Biofeedback assisted deep breathing training in refractory disorders of gut-brain interaction – our first experience, impressions and suggestions for further clinical practice
Biofeedback asistovaný tréning hlbokého dýchania pri refraktérnych poruchách interakcie čreva a mozgu – naše prvé skúsenosti, dojmy a návrhy pre ďalšiu klinickú prax
Úvod: Poruchy interakcie čreva a mozgu predstavujú skupinu širokého spektra chronických gastrointestinálnych ochorení s množstvom symptómov súvisiacich s poruchou špecifického orgánu. Neexistuje žiadny špecifický liek na DGBI a terapia je väčšinou zameraná na zmiernenie symptómov. Jednou z potenciálnych nových terapií na zmiernenie symptómov by mohol byť tréning hlbokého dýchania. Dostupné údaje naznačujú, že stimulácia hlbokého dýchania pomocou biofeedbacku môže viesť k zníženiu vnímania bolesti, dokonca aj viscerálnej bolesti pochádzajúcej z gastrointestinálneho traktu. Metódy: Ide o retrospektívnu analýzu klinických údajov získaných od pacientov, ktorí boli liečení nácvikom hlbokého dýchania pre refraktérny prípad ochorenia interakcie čreva a mozgu. DGBI bol diagnostikovaný na základe kritérií ROME IV. Pred tréningom bol pacientom dôkladne vysvetlený správny mechanizmus hlbokého brušného dýchania. Pacienti tiež vyplnili dotazníky STAI-X1, STAI-X2 na posúdenie úrovne ich úzkosti. Po úvodnom tréningu v ordinácii boli pacienti inštruovaní, aby pokračovali v domácom hlbokom brušnom dýchaní 3 - až 5-krát týždenne. Účinok terapie bol hodnotený po jednom mesiaci. Výsledky: Pätnástim vhodným pacientom bol ponúknutý tréning hlbokého dýchania s pomocou biofeedbacku. Deväť pacientov sa dostavilo na kontrolu po 4 týždňoch, a preto sú zohľadnení v analýze. U piatich pacientov došlo k miernemu zmierneniu symptómov. U dvoch pacientov došlo k vymiznutiu symptómov a naopak dvaja pacienti neuviedli žiadnu zmenu symptómov. V úrovniach úzkosti neboli žiadne štatisticky významné zmeny. Záver: Tréning hlbokého dýchania na zmiernenie symptómov pri poruchách interakcie čreva a mozgu sa zdá byť sľubnou reklamou na terapiu. Vyplýva to z publikovaných štúdií a našich vlastných skúseností. Pred jednoznačnejším záverom sú však potrebné prísnejšie údaje.
Klíčová slova:
dyspepsia – globus – biofeedback – IBS – tréning hlbokého dýchania
Authors:
Peter Lipták 1
; I. Tonhajzerová 2
; Martin Ďuriček 1
; Z. Višňovcová 3
; N. Ferencová 3
; Diana Vážanová 1
; P. Bánovčin Jr. 1
Authors‘ workplace:
Clinic of Internal Medicine – Gastroenterology, Jessenius Faculty of Medicine in Martin, Comenius University, University Hospital in Martin
1; Department of Physiology, Jessenius Faculty of Medicine in Martin, Comenius University in Bratislava
2; Biomedical Centre Martin, Jessenius Faculty of Medicine in Martin, Comenius University in Bratislava
3
Published in:
Gastroent Hepatol 2023; 77(4): 289-294
Category:
Clinical and Experimental Gastroenterology: Original Article
doi:
https://doi.org/10.48095/ccgh2023289
Overview
Introduction: Disorders of gut-brain interaction represents a group of a wide variety of chronic gastrointestinal diseases with plethora of symptoms related to disorder of specific organ. There is no specific cure for DGBI and the therapy is mostly focused on alleviating the symptoms. One of the potential new therapies to alleviate the symptoms could be deep breathing training. Available data suggest that biofeedback assisted deep breathing pacing may lead to reduction of pain perception even visceral pain originating from gastrointestinal tract. Methods: This is a retrospective analysis of clinical data obtained from patients who were treated with deep breathing training for refractory case of disease of gut-brain interaction. The DGBI was diagnosed based on the ROME IV criteria. Before the training, the proper mechanism of deep abdominal breathing was thoroughly explained to the patients. Patients have also filled the STAI-X1, STAI-X2 questionaries to assess their anxiety levels. After initial office-based training, the patients were instructed to continue in home-based deep abdominal breathing for 3 to 5 times a week. The effect of the therapy was evaluated after one month. Results: Fifteen eligible patients were offered biofeedback assisted deep breathing training. Nine patients attended the check-up appointment after 4 weeks and are therefore considered in the analysis. Five patients experienced mild alleviation of the symptoms. Two patients experienced resolution of the symptoms and contrary, two patients didn’t report any change in symptoms. There were no statistically significant changes in the anxiety levels. Conclusion: The deep breathing training for symptom alleviation in disorders of gut-brain interaction seems to be a promising ad on therapy. This is based on published studies and our own experience. However more rigorous data are needed before more definite conclusion.
Keywords:
dyspepsia – globus – biofeedback – IBS – deep breathing training
Introduction
Disorders of gut-brain interaction (DGBI) represent a group of a wide variety of chronic gastrointestinal diseases with plethora of symptoms related to disorder of a specific organ [1]. DGBI does not lead to higher mortality but significantly lower the quality of life of patients [2]. Most prevalent DGBI are functional dyspepsia (FD) [3] and irritable bowel syndrome (IBS) [4].There is no specific cure for DGBI and the therapy is mostly focused on alleviating the symptoms. The pit fall of the management of these disorders is that in more severe cases the available therapy is often unsuccessful or brings unsatisfactory results. Therefore, there is a constant research and clinical focus on delivering more potent and promising forms of therapy.
The relationship of autonomic nervous system dysregulation and irritable bowel syndrome [5] and other disorders of gut brain interaction [6] has been described before. One of the methods to influence the autonomic response of the organism is a biofeedback assisted deep breathing training (DBT). Deep breathing stimulates baroreflex and produce heart rate oscillations [7] represented as a heart rate variability (HRV). The baroreflex integrates heart rate, blood pressure and vascular tone control systems and contributes to respiratory sinus arrythmia (RSA) [8]. Biofeedback training in general consists of learning and enhancing motoric skills with augmented feedback on a physiological response [9]. The goal of HRV biofeedback is to increase RSA magnitude and therefore enhance the autonomic homeostasis capacity [10]. Paced breathing at individually specific resonant frequency could produce large oscillations in heart rate, blood pressure, vascular tone and pulse amplitude resulting in synchronization [11]. The relatively widely utilized model for increase of the HRV and RSA proposed by Vaschillo and collegues [11] describes resonance frequency model with paced breathing. This represents resonance frequency of 0.1 Hz which in practice means breathing at frequency of 6 breaths per minute (bpm). As it has been previously published, the resonant oscillations can train autonomic reflexes with the aim to provide therapeutic effect [11].
Available data suggest that biofeedback assisted deep breathing pacing may lead to decrease in blood pressure in patients with arterial hypertension or reduce depression symptoms [12], anxiety [13] and alleviate pain perception [14] even visceral pain originating from gastrointestinal tract [15]. Published data points out that this approach could have a therapeutical role in the management of post-COVID syndrome symptoms [16]. The wide adaptation of various intelligent portable devices and smartphones is opening up opportunities for personalized home assessed biofeedback therapy [17–19]. However, studies focusing on the effect of biofeedback guided deep breathing training on various disease of gut brain diseases are scarce [9,20–23].
Methods
This is a retrospective analysis of clinical data obtained from patients who were treated with deep breathing training for refractory case of disorders of gut-brain interaction (DGBI). In this case, the word “refractory” means that there was no or minimal clinical response to the previous standard treatment. Standard treatment consists of combination of symptomatic medication, specific for the disease (including neuromodulation therapy in some of the cases) and dietary intervention. None of the patients was treated by psychological intervention prior or during the deep breathing training.
All patients considered for this case series analysis were older than 18 years and had no somatic or physiological disease relevant to DGBI symptoms. The DGBI was diagnosed based on the ROME IV criteria [24].
Before the training, the proper mechanism of deep abdominal breathing was thoroughly explained to the patients by attending physician and the procedure was discussed in detail. Patients filled the STAI-X1, STAI-X2 [25] questionnaires in order to assess their anxiety levels. STAI-X1 shows how the patient feel while answering the questionnaire (anxiety as a condition) and STAI-X2 is based on how the patient feel overall (stress as a personality trait).
The initial biofeedback part of deep breathing training was performed using the ProComp Infinity System with BioGraph Infinity Software (Thought technology, Canada). Patients followed the rolling dot on the screen with their breathing and simultaneously had a visual feedback in the breathing curve. The following of the ideal breathing curve was actively supported by the attending physician to secure the smooth uninterrupted breathing cycles. Besides that, the proper mechanism of abdominal breathing was continuously monitored and the patients were told to adjust to the pattern, if it was needed.
The initial visit consisted of 3 training sessions performed over 2 days. Each training session consisted of 5 modules with 2 minutes duration each. The final breathing frequency of 6 breaths per minute was individually reached by slowly adjusting to patient impressions of the breathing. If needed, the inhalation duration, exhalation duration and breath hold duration were slightly adjusted so the patient would be able to follow the breathing pattern with relative comfort.
After the training, the patients were given the inhalation, exhalation and hold intervals which were then set in application in the cellphone. For users of Android operation system, the Paced Breathing© (San Francisco, USA) application was suggested and for iOS operation system Breathing© (New York, USA) application was suggested.
The patient was than instructed to train the deep abdominal breathing for 3 to 5 times a week for one session daily (5 times 2 minutes modules).
After one month of self-training, the patients were invited for a control clinical visit during which the symptom persistence was assessed by simple scale (worsened-slightly worsened-without change-slightly better-better [resolution]). The control STAI-X1, STAI-X2 were also assessed. If needed, the proper breathing method was once again explained to the patients and/or breathing interval patterns were adjusted.
Results
Fifteen patients with various refractory DGBIs were offered biofeedback assisted deep breathing training as a supportive therapy for symptom alleviation after individual consideration by a responsible physician. Twelve patients showed up to the appointment for the initial training.
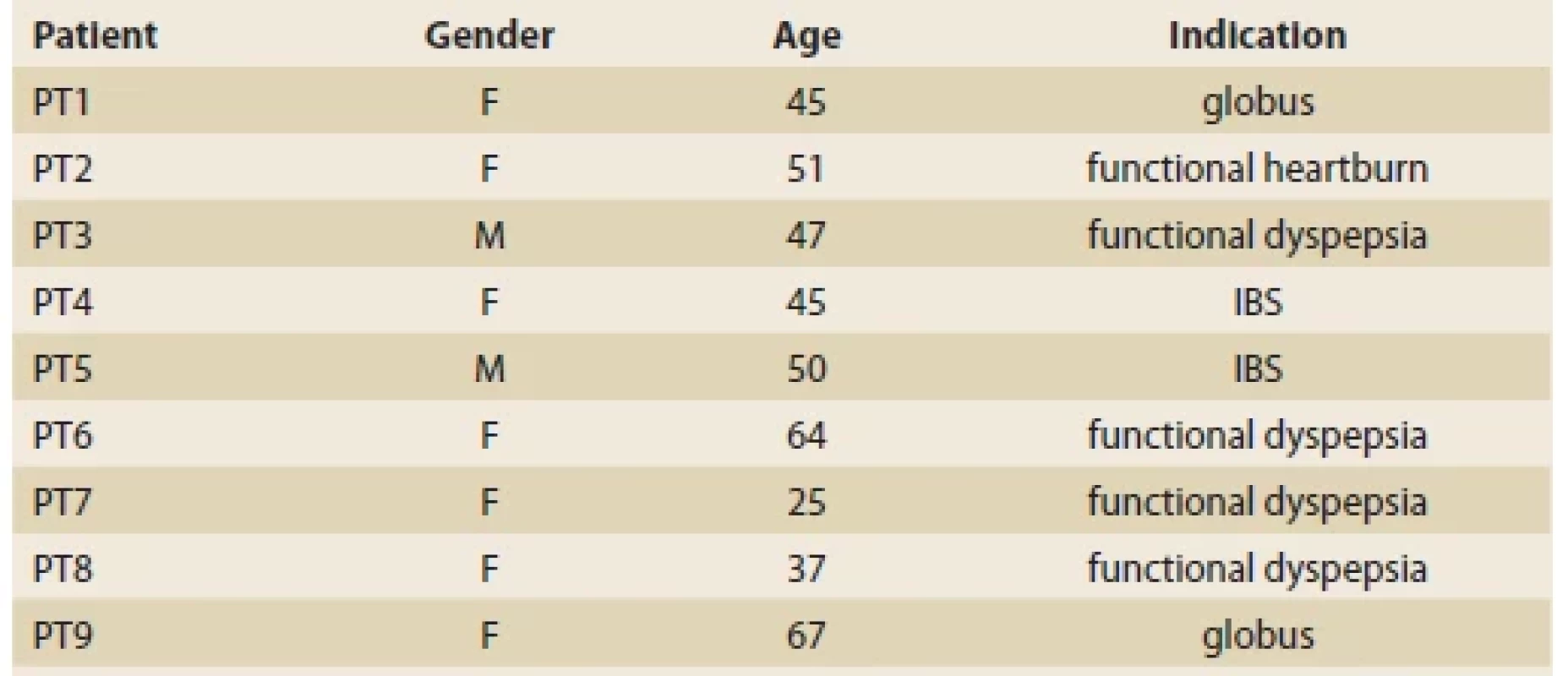
Nine patients attended the check-up appointment after 4 weeks and are therefore included in the analysis. One patient was treated for functional heartburn, two for globus pharyngeus, five for functional dyspepsia and two for irritable bowel syndrome (Tab. 1). The cohort characteristics are marked in Tab. 1.
Tab. 1. Demografi a kohorty a charakterizácia chorôb.
The majority of patients experienced slight alleviation of the symptoms (N = 5). Two patients experienced resolution of the symptoms and contrary, two patients didn’t report any change in symptoms (Tab. 2). One of the patients with complete symptom resolution reported relapse after 6 months while experiencing a stressful life event. This time, the DBT had no effect. The combined average values reported by questionnaires are showing the presence of moderate anxiety before and after the intervention based on STAI-X1 (actual feeling) and change from high anxiety to moderate based on STAI-X2 (as a personal trait perception). However, these changes are not statistically significant.
Tab. 2. Zmena symptómov v analyzovanej kohorte.
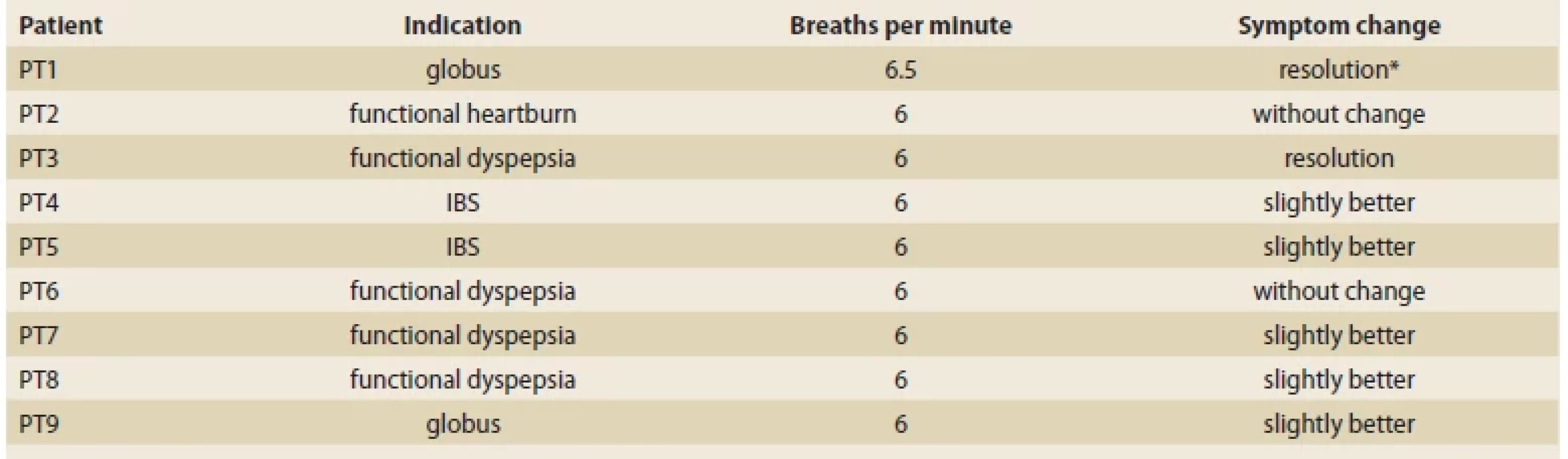
*after initial resolution of the symptoms there was a reported relapse when signifi cant stressful event occurred and the second time the DBT
provide no effect
Discussion
Several authors described various biofeedback nonspecific relaxation techniques for the treatment of irritable bowel syndrome [9,26]. The main point of most of the biofeedback trainings in IBS is to reduce the effect of stress on the organism and thus alleviate the symptoms. Leahy and colleagues developed and used a gut-directed biofeedback computer game which monitored the electrodermal activity and visualized this as stress levels [27]. By implementing the deep relaxation technique, the patients were trying to complete the computer game. As a result, the relaxation maneuver pattern had been memorized. All patients considered for this study have been unresponsive to previous medical treatment. The clinical effect was evaluated after 3 months. Symptom scores were improved in approximately half of the group. Despite promising results, this study did not involve a control group and the patients were not followed for longer period of time. This is an important factor to consider as DGBIs symptoms tend to get worse in response to various external stimuli, therefore some patients are prone to experience slight change of severity of the symptoms over time. As in one of our patients, the initial significant resolution of symptoms was diminished by more stressful life period and the learned deep breathing training had no effect for the second time. It is therefore worth considering long-term observation and ad hoc consultation with a possibility to add on guided training if needed.
Published data suggest that deep slow breathing course over 4 week period could improve the microvascular endothelial function in patients with irritable bowel syndrome [28]. The results of this study further describe that slow deep breathing could improve sympathovagal balance towards parasympathetic overactivity in these patients. But no measurements of anxiety score or quality of life assessment were performed to correlate the possible relation between physiological and psychological effect of DBT in IBS.
Hjelland et al implemented the vagal biofeedback breathing exercise for treatment of functional dyspepsia [22]. They performed a randomized study on 40 patients. The group that received biofeedback trained to achieve 6 breaths/min, 5 min each day for 4 weeks, using specially designed software for vagal biofeedback. The results of this study have shown that regular deep breathing increase the drinking capacity and improve the quality of life in patients with functional dyspepsia, but the vagal basal tone and intragastric volume are not affected.
Another study followed patients with refractory DGBI, more precisely IBS [23]. The aim was to compare deep diaphragmatical breathing biofeedback training to hypnotherapy. Both groups received 3 one-hour long training sessions over the course of 12 weeks. At 24 weeks follow-up, both approaches were equally significantly effective at improving symptom severity score and anxiety ratings. Culminative data from our cohort of refractory DGBI also show improvement in the symptom perception and slightly improved anxiety score although not as significantly as in the mentioned study.
Another group used biofeedback assisted muscle relaxation technique to address the stress factor in etiology of IBS [29]. This was done by randomized open label study with portable device used for monitoring the physical reactions of the patients and to provide feedback part of biofeedback. Patients who received the intervention showed significant decrease in stress perception and depression symptoms compared to controls. The study duration was 8 weeks, with clinical control via telephone every 15 days. Comparing results of the other studies, relatively frequent check-ups in this study seemed to deliver more positive results, which could be useful information while designing further biofeedback protocols.
Although the deep breathing training requires proper guidance, small part of the patients with DGBI use this technique by themselves (without previous training with specialist) in hope to alleviate the symptoms with relatively successful results [30]. One problem with this kind of reports is a strong self-reporting bias and placebo effect in these patients. Also, according to our experience, the majority of patients are not able to perform a proper deep diaphragmatical breathing without professional guidance. And even after several sessions some patients tend to struggle with proper DBT which could be one of the main failure factors of the training.
Another possible factor of lower succession rate in our cohort could be more serious course of the disease. It is reasonable to believe that in patients with milder symptoms of DGBI could DBT be used as an add-on therapeutic modality with more success.
The Cochrane review published in 2019 compared various biofeedback methods in the treatment of irritable bowel syndrome [21]. Biofeedback seems to have positive effect in alleviating the symptoms of the disease and improve the quality of life in these patients. On the other hand, most of the considered studies had small sample size (cumulative number of patients in the review was 300 adult participants) and have heterogenous protocols and methods of intervention. This supports the notion that there is a high probability of biofeedback efficacy in the treatment of IBS but further, more comprehensive, studies are needed. Regarding functional dyspepsia and other diseases of gut brain interactions, no such complex systemic review has been performed to this date.
The important question for further clinical practice is the character of the protocol, mainly the duration and number of sessions per diem. Our current clinical practice is that we suggest patients to train from 3 to 5 times a week, once daily for approximately 15 minutes (5 times 2 minutes interval with several seconds between intervals for more natural pace breathing). Contrary, other published data presents wide variety of protocols [21–23,30], even considering different kinds of deep breathing techniques [31]. There is also a notion that slightly different breathing frequency than established resonant frequency 6 breaths per minute could have a significant clinical effect [32].
To establish the proper protocol more studied with more participants are needed ideally by performing randomized placebo-controlled studies. Another important goal for further clinical research and eventual practice would be the assessment of specific DGBI (e. g., IBS or globus) which would have the highest potential for positive therapy effect.
Conclusion
The deep breathing training for symptom alleviation in disorders of gut-brain interaction seems to be a promising add-on therapy. This is based on current (albeit scarcely) published studies and our own experience. However, more rigorous data, preferably with control group comparison, are needed before more definite conclusion. Our early observation also leads to few points for further clinical practice:
- Long term follow-up is needed to routinely check the adherence and efficacy of the therapy.
- Patients who lack the basic practical skills common in 21st century (comfortable with smartphone applications) should be not considered for the therapy.
- The eligibility for the DBT (the potential to adhere to continuation in home administered self-training) should be thoroughly considered by responsible physician.
- The DBT should be performed by skilled and certified specialist and the approach to the therapy should be personalized based on the actual need and clinical status of the patient.
ORCID authors
P. Lipták ORCID 0000-0001-8257-8567,
I. Tonhajzerová ORCID 0000-0002-1116-6917,
M. Ďuriček ORCID 0000-0002-0754-4532,
Z. Višňovcová ORCID 0000-0003-4538-4645,
N. Ferencová ORCID 0000-0002-3682-404X,
P. Bánovčin ORCID 0000-0001-6694-9364.
Submitted/Doručené: 24. 5. 2023
Accepted/Prijaté: 17. 7. 2023
Peter Lipták, MD, PhD.
Clinic of Internal Medicine – Gastroenterology
University Hospital in Martin
Kollárova 2
036 01 Martin
Conflict of Interest: The authors declare that the article/ manuscript complies with ethical standards, patient anonymity has been respected, and they state that they have no financial, advisory or other commercial interests in relation to the subject matter.
Publication Ethics: This article/ manuscript has not been published or is currently being submitted for another review. The authors agree to publish their name and e-mail in the published article/ manuscript.
Dedication: This publication has been produced with the support of the Integrated Infrastructure Operational Program for the project: Research and development of telemedicine solutions to support the fi ght against the COVID-19 pandemic and to reduce its negative consequences by monitoring human health in order to eliminate the risk of infection in at-risk groups of population, ITMS: 313011ASY8, co-fi nanced by the European Regional Development Fund.
The Editorial Board declares that the manuscript met the ICMJE “uniform requirements” for bio medical papers.
Konflikt záujmov: Autori deklarujú, že text článku zodpovedá etickým štandardom, bola dodržaná anonymita pacientov, a vyhlasujú, že v súvislosti s predmetom článku nemajú fi nančné, poradenské ani iné komerčné záujmy.
Publikačná etika: Príspevok nebol doteraz publikovaný ani nie je v súčasnosti zaslaný do iného časopisu na posúdenie. Autori súhlasia s uverejnením svojho mena a e-mailového kontaktu v publikovanom texte.
Dedikácia: Táto publikácia vznikla s podporou Operačného programu Integrovaná infraštruktúra pre projekt: Výskum a vývoj telemedicínskych riešení na podporu boja proti pandémii covidu-19 a na znižovanie jej negatívnych dôsledkov monitorovaním ľudského zdravia za účelom eliminácie rizika. nákazy v rizikových skupinách obyvateľstva, ITMS: 313011ASY8, spolufi nancované Európskym fondom regionálneho rozvoja.
Redakčná rada potvrdzuje, že rukopis práce splnil ICMJE kritériá pre publikácie zasielané do bio medicínskych časopisov.
Gastroent Hepatol 2023; 77(4): 289 – 294
Sources
1. Drossman DA. Functional Gastrointestinal Disorders: History, Pathophysiology, Clinical Features and Rome IV. Gastroenterology 2016; S0016–5085 (16) 00223-7. doi: 10.1053/j.gastro. 2016.02.032.
2. Sperber AD, Bangdiwala SI, Drossman DA et al. Worldwide Prevalence and Burden of Functional Gastrointestinal Disorders, Results of Rome Foundation Global Study. Gastroenterology 2021; 160 (1): 99.e3–114.e3. doi: 10.1053/ j.gastro.2020.04.014.
3. Aziz I, Palsson OS, Törnblom H et al. Epidemiology, clinical characteristics, and associations for symptom-based Rome IV functional dyspepsia in adults in the USA, Canada, and the UK: a cross-sectional population-based study. Lancet Gastroenterol Hepatol 2018; 3 (4): 252–262. doi: 10.1016/S2468-1253 (18) 30003-7.
4. Oka P, Parr H, Barberio B et al. Global prevalence of irritable bowel syndrome according to Rome III or IV criteria: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol 2020; 5 (10): 908–917. doi: 10.1016/S2468-1253 (20) 30217-X.
5. Polster A, Friberg P, Gunterberg V et al. Heart rate variability characteristics of patients with irritable bowel syndrome and associations with symptoms. Neurogastroenterol Motil 2018; 30 (7): e13320. doi: 10.1111/nmo.13320.
6. Lipták P, Ďuriček M, Prokopič M et al. Autonomic dysregulation in irritable bowel syndrome, functional dyspepsia and globus pharyngeus – a review of literature and pilot results. Gastroent Hepatol 2020; 74 (4): 327–333. doi: 10.14735/amgh2020327.
7. Lehrer PM, Vaschillo EG, Vidali V. Heart Rate and Breathing Are Not Always in Phase During Resonance Frequency Breathing. Appl Psychophysiol Biofeedback 2020; 45 (3): 145–152. doi: 10.1007/s10484-020-09459-y.
8. Shaffer F, Meehan ZM. A Practical Guide to Resonance Frequency Assessment for Heart Rate Variability Biofeedback. Front Neurosci 2020; 14 : 570400. doi: 10.3389/fnins.2020.570400.
9. Chiarioni G, Whitehead WE. The role of biofeedback in the treatment of gastrointestinal disorders. Nat Clin Pract Gastroenterol Hepatol 2008; 5 (7): 371–382. doi: 10.1038/ncpgast hep1150.
10. Vaschillo E, Lehrer P, Rishe N et al. Heart rate variability biofeedback as a method for assessing baroreflex function: a preliminary study of resonance in the cardiovascular system. Appl Psychophysiol Biofeedback 2002; 27 (1): 1–27. doi: 10.1023/a: 1014587304314.
11. Vaschillo EG, Vaschillo B, Lehrer PM. Characteristics of resonance in heart rate variability stimulated by biofeedback. Appl Psychophysiol Biofeedback 2006; 31 (2): 129–142. doi: 10.1007/s10484-006-9009-3.
12. Bartur G, Vatine JJ, Raphaely-Beer N et al. Heart rate autonomic regulation system at rest and during paced breathing among patients with CRPS as compared to age-matched healthy controls. Pain Med 2014; 15 (9): 1569–1574. doi: 10.1111/pme.12449.
13. Alneyadi M, Drissi N, Almeqbaali M et al. Biofeedback-Based Connected Mental Health Interventions for Anxiety: Systematic Literature Review. JMIR Mhealth Uhealth 2021; 9 (4): e26038. doi: 10.2196/26038.
14. Gholamrezaei A, Van Diest I, Aziz Q et al. Controlled breathing and pain: Respiratory rate and inspiratory loading modulate cardiovascular autonomic responses, but not pain. Psychophysiology 2021; 58 (10): e13895. doi: 10.1111/psyp.13895.
15. Gholamrezaei A, Van Diest I, Aziz Q et al. Effect of slow, deep breathing on visceral pain perception and its underlying psychophysiological mechanisms. Neurogastroenterol Motil 2022; 34 (4): e14242. doi: 10.1111/nmo.14242.
16. Corrado J, Halpin S, Preston N et al. HEART rate variability biofeedback for long COVID symptoms (HEARTLOC): protocol for a feasibility study. BMJ Open 2022; 12 (11): e066044. doi: 10.1136/bmjopen-2022-066044.
17. Dillon A, Kelly M, Robertson IH et al. Smartphone Applications Utilizing Biofeedback Can Aid Stress Reduction. Front Psychol 2016; 7 : 832. doi: 10.3389/fpsyg.2016.00832.
18. Parnandi A, Gutierrez-Osuna R. Physiological Modalities for Relaxation Skill Transfer in Biofeedback Games. IEEE J Biomed Health Inform 2017; 21 (2): 361–371. doi: 10.1109/JBHI.2015.2511665.
19. Gummidela VNC, Silva DRDC, Gutierrez-Osuna R. Evaluating the Role of Breathing Guidance on Game-Based Interventions for Relaxation Training. Front Digit Health 2021; 3 : 760268. doi: 10.3389/fdgth.2021.760268.
20. Katherine Jurek M, Seavey H, Guidry M et al. The effects of slow deep breathing on microvascular and autonomic function and symptoms in adults with irritable bowel syndrome: A pilot study. Neurogastroenterol Motil 2022; 34 (5): e14275. doi: 10.1111/nmo.14275.
21. Goldenberg JZ, Brignall M, Hamilton M et al. Biofeedback for treatment of irritable bowel syndrome. Cochrane Database Syst Rev 2019; 2019 (11): CD012530. doi: 10.1002/14651858.CD012530.pub2.
22. Hjelland IE, Svebak S, Berstad A et al. Breathing exercises with vagal biofeedback may benefit patients with functional dyspepsia. Scand J Gastroenterol 2007; 42 (9): 1054–1062. doi: 10.1080/00365520701259208.
23. Dobbin A, Dobbin J, Ross SC et al. Randomised controlled trial of brief intervention with biofeedback and hypnotherapy in patients with refractory irritable bowel syndrome. J R Coll Physicians Edinb 2013; 43 (1): 15–23. doi: 10.4997/JRCPE.2013.104.
24. Schmulson MJ, Drossman DA. What Is New in Rome IV. J Neurogastroenterol Motil 2017; 23 (2): 151–163. doi: 10.5056/jnm16214.
25. Oei TP, Evans L, Crook GM. Utility and validity of the STAI with anxiety disorder patients. Br J Clin Psychol 1990; 29 (4): 429–432. doi: 10.1111/j.2044-8260.1990.tb00906.x.
26. Blanchard EB, Schwarz SP. Adaptation of a multicomponent treatment for irritable bowel syndrome to a small-group format. Biofeedback Self Regul 1987; 12 (1): 63–69. doi: 10.1007/BF01000079.
27. Leahy A, Clayman C, Mason I et al. Computerised biofeedback games: a new method for teaching stress management and its use in irritable bowel syndrome. J R Coll Physicians Lond 1998; 32 (6): 552–556.
28. Jurek KM, Seavey H, Guidry M et al. The effects of slow deep breathing on microvascular and autonomic function and symptoms in adults with irritable bowel syndrome: A pilot study. Neurogastroenterol Motil 2022; 34 (5): e14275. doi: 10.1111/nmo.14275.
29. Exarchopoulou K, Papageorgiou A, Bacopoulou F et al. A Biofeedback-Assisted Stress Management Program for Patients with Irritable Bowel Syndrome: a Randomised Controlled Trial. EMBnet J 2021; 26: e980. doi: 10.14806/ej.26.1.980.
30. Peper E, Mason L, Huey C. Healing Irritable Bowel Syndrome with Diaphragmatic Breathing. Biofeedback 2017; 45 (4): 83–87. doi: 10.5298/1081-5937-45.4.04.
31. Gholamrezaei A, Van Diest I, Aziz Q et al. Psychophysiological responses to various slow, deep breathing techniques. Psychophysiology 2021; 58 (2): e13712. doi: 10.1111/psyp. 13712.
32. Lehrer P. My Life in HRV Biofeedback Research. Appl Psychophysiol Biofeedback 2022; 47 (4): 289–298. doi: 10.1007/s10484-022-09535-5.
Labels
Paediatric gastroenterology Gastroenterology and hepatology SurgeryArticle was published in
Gastroenterology and Hepatology

2023 Issue 4
- Possibilities of Using Metamizole in the Treatment of Acute Primary Headaches
- Metamizole at a Glance and in Practice – Effective Non-Opioid Analgesic for All Ages
- Metamizole vs. Tramadol in Postoperative Analgesia
- Spasmolytic Effect of Metamizole
- The Importance of Limosilactobacillus reuteri in Administration to Diabetics with Gingivitis
-
All articles in this issue
- Clinical and experimental gastroenterology
- Hepatogenous diabetes in liver transplant candidates: prevalence, risk factors and posttransplant outcome – prospective study
- Robotic pancreatic surgery in a high-volume pancreatic cancer surgery center – first experience
- Chest pain as an atypical symptom of acute cholecystitis
- Impact of the COVID-19 pandemic on acute pancreatitis in the Czech Republic – pilot data PANACOTA study (PANcreatitis Acuta in COVid Time Analysis)
- Changing epidemiology of Clostridioides difficile infection – increasing number of community-acquired forms and infections in children
- Why should we and should we not use ChatGPT in gastroenterology?
- EUS guided drainage of gallbladder: own cohort of 66 patients for the period 2016–2022 from the Hospital Jablonec nad Nisou
- Switch from biosimilar infliximab CT-P13 to biosimilar infliximab SB-2 in the long-term maintenance therapy in IBD patients – prospective observational study
- Dosage forms of oral mesalazine and their clinical use
- Subkutánní infliximab – poznatky z praxe a další možnosti využití u pacientů s IBD
- The selection from international journals
- Správná odpověď na předchozí kvíz
- 44. české a slovenské endoskopické dny a Olomouc Live Endoscopy 2023
- Kreditovaný autodidaktický test: Klinická a experimentální gastroenterologie
- Biofeedback assisted deep breathing training in refractory disorders of gut-brain interaction – our first experience, impressions and suggestions for further clinical practice
- 12th Club Symposium on Portal Hypertension April, 14th–15th 2023, Banská Štiavnica
- Gastroenterology and Hepatology
- Journal archive
- Current issue
- About the journal
Most read in this issue
- Changing epidemiology of Clostridioides difficile infection – increasing number of community-acquired forms and infections in children
- Robotic pancreatic surgery in a high-volume pancreatic cancer surgery center – first experience
- EUS guided drainage of gallbladder: own cohort of 66 patients for the period 2016–2022 from the Hospital Jablonec nad Nisou
- Dosage forms of oral mesalazine and their clinical use

