešová 2,3; J. Mužík 1–3
; J. Jarkovský 1–3; L. Dušek 1–3
Authors‘ workplace:
Department of Nursing, Faculty of
Medicine, Masaryk University, Brno
Czech Republic
1; Institute of Health Information and
Statistics of the Czech Republic
Prague, Czech Republic
2; Institute of Biostatistics and Analyses
Faculty of Medicine, Masaryk University
Brno, Czech Republic
3
Published in:
Cesk Slov Neurol N 2017; 80(Supplementum 1): 8-17
Category:
Original Paper
doi:
https://doi.org/10.14735/amcsnn2017S8
Overview
Aim:
The aim of this study is to analyse possibilities for using data from the National Health Information system to monitor the epidemiology of non-healing wounds. Hospital stays related to non-healing wounds (according to ICD-10) in acute and long-term care facilities in the Czech Republic (2007 – 2015), medical interventions and causes of death in patients with monitored diagnosis related to non-healing wounds were analysed.
Methods and sample:
Retrospective observational cross-sectional study using routinely collected data from the National Register of Hospitalized Patients and Information System of Deaths (in Czech: IS ZEM). Monitored diagnoses (ICD-10): I70.2, E10.5, E11.5, L89, L97, I83.0, I83.2, L03.0, L03.1, L02.3, L02.4.
Results:
From a total 19,979,081 hospital records per year, we identified 35,824 (50.7%) with the selected diagnosis related to non-healing wound as a primary diagnosis and 34,785 (49.3%) as a secondary diagnosis.
Conclusion:
Atherosclerosis of arteries of extremities (I70.2) was recorded most frequently. The least frequently reported diagnosis was ulcer of a lower limb (L97). The most commonly reported medical intervention during hospitalization varied according to the type of the hospital (admission) diagnosis. Surgical interventions were reported mostly in hospitalizations with diagnoses E10.5, E11.5, decubitus ulcer (L89), cutaneous abscess, furuncle and carbuncle of buttock and limb (L02.3, L02.4). Conservative treatment was performed in diagnoses of varicose veins of the lower extremities with ulcer (I83.0, I83.2) and ulcer of lower limb, not elsewhere classified (L97). Deaths during hospitalization were reported more often in patients with decubitus ulcers (L89) but for a different diagnosis and cause of death.
Key words:
epidemiology – non-healing wound – hospitalization – monitoring – national registers – medical intervention – death
Introduction
Chronic wounds (or, according to the current terminology, non-healing wounds) include various types of damage to the skin and tissue integrity. The Wound Healing Society classifies chronic wounds according to their aetiology into four categories: pressure ulcers, diabetic ulcers, venous ulcers, and arterial insufficiency ulcers [1]. Chronic wounds used to be defined from a time point of view as wounds in which the normal healing process leading to the anatomic and functional integrity of tissues within three months does not occur [2,3]. Unambiguous terminology is far from agreed upon and chronic wounds are also referred to as non-healing wounds or hard-to-heal wounds and ulcers. Also, the time necessary for classifying such wounds as chronic varies from 4 weeks to 3 months and may be even longer [4,5]. Chronic wounds are often referred to as ulcers and can be defined as wounds with a varying depth of skin and tissue damage in full thickness and with a slow tendency to heal [6]. Chronic wounds are often a manifestation of comorbidity, or multimorbidity and represent the socalled silent epidemic, which affects a large part of the world’s population.
Chronic wounds therefore present a significant and often underestimated burden for an individual, the healthcare system and society as a whole [7 – 9]. Currently, there are no reliable estimations of the total occurrence of chronic wounds in the Czech Republic for various forms of care, types of healthcare providers and categories of chronic wounds. However, information about non-healing wounds is important for planning healthcare costs, not only with regard to demographic trends (namely an increasing number of elderly people) but also to the occurrence of diseases caused by lifestyles which result in the emergence of non-healing of wounds. Knowledge on the prevalence and incidence of chronic wounds in relation to the characteristics of the population is important both for planning of healthcare and resource allocation for such care. Nevertheless,such information is still not available on the national and international levels [5]. Neither in the Czech Republic nor internationally is there any uniform methodology for monitoring the occurrence of non-healing wounds. Most of the monitoring processes depend on the local know-how of individual healthcare providers despite the fact that information on the occurrence of non-healing wounds and pressure ulcers is considered an indicator of healthcare quality and contributes significantly to assessing the cost of such care (prolonged hospitalization, increased usage of medication and medical items necessary for treatment of such complications, etc.) [10]. It is necessary to emphasize once more that there is no information database in the Czech Republic which would enable specific monitoring of the occurrence of non-healing wounds in patients, and therefore the National Register of Hospitalised Patients (NRHOSP) was used for the following analysis. The NRHOSP registers all patients hospitalized in the Czech Republic. Patients whose hospitalization ended in the monitored reference period 2007 – 2015 were selected for the analysis. For evaluation of causes of death in hospitalized patients with non-healing wounds, data from the Information System of Deaths (in Czech: IS ZEM) were used.
Objectives
The main objective of this retrospective observational study was to determine what mandatory and routinely recorded data in the National Register of Hospitalised Patients (NRHOSP) can be used to evaluate diagnoses associated with the occurrence of non-healing wounds in patients. Furthermore, it is aimed at ascertaining whether and how hospital stays differ depending on the individual monitored diagnoses according to the ICD-10 in both acute and post-acute inpatient care. We also focused on what types of medical interventions are most commonly reported in hospitalized patients and what the most common causes of death are in patients with the selected monitored diagnoses.
Methodology
Data from NRHOSP for the period 2007 – 2015 were analysed. We included records which reported some of the monitored diagnoses and where occurrence of non-healing wounds may be expected (Fig. 1). The following diagnoses according to ICD-10 were monitored: I70.2, E10.5, E11.5, L89, L97, I83.0, I83.2, L03.0, L03.1, L02.3, L02.4. A statistical analysis of the data was performed with the use of IBM SPSS Statistics for Windows, version 22.0.0.1.
Methodology and classification of hospitalization records related to the occurence of non-healing wounds
As it follows from the Fig. 1, records of patients’ hospitalizations with selected diagnoses according to ICD-10 were included. Based on an analysis of expert sources, the diagnoses were chosen so that occurrence of non-healing wounds can be expected. Patients were divided into the following groups:
- atherosclerosis of arteries of extremities – I70.2;
- type 1 and 2 diabetes mellitus with peripheral circulatory complications – E10.5, E 11.5;
- decubitus ulcer and pressure area – L89;
- varicose veins of lower extremities with ulcer and with both ulcer and inflammation – I83.0, I83.2;
- cellulitis of finger and toe and other parts of limb – L03.0, L03.1;
- cutaneous abscess, furuncle and carbuncle of buttock and limb – L02.3, L02.4;
- ulcer of lower limb, not elsewhere classified – L97.
Patients were further classified into diagnostic categories based on their primary or secondary hospitalization diagnosis.
Data source
The analysis is based on in the data that are managed by the Institute of Health Information and Statistics of the Czech Republic (IHIS CZ), which are collected within the framework of the National Health Information System (NHIS) and the national health registers.
National Register of Hospitalised Patients (NRHOSP) – is a nationwide population register which records all people who were admitted to inpatient facilities and whose hospitalization ended during the monitored period. From the period 2007 – 2015, 19,979,081 records of hospital stays are available in the Czech Republic in both acute and post-acute care. Information System Deaths (in Czech: IS ZEM) – is the basic source of information on every death and includes information recorded on the death certificate (in Czech: LPZ – List o prohlídce zemřelého). This certificate is completed by the doctor, who examined the dead patient. Besides basic socio-demographic characteristics, the order of causes leading to death are recorded (coded according to ICD-10) and data by the end of 2015 are available.
Limits of the study
A group of diagnoses coded according to ICD-10 was analysed; in these diagnoses the occurrence of a wound can be expected. However, it is not always possible to identify its occurrence from the data of the NRHOSP. Therefore, an analysis of diagnoses was also conducted which may not be defined by all expert sources as non-healing wounds (L03.0, L03.1, L02.3, L02.4), but the aim was to ascertain the length of individual hospital stays and interventions reported for the given diagnoses. The analysis also focused on identification of typical age categories for such infectious diseases which are associated with damage to tissue integrity and with risk of chronicity. Similarly, in hospital stays with reported diagnoses E10.5 and E11.5, it is not possible to determine definitively whether a wound occurred in the patient due to the process of reporting data in clinical practice. Therefore, we conducted a complementary analysis in which we concentrated firstly on the records of patients with the dianosis E10.5/ E11.5/ E13.5, who simultaneously have a recorded code of the diagnosis L97, namely ulcer of lower limb, not elsewhere classified (both in the primary or secondary diagnosis). We identified only 1.2% of such patient for the whole monitored period 2007 – 2015. During analysis of hospital records for L97, we identified 6.1% patients who have simultaneously with the diagnosis L97 also E10.5/ E11.5/ E13.5 (primary or secondary diagnosis) in the period 2007–2015. An other limitation of this study is the form of data kept in NRHOSP, these data namely contain description of individual hospital episodes compiled into so-called hospital stay records (in Czech: pobytové věty) which may result in loss of some of the secondary diagnoses, because according to the current methodology of compiling hospital stay records these reports must include only five major secondary diagnoses. However, almost 90% of hospital stays which were assessed in this analysis are only “one-episodic” and therefore potential loss of data is minimal. We did not analyse records of hospital stays which did not report the monitored diagnoses but in which treatment may have been performed that was included in the monitored medical interventions (change of dressing, etc.) This creates a space for a follow-up analysis of NRHOSP data which will primarily be based on identifying interventions typical of wound care.
Results and discussion
From the total of 19,979,081 hospital stays in the period 2007 – 2015 (i.e. an average of 2,219,898 stays per year), we identified 70,609 hospital stays per year for the selected diagnoses regardless of whether being reported as primary or secondary ones. Out of that total number, 35,824 (50.7%) hospital stays per year for the selected diagnoses were reported as primary diagnosis, and 34,785 (49.3%) as secondary diagnosis (Fig. 1).

While the diagnosis of atherosclerosis of arteries of extremities shows almost equal distribution between primary diagnosis (n = 21,641) and secondary diagnosis (n = 20,141) and cellulitis of finger and toe and other parts of limb – L03.0, L03.1 and cutaneous abscess, furuncle and carbuncle of buttock and limb – L02.3, L02.4 occur more often on the position of primary diagnosis, the other monitored diagnoses were more commonly reported as secondary diagnoses. Recording of individual diagnoses associated with the occurrence of wounds is relatively constant in the monitored period (2007 – 2015) despite the expected influence of the gradual introduction and use of the DRG system and flat-rate payment for medical treatment (Fig. 2). The only exception we can observe is an increase in reporting pressure ulcers, especially as a secondary diagnosis. In Fig. 3 and 4, the occurrence of documented diagnoses related to non-healing wounds according to the sex and age of patients is depicted. In the total number of hospital stays in which the monitored diagnoses were either primary or secondary diagnoses, the number of male patients is higher. It is apparent that the diagnoses of varicose veins of lower extremities with ulcer and inflammation (I83.0, I83.2), decubitus ulcer (L89) and ulcer of lower limb (L97) occur more often in women, and also that the average age of these patients increases. The average age of patients with the monitored diagnoses is 66 (± 13) years for all patients; for women, it is 64 (± 13) years and for men 70 (± 15) years in the case of the primary diagnosis. In the case of secondary diagnosis, the overall average age is higher at 70 (± 13) years. It is also higher for women at 74 (± 13) years but lower for men at 68 (± 12) years.



This corresponds to the well-known fact that non-healing wounds and especiallylower leg ulcers and pressure ulcers are more common in the so-called vulnerable (fragile) groups of patients, including the elderly patients, patients with stroke, diabetes, dementia and immobile patients or patients with impaired mobility [10 – 12]. In their study, Wicke et al. [13] also stated that the dramatic increase of the ageing population related to the demographic trend will lead to an increase in the number of patients with non-healing wounds, because the wound healing process is negatively influenced by age.
The place of providing care during hospitalization in relation to the type of the reported diagnosis
The majority of patients with a reported monitored diagnosis are hospitalized in acute-care departments of hospitals which are not university hospitals. Of the total of 35,824 hospital stays per year, the monitored diagnosis was reported as the primary diagnosis in university hospitals in 22% of cases, 73% of cases were in other hospitals providing acute care, 4% in hospitals for long-term and terminally ill patients (hereinafter LTC except for home care services) and 2% in other healthcare facilities. As regards the monitored diagnoses reported as secondary diagnoses (34,785 per year), the ratio of hospital stays in various facilities is as follows: university hospitals 18%, other hospitals providing acute care 72%, LTC 6% and other healthcare facilities 2%. If different specializations in healthcare are considered, the most hospital stays are reported in surgical departments (56% as the primary diagnosis and 23% as a secondary diagnosis). Internal medicine departments have the second highest number of patients with the monitored diagnoses, although the diagnoses associated with a wound are mostly stated as secondary (34.2% compared to 18.7% of primary diagnoses). The third in this order are departments of nursing care (primary diagnosis 9.2%, secondary diagnosis 12.7%). This order of departments also corresponds to the occurrence of the most types of monitored diagnoses. The exceptions are the diagnoses varicose veins of lower extremities with ulcer and inflammation (I83.0, I83.2) and ulcer of lower limb, not elsewhere classified (L97), which are most commonly reported by the departments of dermatovenerology as the primary diagnosis (53.1% for I83.0, I83.2 and 54.9% for L97) and by internal medicine departments as a secondary diagnosis (15.4% for I83.0, I83.2 and 18.5% for L97).
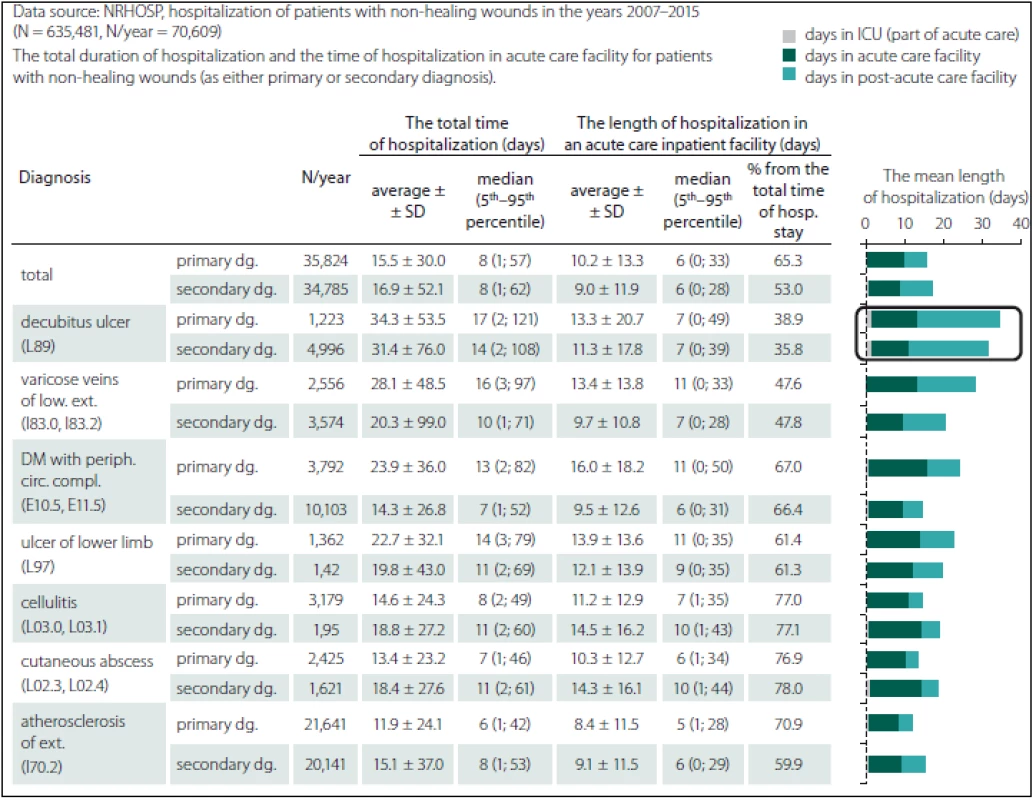
Length of hospitalization of patients with the monitored diagnosis related to the occurrence of non-healing wounds
The average length of hospitalization of all hospital stays and its analysis according to the various diagnoses is summarized in Tab. 1. The longest hospital stays are reported in patients with pressure ulcers, even though it is one of the least often-recorded diagnoses from the monitored set. It was also confirmed that patients with pressure ulcers spend the highest number of days in post-acute care beds. The fact that hospitalization of patients with pressure ulcer is twice as long in post-acute care than in acute care was confirmed in another study analysing data from NRHOSP with a particular focus on the patients with neurological diagnosis [10]. Also, other sources state that pressure ulcers are considered to be a possible cause of prolonged hospitalization [14 – 16], which again is related to higher costs of care.
The most common comorbidities in patients with the monitored diagnosis related to the occurrence of non-healing wounds
Due to their significantly slowed-down process of healing, chronic wounds have a great impact on the health and quality of life of both patients and their families. They cause pain and loss of function and mobility, and lead to development of psychological problems (depression, fear and anxiety), social isolation, financial burden, prolonged time of hospital stay and chronic comorbidity or even death [8,9,16]. The most common comorbidities for all hospital stays regardless of the type of reported diagnoses and whether it is the primary or secondary diagnosis are diseases of the circulatory system, endocrine diseases, diseases of nutrition and metabolism, and certain infectious and parasitic diseases. Understanding the extent of various causes, categories and types of complications in patients with chronic wounds should help to focus on those groups of patients who will benefit from medical interventions, timely screenings, prevention and treatment [18].
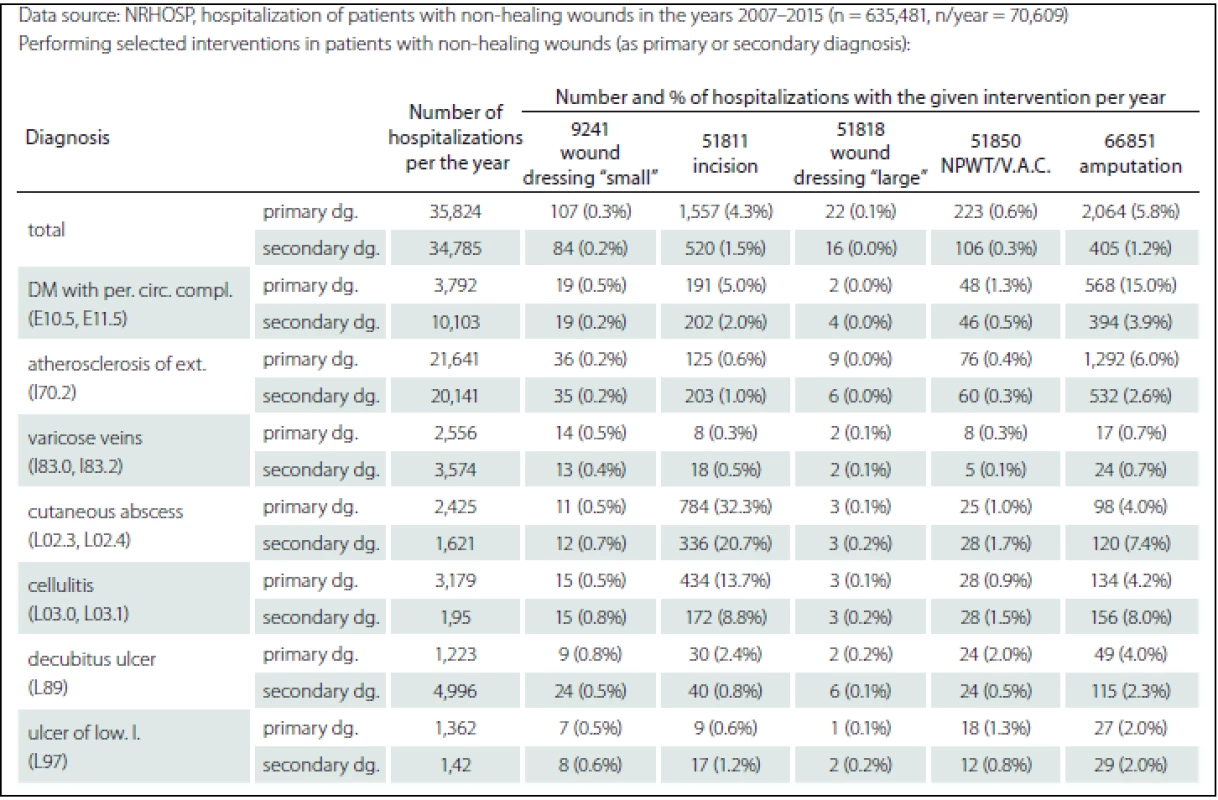
Medical interventions provided to patients with the monitored diagnosis related to the occurrence of non-healing wounds
The most commonly reported medical intervention during hospitalization varied according to the type of the hospitalisation diagnosis. Surgical interventions were more frequent in hospital stays due to type 1 and 2 diabetes mellitus with peripheral circulatory complications (E10.5, E11.5), decubitus ulcer and pressure area (L89), cellulitis of finger and toe and other parts of limb (L02.3, L02.4). Conservative treatment was reported in hospital stays due to diagnoses of varicose veins of lower extremities with ulcer and inflammation (I83.0, I83.2) and ulcer of lower limb, not elsewhere classified (L97) (Tab. 2). The majority of non-healing wounds can be treated conservatively unless an extensive debridement must be performed or unless the patient is in serious condition when an intervention of varying degree and surgical therapeutic intervention are necessary [3,17]. In the Czech Republic, the process of treating non-healing wounds is not regulated by nationally accepted recommended procedures and interventions. Instead, the treatment provided is mostly based on the traditional approach of the given healthcare provider. The situation is made no easier by the fact that therapy is performed using separately charged medical devices, and materials for the so-called moist wound healing and this type of treatment is not usually reported [10]. The costs for the care provided are often paid from the financial resources of the given department or partly by the patient. In the Czech Republic, studies focused on the cost-effectiveness of prevention and treatment of non-healing wounds are still lacking.
The way of ending a hospital stay and rehospitalizations of patients with the monitored diagnosis related to the occurrence of non-healing wounds
Non-healing wounds are a common symptom, or a causal consequence of chronic illness and co-morbidity and are also very frequently the cause of readmission and rehospitalization [6]. Similar conclusions can be drawn from the data we analysed (Fig. 5). Most of the monitored hospitalizations ended by discharging the patient to home care in their natural social environment (81% of hospitalizations with primary monitored diagnosis and 71% secondary monitored diagnosis per year). Transfer of the patient to a different facility was recorded in 12% of cases (n = 4,289) with the main monitored diagnosis and in 15% of cases (n = 5,139) with secondary monitored diagnosis. Most patients (55% in case of primary diagnosis and 50% in case of secondary diagnosis) are transferred to acute-care facilities. Transfer to a facility with follow-up and long-term care is documented in 29% of patients with primary monitored diagnosis and 37% with secondary diagnosis related to the occurrence of the wound. If the diagnosis related to the wound is secondary, in which case we can assumed that it may be a complication of the state described by the primary diagnosis or a result of an exacerbation of the primary disease, then transfer of the patient is more common. In 16% and 14% of primary and secondary diagnoses related to wounds, resp., no records of the location of transfer were found. Death ended hospitalization in 5% of cases with primary monitored diagnosis and in 10% of cases with secondary diagnosis related to the occurrence of non-healing wounds. Based on a more detailed analysis depicted in Fig. 5, it is apparent that the highest percentage of readmissions and rehospitalizations occur in the diagnosis type 1 and 2 diabetes mellitus with peripheral circulatory complications (E10.5, E11.5), while second place is held by the diagnosis decubitus ulcer (L89) and the third position is shared by atherosclerosis of arteries in extremities I70.2 and ulcer of lower limb, not elsewhere classified (L97). Compared to other monitored diagnoses, deaths are most frequently reported for decubitus ulcers. Deaths during hospitalization due to decubitus ulcers (according to the reported cause of death) were found in 19 patients with L89 as the primary diagnosis per year (1.5%) and 24 (0.5%) deaths during hospitalization per year with the L89 as the secondary diagnosis. As Lozano et al. state, death may be a direct result of decubitus ulcers; the real global mortality attributed to decubitus ulcers increased in 2000 – 2016 to 32.7% [18].

If a different cause of death was reported across the whole monitored set, it was most commonly chronic ischemic heart disease (I25) regardless of the type of the primary monitored diagnosis associated with occurrence of wounds. An exception consists of records of deaths during hospitalization with the diagnosis type 1 and 2 diabetes mellitus with peripheral circulatory complications (E10.5, E11.5), in which the reported cause of death was type 1 and 2 diabetes mellitus (E10, E11).
Conclusion
As shown by the analysis of hospital stays, data frdom routinely reported information in the registers of the National Health Information System may be used for comparing records on the occurrence of diagnoses associated with nn-healing wounds. The main limitation of the analysis, however, is that from the retrospective data it is impossible to gain information on the time of formation of the skin and tissue dage and on the number of ulcers. Most of the hospitalization records with monitored diagnosis associated with occurrence of wounds are reported by hospitals providing acute care, mainly in surgical departments and departments of internal medicine (exceptions are varicose veins of lower extremities with ulcer and inflammation – I83.0, I83.2, and ulcer of a lower limb, not elsewhere classified – L97 which are most commonly reported by dermatovenerologic departments and where treatment is conservative). The most common comorbidities in hospitalizations with the monitored diagnoses are diseases of the circulatory system, endocrine diseases, diseases of nutrition and metabolism and certain infectious and parasitic diseases. In cases where the monitored diagnosis associated with wounds is secondary during a hospitalization, the most common comorbidities are neoplasms, and diseases of the digestive and genitourinary systems. More than half of the hospitalizations for the monitored diagnoses ended by transfer to an acute-care facility (55% if reported as a primary diagnosis, 50% as a secondary diagnosis). Regardless of the type of healthcare facility in which the hospitalization for the monitored diagnosis took place, most patients are discharged to home care (exceptions are LTC – hospitals for long-term and terminally ill patients, post-acute care and hospice). When patients with different types of non-healing wounds die during hospitalization, another diagnosis is usually reported as the main cause of death (most commonly chronic ischemic heart disease – I25 and atherosclerosis of arteries of extremities – I70). The analysed data also show that hospitalization is prolonged in cases where the monitored diagnosis is reported as a secondary one. Moreover, hospitalizations associated with occurrence of wounds are commonly ended by a transfer to acute or post-acute care. The presented study is the first to summarize information on hospitalizations due to a diagnosis related to non-healing wounds on a national level in the period 2007 – 2015 in the Czech Republic.
This study was supported by the Ministry of Health of the Czech Republic, grant 15-29111A with the title “The register of decubitus ulcers – integration strategy for monitoring and preventive interventions on the national level”. All rights reserved.
The authors declare they have no potential conflicts of interest concerning drugs, products, or services used in the study.
The Editorial Board declares that the manuscript met the ICMJE “uniform requirements” for biomedical papers.
Accepted for review: 23. 6. 2017
Accepted for print: 3. 7. 2017
Assoc. Prof. Dr. Andrea Pokorna, Ph.D.
Department of Nursing
Faculty of Medicine
Masaryk University
Kamenice 5,
625 00 Brno
e-mail: apokorna@med.muni.cz
Sources
1. Kirsner RS. The Wound Healing Society chronic wound ulcer healing guidelines update of the 2006 guidelines – blending old with new. Wound Repair Regen 2016;24(1):110 – 1. doi: 10.1111/ wrr.12393.
2. Lazarus GS, Cooper DM, Knighton DR, et al. Definitions and guidelines for assessment of wounds and evaluation of healing. Wound Repair Regen 1994;2(3):165 – 70.
3. Werdin F, Tennenhaus M, Schaller HE, et al. Evidence-based management strategies for treatment of chronic wounds. Eplasty 2009;4(9):e19.
4. Cazander G, Pritchard DI, Nigam Y, et al. Multiple actions of Lucilia sericata larvae in hard-to-heal wounds. Bioessays 2013; 35(12):1083 – 92. doi: 10.1002/ bies.201300071.
5. Graves N, Zheng H. The prevalence and incidence of chronic wounds: a literature review. Wound Practice Research 2014;22(1):4 – 19.
6. Sen CK, Gordillo GM, Roy S, et al. Human skin wounds: a major and snowballing threat to public health and the economy. Wound Repair Regen 2009;17(6):763 – 71. doi: 10.1111/ j.1524-475X.2009.00543.x.
7. Heyer K, Augustin M, Protz K, et al. Effectiveness of advanced versus conventional wound dressings on healing of chronic wounds: systematic review and meta-analysis. Dermatology 2013;226(2):172 – 84. doi: 10.1159/ 000348331.
8. Denny K, Lawand C, Perry SD. Compromised wounds in Canada. Healthc Q 2014;17(1):7 – 10.
9. Heyer K, Herberger K, Protz K, et al. Epidemiology of chronic wounds in Germany: analysis of statutory health insurance data. Wound Repair Regen 2016;24(2):434 – 42. doi: 10.1111/ wrr.12387.
10. Pokorná A, Benešová K, Mužík J, et al. Sledování dekubitálních lézí u pacientů s neurologickým onemocněním – analýza Národního registru hospitalizovaných. Cesk Slov Neurol N 2016;79/112(Suppl 1):S8 – 14. doi: 10.14735/ amcsnn2016S8.
11. Jenkins ML, O‘Neal E. Pressure ulcer prevalence and incidence in acute care. Adv Skin Wound Care 2010;23(12):556 – 9. doi: 10.1097/ 01.ASW.0000391184.438 45.c1.
12. Coomer NM, McCall NT. Examination of the accuracy of coding hospital-acquired pressure ulcer stages. Medicare Medicaid Res Rev 2013;3(4). pii: mmrr.003.04.b03. doi: 10.5600/ mmrr.003.04.b03.
13. Wicke C, Bachinger A, Coerper S, et al. Aging influences wound healing in patients with chronic lower extremity wounds treated in a specialized Wound CareCenter. Wound Repair Regen 2009;17(1):25 – 33. doi: 10.1111/ j.1524-475X.2008.00438.x.
14. European Pressure Ulcer Advisory Panel and National Pressure Ulcer Advisory Panel. Treatment of pressure ulcers: Quick Reference Guide. Washington DC: National Pressure Ulcer Advisory Panel 2009.
15. National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers: Quick Reference Guide. Emily Haesler, ed. Cambridge Media: Osborne Park, Western Australia; 2014.
16. Margolis D. Epidemiology of wounds. In: Romanelli M, Shukla V, Mani R, eds. Measurements in Wound Healing. London: Springer 2013 : 145 – 53.
17. Järbrink K, Ni G, Sönnergren H, et al. Prevalence and incidence of chronic wounds and related complications: a protocol for a systematic review. Syst Rev 2016;5(1):152. doi: 10.1186/ s13643-016-0329-y.
18. Lozano R, Naghav M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380(9859):2095 – 128. doi: 10.1016/ S0140-6736(12) 61728-0.
Labels
Paediatric neurology Neurosurgery NeurologyArticle was published in
Czech and Slovak Neurology and Neurosurgery

2017 Issue Supplementum 1
- Advances in the Treatment of Myasthenia Gravis on the Horizon
- Memantine Eases Daily Life for Patients and Caregivers
- Memantine in Dementia Therapy – Current Findings and Possible Future Applications
-
All articles in this issue
- Wound Healing – Cost-effectiveness Data from the Providers and Payers Viewpoint
- Employment of Flap Surgery in Pressure Ulcers Surgical Treatment
- The Pressure Ulcers Evidence in Patients with Spinal Cord Injury at Spinal Unit of Department of Traumatology at University Hospital Brno 2013– 2016
- The Skin Lesions as a Complications of Parkinson’s Disease
- Validaton of Nursing Diagnosis of Acute and Chronic Pain According to NANDA International in the Patients with Wound
- Pressure Ulcers Represents a Constant Nightmare for Me
- Deformation is a Cell “Killer” – Implications for Protecting Persons with a Spinal Cord Injury from Pressure Ulcers
- The Relationship between Risk Factors, Risk Assessment, and the Pathology of Pressure Ulcer Development
- Differential Diagnosis in Pressure Ulcers and Medical Devices
- Possibilities of Evaluation of Psychometric Properties of Scales for Assessment of the Risk of Pressure Lesions at Selected Intensive Care Workplaces – a Pilot Study
- Editorial
- Data Sources for Monitoring of Non-healing Wounds in a National Health Information System – Epidemiology of Non-healing Wounds – Analysis of the National Register of Hospitalized Patients in 2007– 2015
- Czech and Slovak Neurology and Neurosurgery
- Journal archive
- Current issue
- About the journal
Most read in this issue
- Validaton of Nursing Diagnosis of Acute and Chronic Pain According to NANDA International in the Patients with Wound
- Employment of Flap Surgery in Pressure Ulcers Surgical Treatment
- Differential Diagnosis in Pressure Ulcers and Medical Devices
- Pressure Ulcers Represents a Constant Nightmare for Me
