The indications for performing colonoscopy in Iranian children – a cross-sectional study
Indikace pro provádění koloskopie u íránských dětí – průřezová studie
Východiska: Koloskopie je zlatým diagnostickým standardem pro onemocnění tlustého střeva poskytující vynikající pohled na slizniční povrch tlustého střeva a terminálního ilea. Koloskopie u dětí je indikována k diagnostice a léčbě gastrointestinálních onemocnění. V této studii jsme hodnotili důvody pro provádění koloskopie u dětí. Metody: Jednalo se o deskriptivní průřezovou studii zahrnující všechny děti odeslané ke koloskopii na gastroenterologickou kliniku přidruženou k Shiraz University of Medical Sciences. Děti byly vybrány vhodnou metodou vzorkování. Statistická analýza byla provedena v softwaru SPSS 22. Výsledky: Z 389 dětí odeslaných na koloskopii bylo 203 chlapců a 186 dívek. Průměrný věk byl 8,36 ± 4,8 roku. Nejčastějším důvodem pro koloskopii bylo krvácení z konečníku (63,5 %), přičemž nejčastějšími diagnózami byly juvenilní polyp a idiopatický střevní zánět (IBD), z nichž každá tvořila 11,3 % pacientů. Závěry: Nejčastějšími nálezy koloskopie byly polyp, IBD a zánět tlustého střeva a nejčastější symptomy vedoucí ke koloskopii byly krvácení z konečníku, chronický průjem, sledování léčby IBD, podezření na IBD a bolesti břicha. Vysoká prevalence dětských pacientů s těmito příznaky ukazuje na rostoucí význam koloskopie u těchto pacientů.
Klíčová slova:
koloskopie – polypy tlustého střeva – idiopatický střevní zánět – gastrointestinální onemocnění – gastrointestinální krvácení
Authors:
Dehghani M. S. 1; Doosti M. 1; I. Shahramian 2
; Mirzaie H. 2; F. Parooie 2
; Salarzaei M. 2; M. Ataollahi 1
Authors‘ workplace:
Gastroenterohepatology Research Center, Shiraz, Iran
1; Pediatric Gastroenterology and Hepatology Research Center, Zabol University of Medical Sciences, Zabol, Iran
2
Published in:
Gastroent Hepatol 2021; 75(6): 515-518
Category:
doi:
https://doi.org/10.48095/ccgh2021515
Overview
Background: Colonoscopy is the gold standard diagnostic method for colon diseases providing an excellent view of the mucosal surface of the colon and terminal ileum. Colonoscopy in children is indicated for diagnosis and treatment of gastrointestinal diseases. In this study, we evaluated the reasons for performing colonoscopy in children. Methods: This was a descriptive cross-sectional study including all children referred for colonoscopy to the Gastroenterology clinic affiliated with the Shiraz University of Medical Sciences. The children were selected by a convenient sampling method. Statistical analysis was conducted in the SPSS 22 software. Results: From 389 children referred for colonoscopy, 203 were boys and 186 were girls. The mean age was 8.36 ±4.8 years. The most common reason for colonoscopy was rectal bleeding (63.5%) with the most prevalent diagnoses being juvenile polyp and inflammatory bowel disease, each accounting for 11.3% patients. Conclusions: The most common findings of colonoscopy were polyp, IBD and colon inflammation, and the most prevalent symptoms leading to colonoscopy were rectal bleeding, chronic diarrhea, IBD treatment follow-up, suspected IBD and abdominal pain. The high prevalence of pediatric patients presenting with these symptoms indicates the increasing importance of colonoscopy in these patients.
Keywords:
inflammatory bowel disease – colonoscopy – gastrointestinal bleeding – gastrointestinal diseases – colon polyps
Introduction
Introduction of flexible sigmoidoscopy (FS) and colonoscopy greatly developed the gastroenterology science by improving sensitivity and specificity for diagnosis of gastrointestinal disorders including colon cancer [1,2]. Since its introduction in 1970, colonoscopy has been utilized as a diagnostic modality for pediatric colon diseases [3,4]. Colonoscopy is the gold standard for diagnosis of colon disease providing high quality view of the entire colon and ileum [5–7]. It can assist gastroenterologists in the diagnosis of various diseases including colitis (ulcerative, pseudomembranous, acute bacterial, ameboid, collagenous and lymphocytic, enemas etc.) and Crohn’s disease. Colonoscopy can also be used for diagnosis of vascular lesions, hemangiomas, Kaposi sarcoma, colon lymphoma, colon constriction as well as for therapeutic purposes such as stopping colon bleedings, dilatation of colon strictures, decompressing, and polyp removal [8]. In order to perform colonoscopy, the patient’s colon need to be cleansed using specific preparation strategies by administrating oral agents such as polyethylene glycol (PEG) [9,10]. Colonoscopy complications have been noted in 0.4–1.4% of patients [11]. Bleeding after colonoscopy may happen following removal of polyps and due to colon rupture in 0.2–2.5% of cases [12]. Bacteremia may also be seen in 25% of patients undergoing colonoscopy [13,14]. Colonoscopy in children is indicated for both diagnostic and therapeutic purposes in patients with inflammatory bowel disease (IBD), lower gastrointestinal bleeding, chronic diarrhea etc. [15,16]. On the other hand, colonoscopy is contraindicated in patients with a high risk of intestinal perforation, acute peritonitis, coagulopathies, thrombocytopenia, intestinal ischemia, recent surgeries etc. [17,18]. Therefore, colonoscopy imparts an essential role in both diagnosis and treatment of various gastrointestinal diseases in children. There is little information on the causes and indications of colonoscopy in Iranian children. In this study, we aim to describe various indications for performing colonoscopy in children referred to the gastroenterology clinic of the Shiraz University of Medical Sciences as the center most referred to in the south of Iran.
Methods
This was a descriptive retrospective study including children aged <18 years referred to the Gastroenterology clinic of the Nemazee Hospital affiliated with the Shiraz University of Medical Sciences during 2015 until 2017. Overall, 429 children were referred to the clinic during this time, out of which 30 were excluded because of incomplete data. Finally, 389 children were included. The data was collected using a researcher-made questionnaire addressing variables including age at colonoscopy, sex, colonoscopy indication, colonoscopy findings, complications, and final diagnosis. Statistical analyses were performed in IBM SPSS Statistics version 22. Normality of the data was checked by the Kolmogorov-Smirnov test. Independent samples Student’s t test was used for inferential statistics.
Results
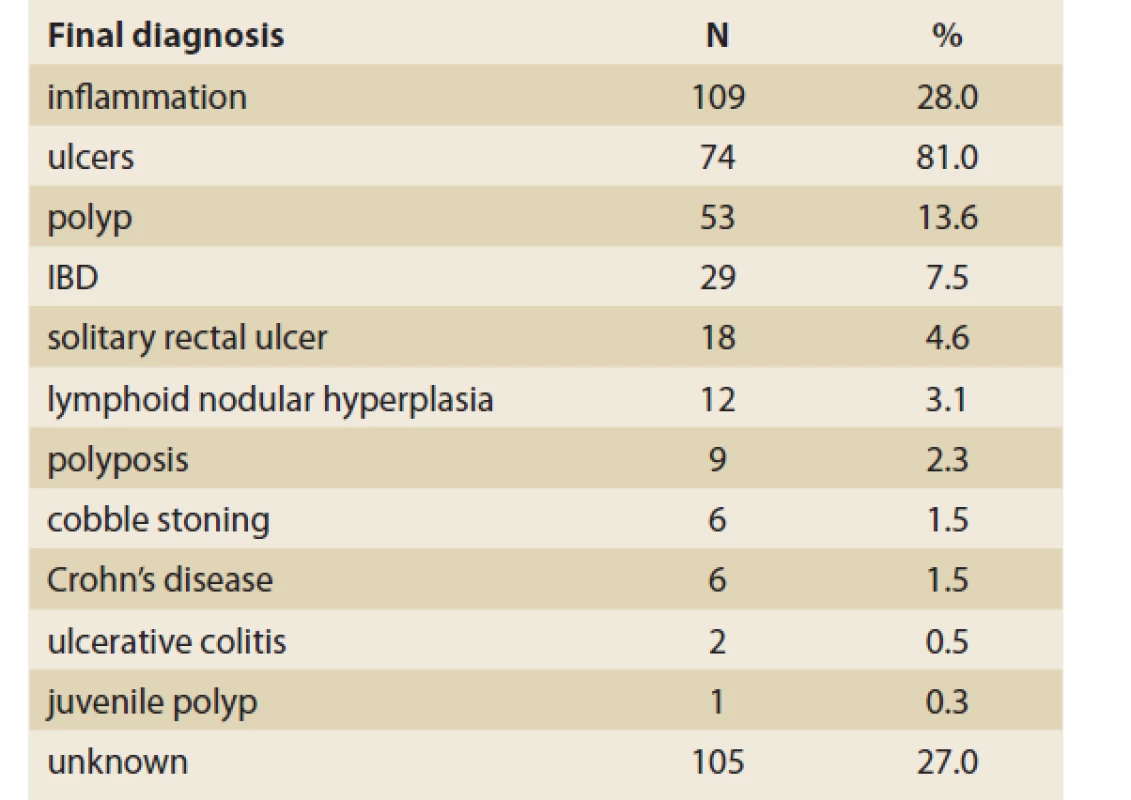
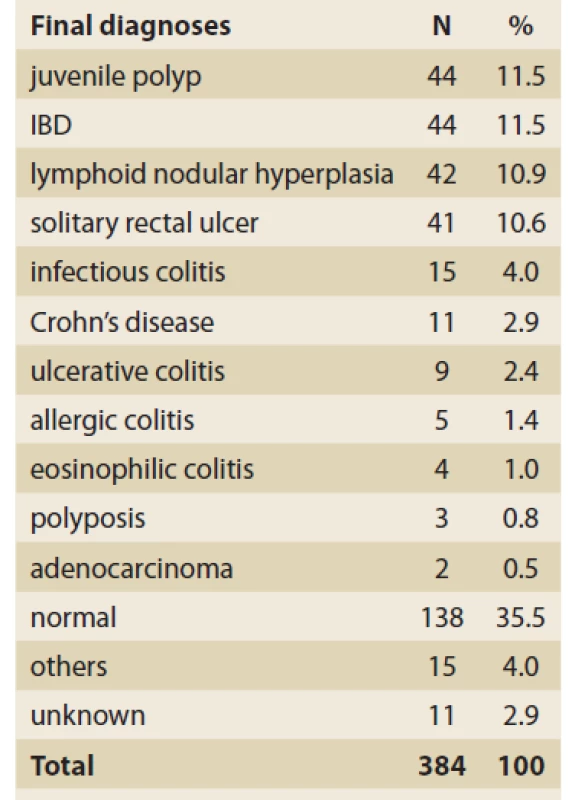
Out of the 389 children who underwent colonoscopy, 203 were male and 186 were female. The mean age of the children was 4.8 ±8.36 years, ranging from 30 days to 18 years old. The most prevalent symptoms leading to colonoscopy were rectal bleeding (63.5%), chronic diarrhea (35%), IBD treatment follow-up (16%), suspected IBD (11.6%) and abdominal pain (2.6%) (Tab. 1). Out of the 389 children, the primary diagnosis was made by colonoscopy in 284. The most frequent endoscopic findings were colon ulcer (81%), polyp (53%), IBD (29%), and colon inflammation (28%) (Tab. 2). The distribution of histologically confirmed diagnoses is shown in Tab. 3. Juvenile polyp (11.3%), IBD (11.3%), lymphoid nodular hyperplasia (10.8%), and solitary rectal ulcer (10.5%) constituted the most frequent etiologies.
Tab. 1. Indikace koloskopie u 389 dětí.
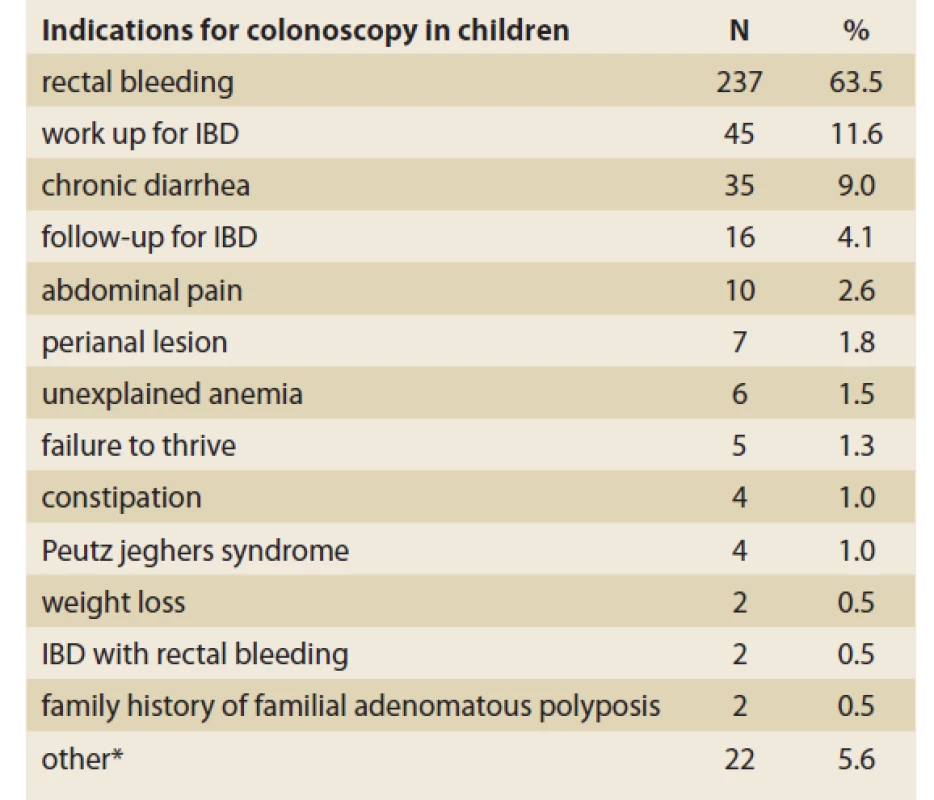
IBD – inflammatory bowel disease
Tab. 2. Endoskopický nález onemocnění tlustého střeva
u 284 dětí.
Tab. 3. Konečné diagnózy na základě
koordinace klinických, koloskopických
a histologických nálezů.
Discussion
In our study, rectal bleeding, suspected IBD, and chronic diarrhea were the most frequent indications for colonoscopy with 63.5%, 11.6%, and 9% prevalence, respectively. In addition, juvenile polyp and IBD constituted the most frequent final diagnoses based on clinical, colonoscopy and histological examinations. In a study on 72 Indian children, rectal bleeding was the most common indication for colonoscopy (83.3%), followed by prolonged colitis (14%), and colon obstruction (2.7%) [19]. Furthermore, juvenile polyp was the most frequent final diagnosis (69.4%) in the mentioned study [19]. In another report from Kuwait, IBD was the most common diagnosis in 151 children who underwent colonoscopy [20]. Furthermore, rectal bleeding (35%) and abdominal pain (27%) were the most frequent reasons for colonoscopy in children in Saudi Arabia (21). In a five-year-long survey on 7,792 colonoscopy procedures in 7,007 children, Thakkar et al reported the most common indications as lower GI bleeding (27.1%), abdominal pain (20.3%), diarrhea (14.2%), and IBD (8.5%) [22]. Similar results were reported by the American National Health Association on 13,115 children treated in 2000–2007 [23]. Likewise, a study on 123 Spanish children revealed that lower GI bleeding was the most common (71%) reason for colonoscopy in this population with rectal polyps and hemorrhagic colitis as the most frequently encountered diagnoses [24]. Consistently, rectal bleeding has been the leading cause for colonoscopy indication in children in other reports ranging from 48 to 97% [18,25–29]. Along with these common causes, other reasons for performing colonoscopy in children have been noted as weight loss, growth retardation, family history of polyps, nausea, abdominal distension, diagnosis of GVHD, and crissum abscess [29–31]. In an Australian report, from 652 colonoscopies performed within 2011–2015, following-up IBD was the most frequent reason (57.9%) for this procedure in children, followed by abdominal pain and rectal bleeding, each with 10.4% prevalence [32]. In previous studies in India [19], Saudi Arabia [21], the United States [22,23], Spain [24], South Korea [18,25], China [27], Taiwan [28], Kuwait [20], and Australia [32,33], IBD was reported as the most common indication for colonoscopy, while in our study IBD was the second rank indication. In other reports from the United States [29] and China [31], abdominal pain was described as the most indicated reason for colonoscopy. In our study, abdominal pain ranked as the 5th indication. It seems that indications for colonoscopy in children around the world are similar; however, the frequencies of these may be different in various geographic locations. In most regions including Iran, gastrointestinal bleeding and IBD work up include the most frequent reasons. The commonest final diagnoses in our study, based on clinical, colonoscopy, and histological examinations, were juvenile polyp and IBD. On the other hand, studies in India [19], China [27,31], South Korea [18], Kuwait [20], Australia [32], and Saudi Arabia [21] reported colitis as the most common final diagnosis. In our study; however, colitis was the 5th most frequent etiology. Overall, juvenile polyp, IBD, and colitis all comprised the most common diagnoses made after colonoscopy in children. Neither of the children assessed here were affected by colonoscopy complications such as bleeding, intestinal rupture, etc. Overall, colonoscopy-related complications may be seen in 1.1% of children undergoing this procedure [22]. Finally, colonoscopy provided a reliable diagnostic procedure for gastrointestinal disorders in children.
Conclusion
The most common findings of colonoscopy were colon ulcer, polyp, IBD, and colon inflammation and the most prevalent symptoms leading to colonoscopy were rectal bleeding, chronic diarrhea, IBD treatment follow-up, suspected IBD and abdominal pain. The high prevalence of pediatric patients presenting with these symptoms indicates the increasing importance of colonoscopy in these patients.
ORCID authors
S. M. Dehghani ORCID 0000-0001-5930-0110,
I. Shahramian ORCID 0000-0002-3760-7717,
H. Mirzaie ORCID 0000-0002-3271-1937,
F. Parooie ORCID 0000-0002-2367-3780,
M. Salarzaei ORCID 0000-0001-5508-8669,
M. Ataollahi ORCID 0000-0003-1876-5266.
Submitted/ Doručeno: 24. 8. 2020
Accepted/ Přijato: 9. 10. 2021
Prof. Iraj Shahramian, MD
Pediatric Gastroenterology and Hepatology
Research Center
Zabol University of Medical Sciences
Shahid Rajaei Street
9861615881 Zabol
Iran
Sources
1. Britto E, Borges AM, Swaroop VS et al. Solitary rectal ulcer syndrome. Dis Colon Rectum 1987; 30 (5): 381–385. doi: 10.1007/BF02555459.
2. Winawer SJ, Zauber AG, Ho MN et al. Prevention of colorectal cancer by colonoscopic polypectomy. N Engl J Med 1993; 329 (27): 1977–1981. doi: 10.1056/NEJM199312303292701.
3. Steffen RM, Wyllie R, Sivak MV Jr et al. Colonoscopy in the pediatric patient. J Pediatr 1989; 115 (4): 507–514. doi: 10.1016/s0022 - 3476 (89) 80272-0.
4. Badiali D, Marcheggiano A, Pallone F et al. Melanosis of the rectum in patients with chronic constipation. Dis Colon Rectum 1985; 28 (4): 241–245. doi: 10.1007/BF02554044.
5. Rex DK, Bond JH, Winawer S et al. Quality in the technical performance of colonoscopy and the continuous quality improvement process for colonoscopy: recommendations of the US Multi-Society Task Force on Colorectal Cancer. Am J Gastroenterol 2002; 97 (6): 1296–1308. doi: 10.1111/j.1572-0241.2002.05812.x.
6. Grassini M, Verna C, Niola P et al. Appropriateness of colonoscopy: diagnostic yield and safety in guidelines. World J Gastroenterol 2007; 13 (12): 1816–1819. doi: 10.3748/wjg.v13.i12.1816.
7. Hassall E, Barclay GN, Ament ME. Colonoscopy in childhood. Pediatrics 1984; 73 (5): 594–599.
8. Cappell MS, Friedel D. The role of sigmoidoscopy and colonoscopy in the diagnosis and management of lower gastrointestinal disorders: endoscopic findings, therapy, and complications. Med Clin North Am 2002; 86 (6): 1253–1288. doi: 10.1016/s0025-7125 (02) 00077-9.
9. Dahshan A, Lin C-H, Peters J et al. A randomized, prospective study to evaluate the efficacy and acceptance of three bowel preparations for colonoscopy in children. Am J Gastroenterol 1999; 94 (12): 3497–3501. doi: 10.1111/j.1572-0241.1999.01613.x.
10. Balsells F, Wyllie R, Kay M et al. Use of conscious sedation for lower and upper gastrointestinal endoscopic examinations in children, adolescents, and young adults: a twelve-year review. Gastrointest Endosc 1997; 45 (5): 375–380. doi: 10.1016/s0016-5107 (97) 70147-0.
11. Jentschura D, Raute M, Winter J et al. Complications in endoscopy of the lower gastrointestinal tract. Surg Endosc 1994; 8 (6): 672–676. doi: 10.1007/BF00678564.
12. Friedt M, Welsch S. An update on pediatric endoscopy. Eur J Med Res 2013; 18 (1): 24. doi: 10.1186/2047-783X-18-24.
13. Hirota WK, Petersen K, Baron TH et al. Guidelines for antibiotic prophylaxis for GI endoscopy. Gastrointest Endosc 2003; 58 (4): 475–482. doi: 10.1067/s0016-5107 (03) 01883-2.
14. Low DE, Shoenut JP, Kennedy JK et al. Prospective assessment of risk of bacteremia with colonoscopy and polypectomy. Dig Dis Sci 1987; 32 (11): 1239–1243. doi: 10.1007/BF01296372.
15. Thomson M. Colonoscopy and enteroscopy. Gastrointest Endosc Clin N Am 2001; 11 (4): 603–639.
16. Gilger MA, Gold BD. Pediatric endoscopy: new information from the PEDS-CORI project. Curr Gastroenterol Rep 2005; 7 (3): 234–239. doi: 10.1007/s11894-005-0040-y.
17. Kay M, Wyllie R. Esophagogastroduodenoscopy, colonoscopy and related techniques. Pediatric Gastrointestinal and Liver Disease: Elsevier Inc. 2006.
18. Park JH. Pediatric colonoscopy: the changing patterns and single institutional experience over a decade. Clin Endosc 2018; 51 (2): 137–141. doi: 10.5946/ce.2018.051.
19. Thapa BR, Mehta S. Diagnostic and therapeutic colonoscopy in children: experience from a pediatric gastroenterology centre in India. Indian Pediatr 1991; 28 (4): 383–389.
20. Kalaoui M, Radhakrishnan S, al Shamali M et al. Findings of colonoscopy in children: experience from Kuwait. J Trop Pediatr 1998; 44 (6): 371–375. doi: 10.1093/tropej/44.6.371.
21. El Mouzan MI, Al-Mofleh IA, Abdullah AM et al. Colonoscopy in children. Saudi J Gastroenterol 2005; 11 (1): 35–39. doi: 10.4103/1319 - 3767.33335.
22. Thakkar K, El-Serag HB, Mattek N et al. Complications of pediatric colonoscopy: a five-year multicenter experience. J Clin Gastroenterol Hepatol 2008; 6 (5): 515–520. doi: 10.1016/j.cgh.2008.01.007.
23. Thakkar K, Alsarraj A, Fong E et al. Prevalence of colorectal polyps in pediatric colonoscopy. Dig Dis Sci 2012; 57 (4): 1050–1055. doi: 10.1007/s10620-011-1972-8.
24. Gana JA, Glenz C, Marchant P et al. Prospective evaluation of the safety and tolerance of colonoscopy in children. Rev Med Chil 2006; 134 (5): 613–622. doi: 10.4067/s0034 - 98872006000500010.
25. Lee BG, Shin SH, Lee YA et al. Juvenile polyp and colonoscopic polypectomy in childhood. Pediatr Gastroenterol Hepatol Nutr 2012; 15 (4): 250–255. doi: 10.5223/pghn.2012.15.4. 250.
26. Okon J, Assi C, Diakité M et al. Pediatric colonoscopy at the University Hospital of Cocody (Ivory Coast). Med Sante Trop 2012; 22 (2): 222–223. doi: 10.1684/mst.2012.0038.
27. Lei P, Gu F, Hong L et al. Pediatric colonoscopy in South china: a 12-year experience in a tertiary center. PLoS One 2014; 9 (4): e95933. doi: 10.1371/journal.pone.0095933.
28. Wu C-T, Chen C-A, Yang Y-J. Characteristics and diagnostic yield of pediatric colonoscopy in Taiwan. Pediatr Neonatol 2015; 56 (5): 334–338. doi: 10.1016/j.pedneo.2015.01.005.
29. Manfredi MA, Jiang H, Borges LF et al. Good agreement between endoscopic findings and biopsy reports supports limited tissue sampling during pediatric colonoscopy. J Pediatr Gastroenterol Nutr 2014; 58 (6): 773–778. doi: 10.1097/MPG.0000000000000317.
30. Tafner E, Tafner P, Mittledorf C et al. Potential of colonoscopy as a treatment for intussusception in children. Endosc Int Open 2017; 5 (11): E1116–E1118. doi: 10.1055/s-0043-117950.
31. Chen J, Yu H, Zhong W et al. Pediatric colonoscopy in South China: a single-center experience from 229 cases. Zhonghua Wei Chang Wai Ke Za Zhi 2017; 20 (12): 1404–1408.
32. Singh H, Withers GD, Ee LC. Quality indicators in pediatric colonoscopy: an Australian tertiary center experience. Scand J Gastroenterol 2017; 52 (12): 1453–1456. doi: 10.1080/00365521.2017.1380224.
33. Singh HK, Ee LC. Recurrent abdominal pain in children: is colonoscopy indicated? J Pediatric Gastroenterol Nutr 2018; 68 (2): 214–217. doi: 10.1097/MPG.0000000000002155.
Labels
Paediatric gastroenterology Gastroenterology and hepatology SurgeryArticle was published in
Gastroenterology and Hepatology

2021 Issue 6
- Possibilities of Using Metamizole in the Treatment of Acute Primary Headaches
- Metamizole at a Glance and in Practice – Effective Non-Opioid Analgesic for All Ages
- Metamizole vs. Tramadol in Postoperative Analgesia
- Spasmolytic Effect of Metamizole
- The Importance of Limosilactobacillus reuteri in Administration to Diabetics with Gingivitis
-
All articles in this issue
- Paediatric gastroenterology and hepatology
- Léčba obezity – aby se bariatricko-metabolická chirurgie nestala obětí vlastního úspěchu
- Azathioprine in the therapy of paediatric inflammatory bowel disease – part I: treatment indications, dosing and thiopurine-related adverse events
- Azathioprine in the therapy of paediatric inflammatory bowel disease – part II: pharmacodynamics, pharmacokinetics, and the possibilities of measuring its metabolites in clinical practice
- Gluten-related immunogenic peptides in stool as means to monitor compliance with gluten-free diet in children with newly diagnosed coeliac disease
- The role of bariatric surgery in patients with type 1 diabetes mellitus
- Diet after bariatric surgery in practice
- Spontaneous intramural duodenal hematoma in a young woman
- Assistance system for real-time polyp detection based on convolutional neural network
- Effect of ursodeoxycholic acid in postcholecystectomy cholestatic hepatopathy verified by ultrasonography
- Biosimilars monoclonal antibodies in the therapy of inflammatory bowel diseases An important milestone in the development of Crohn’s disease and ulcerative colitis therapy, or just a sophisticated generic?
- The selection from international journals
- Idiopatické střevní záněty. Nové trendy a mezioborové souvislosti
- Idiopatické střevní záněty II. Nové trendy a mezioborové souvislosti
- Gastroenterologie a hepatologie v algoritmech
- Prof. MUDr. Petr Dítě, DrSc., slaví 80 let
- Správná odpověď na předchozí kvíz Gastrointestinální stromální tumor
- Kreditovaný autodidaktický test: dětská gastroenterologie a hepatologie / bariatrie a obezitologie
- Janus kinase inhibitor in modern treatment of ulcerative colitis
- Smoking and oncology – offering smokers a scientifically based, less harmful alternative is ethical
- Ružinovský gastroenterologický deň 2021 5. november 2021
- The indications for performing colonoscopy in Iranian children – a cross-sectional study
- Gastroenterology and Hepatology
- Journal archive
- Current issue
- About the journal
Most read in this issue
- Azathioprine in the therapy of paediatric inflammatory bowel disease – part I: treatment indications, dosing and thiopurine-related adverse events
- Diet after bariatric surgery in practice
- Gluten-related immunogenic peptides in stool as means to monitor compliance with gluten-free diet in children with newly diagnosed coeliac disease
- Prof. MUDr. Petr Dítě, DrSc., slaví 80 let
