Micronail Insertion into Cadaver Distal Radius: A Study of Insertion Location, Rotation and Screw Articular and Cortical Penetration
Aplikace nitrodřeňové fixace Micronail do distálního radia, kadaverózní studie o pozici jeho vstupu, rotaci a penetraci šroubů přes kortikalis kosti a do kloubů
CÍL:
Cílem této studie bylo zhodnotit rizika spojená s léčbou nestabilních zlomenin distálního radia Mikronailem. Na kadaverech bylo hodnoceno riziko penetrace distálních zamykatelných šroubů do radiokarpálního skloubení nebo jejích umístění proximálně od subchondrální kosti a riziko jejích proniknutí do dorzální nebo volární plochy distálního radia.
MATERIÁL A METODIKA:
Mikronail byl aplikován 40 kadaverózních distálních radií. Kortikální okno pro vstup Mikronailu bylo umístěno v třech různých lokalitách: v I. extenzorovém kompartmentu, mezi I. a II. extenzorovým kompartmentem a ve II. extenzorovém kompartmentu. Kortikální okno bylo provedeno také na třech různých vzdálenostech od hrotu processus styloideus radii (0,5, 1,0 a 1,5 cm). Šrouby byly umístěny v různých úhlech rotace Mikronailu.
VÝSLEDKY:
Optimální poloha pro kožní incizi je 0,5 cm proximálně od hrotu processus styloideus radii, na dorzální třetině výšky distálního radia, v délce 2,0 cm proximálním směrem. Kortikální okno pro vložení Mikronail ™ je 1,0 cm proximálně od hrotu processus styloideus radii mezi I. a II. extenzorovým kompartmentem s jeho zaváděním v 0° rotaci v transverzální rovině. V této poloze jsou rizika jeho použití nejmenší.
ZÁVĚR:
Léčba zlomenin distálního radia nitrodřeňovou fixací Mikronailem je miniinvazivním chirurgickým řešení. Použitím správné operační techniky a správný výběr pacientů vede k úspěšným výsledkům s minimální kloubní nebo kortikální penetrací šroubů a s minimálním rizikem poškození či podráždění měkkých tkání.
Klíčová slova:
Mikronail, zlomenina distálního radia, intramedulární fixace.
Authors:
Adel Safi 1; Radek Hart 1,2; Martin Feranec 1; Martin Komzák 1
Authors‘ workplace:
Ortopedicko-traumatologické oddělení, Nemocnice Znojmo
1; Traumatologické oddělení, Lékařská fakulta Masarykovy Univerzity Brno
2
Published in:
Úraz chir. 21., 2013, č.3
Overview
OBJECTIVE:
The purpose of the study was to estimate the range of risks related to the treatment of unstable fractures of distal radius with Micronail™. In this study were evaluated, on cadavers, the incidence of penetration of distal locking screws into the radiocarpal joint or their displacement proximally from subchondral bone; and the incidence of their penetration into the dorsal or volar surface of radius.
MATERIAL AND METHODS:
The Micronail was placed in 40 cadaver distal radii. Cortical window for Micronail insertion was made in different locations: in I. extensor compartment, between I. and II. extensor compartments and in II. extensor compartment. Cortical window was made also in three different distances from the tip of radial styloid (0.5, 1.0 and 1.5 cm). The screws were placed at different angles of rotation of Micronail.
RESULTS:
Optimal position for skin incision is about 0.5 cm proximal from the tip of radial styloid, on dorsal third of altitude of the distal radius, and extends for 2.0 cm proximally. The cortical window for Micronail™ insertion is about 1.0 cm proximal from the tip of radial styloid between I. and II. extensor compartments in 0° tilt in transversal plane. In this position, the risks of this treatment are the least.
CONCLUSION:
Treatment of distal radius fracture by intramedullary fixation with Micronail™ is a miniinvasive surgical option. Applying the correct surgical technique and proper patient selection lead to successful outcomes with minimum articular or cortical penetration and minimum risks of soft tissue injury or irritation.
Keywords:
Mirconail, distal radial fracture, intramedullary fixation.
INTRODUCTION
Fractures of the distal radius are the most common fractures in the human skeleton [3]. Moreover, according to published data worldwide, these fractures are more frequent among women (the approximate ratio being 3-4 : 1), with a significant increase in the number of injuries after menopause [5, 10]. For stable fractures (51–60 %), treatment by closed reduction and immobilization is usually sufficient. For unstable fractures (40–49 %), on the other hand, osteosynthesis fixation treatment after reduction is often necessary [3, 7, 9, 11, 14, 19]. Currently, there are several methods of fixation of the unstable fractures of the distal end of the radius, such as: percutaneous K-wire fixation; fixation with external fixators; open reduction and internal fixation (ORIF); or a combination of the three methods [3, 10, 19]. Recently, intramedullary nailing has also been used. In our study, we used intramedullary implant Micronail™ (Wright Medical Technology, Inc., Arlington, TN, USA) (Fig. 1a, 1b, 2a and 2b). This implant is designed to treat extra-articular metaphyseal distal radial fractures and simple or multifragmentary sagittal articular ones (AO classification types A2, A3, B1.1 and B1.2). Contraindications include: comminuted articular fractures, Barton‘s fractures, fractures that cannot be treated adequately by closed reduction and metaphyseal fractures less than 1 cm or more than 4 cm from the radiocarpal joint [15].

The purpose of this study was to estimate the range of risks related to the treatment of unstable fractures of distal radius with intramedullary implant Micronail™. In this study, were evaluated, on cadavers, the incidence of penetration of distal locking screws into the radiocarpal joint or its displacement proximally from subchondral bone; and the incidence of its penetration into the dorsal or volar surface of radius.


MATERIALS AND METHODS
The insertion path of Micronail™ into the distal end of the radius was accomplished in 40 cadaver distal radii; dying at the ages of 71 to 90 years (the mean being 82 years), without prior surgery on the wrist and no anatomical deformities of the upper limbs. All cadavers were from 16 to 48 hours after death. We used a Micronail™ of size 2 and a locking screw of 24 mm long.

During the experiment, we investigated the best localization of cortical window to insert the nail into the medullary cavity; the risk of penetration of the fixed-angle locking screws to the radiocarpal joint or to the distal radioulnar joint (DRUJ) or their displacement proximally from subchondral bone and the risk of the dorsal or volar screws penetration at different angles of rotation of the Micronail™ in the transverse plane.
Initially, a skin incision of 2.0 cm long was performed at the lateral side of the distal end of radius above the radial styloid. In the dermis, the superficial branch of the radial nerve was isolated. Then, for experimental reasons, the incision was distally extended the incision was distally extended to the tip of the radial styloid and proximally about 5 cm. The incision was finally extended from its distal end transversally on the dorsal and volar sides. The tendons, on the dorsal side of the wrist, pass through six osteofibrosis channels under extensor retinaculum. In this research, we inserted the implant in the I. and II. extensor compartments in various ways, as will be explained below. After removing the dorsal retinaculum, the tendons of m. extensor digitorum communis (EDC), m. Extensor pollicis longus (EPL), m. flexor carpi radialis (FCR) were released, and the pronator quadrates and joint capsule were incised to expose the dorsal and volar surfaces of the distal end of the radius with radiocarpal joint.
Three positions for the nail entry in dorso-volar direction were investigated between the m. abductor pollicis longus (APL) tendon and m. extensor pollicis brevis (EPB) tendon in the first extensor compartment; between the APL-EPB tendons and m. extensor carpi radialis longus (ECRL) tendon (between I and II. extensor compartments); and between the ECRL tendon and the tendon of m. extensor carpi radialis brevis (ECRB) in II. extensor compartment. Each of these positions was accomplished in three different distances from the tip of the radial styloid (0.5, 1.0 and 1.5 cm) measured with ruler. In each of these variants, the fixed-angle locking screws were inserted in various degrees of rotation of the nail to the transverse axis of the radius (20° and 10° dorsal, 0° and 10° and 20° volar) measured with gonio meter. Each variant was accomplished twenty times. The t-test was used to evaluate the significance of parameters (the real severity of penetrations).
RESULTS
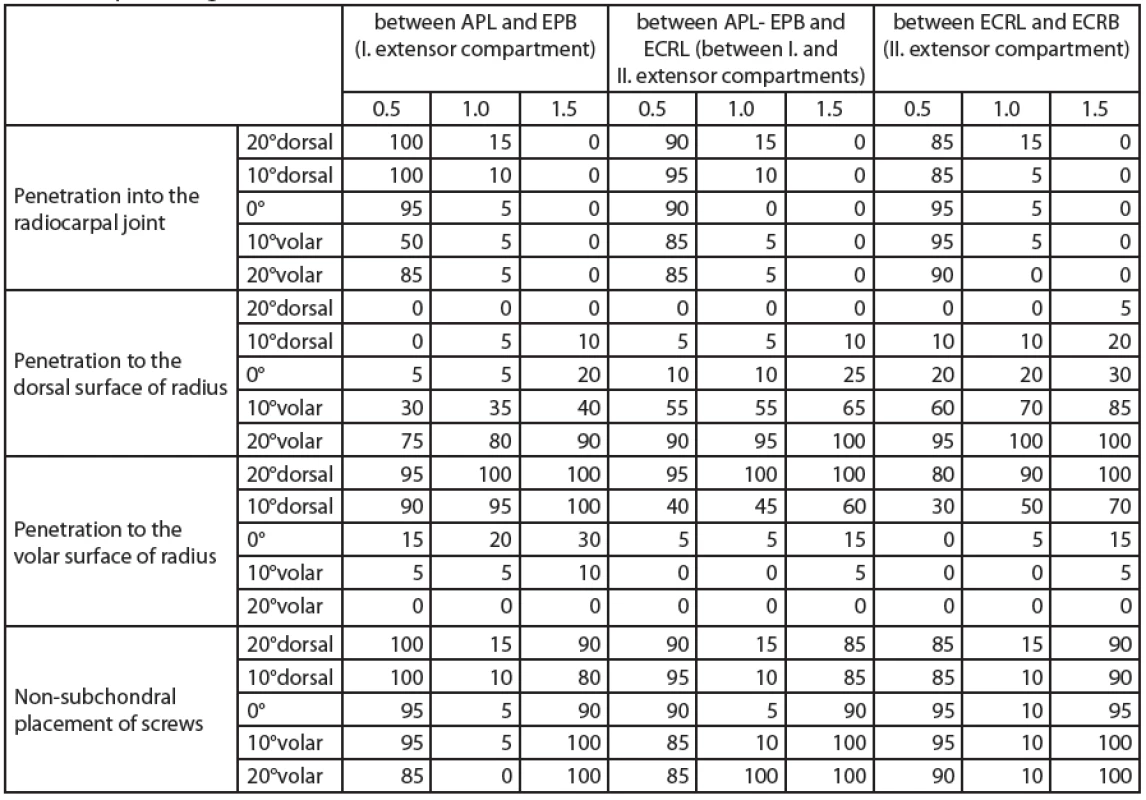
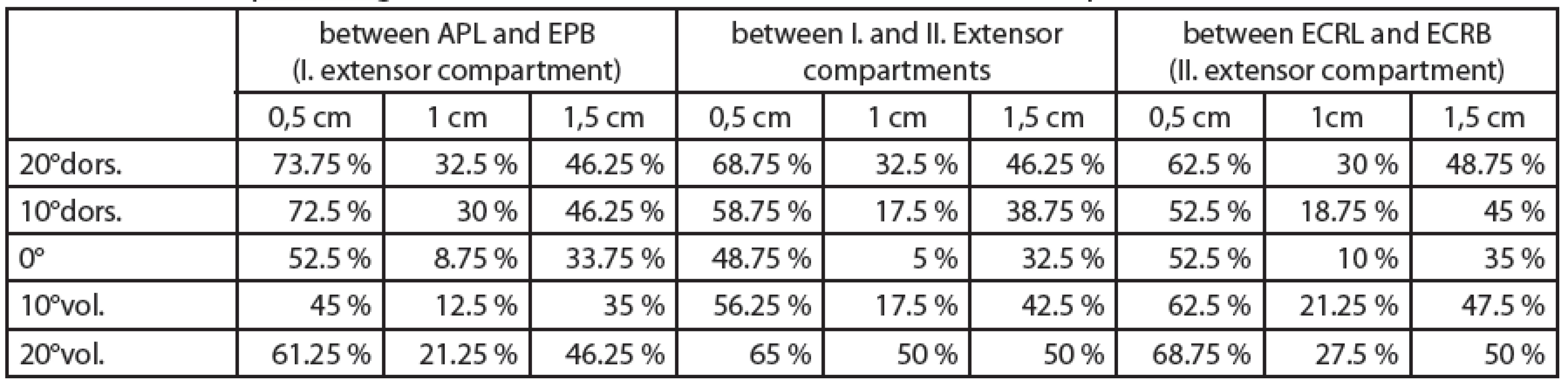
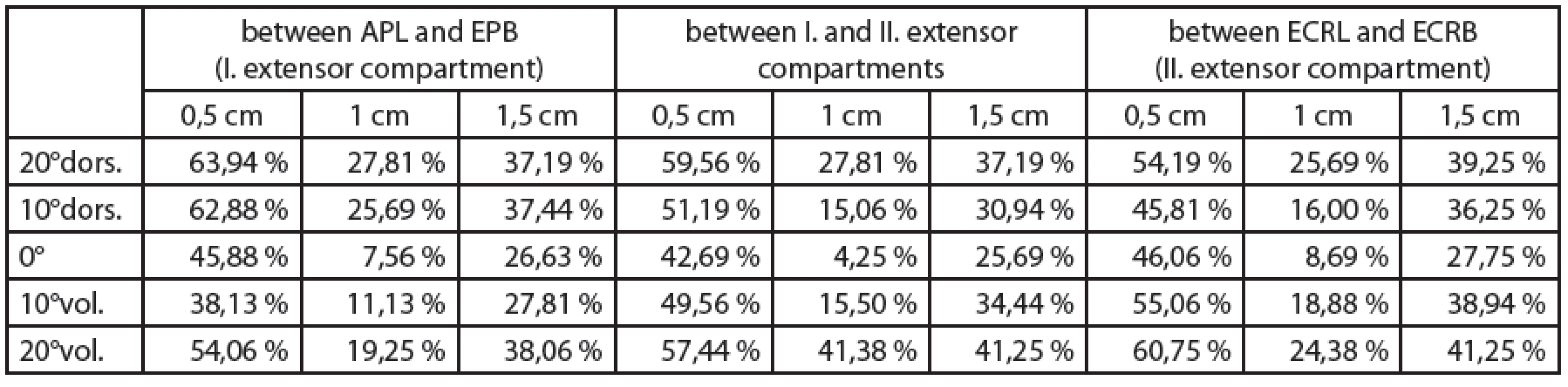
Table 1 shows the percentages of adverse conditions (screw penetration) for a particular location and angle of nail placement; here comes the statistical deviation of about 10 % (0.1). The results have been statistically processed in tables (Tables 2 and 3) and on graphs (Figures 3-7). Figures 3 and 6 show that the penetration into the radiocarpal joint and non-subchondral displacement depend mainly on the distance from the tip of the radial styloid. Rotation of the nail in the horizontal plane affects the least. Figures 4 and 5 show that the penetration into the dorsal or volar sides of the distal radius depends mainly on the rotation of the nail in the transverse plane and is affected the least by the distance from the tip of the radial styloid. In the case of penetration into the dorsal surface of radius, there is a risk of injury of the extensor tendons in the III., IV. and V. extensor compartments, mainly EDC tendon, which lies on the ulnar half of dorsal surface of the distal radius. In the case of the penetration to the volar surface, there is a risk of injury in m. pronator quadratus that is not significant.





Rough drilling or use of screws much longer than needed may cause injury of the m. flexor digitorum profundus tendon. Injuries of the m. flexor pollicis longus tendon and the median nerve are unlikely. There was no case of penetration to DRUJ in all positions of Micronail in all trials.
Table 2 is a summary of the four aforementioned conditions of screw penetration. It shows the percentage of all adverse conditions in each trial (i.e. entry positions). Since the individual penetrations do not result in side effects of same severity and Table 2 does not, indeed, reflect the real severity of each, it is advisable to take decisions in accordance with the recalculated values (more reflective) (Table 3). Screw penetration into the joint space is considered the most serious penetration, thus it is assigned the value of 1.0. For the same reason, penetration to the dorsal side was given the value of 0.9; the penetration to the volar side the value of 0.85 and non-subchondral screws placement the value of 0.75. The values in Table 3 are shown in Figure 7.
To sum up, the results show that the best location of a cortical window is between I. and II. extensor compartments and 1 cm from the tip of the radial styloid with insertion at 0° rotation in the transverse plane. For an ideal position of the cortical window, the best location of skin incision is on the radial side of distal radius on the dorsal third of its altitude. It begins 0.5 cm proximal to the tip of radial styloid and continues proximally 2.0 cm. In the subcutaneous tissue, it is necessary to isolate the superficial branch of the radial nerve cautiously. The nerve should remain uninjured on the dorsal side of approach. Then, the fascia between I. and II. extensor compartments is to be dissected longitudinally.
DISCUSSION
Masao [10] made a cortical window at the tip of the radial styloid through a 2 cm longitudinal skin incision centred over the radial styloid. In two patients from the total twenty-nine, there occurred a loss of fracture reduction which required no reoperation; one patient developed transient superficial radial sensory neuritis, which resolved within two months. There were no cases of infection, tendon rupture, tendon irritation or loss of digital motion or implant failure.
Tan [19] used a 2–3 cm longitudinal skin incision over the radial styloid as a surgical approach in inserting Micronail™. They indicated that the best place for bone window is over the radial styloid 3–4 mm proximal to the tip of the radial styloid between I. and II. extensor compartments. But in this position the risk of disruption of the tip of the radial styloid or breach of the scaphoidal facet of the articular surface of the radius is great, because the diameter of cannulated drill is 6.1 mm. Also, in this position, the danger of penetration into the radiocarpal joint is large. They stated that it is preferable to make the starting point for the bone window to the radial edge of the II. extensor compartment in case of dorsal dislocation of the distal fragment and on the ulnar edge of the I. dorsal compartment in case of volar dislocation. They presented a prospective clinical study using Micronail™ on 23 patients with unstable fracture of the distal radius. In two patients, there was a slight re-dislocation but it required no reoperation. In one patient, two weeks after surgery, there was a collapse of the fracture - which was comminuted - that required open reduction and treatment with volar plate osteosynthesis. Three patients had temporary mild numbness in the innervations of the superficial branch of the radial nerve, which disappeared within two months after surgery. No patient had irritation or injury in soft tissue or any infectious complications.
Dantuluri [4] used the same approach, but the bone window was placed 5 mm proximal to the tip of the radial styloid between I. and II. extensor compartments and pointed out how the cortical entry point of Micronail must be proximally enough to avoid disruption of the tip of the radial styloid or breach of the scafoidal facet of the articular surface of the radius. At the same time, it must not be too proximally so as to avoid nonsubchondral displacement of the fixed-angle locking screws. Then, he extended cortical window about 0.5 cm proximally while preparing a channel of a suitable size for Micronail with the aid of rasps. Shin [16] described the same surgical approach with the placement of the cortical window between I. and II. extensor dorsal compartments without stating the proper distance from the tip of the radial styloid. In these studies, the angle in the transverse plane, in which the implant is to be implemented, was not mentioned.
In this anatomical study, in 89 % of the attempts, in which Micronail™ was placed only 5mm from the tip of the radial styloid, there was penetration to the radiocarpal joint. During rasping, almost always a minor extension in cortical window proximally occurred, which makes the distal end of Micronail™ be more proximally than the original bone entry point. This explains why there was no screw penetration to the radiocarpal joint space in the aforementioned works. In our study, the final placement of the distal end of the implant was exactly in the original entry point.
In our clinical study, 31 patients were treated with Micronail and other 31 patients with volar locking plate (APTUS). Micronail method has better outcomes 6 weeks after operation than treatment with volar plate fixation. Three and 12 months after operation, there were no significant differences in the clinical outcomes between both groups. Radiological outcomes of both groups were excellent and almost identical. One patient, who was treated with Micronail, developed transient superficial radial sensory neuritis, which resolved within 6 weeks. One patient, who was treated with volar locking plate, developed a minor superficial infection with delayed wound healing requiring oral antibiotics. Also in this group, one patient had extensor pollicis longus tendonitis, for which we had to remove the volar plate 6 months after the primary surgery. There were no cases of neuropathy, deep infection, reflex sympathetic dystrophy or mal-union in either group [15].
Ilyas [6] treated ten patients with AO Type A and C distal radius fractures with an intramedullary nail (MICRONAIL™). There were two cases of transient superficial radial sensory neuritis and 3 cases of screw penetration into the distal radioulnar joint (DRUJ), 1 leading to symptomatic late DRUJ arthritis. There were no cases of infection, tendon injury, hardware failure or removal. He concluded that the treatment of the displaced distal radial fractures with Micronail can result in good functional outcome, but a high incidence of complications. In our study, there was no case of penetration to DRUJ in all positions of Micronail in all trials.
Brooks [2] described the insertion technique of the implant Dorsal Nail Plate (Hand Innovations LLC, Miami, FL, USA). Indications and contraindications of the use of this implant are the same as Micronail™. The insertion of the nail needs 3–4 cm skin incision on the dorsal side of the distal radius over Lister prominent. After preparation of the superficial branch of the radial nerve, EPL tendon is released and Lister tubercle is removed. The cortical window is placed in the proximal fragment in parallel with III. extensor compartment. The distal edge of implant has to be 4 mm from the radiocarpal joint line and just sit on the dorsal cortex. Using Micronail™, however, skin incision is smaller, the EPL tendon is not released and Lister tubercle is not removed. Plate portion of the implant Dorsal Nail Plate remains on the dorsal surface of the distal radius, which can lead to extensor tendon injury.
Street [18] stated that intramedullary fixation of forearm fractures heals faster because of the greater implant stability and the preservation of periostal blood supply. In addition, a smaller skin incision with minimal soft tissue trauma results in shorter operating-time and better cosmetic results. With intramedullary fixation, it is not necessary to mobilize or cut the surrounding muscles, in contrast to the plate fixation through volar approach, thus avoiding any violation of the perfusion of the distal fragment [17].
In comparison with plate fixation, Micronail has fewer complications. Among the disadvantages of dorsal plate fixation is the need for extensor tendon mobilization; the risk of extensor tenosynovitis; the risk of tendon rupture in case of which it is likely to do an additional operation to extract the plate (according to some studies, in 30-35 % of the cases) [1, 12, 13, 16, 20]. Other complications of plate osteosynthesis include: an extensive surgical approach; interruption of periostal blood supply and the risk of re-fracture at the end of the plate [8]. All of these complications are unlikely when Micronail is used.
CONCLUSION
Intramedullary fixation with Micronail™ is a minimally invasive method that gives excellent results with minimum operation risks if the right indication is decided upon and the insertion of the implant is done in a proper manner. On the other hand, Micronail™ is designed to treat only extra-articular and simple articular fractures of the distal part of radius, which is a significant limitation for its using.
There are no financial relationships, conflict of interests, or competing interests that may potentially influence the results of the research or scientific judgement.
Adel Safi, MD
adel.safi@seznam.cz
Článek byl recenzován a přijat do tisku v roce 2013. Vzhledem k technických a organizačním problémům redakce byl tiskem vydán v roce 2014.
Za problémy se redakce autorům omlouvá.
Redakce časopisu Úrazová chirurgie
Sources
1. AXELROD, T.S., MCMURTRY, R.Y. Open reduction and internal fixation of comminuted intraarticular fractures of the distal radius. J Hand Surg Am. 1990, 15, 1–11.
2. BROOKS, K.R., CAPO, J.T., WARBURTON, M. et al. Internal fixation of distal radius fractures with novel intramedullary implants. Clin Orthop. 2006, 445, 42–50.
3. CHUNG, K.C., WATT, A.J., KOTSIS, S.V. et al. Treatment of unstable distal radial fractures with the volar locking plating system. J Bone Joint Surg Am. 2006, 88, 2687–2693.
4. DANTULURI, P.K. Minimally invasive surgical fixation of distal radius fractures. In: Scuderi GR, Tria AJ, editors. Minimally invasive surgery in orthopedics. New York: Springer, 2010, 109-121.
5. HANUS, M., TRČ, T., HANDL, M. Využití funkční léčby v terapii zlomenin distálního radia. Acta Chir Orthop Traumatol Cech. 2009, 76, 116–120.
6. ILYAS, A.M., THODER, J.J. Intramedullary fixation of displaced distal radius fractures: a preliminary report. J Hand Surg Am. 2008, 33, 1706–1715.
7. KOENIG, K.M., DAVIS, G.C., GROVE, M.R. et al. Is early internal fixation preferred to cast treatment for well-reduced unstable distal radial fracture? J Bone Joint Surg Am. 2009, 91, 2086–2093.
8. MACINTYRE, N.R., ILYAS, A.M., JUPITER, J.B. Treatment of forearm fractures. Acta Chir Orthop Traumatol Cech. 2009, 76, 7–14.
9. MACKENNEY, P.J., McQUEEN, M.M., ELTON, R. Prediction of instability in distal radial fractures. J Bone Joint Surg Am. 2006, 88, 1944–1950.
10. MASAO, N., KENICHI, T., HIDENORI, S. et al. Prospective study of distal radial fractures treated with an intramedullary nail. J Bone Joint Surg Am. 2011, 93, 1436–1441.
11. NIEMEYER, P., HAUSCHILD, O., STROHM, P.C. et al. Fracture treatment in the elderly. Acta Chir Orthop Traumatol Cech. 2004, 71, 329–338.
12. ROZENTAL, T.D., BEREDJIKLIAN, P.K., BOZENTKA, D.J. Functional outcome and complications following two types of dorsal plating for unstable fractures of the distal part of radius. J Bone Joint Surg Am. 2003, 85, 1956–1960.
13. ROZENTAL, T.D., BLAZAR, P.E., FRANKO, O.I. et al. Functional outcomes for unstable distal radial fractures treated with open reduction and internal fixation or closed reduction and percutaneous fixation. J Bone Joint Surg Am. 2009, 91, 1837–1846.
14. ROZENTAL, T.D., BLAZAR, P.E. Functional outcome and complications after volar plating for dorsally displaced unstable fractures of the distal radius. J Hand Surg Am. 2006, 31, 359–365.
15. SAFI, A., HART, R., TĚKNĚDJANŽJAN, B. et al. Treatment of extra-articular and simple articular distal radial fractures with intramedullary nail versus volar locking plate. J Hand Surg Eur. 2013, 38, 774–779.
16. SHIN, E.K., JUPITER, J.B. Current concepts in the management of distal radius fractures. Acta Chir Orthop Traumatol Cech. 2007, 74, 233–246.
17. SHORT, W.H., PALMER, A.K., WERNER, F.W. et al. A biomechanical study of distal radial fracture. J Hand Surg Am. 1987, 12, 529–534.
18. STREET, M.D. Intramedullary Forearm Nailing. Clin Orthop. 1986, 212, 219–230.
19. TAN, V., CAPO, J. Distal radius fracture fixation with an intramedullary nail. Tech Hand Up Extrem Surg. 2005, 9, 195–201.
20. WILLIS, A.A., KUTSUMI, K., ZOBITZ, M.E. et al. Internal fixation of dorsally displaced fractures of the distal part of the radius. J Bone Joint Surg Am. 2006, 88, 2411–2417.
Labels
Surgery Traumatology Trauma surgeryArticle was published in
Trauma Surgery

2013 Issue 3
- Possibilities of Using Metamizole in the Treatment of Acute Primary Headaches
- Metamizole at a Glance and in Practice – Effective Non-Opioid Analgesic for All Ages
- Metamizole vs. Tramadol in Postoperative Analgesia
- Spasmolytic Effect of Metamizole
- Metamizole in perioperative treatment in children under 14 years – results of a questionnaire survey from practice
-
All articles in this issue
- Surgery treatment intraarticular fractures of proximal humerus
- Humerus head osteonecrosis in surgical treatment intraarticular fractures of proximal humerus by PHILOS plate
- Injury of soft tissues as limiting factor in treatement fractures of lower leg
- Micronail Insertion into Cadaver Distal Radius: A Study of Insertion Location, Rotation and Screw Articular and Cortical Penetration
- Trauma Surgery
- Journal archive
- Current issue
- About the journal
Most read in this issue
- Humerus head osteonecrosis in surgical treatment intraarticular fractures of proximal humerus by PHILOS plate
- Injury of soft tissues as limiting factor in treatement fractures of lower leg
- Surgery treatment intraarticular fractures of proximal humerus
- Micronail Insertion into Cadaver Distal Radius: A Study of Insertion Location, Rotation and Screw Articular and Cortical Penetration
