Addressing of trochanteric femoral fractures using a revision femoral stem with a cervicocapital prosthesis – coxofemoral by-pass
Authors:
Jan Káňa
Authors‘ workplace:
Ortopedicko-traumatologické oddělení nemocnice Nový Jičín
Published in:
Úraz chir. 26., 2018, č.2
Overview
The aim of this work is to introduce the methods used by us in addressing trochanteric fractures of femur. The fractures of the trochanteric massif are the cause of hospitalization in nearly 20 of patients admitted to our department for curing a fracture. The treatment is currently almost exclusively surgical. However, the results are not satisfactory and proximal femoral fractures are burdened with up to 30 mortality within 1 year of injury. Currently, a proximal femoral nail is usually used to allow correct fracture stabilization, but some patients are not supposed to be able to relieve the loaded extremity and there is a higher risk of failure. Therefore, the authors present their concept of a „palliative“ solution to these fractures using a revision stem and a femoral head replacement, where cervicocapital replacement is used in biologically elderly patients and the condition is reversed by total revision endoprosthesis in biologically younger patients. I consider this solution to be fast, efficient and affordable. In the given cohort then, with better survival rates against standard operations, I consider it at least a full-fledged alternative to osteosynthesis.
Keywords:
Trochanteric femoral fractures – coxofemoral bypass – cervicocapital prosthesis – revision stem – proximal femoral nail
Aim of the work
The aim of our study is to point out the borderline possibility of solving complex, unstable and pathological fractures in the trochanteric region using the revision femoral stem – in the literature this technique is called coxofemoral bypass [4, 11, 12, 14] and points to the advantages of this technique consisting in the possibility of earlier limb load and points to the limits of this technique.
Introduction
Proximal femoral fractures are a global social issue and a challenge for traumatology. Their incidence over the last decade has increased significantly [1, 2, 7, 9]. This is related to the increase in life expectancy and the occurrence of not only osteoporosis in older age, but also a worse motor skills of the elderly people. This is a typical fracture associated with older age.
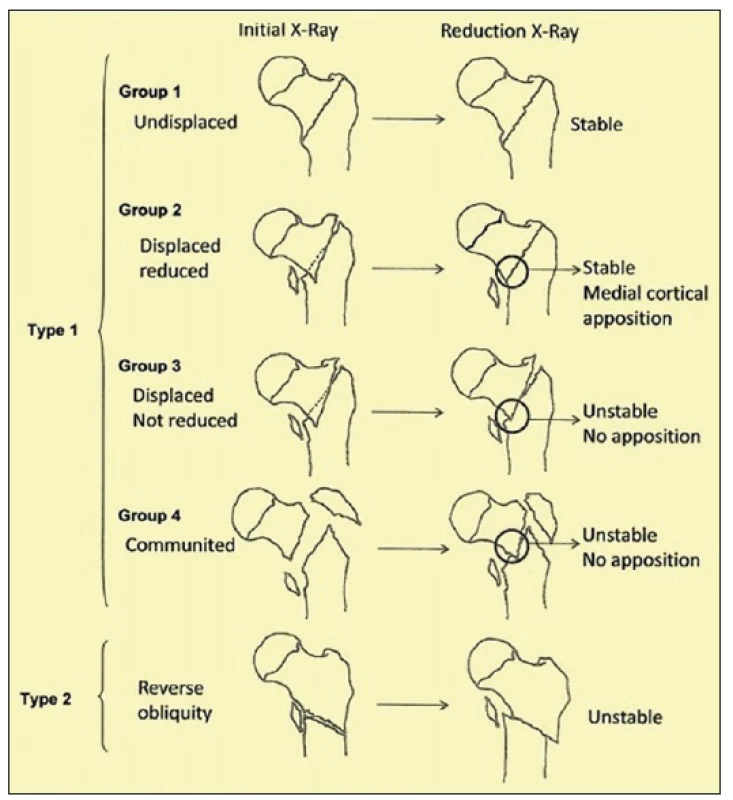
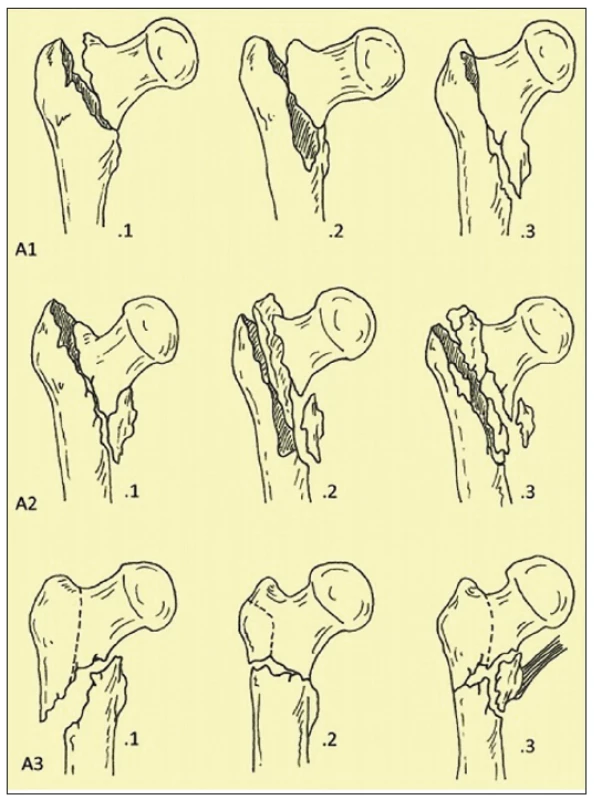
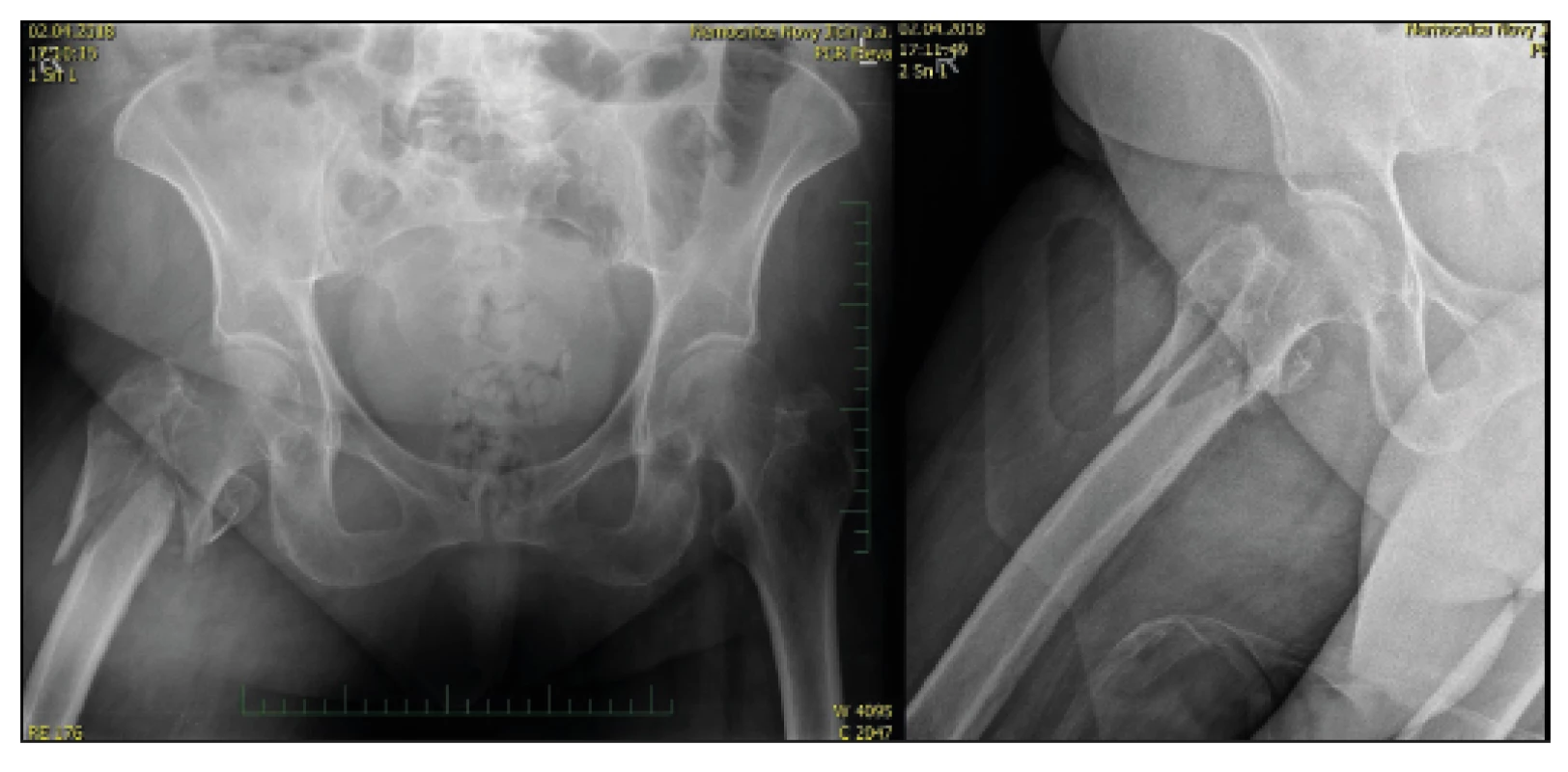
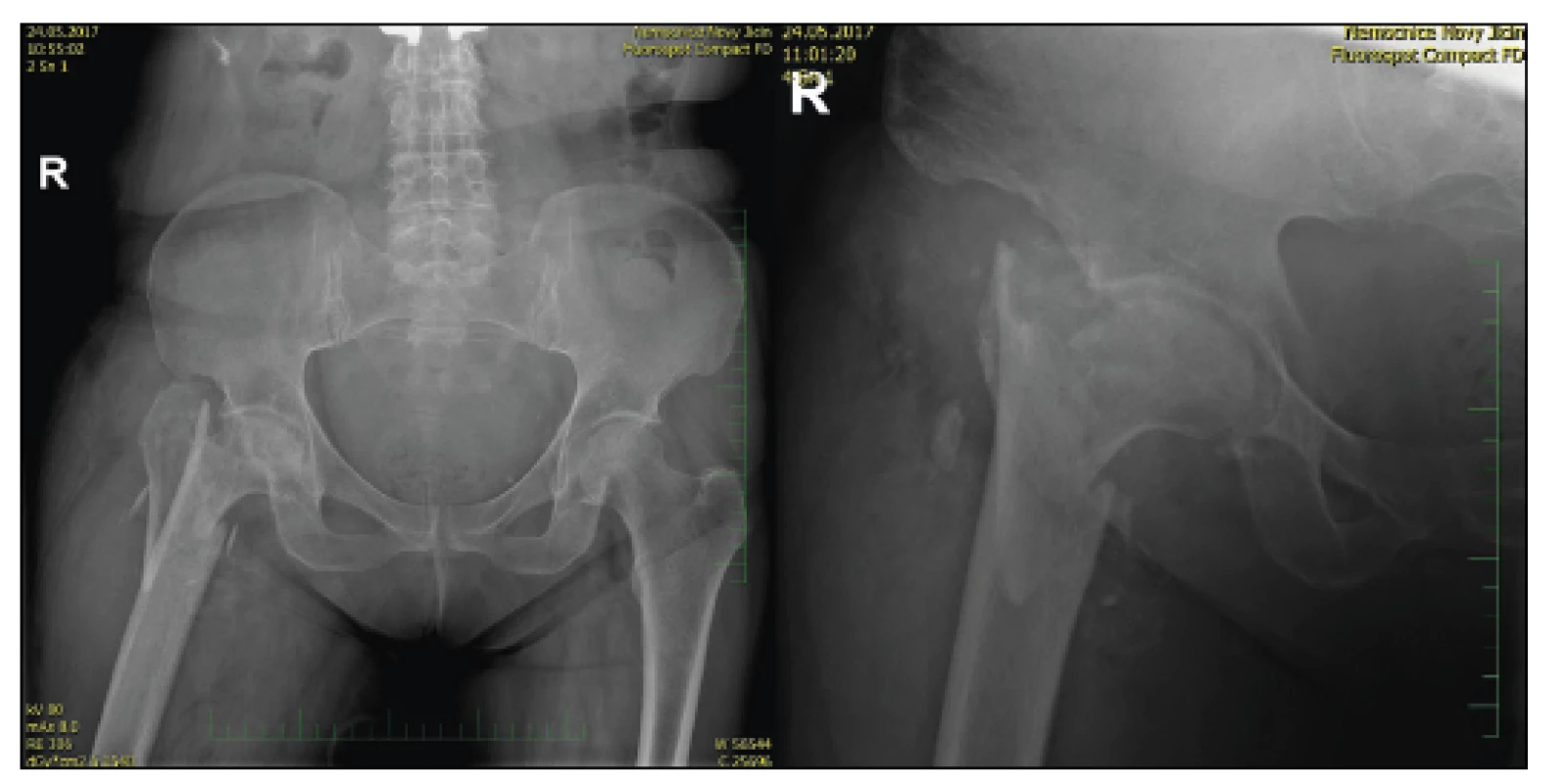
In our department, they constitute a significant part of hospitalizations for injuries and their incidence increases constantly. In 2017, out of 502 fracture surgeries, 183 were proximal femoral fractures - which fully corresponds to the data reported in literature [5]. In our group, the average age of patients with a proximal femoral fracture was 76.3 years with a range of 32 to 96 years. Women were represented in 74 . The solution to these fractures is almost exclusively surgical, when we usually use the proximal femoral nail - PFN (Medin event Synthes or Zimmer). Fractures are divided historically in accordance with the established classification by Ewanse [3] (Fig. 1) and we currently we use AO classification [1, 7] (Fig. 2), when trochanteric fractures are classified accordingly as 31-A1 to 31-A3.
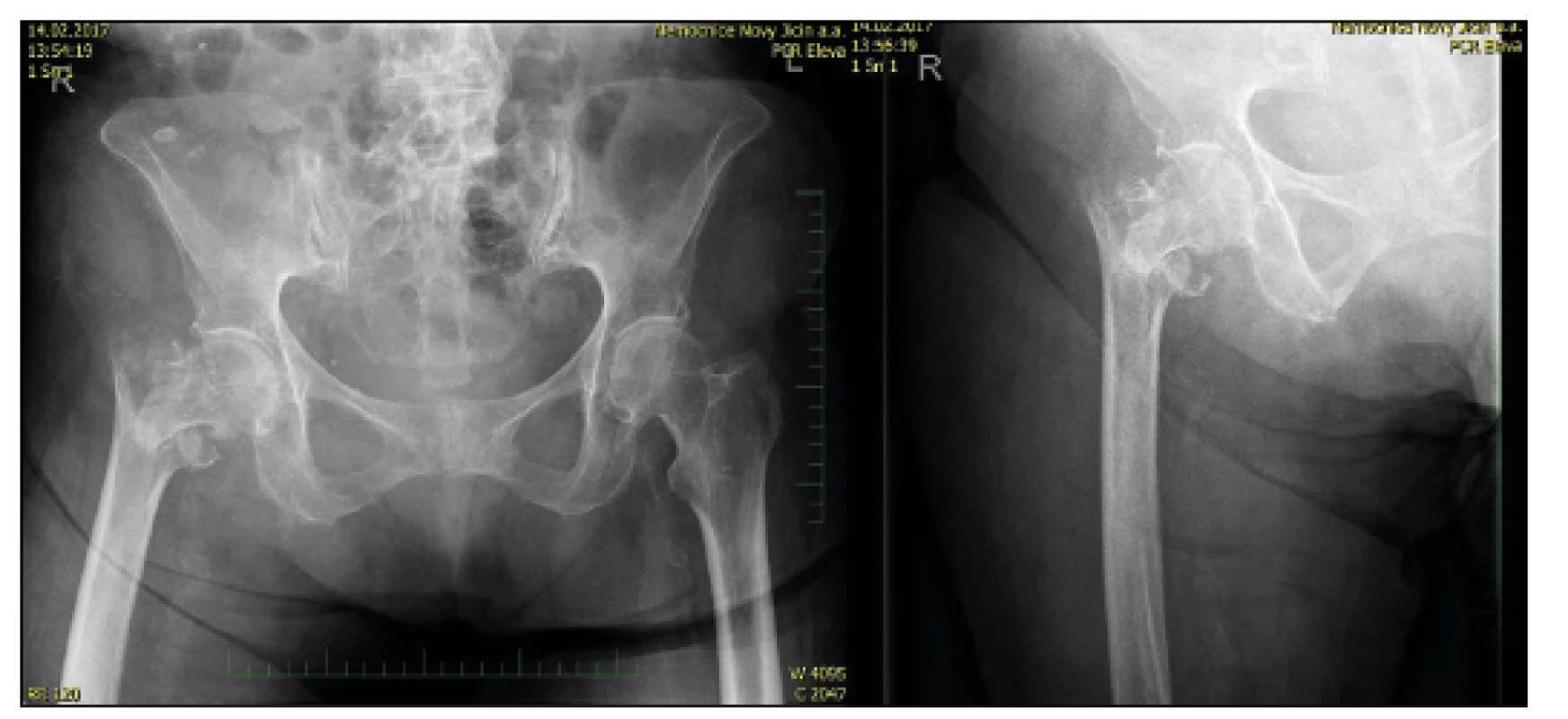
In particular, the unstable fractures pose the most significant issue (A22, A23, A33). In our consideration of the use of a revision femoral stem we derived from experience with revision endoprosthetics and with the awareness of the possibility of faster mobilization and higher stress during post-operative rehabilitation in cervicocapital fractures [11, 12, 14] and therefore in the case of major comminutions and in case of pathological fractures we did not proceed with reconstruction, but replaced the proximal part of the CKP fracture using a long-revision Centrament stem from Aesculap (Fig. 3).
Material and methods
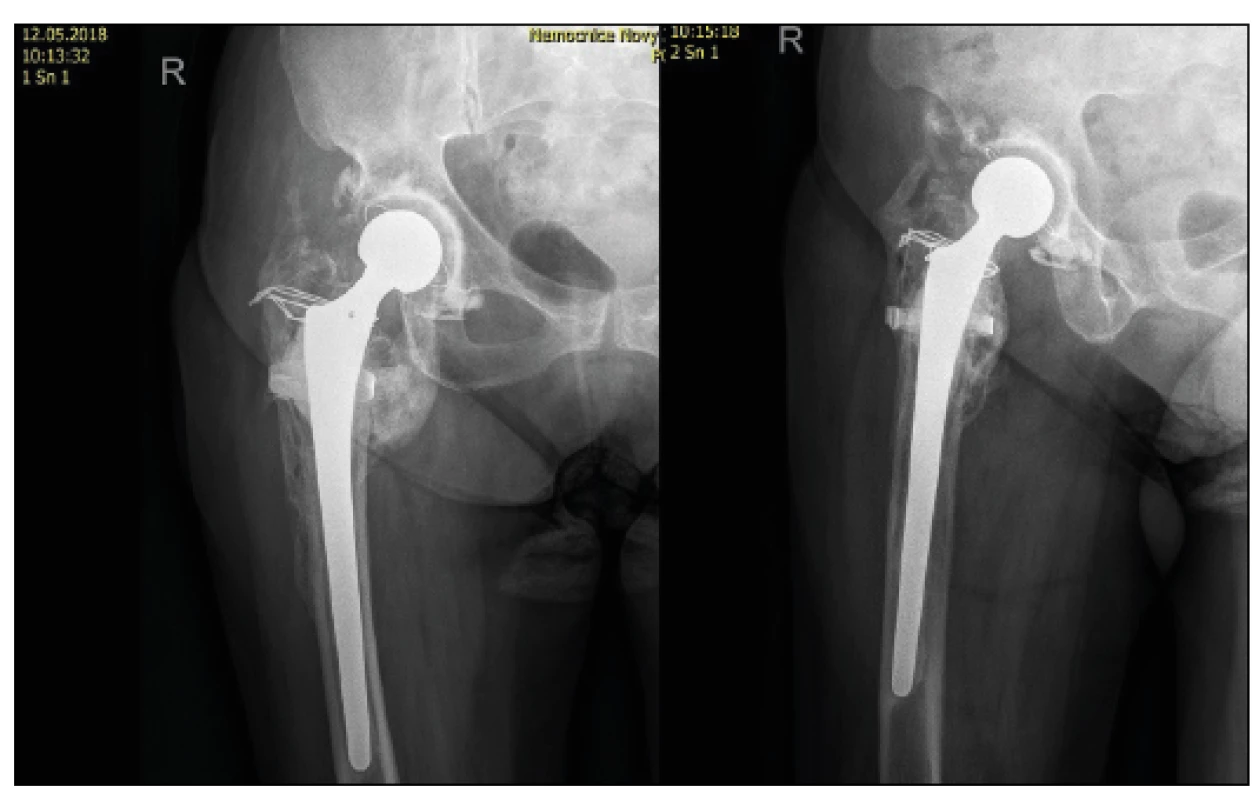
In 2017, we treated 113 patients with trochanteric fracture using the proximal femoral nail. Mechanical failure (penetration of nails into the head, non-union) occurred in 3 cases (2.7 %). In five patients, however, we chose the proximal femoral replacement method for an unfavorable situation on an X-ray image. These were head necrosis conditions, or in case of pathological fracture in the terrain of osteolytic focus and in the case of biomechanically unfavourable fragmentation zones in the trochanteric region. We used the Centrament revision stem, which is firmly fixed in the femoral diaphysis by bone cement, and the trochanteric region or muscle group area is fixed to the stem using the Orthocord suture (Fig. 4, 5), which has proven to be better compared to the wire loop.
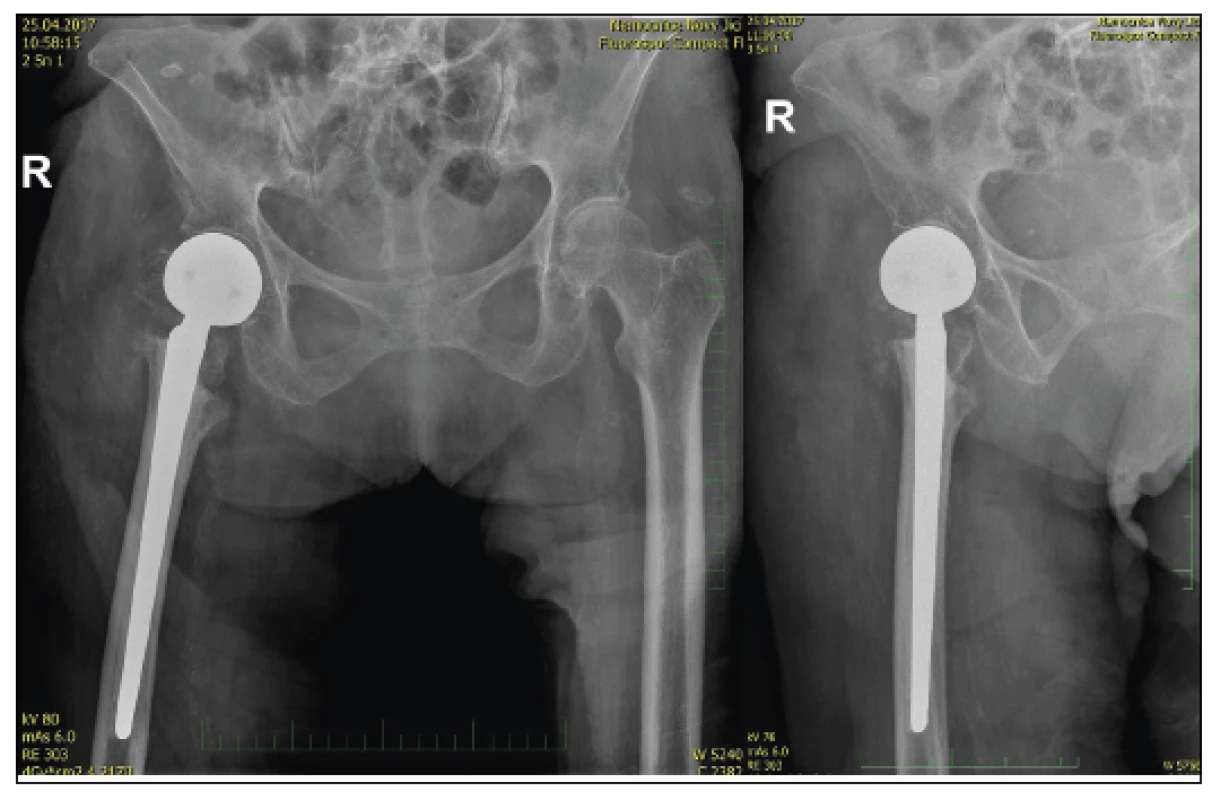
The Centrament stem has a diameter of 12 m and a length of 220 m. Thanks to our experience with TEP reimplants, we know that 2 diameters of the femoral shaft - i.e. approx. 7cm are sufficient for fixing the same. Therefore, we are able to solve fractures with a line of up to about 14–15 m distally from the apex of the greater trochanter. It was a small group where the age variance was from 58 years (pathological fracture in the osteolytic process in the intertrochanteric region) up to 87 years in a patient with a fragmentation zone and the presumption of no relief in postoperative verticalization. The higher proportion of women in the cohort (⅘) corresponds to the usual distribution in the population. The average period of hospitalization was 7 days followed by relocation to the aftercare department. The key to success is an early verticalization, preferably the first postoperative day. Conversely, due to the damaged insertion of the gluteal muscles and the refixation of the trochanter, we try to reduce the deeper sitting position, which causes significant fixation stress. We make an X-ray in all patients on the first postoperative day and then in about 8 weeks on the ambulance. Further monitoring depends on the patient›s condition.
Surgical technique
Usually we operate on healthy hip using standard, modified, lateral (Bauer) approach. After exposing the proximal femur, we try to protect the gluteal muscles as much as possible and revise the fracture area, where the stable fragment of the diaphysis and part of the trochanteric massif with the muscle insertion are the most important for us. If the line reaches the subtrochanteric region or if we have doubts about the quality of the bone, then we insert the diaphysis cerclage to reinforce it as in reimplantation (Fig. 6, 7, 8, 9).
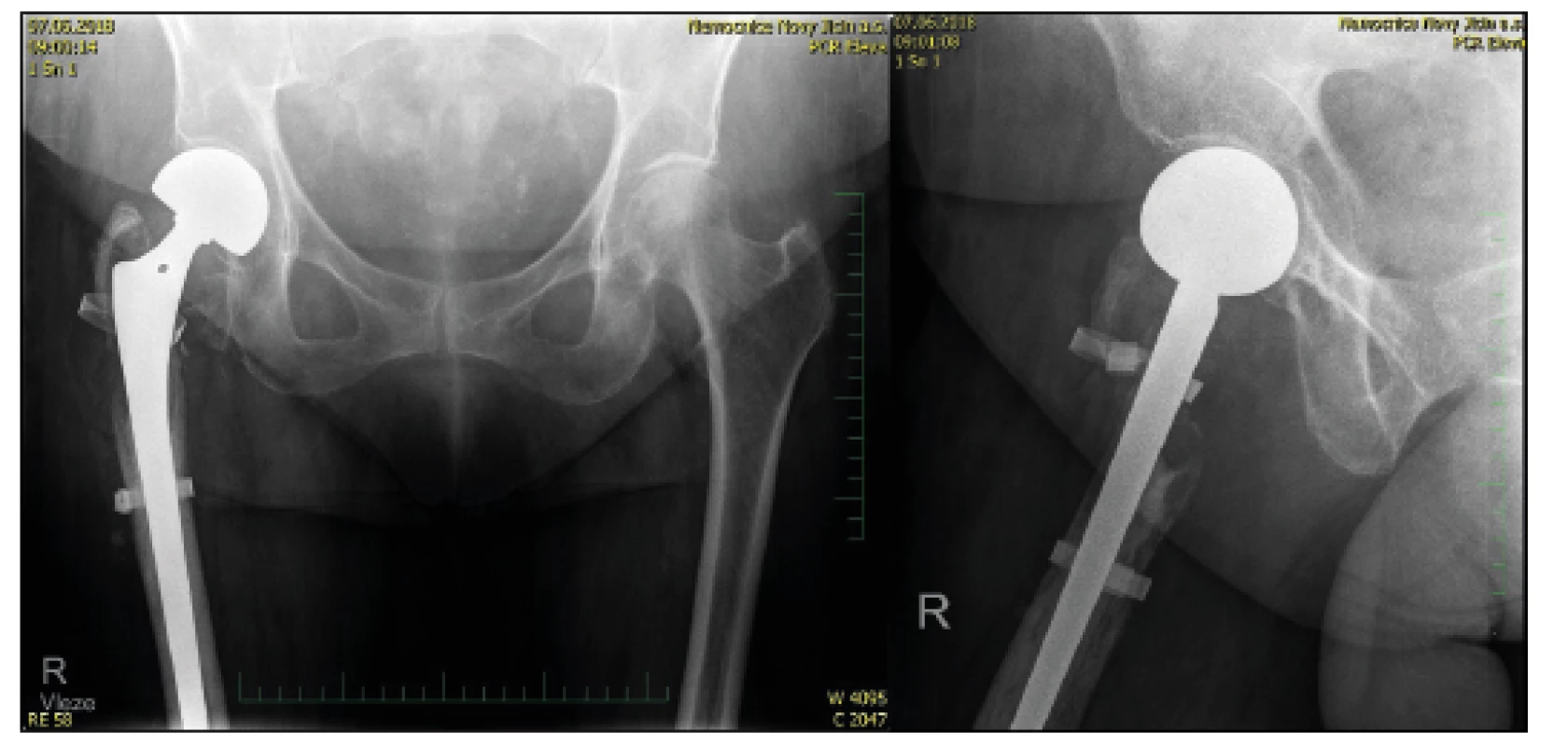
We subsequently extract the head and measure the acetabulum diameter as with CKP implantation, then use the calibrated drill bits to prepare the proximal femur, making sure during rasping that the bone bed matches the future need for implant embedding. We estimate the length of the limb and adequate muscle tone by using a test insertion without cement, indicating the length of the prominent part of the stem - the sterile fix. Then we cement the original stem with the use of a bone plug from the head and, after the cement has solidified, we deploy the CEP modular head and repose. Careful reconstruction is required - fixation of the trochanteric area to the stem and suture over the anatomical layers. Usually we remove the drain on the first postoperative day, when we start with verticalization and relief according to the patient‘s capabilities.
Results
The statistical evaluation of the cohort is not possible due to the small number of patients, therefore we will focus on individual cases. Of the patients treated with this technique, 4 were healed. One patient presented an insufficient insertion of the stem as a result of a technical fault during surgery and subsequent muscle hypertension, which led to repeated luxations with the necessity to extract the prosthesis and leave the resection arthroplasty - this patient shows minimum mobility - transfer to personal hygiene, otherwise having to use a wheelchair. The remaining patients were healed and suitable for verticalization with full load - or walking on crutches. In the patient with a pathological fracture resulting from metastatic affection, the underlying disease led to death after six months, but the treatment of the pathological fracture by resection of the site and revision stem enabled the patient to have an early dimission (5th day) and painless walking with a stick. There was no superficial or deep infection observed in the cohort.
Discussion
Proximal femoral fractures are an issue of contemporary traumatology from several points of view. This is a predominantly socio-economic problem where patients are usually older and require post-treatment after surgery. The fracture of the proximal femur always affects their health condition and, above all, their quality of life [2, 5, 7].
The technical solution using slip implants, whether PFN or DHS, in most cases ensures fracture stabilization, but the problem with osteoporosis persists (implants with the possibility of injecting bone cement into the head are on the market, but we do not have experience with them in our department). Furthermore, there may be problems with the stability of the osteosynthesis in the area of a bone of a lesser quality. In addition, the relief options are considerably limited by the overall patients´ condition. Therefore, in patients with a high risk of osteosynthesis failure and the need for early mobilization, we have recently chosen a revision femoral stem combined with a modular CKP head - i.e. coxofemoral by-pass. This surgery is not technically demanding, moreover, it allows almost instantaneous verticalization with loading until a feeling of pain. It is only necessary to carefully measure the length of embedding of the stem into the distal fragment in order to restore the length of the limb and adequate pelvifemoral muscle tone.
In the literature, the need for a correct surgical technique (valgization of the proximal fragment corresponding to the angle of the hip screw, restoration of the Adams arch, adequate compression of the fragments) is reported for osteosynthesis [3, 7, 8], but we believe that primarily unstable fractures with a comminuted zone are always assocciated with risk in the case of use of an exact surgical technique. These are often polymorbid patients, where the surgical solution needs to be fast and preferably once and for all. Therefore, we believe that the solution using a cement inspection stem meets these conditions. In addition, the solution is also advantageous in terms of economics, when the price of the stem - head - cement assembly is lower than that of the imported PFN stems. It is clear that this is the first experience with the method, but our results and especially the short immobilization of patients seems to be a great advantage of this technique. European literature on the use of the revision stem in primary fractures is relatively poor and comparing the technique with the nail is problematic because we use it in cases where the possibility of nail failure and therefore a biomechanically unfavourable situation is assumed. However, we consider 80 % healing a good result as well as 20 % postoperative mortality, which is always influenced by general conditions of the patients rather than the surgical technique.
Conclusion
The indication of the strategy for solving complex trochanteric fractures depends on the presumption of the patient survival. In relatively healthy patients, we always try to maintain their own joint with the assumption of healing. In polymorbid patients and patients with severe hip affection we prefer a palliative solution - by replacing the proximal femur with a revision cement implant that will allow early mobility and eventual return to the home environment. However, this solution is not suitable for patients with a presumed longer survival; here, if a proximal femoral replacement is needed, we choose the revision stem along with the acetabular replacement - implantation of the TEP hip joint with revision/tumorous stem.
MUDr. Jan Káňa
Sources
1. BARTONÍČEK, J., BARTOŠKA R. Trochanterické zlomeniny – anatomie a klasifikace. Rozhl Chir. 2013, 92, 581–588. ISSN 0035-9351
2. BURGET, F., PLEVA, L., KUDRNA, K. et al. Distribuce zlomenin horního konce stehenní kosti v závislosti na roční době a počasí. Acta Chir Orthop Traumatol Cech. 79, 2012, 140–143. ISSN 0001-5415
3. ČECH, O., STRYHAL, F. Moderní osteosyntéza v traumatologii a ortopedii. 1. vyd. Praha : Avicenum, 1972. 273 s. ISBN 80-6709.789-5
4. DAS, S., KALAMBE, H., HANDRALMATH, S. Comparative study of unstable intertrochanteric fracture treatment by trochanteric femoral nail versus hip hemiarthroplasty. International Journal of Orthopaedics Sciences. 2017, 3, 548–552. ISSN 2395-1958
5. DOKLÁDALOVÁ P., MAJERNÍČEK M., VACULÍK J. et al. Výsledky po operacích zlomenin proximálního femuru – komplikace, letalita. Acta Chir Orthop Traumatol Cech. 2017, 84, 424–430. ISSN 0001-5415
6. DOUŠA P., BARTONÍČEK J., PAVELKA T. et al. Ipsilaterální zlomeniny proximálního konce a diafýzy femuru. Acta Chir Orthop Traumatol Cech. 2010, 77, 378–388. ISSN 0001-5415
7. DOUŠA, P., ČECH, O., WEISSINGER, M. et al. Trochanterické zlomeniny femuru. Acta Chir Orthop Traumatol Cech. 2013, 80, 15–26. ISSN 0001-5415
8. FALKENSAMMER, ML., BENNINGER, E., MEIER, C. Reduction Techniques for Trochanteric and Subtrochanteric Fractures of the Femur a Practical Guide. Acta Chir Orthop Traumatol Cech. 2016, 83, 300–310. ISSN 0001-5415
9. HOZA, P., HÁLA, T. PILNÝ, J. Zlomeniny proximálního femuru a jejich řešení. Med pro Praxi. 2008, 5, 393–397. ISSN 1214-8687
10. HRUBINA, M., SKOTÁK, M., LETOCHA, J. Osteosyntéza zlomenin proximálního femuru metodou DHS v terénu koxartrózy. Acta Chir Orthop Traumatol Cech. 2015, 82, 364–368. ISSN 0001-5415
11. MEDAGAM, NR., REDDY, B. Study of Effectiveness of Coxofemoral Bypass in Comparision to Proximal Femoral Nail in the Treatment of Unstable Intertrochanteric Fractures in the Elderly. Journal of Orthopaedics, Traumatology and Rehabilitation. 2018, 10, 19–22. DOI: 10. 4103/jotr.jotr_35_16
12. NAIK, LG., BADGIRE, KS, SHARMA, GM. et al. Treatment of unstable intertrochanteric fractures with cemented bipolar prosthesis – A prospective study. Indian Journal of Orthopaedics Surgery. 2017, 3, 27–30. ISSN 0019-5413
13. PAVELKA, T., HOUČEK, P., LINHART, M. et al. Osteosyntéza zlomenin horního konce diafýzy pomocí PFN-long. Acta Chir Orthop Traumatol Cech. 2007, 74, 91–98. ISSN 0001-5415
14. SINNO, K., SAKR, M., GIRARD, J. et al. The effectiveness of primary bipolar arthroplasty in treatment of unstable intertrochnateric fractures in elderly patients. N Am J Med Sci. 2010, 12, 561–568. ISSN 0002-9629
Labels
Surgery Traumatology Trauma surgeryArticle was published in
Trauma Surgery

2018 Issue 2
- Metamizole vs. Tramadol in Postoperative Analgesia
- Metamizole at a Glance and in Practice – Effective Non-Opioid Analgesic for All Ages
- The Importance of Hydration in Wound Healing
- Obstacle Called Vasospasm: Which Solution Is Most Effective in Microsurgery and How to Pharmacologically Assist It?
- Possibilities of Using Metamizole in the Treatment of Acute Primary Headaches
Most read in this issue
- Results of Achilles tendon rupture repair. Classical open approach versus percutaneous suture
- Complex Response of the Organism to Trauma
- Addressing of trochanteric femoral fractures using a revision femoral stem with a cervicocapital prosthesis – coxofemoral by-pass
- Abdominal trauma and wandering spleen - case report

