Treatment strategy for ruptured abdominal aortic aneurysms
Léčebná taktika ruptury výdutí břišní aorty
Ruptura je nejzávažnější a smrtící komplikací aneurysmatu abdominální aorty. I přes zlepšení situace za posledních 50 let jsou ruptury aneurysmat abdominální aorty spojeny s vysokou mortalitou. Mortalita z ruptury aneurysmatu abdominální aorty je 90 %, zejména se zahrnutím pacientů, kteří zemřou dříve než jsou transportováni do nemocnice. Na druhé straně počet aneurysmat abdominální aorty se za posledních 20 let výrazně zvýšil. Jeden z důvodů je stárnutí populace ve většině zemí, a proto počet degenerativních AAA se zvyšuje. Stejně tak je tomu u pacientů s rupturou aneurysmatu břišní aorty. Věk nesmí být důvodem odmítnutí léčby. Je nutné nalézt optimální léčebné možnosti.
Následující práce je založena na analýze literatury včetně součaných doporučení, ale také na významných zkušenostech naší kliniky. Tento článek dále představuje možnosti vaskulární medicíny v rozvojových zemích, kde nelze aplikovat endovaskulární metody na dostačující úrovni a v dostatečném rozsahu. V tuto chvíli je jasné následující. 30denní mortalita po ošetření ruptur AAA je významně nižší v tzv. high-volume nemocnicích. Z odlišných důvodů nejsou všechny ruptury aneurysmat břišní aorty vhodné k EVAR. Otevřené řešení ruptur aneurysmat břišní aorty by mělo být operováno zkušeným cévním chirurgem pro otevřené výkony. Stejné by mělo platit pro léčbu endovaskulárních komplikací, které vyžadují konverzi v otevřený chirurgický výkon.
Neexistuje ideální výkon pro léčbu AAA. Každý výkon má své výhody a nevýhody, své limity a komplikace, a také indikace a kontraindikace. Další snížení mortality u ruptur AAA bude záležet na zavedení populačně založeného skríningu, na strategii prevence pooperačního poškození orgánů, a také na pokroku nové lékařské technologie. Z toho důvodu je vzdělávání nových mladých cévních chirurgů nejen v endovaskulární, ale i v otevřené aortální chirurgii nesmírně důležité.
Klíčová slova:
břišní aorta – výduť – ruptura
Authors:
L. Davidovic 1,2
Authors‘ workplace:
Faculty of Medicine, University of Belgrade
1; Clinic for vascular and endovascular surgery, Clinical Center of Serbia, Belgrade
2
Published in:
Rozhl. Chir., 2014, roč. 93, č. 7, s. 357-365.
Category:
Review
Overview
Rupture is the most serious and lethal complication of the abdominal aortic aneurysm. Despite all improvements during the past 50 years, ruptured abdominal aortic aneurysms are still associated with very high mortality. Namely, including patients who die before reaching the hospital, the mortality rate due to abdominal aortic aneurysm rupture is 90%. On the other hand, during the last twenty years, the number of abdominal aortic aneurysms significantly increased. One of the reasons is the fact that in majority of countries the general population is older nowadays. Due to this, the number of degenerative AAA is increasing. This is also the case for patients with abdominal aortic aneurysm rupture. Age must not be the reason of a treatment refusal. Optimal therapeutic option ought to be found.
The following article is based on literature analysis including current guidelines but also on my Clinic’s significant experience. Furthermore, this article show cases options for vascular medicine in undeveloped countries that can not apply endovascular procedures at a sufficient level and to a sufficient extent. At this moment the following is evident. Thirty-day-mortality after repair of ruptured abdominal aortic aneurysms is significantly lower in high-volume hospitals. Due to different reasons all ruptured abdominal aortic aneurysms are not suitable for EVAR. Open repair of ruptured abdominal aortic aneurysm should be performed by experienced open vascular surgeons. This could also be said for the treatment of endovascular complications that require open surgical conversion.
There is no ideal procedure for the treatment of AAA. Each has its own advantages and disadvantages, its own limits and complications, as well as indications and contraindications. Future reductions in mortality of ruptured abdominal aortic aneurysms will depend on implementation of population-based screening; on strategies to prevent postoperative organ injury and also on new medical technology improvements. Taking this into consideration, education of young vascular surgeons in endovascular but also in open aortic surgery, is of vast importance.
Key words:
abdominal aorta – aneurysm – rupture
Introduction
The most severe complication of an abdominal aortic aneurysm (AAA), is rupture. AAA rupture (RAAA) is a lethal event [1,2]. The United Kingdom Small Aneurysm Trial has shown that RAAA is followed with a much higher primary mortality than is acceptable[3,4]. Namely, 25% of patients with RAAA died before addmision to the hospital, while an additional 51% died after addmission during diagnostic procedure. Because of this, RAAA has great medical importance. The following article is based on literature analysis (including current guidelines) but also on my Clinic’s significant experience of more than 1000 open repairs (OR) of RAAA have been performed in the last 22 years [5−13] (Graph 1).

Until the mid-eighties, the AAA’ s diameter was the main indicator of their rupture [14]. However, an epidemiological study performed by Cronenwett and coworkers showed that, besides initial aneurysmatic diameter, COPD and arterial hypertension independently affect the rupture [14]. It means that small AAA can also rupture, but how? According to Laplace, low AAA rupture risk increases exponentially with the growth of the aneurysmatic diameter due to exponentially increased wall stress [15]. Unfortunately, the application of Laplace’s law on a biological model such as AAA is incomplete for two reasons. Firstly, AAA is not a symmetrical, spherical or cylindrical figure to which this law could be applied [15]. On the contrary, AAA consists of many small and large curves. Therefore, it is more difficult to estimate wall stress in the aneurysmatic wall. A computer 3D model for „peak wall stress“analysis was first used in 2000 [17]. It was named „Finite Element Model“(FEM) and based on a computer program which separates the aortic wall in 5000 to 30 000 squares depending on its capacity. The program calculates wall stress in each square and provides data on regional wall stress allocation, as well as on peak wall stress location [16]. According to this method, the highest wall stress foundin a healthy aorta, is five times lower than in AAA [17]. A significantly higher wall stress in ruptured and symptomatic AAA in comparison to asymptomatic AAA was also found [17,18]. The greatest confirmation of the method’s efficiency is the fact that the peak wall stress and rupture are located at the same place [18].

But what is a more important predictor of RAAA, wall stress or diameter? Eleven years ago, this was answered by Fillinger and his coworkers [19]. The peak AAA wall stress seems superior to diameter. Life tables for freedom from rupture have shown that a larger diameter was a highly significant predictor for rate of rupture. Additionally, high stress was also a highly significant predictor for the rate of rupture. Finally, subgroups were analyzed for combinations of small and large diameter and low and high wallstress, with the same thresholds as used in the other life tables. Low-stress aneurysms had a low rupture rate whether they were small or large, and high-stress aneurysms had a high rupture rate regardless of size [19].
What is the second problem with the applicability of Laplace’s law on AAA rupture? Laplace’s law neglects the aneurysmatic wall strength which is an independent factor of rupture [20]. Also, the wall strength is different on different allocations. According to recent conceptions, the lack of balance between „wall stress“and „strength“of the aneurysmatic wall causes aneurysmatic rupture [21]. What should not be forgotten are the calcifications in the aneurysmatic wall, and especially thrombosis at the aneurysmatic sac [22,23].
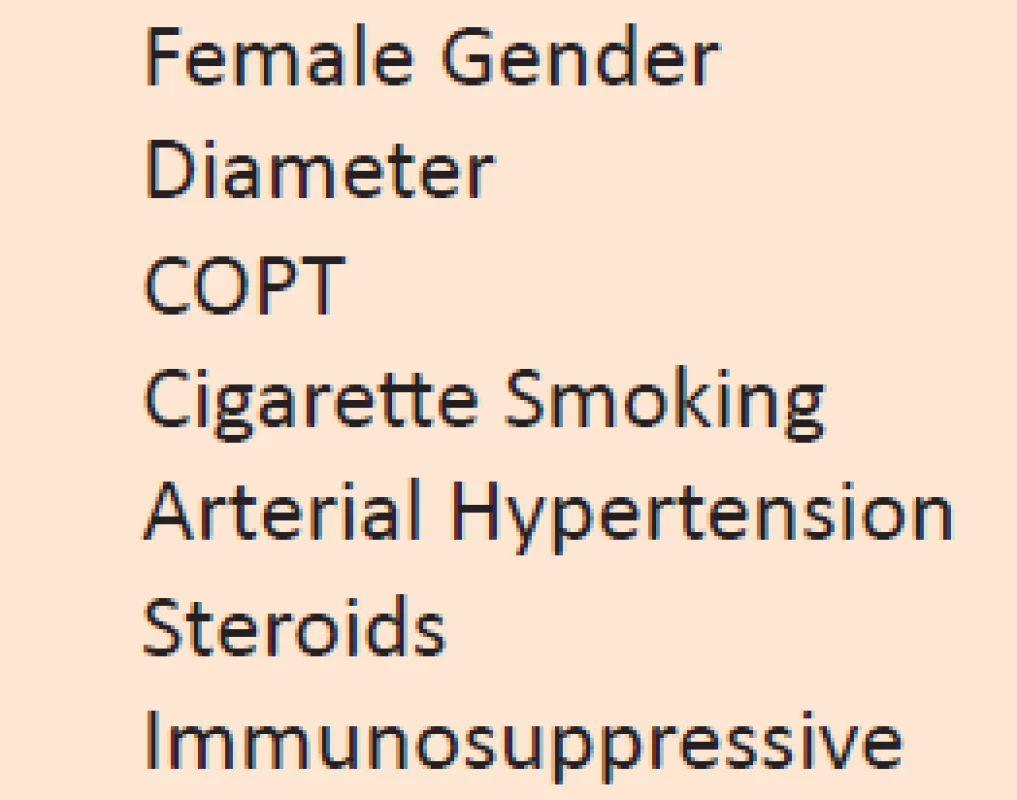
According to recent conception, RAAA is caused by many factors. These are: female gender, large diameter, COPT, cigarette smoking, arterial hypertension, steroid and immunosuppressive drugs [1−4] (Tab. 1).
Still, it is believed that biomechanical factors would be the best indicator for AAA rupture. Because of that, they will be one of the main aims of our investigations regarding AAA rupture in the following period.
Forms of abdominal aortic aneurysm rupture
AAA rupture includes intra-peritoneal, retro-peritoneal and unusual forms [1−4]. Intra-peritoneal AAA rupture causes exsanguination quite quickly, as well as cardiac arrest and results in a lethal outcome [1−4]. Due to this reason, it is primarily of pathological - not of clinical interest. The majority of other RAAAs rupture into the retroperitoneal space with the formation of a retroperitoneal hematoma [5−13]. These patients usually inform doctors about having collapsed which was preceded by abdominal or lower back pain. The diagnosis begins with physical examination. The RAAA is described as a painful, pulsating abdominal tumor in a shocked patient [5−11].
Chronic contained rupture is a very rare outcome of RAAA [10,24,25]. The term was introduced by Jones in 1986. The same author classified the clinical concept of chronic contained rupture [26]. His criteria to identify this entity are: previous knowledge of the AAA; previous symptoms or signs that may have been resolved; normal arterial tension, pulse rate and hematocrit on admission; retroperitoneal hematoma detected by Duplex ultrasonography, CT scan or MRI; intraoperative and histologic confirmation of organized retroperitoneal hematoma (Fig. 2).

AAA can also rupture into the duodenum or inferior vena cava with fistula formation [10]. The main characteristic of aorto-caval fistula (ACF) is its dramatic hemodynamic turnover caused by sudden diversion of high-pressure arterial blood flow to low resistance and high-capacitance venous blood flow. It causes two pathophysiological processes [27,28]. The first one is decreased systemic arterial pressure which is equal to hypovolemic shock. It leads to bursting heart syndrome. The second process is elevated renal venous pressure which reduces arterial perfusion of the kidneys and activates the renin/angiotensin system ending in a vicious cycle of heart failure. Taking this into account, clinical presentation of ACF includes quite variable symptoms and signs [5,9,10,12,13]. The classic triad consisting of lower back pain, pulsatile abdominal mass is seen in less than 50% of patients. Other signs are state of shock, ARI, high output cardiac failure with increased jugular vein pressure, as well as very specific pelvic venous hypertension with hematuria, rectal bleeding, scrotal hematoma or edema, lower limb edema and/or deep vein thrombosis (Fig. 3).

In less than 1% of cases, AAA’s rupture into the duodenum with the formation of primary aorto-duodenal fistula (ADF) [8]. Most often the third and fourth duodenal portions are involved, due to their anatomic relation with the abdominal aorta. Primary ADF produces gastrointestinal bleeding. However, gastrointestinal bleeding is much more often caused by gastric and duodenal ulcers. Therefore, how to suspect an ADF? If gastrointestinal bleeding is associated with lower back pain and a pulsatile abdominal mass, we ought to think of ADF [29,30].
Treatment options of ruptured abdominal aortic aneurysms
The latest meta-analysis, with more than 60 000 cases of RAAA, includes our experience as well [31]. The overal 30 day mortality was 48.5%. One of the conclusions is that mortality has not changed over the past 15 years. So, is EVAR a better solution for patients with RAAA [32]? The main advantages of REVAR are avoiding laparotomy, aortic cross clamping, general anesthesia, together with significantly lower blood loss. Meta-analyses regarding REVAR have shown significantly lower 30 day mortality (21 to 31.7%) in comparison to open surgery [33−36]. At the same time, REVAR is followed with a shorter length of hospital stay [36]. The first randomized prospective multicenter study followed. The AJAX trial randomized 116 patients to EVAR or OR groups [36]. The 30-day mortality was 21% in patients assigned to EVAR compared with 25% for OR. This trial did not show a significant difference in combined death and severe complications between EVAR and OR. Two months ago we received results of the IMPROVE trial performed in the UK [37]. Overall, there was no difference in 30-day mortality, 35% in the endovascular strategy group versus 37% in the open repair group. The median length of the procedure was 180 minutes for the endovascular strategy and 199 minutes for the open repair group. Costs after 30 days were not significantly lower in the endovascular strategy group. Patients who received endovascular repair under local anesthesia had lower mortality (13%) than those who underwent the procedure under general anesthesia (34%). Finally, the IMPROVE trial showed that for patients with good aortic anatomy and relative hemodynamic stability, the operative mortality for EVAR is only 25%, but this only represents about 60% of the cohort presenting for emergency aneurysm repair. Patients with ruptured abdominal aortic aneurysms should be treated in centers that can offer both endovascular and open aortic surgery at all times [38].
REVAR includes some important technical prerequisites. Namely, the hospital ought to have MSCT angiography, a hybrid theatre, as well as a sufficient choice of stent grafts available [39]. Besides well known already mentioned advantages, REVAR also has some limitations. Those are profound hypovolemic shock and unfavorable aneurysmal anatomy. An additional problem might be mid - and long term results. Developing countries such as Serbia should also consider financial issues. Let us start with the hemodynamic status of patients with RAAA. A significant number of patients with RAAA are hemodynamically unstable, and, if not treated immediately, more than 80% will die within two hours [40]. In a significant number of hospitals, MSCT is difficult or impossible to perform on such patients, and yet, without it, EVAR is not possible. According to some articles, due to anatomic limitations, only 40% to 60% of patients with RAAA are feasible for EVAR [38]. Aneurysmal sac shrinkage and enlargement during the follow up period is also a potential problem after REVAR. According to an article from the Lachat group, the cumulative risk of secondary intervention after REVAR was 35% at two years and more than 40% at three years [41] (Fig. 4).

According to some of the latest studies, five-year survival rate after open and endovascular repair of RAAA is almost the same [42].
Although an unpleasant fact, it should be stated that the difference between the possibilities of vascular medicine in developed and undeveloped countries is increasing significantly. Serbia and other undeveloped countries cannot apply endovascular procedures at a sufficient level and to a sufficient extent. Therefore, we need to apply open aortic surgery even in cases where the endovascular surgery has been proven better. I am sure that you do not possibly expect us to give up on our patients due to the lack of stent grafts.
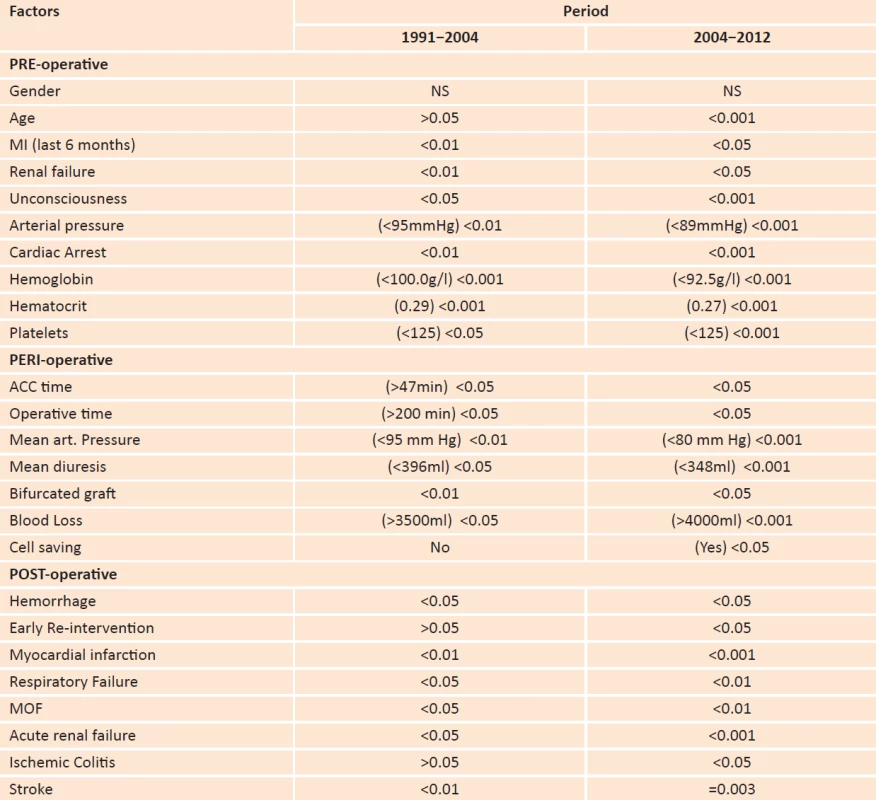
All this being said, open RAAA repair is still very important. But, can we improve early survival? Yes we can - according to the results from our analysis. In the period between 1991 and 2004, the 30-day-mortality after RAAA OR at our Clinic was 48.3%, while in the period between 2004 and 2012 it was 37.4% [6,8]. The difference is obvious. What has been shown by the analysis of mortality? Considering factors that have been associated with 30 day mortality, our two studies were not so different (Tab. 2).
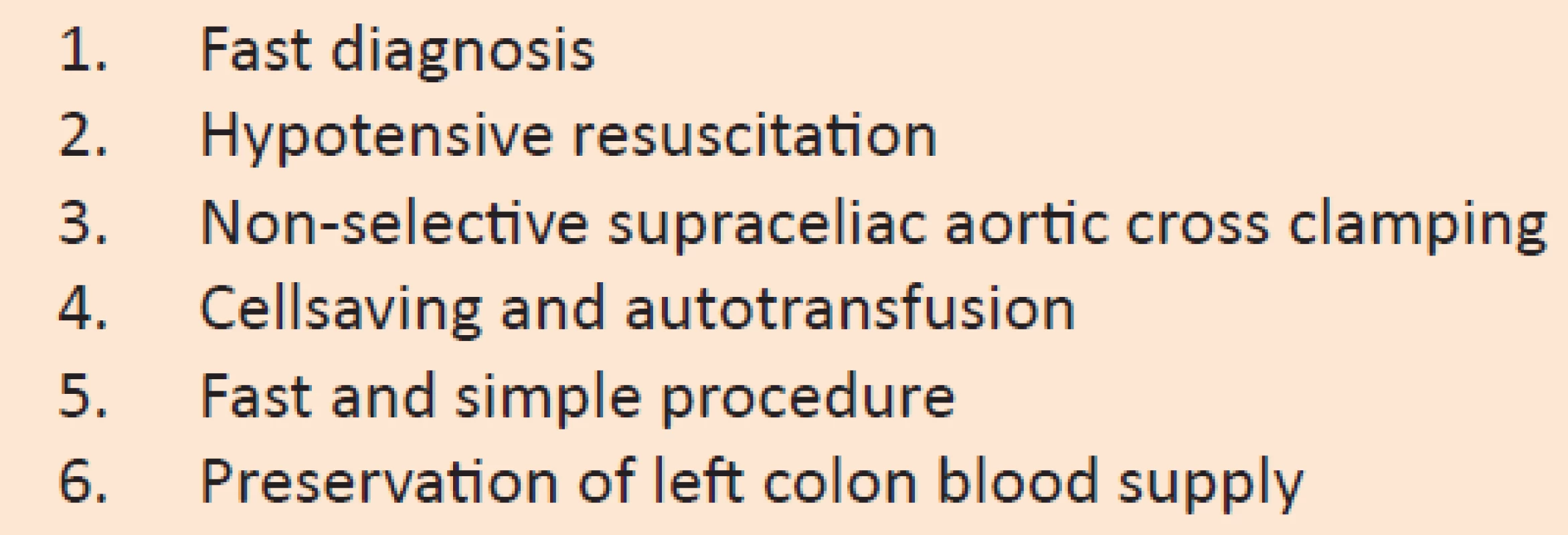
How did we manage to improve early survival during the second period of our investigation? I believe that it was the employment of modified Crawford’s strategy that includes: fast diagnosis, hypotensive resuscitation, non-selective supraceliac aortic cross clamping, cellsaving and autotransfusion, fast and simple procedure, as well as preservation of left colon blood supply [43] (Tab. 3).
In patients with onset abdominal or lower back pain who have a pulsatile abdominal tumor and profound shock, we perform emergency surgery only after ultrasonography confirmation. If the arterial pressure is over 100 mmHg, after ultrasonography confirmation, the patient is admitted to ICU. Emergency surgery is performed after additional analysis. MSCT is performed only in perfectly hemodynamically stable patients, or in those with suspected suprarenal or thoracoabdominal aneurysms. Thus the mean arrival time to the operating room is 35 minutes. It is very good time considering the fact that diagnosis of RAAA is established in a building that is 100 m away from our department. In the AJAX trial, the mean arrival time to the operating room for EVAR was over 70 minutes, almost 30 minutes longer than the time taken to reach the operating theatre for open repair [37]. In the IMPROVE trial, the time for patients with rupture to reach the operating room was much shorter, 37 and 47 minutes for the open and endovascular groups respectively [38] (Graph 2).

One of the biggest mistakes in the initial RAAA treatment is aggressive restitution of circulatory volume [44]. It increases arterial pressure that, in addition, disrupts the initial retroperitoneal tamponade and leads to new bleeding with conversion of retroperitoneal rupture into an intra-peritoneal one. Crawford was the first to insist on “permissive hypotension” [43]. Volume should be compensated to a level required to maintain consciousness and to prevent ST depression.
We routinely perform RAAA OR under supraceliac aortic cross clamping. It is a fast, efficient and safe proximal bleeding control, which, at the same time, enables prevention of iatrogenic injuries in the presence of retroperitoneal hematoma. Due to the same reasons, distal bleeding control is performed by placing ballon occlusive catheters into both iliac arteries (Fig. 5).

However, during OR of ACF caused by RAAA, a surgeon has one additional problem - controlling retrograde bleeding from the fistula. Proximal aortic cross clamping decreases AV shunting; however, not sufficiently. On the other hand, the manipulation of the aneurysmatic neck and dissection of the inferior vena cava can cause mobilization of the mural thrombus. Its exit through the fistula results in paradoxal pulmonary embolism which may be fatal. The first method for controlling bleeding from the fistula is compression after opening the aneurysm sac. However, I recommend a different procedure [5,9,13]. The insertion of two occlusion balloon catheters via femoral vein into the inferior vein cava above and below the fistula is a rather simple and useful procedure. It should be performed prior to laparotomy (Fig. 6).

In contrast to our previous study, during our second one, ICS was used routinely. This procedure is significant during RAAA OR for three reasons. First of all, it enables immediate operation. In the past, blood type was determined and appropriate blood was supplied. Another problem with RAAA OR could be blood shortage. Only 3% of Serbia’s population donates blood annually, which is absolutely insufficient for the successful functioning of the health system – minimum being 5%. Thus, the consequences of allogeneic blood deficit are annulled by intra operative cell saving and auto-transfusion. Quite often, exsanguinous transfusion is necessary during OSR of RAAA. The situation is different when the patient receives a large amount of his own blood in contrast to allogeneic blood. ARDS occurs more often in the case of allogeneic blood. According to our study, intraoperative cell saving with autotransfusion has evident clinical and financial effects during RAAA OR [45,46].
Vascular reconstruction during RAAA OR should be performed by the simplest method possible. The majority of papers, including our studies, show that the us of bifurcated graft increases mortality [6,8,47]. To be more precise, the usage of bifurcated graft (especially aorto bifemoral reconstruction) prolongs total operative time and increases the incidence of ischemic colitis.
According to different studies, the incidence of ischemic colitis following RAAA open surgery ranges from 3 to 16% [1,2,6,8,47]. Ischemic colitis following a RAAA open repair has major clinical importance because of the very high mortality rate [48−50]. The most influential on the development of ischemic colitis after elective AAA repair are: associated celiac, superior mesenteric or pelvic artery occlusive disease; the presence of a large meandering mesenteric or marginal artery; previous bowel resection, prolonged proximal aortic cross clamping, extensive blood loss and ligature of both hypogastric arteries [48−50]. One of the greatest problems with colon ischemia is early diagnosis. Hemorrhagic diarrhea, abdominal distension, pain, fever, anuria, hypotension, elevated WBC count, thrombocytopenia, postoperative fluid requirements >5l, and lactic acidemia, occurs in only 30% of patients with ischemic colitis developed after aortic surgery [1,2,48−50]. On the other hand, unnecessary explorative laparotomy may be hazardous for patients, while a laparotomy performed too late is futile. This is why the first step should be colonoscopy. 95% of ischemic colitis after aortic surgery is within the recto sigmoid colon. Therefore colonoscopy of the left colon is sufficient [48−50]. Concerning the possible causes, as well as the consequences of ischemic colitis, one of the most important questions during an elective AAA repair is: What should be done with the IMA - ligature or routine re implantation? [51]. The safety of a ligature depends on other collateral pathways. Doppler ultrasound, intraoperative photoplethysmography, endoluminal pulse oximetry, laser Doppler flowmetry, measurements of intramural pH, air-automated sigmoid capnometry and IMA stump pressures, have been used intraoperatively for collateral flow estimation [52−58]. This indicates that none of these methods is good enough. The majority of authors, as well as my colleagues and I, usually use a very simple strategy. The presence of retrograde bleeding from the inferior mesenteric artery with a normal-appearing colon would indicate that it is safe to perform a ligature. This ligature has to be done at its origin from the aneurysm sac, to preserve the left colic artery [1,2,6,8]. Reattachment of the inferior mesenteric artery is only indicated for patients who are at increased risk of colonic ischemia. At the same time, anterograde blood flow should be preserved to at least one hypogastric artery [1,2] (Fig. 7,8).


Conclusion
Regarding repair of RAAA, the following is clear and evident:
- 30-day-mortality after repair of RAAA is significantly lower in high-volume hospitals.
- Currently, all RAAAs are not suitable for EVAR.
- OR for RAAA should be performed by very experienced open vascular surgeons.
- Endovascular complications that require open surgical conversion should be performed by very experienced open vascular surgeons.
- Education of young vascular surgeons in both open and endovascular aortic surgery is extremely important.
- There is no ideal procedure for the treatment of AAA. Each has its own advantages and disadvantages, its own limits and complications, as well as indications and contraindications.
Lazar B. Davidovic
Clinic for Vascular and Endovascular Surgery,
Clinical Center of Serbia
Koste Todorovića Street 8,
110 00 Belgrade, Serbia.
e-mail: davidovic.lazar@gmail.com
Sources
1. Chaikof EL, Brewster DC, Dalamn RL, et al. The care of patients with and abdominal aortic aneurysm: The society for Vascular Surgery practice guidelines. J Vasc Surg 2009;50 (8S):1−50.
2. Moll FL, Powell JT, Fraedrich G, et al. Management of abdominal aortic aneurysms clinical practice guidelines of the European Society for Vascular Surgery. Eur J Vasc Endovasc Surg 2011;41:S1−S58.
3. The UK Small Aneurysm Trial Participants. Health service costs and quality of life for early elective surgery or ultrasonographic surveillance for small abdominal aortic aneurysms. Lancet 1998;352 : 1656−60.
4. United kingdom small aneurysm trial participants. Long-term outcomes of immediate repair compared with surveillance of small abdominal aortic aneurysms. New Engl J Med 2002;346 : 1445−1452.
5. Davidovic L, Kostic D, Cvetkovic S, et al. Aorto-Caval Fistulas. Cardiovascular surgery 2002;10 : 555−60.
6. Marković M, Davidović L, Maksimović Ž, et al. Ruptured abdominal aortic aneurysm. predictors of survival in 229 consecutive surgical patients. HERZ 2004;29 : 123−9.
7. Davidović L, Kostić D, Jakovljević N, et al. Abdominal aortic surgery and horseshoe kidney. Ann Vasc Surg 2004;18 : 725−8.
8. Davidović L, Marković M, Kostić D, et al. Ruptured abdominal aortic aneurysms: Factors influencing early survival. Ann Vasc Surg 2005;19 : 29−3.
9. Cinara I, Davidovic L, Kostic D, et al. Aorto-caval fistulas: a Review of eighteen years Experience. Acta Chir Belg 2005;105 : 616−20.
10. Davidovic L, Markovic M, Jakovljevic N, et al. Unusual forms of ruptured abdominal aortic aneurysms. Vascular 2008;16 : 17−24.
11. Markovic M, Davidovic L, Savic N, et al. Intraoperative cell salvage versus allogeneic transfusion during abdominal aortic surgery: Clinical and financial outcomes. Vascular 2009;17 : 83−92.
12. Dragas M, Davidovic L, Pejkic S, et al. Aorto-left retroaortic renal vein fistula is a rare complication of abdominal aortic aneurysm with unique clinical presentation. J Vasc Surg 2010, 52 : 1658−61.
13. Davidovic L, Dragas M, Cvetkovic S, et al. Twenty years of experience in the treatment of spontaneous aorto-venous fistulas in a developing country. World J Surg 2011;35 : 1829−34.
14. Cronenwett IL, Murphy TF, Zelenock GB, et al. Actuarial analysis of variables associated with rupture of small abdominal aortic aneurysms. Surgery 1985;98 : 472.
15. Pierre Simon, marquis de Laplace, Traité de Mécanique Céleste, volume 4, Paris, France: Courcier, 1805, Supplément au dixième livre du Traité de Mécanique Céleste.
16. Raghavan ML, Vorp DA, Federle MP, et al. Wall stress distribution on three-dimensionally reconstructed models of human abdominal aortic aneurysm. J Vasc Surg 2000;31 : 760−9.
17. Filinger MF, Raghavan ML, Marra SP, et al. In vivo analysis of mechanical wall stress and abdominal aortic aneurysm rupture risk. J Vasc Surg 2002;36 : 589−597.
18. Venkatasubramaniam AK, Fagan MJ, Mehta T, et al. A comparative study of aortic wall stress finite element analysis for ruptured and non ruptured abdominal aortic aneurysms. Eur J Vas Endovasc Surg 2004;28 : 168−176.
19. Fillinger MF, Marra SP, Raghavan ML, Kennedy FE. Prediction of rupture risk in abdominal aortic aneurysm during observation: Wall stress versus Diameter. J Vasc Surg 2003; 37 : 724−32.
20. Vande Geest JP, Wang DHJ, et al. A noninvasive method for determination of patient specific wall strength distribution in abdominal aortic aneurysms. Ann Biomed Eng 2006; 34 : 1098−1106.
21. Di Martino ES, Bohra A, VandeGest JP, et al. Biomechanical properties of rupture vs electively repaired abdominal aortic aneurysm wall tissue. J Vasc Surg 2006;43 : 570−576.
22. Stenbaek J, Kalin B, Swedenborg J. Growth of thrombus may be a better predictor of rupture than diameter in patients with abdominal aortic aneurysms. Eur J Vasc Endovasc Surg 2000;20 : 466–9.
23. Wang DHJ, Makaroun MS, Webster MW, Vorp DA. Effect of intraluminal thrombus on wall stress in patient-specific models of abdominal aortic aneurysm. J Vasc Surg 2002;36 : 598−604.
24. Defraigne JO, Sakalihasan N, Lavigne JP, Van Damme H, Limet R. Chronic rupture of abdominal aortic aneurysm manifesting as crural neuropathy. Ann Vasc Surg 2001; 15 : 405−11.
25. Nowami Y, Okozaki Y, Yamashiro T, Ogoshi S. Chronic contained rupture of abdominal aortic aneurysms. J Cardiovasc Surg 1996;37 : 25−28.
26. Jones CS, Reilly MK, Dalsing ME, et al. Chronic contained rupture of abdominal aortic aneurysm. Arch Surg 1986; 121 : 542−546.
27. Dardik H, Dardik I, Strom MG, Attai L, Carnevale N, Veith FJ. Intravenous rupture of arteriosclerotic aneurysms of the abdominal aorta. Surgery 1972;80 : 647−51.
28. Skinner JA, Prabhakar G, Genecov DG, et al. Presentation and treatment of spontaneous aortocaval fistula. South Med J 1997;90 : 993−6.
29. Voorhoeve R, Moll FL, Bast TJ. The primary aortoenteric fistula in the netherlands-the unpublished cases. Eur J Vasc Endovasc Surg 1996;11 : 429−431.
30. Tareen AH, Schroeder TV. Primary Aortoenteric Fistula: Two New Case Reports and a Review of 44 Previously Reported Cases. Eur J Vasc Endovasc Surg 1996;12 : 5−10.
31. Hoornweg LL, Storm-Versloot MN, Ubbink DT, et al. Meta analysis on mortality of ruptured abdominal aortic aneurysms. Eur J Vasc Endovas Surg 2008; 35: 558−570.
32. Park BD, Azefor N, Huang C-C, Ricotta JJ. Trends in treatment of ruptured abdominal aortic aneurysm: Impact of endovascular repair end implications for future care. J Am Coll Surg 2013;216 : 745−755.
33. Mastracci TM, Luis-Garrido Olivares, Cina CS, et al. Endovascular repair of ruptured abdominal aortic aneurysms: A systemic review and metaanalysis. J Vasc Surg 2008;47 : 214−21.
34. Rayt HS, Sutton AJ, London NJM, et al. A systemic review and metaanalysis of endovascular repair (EVAR) for ruptured abdominal aortic aneurysms. Eur J Vasc Endovasc Surg 2008;36 : 536−44.
35. Veith FJ, Lachat M, Mayer D, et al. Collected world and single centre experience with endovascular treatment of ruptured abdominal aortic aneurysms. Ann Surg 2009;250 : 818−24.
36. McPhee J, Esatami MH, Arous EJ, et al. Endovascular treatment of ruptured abdominal aortic aneurysms in the United States. A significant survival benefit over open repair is indenpendently associated with inreased institutional volume. J Vasc Surg 2009; 49 : 817−26.
37. Reimerink JJ, Hoornweg LL, Vahl AC, et al. Amsterdam acute trial collaborations. Endovascular repair versus open repair of ruptured abdominal aortic aneurysms: a multicenter randomized controlled trial. Ann Surg 2013;258 : 248−56.
38. IMPROVE Trial Investigators. An endovascular strategy for suspected ruptured abdominal aortic aneurysm brings earlier home discharge but not early survival or cost benefits. Eur J Vasc Endovasc Surg 2014;47 : 333−4.
39. Veith F, Powel JT, Hinchliffe RJ. Is a randomized trial necessary to determine whether endovascular repair is the preferred management strategy in patients with ruptured abdominal aortic aneurysms? J Vasc Surg 2010;52 : 1087−93.
40. Lloyd GM, Bown MJ, Norwood MGA, et al. Feasibility of preoperative computer tomography in patients with ruptured abdominal aortic aneurysm: A time-to-death study in patients without operation. J Vasc Surg 2004;39 : 788−91.
41. Hechelhammer L, Lachat M, Wildermuth S, et al. Midterm outcome of endovascular repair of ruptured abdominal aortic aneurysms. J Vasc Surg 2005;41 : 752−7.
42. Eefting D, Ultee KH, Von Meijenfeldt GCI, et al. Ruptured AAA. state of the art managemnet. J Cardiovasc Surg 2013;54 (Suppl.1):47−53.
43. Crawford S. Ruptured abdominal aortic aneurysm. An Editorila. J Vasc Surg 1991;13 : 348.
44. Roberts K, Ravell M, Youssef H, et al. Hypotensive rescucitation in patients with ruptured abdominal aortic aneurysm. Eur J Vasc Endovasc Surg 2006;31 : 339−44.
45. Markovic M, Davidovic L, Savic N, et al. Intraoperative cell salvage versus allogeneic transfusion during abdominal aortic surgery: Clinical and financial outcomes. Vascular 2009;17 : 83−92.
46. Shantikumar S, Patel S, Handa A.The role of cell salvage autotransfusion in abdominal aortic aneurysm surgery. Eur J Vasc Endovasc Surg 2011;42 : 577−84.
47. Van Dongen H, Leusink J, Moll F, Brons F, De Boer A. Ruptured abdominal aortic aneurysms: factors influencing postoperative mortality and long-term survival. Eur J Vasc Endovasc Surg 1998;15 : 62−66.
48. Jarvinen O, Laurikka J, Salenius JP, Lepanto M. Mesenteric infarction after aortoiliac aurgery on the basis of 1752 operations from the National Vascular Registry. World J Surg. 1999;23 : 243−247.
49. Bjorck M, Bergqvist D, Troeng T. Incidence and clinical presentation of bowel ischemia after aortoiliac surgery-2930 operations from a population based registry in Sweden. Eur J Vasc Endovasc Surg. 1996;12 : 139−144.
50. Björck M, Troëng T, Bergqvist D. Risk factors for intestinal ischemia after aortoiliac surgery. A combined cohort and case-control study of 2824 operations. Eur J Vasc Endovasc Surg 1997;13 : 531−539.
51. Batt M, Ricco JB, Staccini P. Do internal iliac arteries contribute to vascularization of the descending colon during abdominal aortic aneurysm surgery? An intraoperative hemodynamic study. Ann Vasc Surg 2001;15 : 171−174.
52. Hobson RW 2nd, Wright CB, Rich NM, Collins GJ Jr. Assessment of colonic ischemia during aortic surgery by Doppler ultrasound. J Surg Res 1976;20 : 231−235.
53. Ouriel K, Fiore WM, Geary JE. Detection of occult colonic ischemia during aortic procedures: use of an intraoperative photoplethysmographic technique. J Vasc Surg 1988;7 : 5−9.
54. Oakland C. Endoluminal pulse oximetry of the sigmoid colon and the monitoring of the colonic circulation. Cardiovasc Surg 1999;7 : 704−709.
55. Krohg-Sorensen K, Kvernebo K. Laser Doppler flowmetry in evaluation of colonic blood flow during aortic reconstruction. Eur J Vasc Surg 1989;3 : 37−41.
56. Fiddian-Green RG, Amelin PM, Herrmann JB, et al. Prediction of the development of sigmoid ischemia on the day of aortic operations: indirect measurements of intramural pH in the colon. Arch Surg 1986;121 : 654.
57. Lebuffe G, Decoene C, Raingeval X, et al. Pilot study with air-automated sigmoid capnometry in abdominal aortic aneurysm surgery. Eur J Anaesthesiol 2001;18 : 585−592.
58. Schiedler MG, Cutler BS, Richard G. Sigmoid Intramural pH for prediction of ischemic colitis during aortic surgery: A comparison with risk factors and inferior mesenteric artery stump pressures. Arch Surg 1987;122 : 881−886.
Labels
Surgery Orthopaedics Trauma surgeryArticle was published in
Perspectives in Surgery

2014 Issue 7
- Possibilities of Using Metamizole in the Treatment of Acute Primary Headaches
- Metamizole vs. Tramadol in Postoperative Analgesia
- Spasmolytic Effect of Metamizole
- Metamizole at a Glance and in Practice – Effective Non-Opioid Analgesic for All Ages
-
All articles in this issue
- Interdisciplinary European guidelines on metabolic and bariatric surgery
- Risks and complications of urological surgical procedures in elderly patients
- Staged management of open tibial fractures with soft tissue defect
- Sarcoma of the chest wall after radiotherapy for breast carcinoma – a case report
- Treatment strategy for ruptured abdominal aortic aneurysms
- Pancreatic leakage and acute postoperative pancreatitis after proximal pancreatoduodenectomy
- Perspectives in Surgery
- Journal archive
- Current issue
- About the journal
Most read in this issue
- Sarcoma of the chest wall after radiotherapy for breast carcinoma – a case report
- Treatment strategy for ruptured abdominal aortic aneurysms
- Risks and complications of urological surgical procedures in elderly patients
- Pancreatic leakage and acute postoperative pancreatitis after proximal pancreatoduodenectomy



