Methods of improving the quality of life in patients with stable maculopathy-pilot results of a new study
Authors:
J. Nekolová 1; J. Kremláček 2; M. Kuba 2; M. Středová 1; D. Morávková 3; K. Drtílková 3; N. Jirásková 1
Authors‘ workplace:
Oční klinika, Fakultní nemocnice Hradec Králové, přednostka: prof. MUDr. Naďa Jirásková, Ph. D., FEBO
1; Ústav patologické fyziologie, Lékařská fakulta v Hradci Králové, přednosta: prof. MUDr. Miroslav Kuba, CSc.
2; Tyfloservis o. p. s., pobočka Hradec Králové, vedoucí: Mgr. et Mgr. Daniela Morávková
3
Published in:
Čes. a slov. Oftal., 75, 2019, No. 3, p. 130-135
Category:
Original Article
doi:
https://doi.org/10.31348/2019/3/3
Overview
Purpose: To present pilot results of the project in which the primary goal is to optimize way how to increase the quality of life of patients with the stable maculopathy by implanting intraocular Scharioth macular lens (SML) and modulating visual plasticity by a transcranial electrical stimulation (tES) together with a visual rehabilitation.
Materials and Methods: The study will include 20 patients with stable maculopathy (mainly age-related macular degeneration - AMD) who underwent cataract surgery in past and are eligible for SML implantation. The duration of the project is 3 years. During the first year of the project 17 patients were screened, SML implantation was recommended to 4 of them. They met the indication criteria of SML implantation and SML was implanted into the better seeing eye. The third postoperative day, the tES sessions started and were applied 20 times in the first month after SML implantation. The stimulation was delivered in double blind design (a stimulated and a shame group). Visual exercises and rehabilitation took place during the tES. The patients were examined ophthalmologically and also using electrophysiological methods.
Results: Before the implantation, the best corrected distance visual acuity was 0.23. At near it was Jaeger number 15 uncorrected, with +3.0 sphere dioptres J.No.10.5 and with +6.0 sph dpt J.No. 4.5. After the surgery and visual rehabilitation BCVA was 0.13 after 3 weeks, 0.2 after 2 months and 0.14 after 6 months. At near it was uncorrected J.No.7.5 after 3 weeks, J.No.7 after 2 months and J.No.5 after 6 months.
Conclusion: According to a few participants, the impact of SML implantation together with intensive visual rehabilitation on vision at near and on satisfaction of patients with AMD could not be significantly established. Nevertherless, these patients are limited in their daily activities and SML is one of the solutions for them. The project is ongoing and blinded still, there is also a need of more participants to assess the effect of tES on vision, the results will be presented. We have proven the safety of methods used in the project.
Keywords:
maculopathy – Scharioth macula lens – transcranial electrical stimulation
INTRODUCTION
Patients with stable maculopathy are often very limited in their everyday activities as a consequence of the pathology, in which a large restriction is mainly their inability to distinguish details and the inability to read ordinary text. The aim of this paper is to present the pilot results of a study focusing on improving the quality of life in patients with stable maculopathy by means of implanting an intraocular macular lens, visual rehabilitation and modulation of visual plasticity by means of transcranial electrical stimulation (tES).
The most frequent causes of maculopathy include dry and wet form age-related macular degeneration (ARMD), myopic maculopathy, diabetic maculopathy and hereditary macular dystrophy. For patients with stable forms of macular pathologies, a Scharioth macular lens (SML) is designated (9). This is a bifocal intraocular lens which functions as a magnifying glass in the eye and thus enables patients to see close up without external optic or other aids. It provides approximately twofold magnification, and thereby apparent enlargement of the image. It is inserted into the better seeing artephakic eye as an “add-on” intraocular lens, the haptics of which are inserted into the cartridge. The basis of the success is above all correct indication and motivation of the patient for subsequent rehabilitation (7).
Visual rehabilitation is based on repeated training of visual skills such as localisation, fixation, scanning and tracing of an object and improvement of reading speed (5, 10). Reading with an SML has its own specifics. It is necessary to maintain a shorter reading distance, on average around 15 cm of the eye from the text, and upon reading sufficient lighting is necessary in order to ensure miosis and improvement of contrast. Patients may have difficulties with focusing on details directly in the area of the enlarging surface of the SML.
Transcranial electrical stimulation is used for modulation of brain activity by a weak electric current, and thanks to changes in excitability in the cortical regions it supports “associative plasticity”. It serves for accelerating visual rehabilitation, in which positive experiences have been recorded e.g. in patients with hemianopsia (1, 4) or in laboratory animals (8).
METHOD
Over the course of 3 years, the study will include 20 patients aged over 54 years with stable maculopathy, who have already undergone cataract surgery and have a posterior chamber intraocular lens implanted in the sac. All must meet the indication criteria for implantation of an SML, which corresponds to visual acuity in the region of central purblindness, thus best corrected visual acuity for distance vision within the range of 0.05-0.4 as a consequence of maculopathy. For inclusion in this study it is necessary to meet the fundamental condition of close-up reading, which is improvement on Jaeger charts at least to no. 7, with application of +6.0 spherical dioptres at a distance of approx. 10-15 cm from the text and improvement by at least 3 sizes of Jaeger text in comparison with close-up vision with standard addition of +3.0 sph. Suitable candidates must not have any of the contraindications for implantation of an SML – see table 1. With regard to tES, patients who in the past have suffered a head trauma with unconsciousness, who have or have had epilepsy or other paroxysmal disorders, who have a metal implant in the brain, an implanted cardiac pacemaker or who have suffered from skin diseases on the head or neck are not included in this project.

Implantation of an SML into the cartridge is performed by the standard recommended method. The surgical technique of implantation of a macular lens is not difficult, and is similar to standard cataract surgery. Following artificial dilation of the pupil and topical anaesthesia, a corneal incision is made by no 12 of the size of 2.2 millimetres, and service paracenteses are made according to the customs of the surgeon. The anterior chamber is filled with viscoelastic material, and the macular lens is placed in the cartridge. In this phase the surgeon must take care to ensure the correct insertion of the haptics and optics in order to prevent any damage thereto. After the insertion of the macular lens behind the iris, the operating surgeon must insert the haptics correctly into the cartridge and perfectly centre the 1.5 millimetre wide enlargement zone of the macular lens into the axis of vision. In the last steps of the operation, the viscoelastic material is evacuated from the eye and the wound is hydrated. Postoperatively antibiotics and steroids are applied prophylactically as standard intensively in drops for a period of 1 week, and thereafter with reducing frequency until complete discontinuation 1 month after the operation. Intraocular pressure is monitored by measurement on a non-contact tonometer. The patients are carefully opthalmologically monitored also after implantation and during the course of stimulation, and similarly in the following period. Best corrected visual acuity for distance is examined on projection charts and ETDRS tables. Natural and applicable corrected visual acuity for near vision is tested with the aid of Jaeger charts. In addition a detailed examination of the anterior and posterior segment is conducted, including photography and also examination of the centre of the retina by optical coherence tomography (OCT).
Transcranial electrical stimulation is commenced according to the patient's condition on the second or third day after surgery, and in total it is necessary to perform 20 sessions, once per day. Stimulation is performed by specially trained laboratory assistants at the Department of Pathological Physiology at the Faculty of Medicine in Hradec Králové. The procedure is identical to the method described in the study by Antal et al. (2). One half of patients in the study will be simulated by functional tES, the second group will only have electrodes placed without functional stimulation (placebo group). During the course of the 30 minute session, patients will be given the task of reading training texts. The selection of patients is double-blind, neither the laboratory assistants nor the examiner will know whether or not the patients are being stimulated. Within the framework of the monitoring examinations the patients will complete a satisfaction questionnaire, the patients are examined by visually generated sensory and cognitive evoked potentials.
At the same time all patients will be attended to by employees of Tyfloservis, who will ensure visual rehabilitation of the patients on adapted texts.
At the beginning of each 30 minute session, the patients are always tested in their reading skills. A printed text is used for testing, in rows with sufficient contrast of characters against the background, in the size of Jaeger charts no. 7. Within the framework of a single text, patients read 256 characters including spaces. If patients are unable to read this text, they will be offered texts simplified to single syllables or words ranked in size of Jaeger charts no. 14-6.
During the course of the entire session, ideal conditions are created for visual work with the aid of a reading desk which holds the text in an optimal position toward the eyes, and suitable lighting with adjustable light intensity according to the requirements of the individual patients. For each day of tES, one working sheet is prepared within the framework of visual rehabilitation, with exercises for developing visual skills and reading techniques with a Scharioth macular lens. The individual exercises are focused on training seeking and fixation on objects, seeking matches and differences between objects, scanning images, distinguishing figures and background, cultivation of visual awareness and memory, hand-eye co-ordination and work with text. The difficulty of the individual exercises if progressively increased. The main emphasis has been placed on patient comfort during visual work, which should be enjoyable for them and help them familiarise themselves with the new aid. The observation and examination of patients shall last for at least six months from implantation. During this period further adjustments to the reading technique will be made by the Tyfloservis employees directly within the patients' home environment.
Reading speed has been tested as the average time required for reading 10 words of text with a size of Jaeger no. 10. This was tested shortly after implantation and at the end of the period of stimulation of vision.
RESULTS
In the first year of the project the initial examination was undergone by 17 patients, out of whom four entered the study. The 8 patients who met the entrance criteria but decided not to enter the study stated concerns about the time demands of the study (n=6) or fear of surgery (n=2). The remaining five patients did not meet the entrance criteria. One patient had a cardiac pacemaker, which was a contraindication of tES, four patients did not meet the conditions for implantation of an SML. One patient had unstable wet form ARMD, one patient had excessively poor vision, one patient had excessively good vision and one was unsuitable for implantation of an SML due to the presence of severe endotheliopathy. This concerned 10 women and 3 men with an average age of 81 years.
Four patients agreed to the conditions of the study, comprising 3 women and 1 man with an average age of 79 years (73-84 years). All had stable age-related macular degeneration and all were artephakic. They met the indication criteria for entry into the project and had no contraindications. They were motivated and willing to provide long-term co-operation. Preoperatively best corrected visual acuity for distance vision was on average 0.18 in the right eye and 0.19 in the left eye. Visual acuity of the patients for near vision expressed by the value of text size of Jaeger charts was on average Jaeger no. 16 in the right eye naturally, with correction of +3.0 spherical dioptres Jaeger no. 12, and with correction of +6.0 spherical dioptres Jaeger no. 7.5. In the left eye the values for near vision were on average natural Jaeger no. 15.5, with correction of +3.0 dioptres Jaeger no. 12.5 and with correction of +6.0 dioptres Jaeger no. 7. Average preoperative intraocular pressure in the right eye was 13.3 and in the left eye 15.8 millimetres of the mercury column. On OCT of the macula all patients had atrophy of the neuroretina, in which the average values of central retinal thickness were 141.5 micrometres in the right eye and 180.3 micrometers in the left eye. The preoperative values of all patients are expressed in table 2.

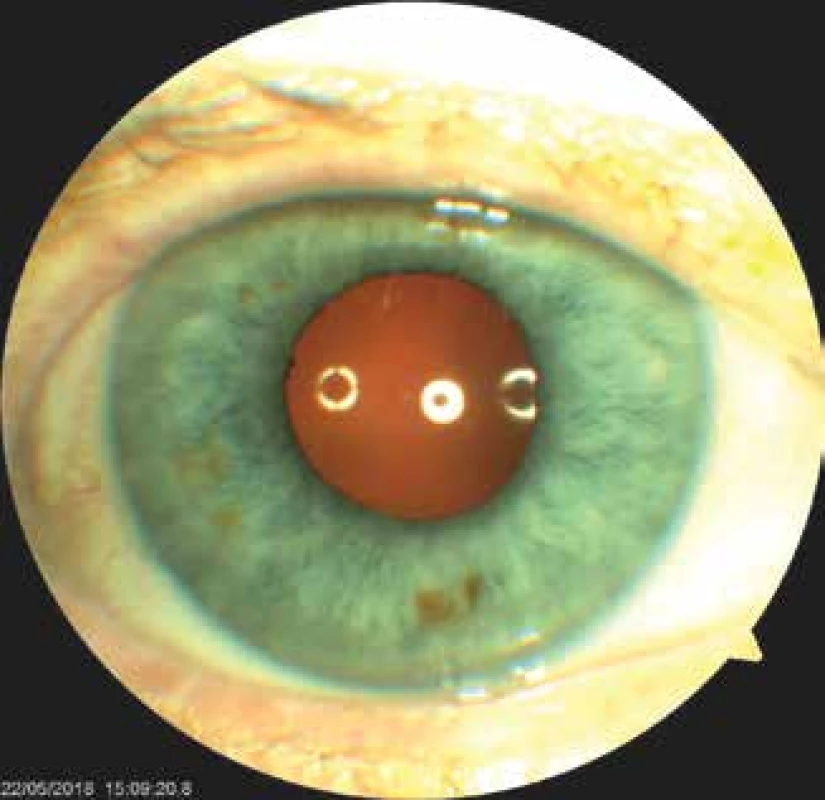
No perioperative or postoperative complications of SML implantation were recorded. Good centration of the SML was achieved in all the patients (Fig. 1).
Postoperatively there was a temporary reduction of corrected distance visual acuity from the average preoperative values of 0.23 (min. 0.13, max. 0.4) to 0.06 on the first postoperative day – values of implanted eye (3x right eye, 1x left eye). After one week visual acuity improved to an average of 0.1 (min. 0.06, max 0.17) and after 3 weeks to 0.13 (min. 0.06, max. 0.25). Two months after implantation of the SML, distance visual acuity was within the range of 0.13 to 0.3 – on average 0.2, and six months after implantation reached values of 0.14.
For near vision the average value of Jaeger charts on the operated eye preoperatively was Jaeger no. 15 naturally, with +3.0 dioptres Jaeger no. 10.5 and with +6.0 dioptres Jaeger no. 4.5. Postoperatively the ability to read naturally improved, on the second day patients attained an average value of Jaeger no. 9 and on the seventh day Jaeger no. 8. By this time reading ability had already improved in comparison with reading with regular correction (+3.0 sph) before implantation and training. After two months, two of the four patients were able to read Jaeger no. 3 naturally, the remaining two patients Jaeger no. 11 and 13. After six months the average size of the text on Jaeger charts was Jaeger no. 5.
In the postoperative period intraocular pressure did not increase in comparison with the preoperative values, and was within the range of 13 to 15 torr. Central retinal thickness (CRT) measured by optical coherence tomography upon entry into the project was on average (min-max) 153 (107-203) micrometres. After two months the CRT values were on average 180 micrometres and after six months 142.5 micrometres. A complete overview of the postoperative results is presented in table 3.

On the third day after implantation of the SML the patients were not able to read the text at the test speed, nevertheless after the first visual rehabilitation reading speed was 23, 60 and 127 seconds, while one patient was unable to read the tested size of the text of Jaeger no. 10 naturally. After one month of intensive visual rehabilitation, reading speed was 8, 13 and 33 seconds, while again one patient was unable to read Jaeger no. 10. Reading speed therefore improved by visual rehabilitation in 3 out of 4 patients.
It has not yet been possible to determine which of the patients underwent active tES stimulation and which did not, since the project is still ongoing and the results shall be presented in future.
DISCUSSION
At present recruitment into the project is taking place for a further 2 years, in which it is planned to include eight patients into the study each year, therefore the study will include a total of 20 purblind patients.
On the basis of our initial experiences, the necessity of the operation itself was shown to be a certain problem, since some patients, often of an advanced age, feared any kind of surgical procedure. A similarly limiting factor was the necessity of daily stimulation of the brain and training for a period of 3 weeks. Patients who so required were provided with residence in an inpatient department throughout the period of stimulation if possible, so that they could attend a stimulation session every day. However, for some of the addressed candidates even this option was not acceptable, since they did not want to leave their home environment for such a long time. Daily commuting for 3 weeks (or more, if stimulation is not provided also at weekends) is a large problem for purblind patients, who are not capable of transporting themselves and must therefore rely on friends and relatives to accompany them. Finances were earmarked for these patients within the framework of the project in order to ensure transport by a specialised firm.
On the other hand, if the patients had decided to enter the project, they reacted very positively to the everyday training and visual stimulation provided by the laboratory assistants and Tyfloservis employees. They appreciated both the improvement of vision itself and the endeavour of the staff to help them return to regular life as before they were afflicted by the pathology.
The set goal of our project is to evaluate whether tES is capable of accelerating or stimulating visual rehabilitation, as described in several studies (1, 2, 8, 6). However, it is not possible to evaluate the effect of this method at the present time, since the study is still currently double-blind. Nevertheless, even despite this it is possible to determine the effect of the actual implantation of an SML together with professionally conducted visual rehabilitation. It is also possible to confirm the safety of the methods used, and that they are well tolerated.
A Scharioth macular lens was implanted in these patients for the purpose of enlarging the observed object in such a manner that the image falls upon the preserved paramacular part of the retina, when the centre of the retina is damaged (3, 7, 9). A fundamental factor is correct indication and education of patients. In the first year of evaluation, 76% of patients who had originally seemed suitable did not pass the indication criteria. From the above it ensues that a Scharioth macular lens is suitable for a relatively narrow section of patients.
Another problem is the progression of the macular pathology itself. Age-related macular pathology is a condition that deteriorates over time. At the time of implantation, it is imperative that none of the patients show signs that would indicate the possibility of worsening as a result of the operation or in the early postoperative period, and therefore must have an entirely “dry” macula. Unfortunately, the available examinations are not yet capable of pointing to the speed of negative development of the pathology over time. As a result, the effect of a Scharioth macular lens need not necessarily be permanent. All patients were informed of this fact.
Upon testing of close-up reading, spherical correction of +3.0 and +6.0 dioptres was used, not as addition, for the reason that the patients were artephakic and therefore none of them wore glasses for distance vision. Again a relatively good accordance of near visual acuity was observed with the application of +6.0 spherical dioptres and subsequent visual acuity after implantation of an SML. Thanks to the operation the patients gained the ability to read a regular text, on average Jaeger no. 7, without the use of further aids, naturally. However, reading is a tiring activity for these patients, and it is necessary to ensure sufficient quality lighting and to shorten the reading distance to an average of 15 centimetres of the text from the eye. Even despite this, reading speed improved after implantation and training. None of the patients regrets taking part in the study and the time spent on training visual abilities. One of the patients even wrote a letter of thanks and another expressed her satisfaction in a video interview with a Tyfloservis employee (https://youtu.be/sGz9Jlfdq2M). Thanks to this positive reception we shall continue further with the study and more detailed results will be published.
The study is entirely unique, and we have found no combination of tES and implantation of SML in the international literature, thus as yet it is not possible to compare our pilot results.
CONCLUSION
With regard to the small number of patients in the cohort, it is not possible to evaluate the effect of implantation of an SML simultaneously with professionally guided visual rehabilitation on sight and patient satisfaction with certainty. These patients were otherwise very limited in their everyday activities as a consequence of the pathology of the centre of the retina, and SML represents the only option for solution. The significance of transcranial electrical stimulation in these patients is the subject of further research, the results of which shall be presented in future. We demonstrated the safety of the methods used.
MUDr. Jana Nekolová, Ph.D.
Oční klinika
Fakultní nemocnice Hradec Králové,
Sokolská 581,
500 05 Hradec Králové
Received: 5. 2. 2019
Accepted: 13. 5. 2019
Available on-line: 19. 10. 2019
Sources
1. Alber, R., Moser, H., Gall, C. et al.: Combined Transcranial Direct Current Stimulation and Vision Restoration Training in Subacute Stroke Rehabilitation: A Pilot Study. PM R, 9; 2017 : 787-794.
2. Antal, A., Alekseichuk, I., Bikson, M. et al.: Low Intensity Transcranial Electric Stimulation: Safety, Ethical, Legal Regulatory and Application Guidelines. Clin Neurophysiol, 128; 2017 : 1774-1809.
3. Grzybowski, A., Wasinska-Borowiec, W., Alio, JL. et al.: Intraocularlenses in age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol, 255; 2017 : 1687-1696.
4. Ko, MH., Han, SH., Park, SH., et al.: Improvement of Visual Scanning after DC Brain Polarization of Parietal Cortex in Stroke Patients with Spatial Neglect. Neurosci Lett, 448; 2008 : 171–4.
5. Kremláček, J., Jirásková, N., Nekolová, J. et al.: Electrophysiological Testing of Visual Function after Mirror Telescope Implantation: A Case Report. Doc Ophthalmol, 133; 2016 : 171–81.
6. Kremláček, J., Kuba, M., Kubová, Z. et al.: Motion-Onset VEPs to Translating, Radial,
Rotating and Spiral Stimuli. Doc Ophthalmol, 109; 2004 : 169–75.
7. Nekolová, J., Rozsíval, P., Šín, M., et al.: Scharioth Macula Lens: A new intraocular implant for low-vision patiens with stabilized maculopathy-first experience. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub, 161; 2017 : 206-209.
8. Rushmore, RJ., DeSimone, C., Valero-Cabré, A.: Multiple Sessions of Transcranial Direct Current Stimulation to the Intact Hemisphere Improves Visual Function after Unilateral Ablation of Visual Cortex. Eur J Neurosci, 38; 2013 : 3799–3807.
9. Scharioth, GB.: New Add-on Intraocular Lens for Patients with Age-Related Macular Degeneration. J Cataract Refract Surg, 41; 2015 : 1559–63.
10. Seiple, W., Grant, P., Szlyk, JP.: Reading Rehabilitation of Individuals with AMD: Relative Effectiveness of Training Approaches. Invest Ophthalmol Vis Sci, 52; 2011 : 2938–44
Labels
OphthalmologyArticle was published in
Czech and Slovak Ophthalmology

2019 Issue 3
-
All articles in this issue
- The use of optical coherence tomography in chiasmal compression
- Selective angiography with the possibility of thrombolysis in patients with central retinal artery occlusion
- Influence of cornea on intraocular pressure measurement by ICARE PRO and ORA
- Methods of improving the quality of life in patients with stable maculopathy-pilot results of a new study
- Ranibizumab for the treatment of choroidal neovascularization due to cause other than age related macular degeneration
- Pupillary abnormalities in childhood – 2 case presentations
- Czech and Slovak Ophthalmology
- Journal archive
- Current issue
- About the journal
Most read in this issue
- Pupillary abnormalities in childhood – 2 case presentations
- Influence of cornea on intraocular pressure measurement by ICARE PRO and ORA
- Ranibizumab for the treatment of choroidal neovascularization due to cause other than age related macular degeneration
- Methods of improving the quality of life in patients with stable maculopathy-pilot results of a new study
