-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
An audit of the i-gel supraglottic airway for general anaesthesia with spontaneous and controlled ventilation – the effect of ventilation mode and operator experience on device performance
Audit použití supraglotické pomůcky i-gel při celkové anestezii se spontánní a řízenou ventilací – vliv ventilačního režimu a zkušenosti lékaře na sledované parametry
Cíl studie:
I-gel je relativně novou pomůckou k zajištění dýchacích cest. Některé jeho vlastnosti mohou podmínit větší úspěšnost a nižší výskyt pooperačních komplikací ve srovnání s laryngeální maskou.Typ studie:
Prospektivní observační studie (klinický audit).Typ pracoviště:
Anesteziologické oddělení oblastního výukového pracoviště.Materiál a metoda:
Provedli jsme prospektivní audit použití i-gelu u 96 pacientů a sledovali jsme úspěšnost zavedení, únik dýchací směsi v souvislosti s použitým ventilačním režimem a četnost výskytu pooperačních komplikací. I-gel byl zaváděn na operačním sále pro výkony obecné a cévní chirurgie, urologie a gynekologie. Sledované parametry zahrnovaly demografické údaje pacientů a anesteziologů, zavádění pomůcky, přítomnost krve nebo žaludeční tekutiny na pomůcce po vyjmutí a pooperační komplikace: bolesti v krku, bolesti jazyka, potíže při mluvení, potíže při polykání, nevolnost a zvracení. Srovnáván byl výkon specializovaných anesteziologů s lékaři v tréninku.Výsledky:
Spontánní ventilace byla zachována u 35 pacientů (36,5 %) se zavedeným i-gelem, u 61 výkonů (63,5 %) byla použita asistovaná nebo řízená ventilace. I-gel byl zaveden na první pokus u 86,5 % pacientů, na druhý pokus u 9,4 % případů a u 4,2 % pacientů byly nezbytné tři nebo více pokusů o zavedení. Malý únik směsi byl zaznamenán u 15,6 % výkonů. U 17,7 % pacientů byla nutná změna polohy po prvním zavedení i-gelu. Krev byla nalezena na 5,2 % pomůcek po vynětí. 9,4 % pacientů udávalo bolesti v krku po výkonu. Tato komplikace spontánně odezněla u všech pacientů do 48 hodin po operaci. Nebyl zaznamenán žádný rozdíl v úspěšnosti zavedení mezi zkušenými a nezkušenými anesteziology. Únik směsi byl častěji pozorován u řízené ventilace (p = 0,03).Závěr:
Pomůcku je relativně snadné zavést, je možné ji použít při spontánní i řízené ventilaci a byla dobře tolerována ze strany pacientů.Klíčová slova:
i-gel – laryngeální maska – komplikace
Authors: Donaldson William 1; Michálek Pavel 1,2; Pokorný Lukáš 1; Leyden Paul 1
Authors place of work: Department of Anaesthesia, Antrim Area Hospital, Antrim, United Kingdom/Northern Ireland 1; Klinika anesteziologie resuscitace a intenzivní medicíny, 1. lékařská fakulta UK a Všeobecná fakultní nemocnice, Praha 2
Published in the journal: Anest. intenziv. Med., 23, 2012, č. 2, s. 63-68
Category: Anesteziologie - Původní práce
Summary
Objective:
The i-gel supraglottic airway has features that may confer advantage over the standard laryngeal mask in terms of performance and postoperative complications.Design:
Prospective observational study (clinical audit).Setting:
Anaesthetic department of district general teaching hospital.Material and methods:
We carried out a prospective audit of 96 i-gel insertions in order to assess insertion success rate, airway leak associated with a mode of ventilation and postoperative complications. The i-gel was inserted in theatre settings for general surgery, gynaecology, urology and vascular surgical procedures. Data collected included patient and operator demographics, information about device insertion, the presence of blood or gastric fluid on the device after removal and postoperative complications: sore throat, sore tongue, difficulty speaking, difficulty swallowing, nausea and vomiting. The performances of experienced and inexperienced operators were compared.Results:
The i-gel was used with spontaneous ventilation in 35 (36.5%) of patients, while 61 (63.5%) of patients were ventilated with assisted or controlled mode. The device was inserted at the first attempt in 86.5% cases, at the second attempt in 9.4% and in 4.2% of patients three or more attempts were necessary. A minor leak was noted in 15.6% while in 17.7% of cases repositioning was required after insertion. The presence of blood on the device was noted in 5.2% of the patients and 9.4% of patients described sore throat postoperatively. No patients complained of sore throat at 48 hrs. There was no statistical difference between any variables between experienced and inexperienced operators. A leak was more often seen with controlled ventilation (P = 0.03).Conclusion:
The device proved relatively easy to insert, performed well under both spontaneous and controlled ventilation and was well tolerated by patients.Keywords:
i-gel supraglottic airway – laryngeal mask airway – complicationsIntroduction
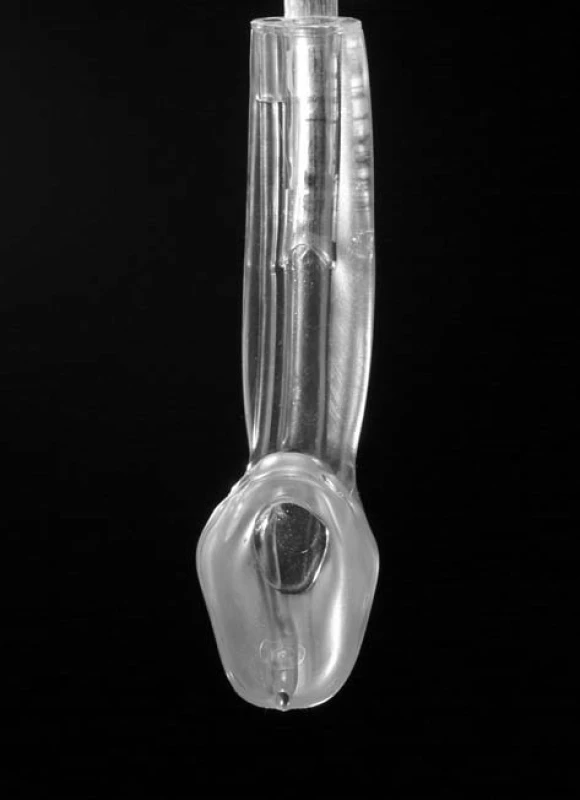
The i-gel [Intersurgical Ltd, Wokingham, United Kingdom] was introduced into clinical practice in the United Kingdom in January 2007. It is a disposable, supraglottic airway that comprises a non-inflatable cuff, bite block, epiglottis blocker and gastric channel (Figure 1). It is made from a compound that is thermoplastic and said to mould to the laryngeal anatomy, which it is designed to mirror.
Studies on both cadavers and in manikins have found it to be easy to insert [1, 2] and that it provides a good view of the glottic aperture when a fibreoptic scope is passed through it [1]. It has been suggested as a method of airway management in cardiorespiratory arrest [3] and as a device that can be used as a rescue device in “can’t intubate, can’t ventilate” situations [4]. The authors have used the i-gel as a conduit for fibreoptic intubation in expected difficult airways in both theatre and intensive care settings [5, 6] an in one patient with subglottic tracheal stenosis [7].
The goals of this prospective audit were to assess the success rate of device insertion, difference between spontaneous and controlled ventilation through this device, difference between experienced and inexperienced operators, frequency of traumatic insertion and the incidence of postoperative complications associated with the device, including sore throat and sore tongue, speaking and swallowing difficulties and postoperative nausea and vomiting.
Materials and methods
After Local Audit Committee approval a prospective audit was set up. This project was classified as a service evaluation and therefore not requiring Trust Ethical Committee approval. A proforma was devised for collection of data. Demographic data included age, sex, weight and American Society of Anesthesiologists (ASA) classification for the patient. Operator grade, number of previous i-gel insertions (0–10, 11–20, 21+) and number of insertions of any supraglottic device (0–10, 11–20, 21–5-, 50+) was recorded for the operator. Airway assessment comprised mouth opening (< 2 finger breadths (FB), 2–3 FB, > 3 FB), thyromental distance (< 6.5 cm, > 6.5 cm) and Mallampati classification (I, II, III, IV). For device insertion the size of i-gel used, number of attempts, presence or absence of a leak and whether repositioning was required were all recorded. Modes of ventilation used during the procedure – spontaneous, assisted or controlled – were also recorded. On removal, the presence or absence of blood on the device and whether the inner surface of the device was dry were both recorded. In the recovery area, 2 hrs after awakening, the patients were assessed by means of a questionnaire for sore throat, sore tongue, difficulty swallowing, difficulty speaking, nausea and vomiting – with a grading of none, mild, moderate and severe for each. Patients were also assessed for postoperative complaints at 24 h post procedure.
Data were entered into a database created using Filemaker Pro™.
All patients received standard anaesthetic monitoring (ECG, pulse oximetry and non-invasive blood pressure measurement). Induction was performed with 1–3 mg/kg propofol and fentanyl. Anaesthesia was maintained using sevoflurane and non-depolarizing neuromuscular blocking agents (atracurium or rocuronium) were administered to patients undergoing controlled ventilation.
Statistical analysis
The performance of experienced (consultants, staff grades) and inexperienced (trainees) operators was compared using Fisher’s exact test using the online statistical freeware (www.quantitativeskills.com). The same statistical method was employed for a comparison of audible leak between controlled and spontaneous ventilation through the i-gel. P values of less than 0.05 were considered significant.
Results
During the 3 month audit period 107 completed forms were received of which 96 were suitable for analysis – data were incomplete in the remainder. In total, 15 anaesthetists (8 doctors in training and 7 consultants/staff grades) participated in the audit.
Demographic data – patients
There were 83 women and 13 men, whose age ranged from 14 years to 87 years, with a mean of 45 years. The preponderance of female patients in the audit reflects the types of surgery performed in our hospital for which supraglottic airways are appropriate: mainly gynaecological and breast surgery. Weight ranged from 40 kg to 116 kg, with a mean of 72 kg. There were only 5 patients with an ASA grading of 3, the remainder being grade 1 or 2. No patients had mouth opening of less than 2 fingerbreadths, only 10 had a thyromental distance of less than 6.5 cm and 91 of the patients had a Mallampati classification of either I or II.
Demographic data – operators
All grades were represented, with the majority being middle to senior grade trainees – Table 1. Previous experience with the i-gel was fair: those who had previously inserted more than 21 devices made 65 insertions.
Tab. 1. Operator demographics 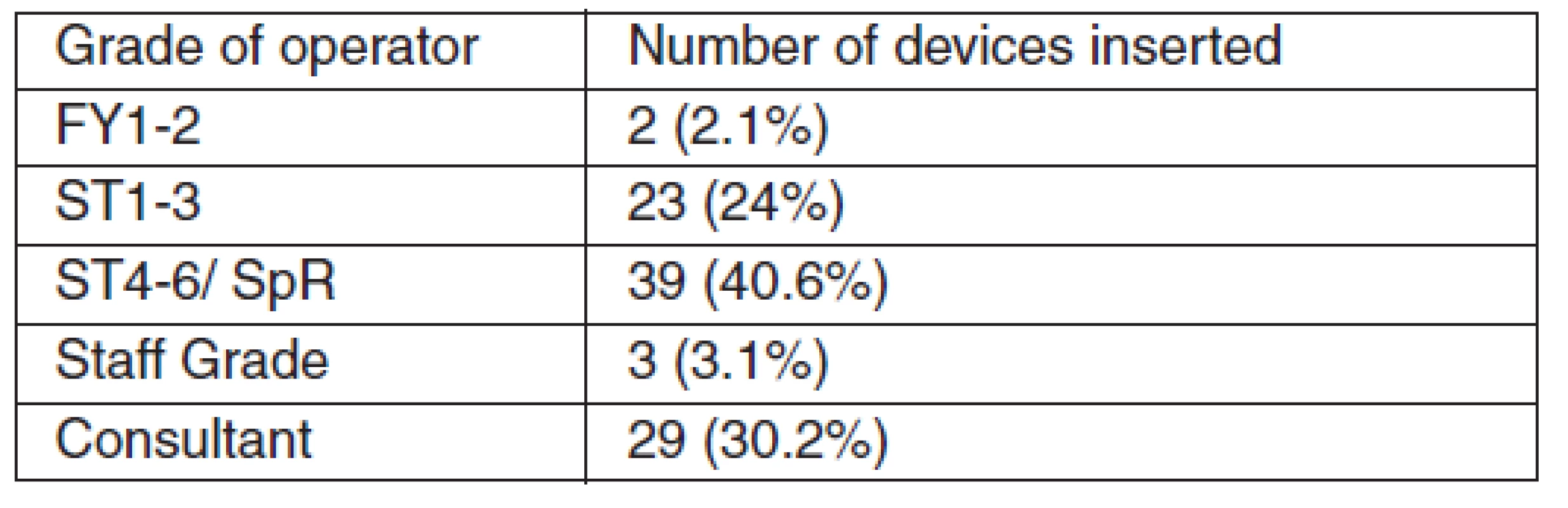
Legend: FY – Foundation Year trainee, ST – Specialty Trainee, SpR – Specialist Registrar Device insertion and removal
The i-gel was inserted at the first attempt in 83 (86.5%) cases, at the second attempt in 9 (9.4%) and in 4 patients three or more attempts were made (4.2%). In 15 patients (15.6%) there was a leak and in 17 patients (17.7%) the device required repositioning – Table 2. Only 35 patients (36.5%) were managed with spontaneous ventilation (SV), the remainder being managed with either Synchronised Intermittent Mandatory Ventilation (SIMV) or Intermittent Positive Pressure Ventilation (IPPV). The incidence of leak was significantly higher in the patients ventilated with controlled mode – 21.3% vs. 5.7%, respectively (P = 0.03) – Table 3. On removal there was blood on 5 devices (5.2%) and 82 were reported as having a dry inner surface (85.4%).
Tab. 2. Mode of ventilation and audible leak 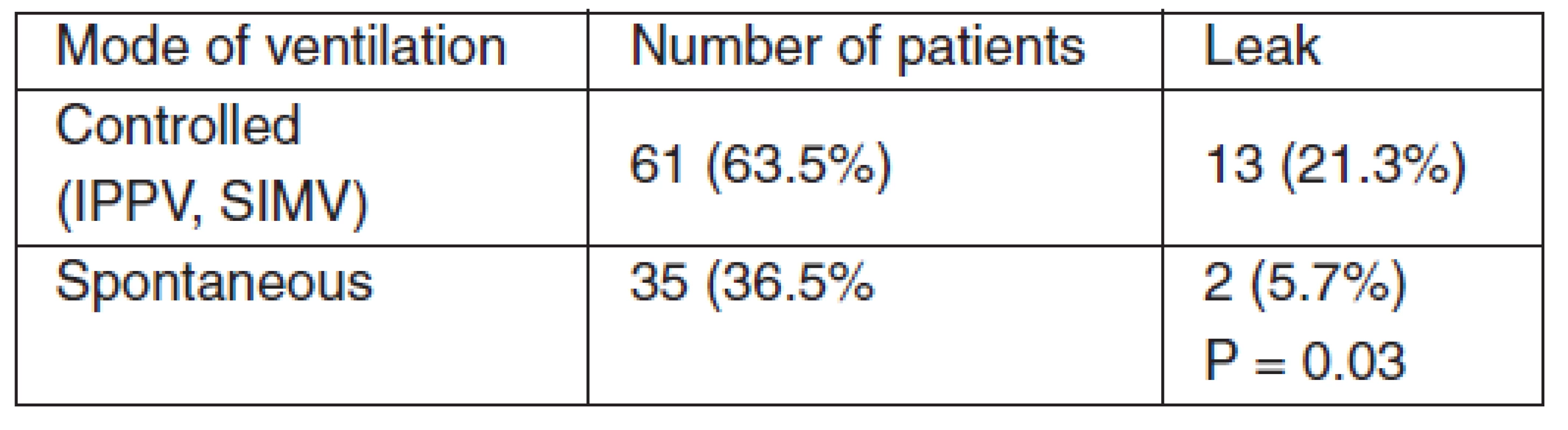
Tab. 3. Insertion attempts, leak and traumatic insertion: comparison between inexperienced and experienced operators 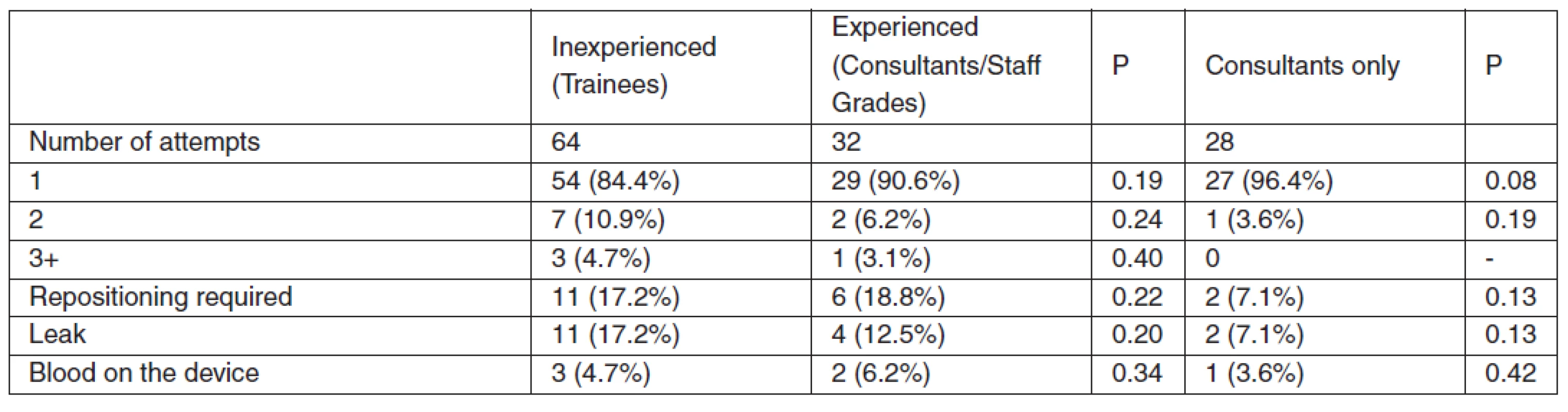
Postoperative assessment
Nine patients described sore throat (9.4%) of whom 7 (7.3%) had mild and 2 (2.1%) moderate symptoms. 4 patients described a sore tongue (4.2%) all of which reported mild symptoms. There were no reports of difficulty speaking wheras 4 (4.2%) patients reported mild difficulty in swallowing – Table 4. Nausea was reported by 10 patients (10.4%), 2 of whom described severe symptoms (2.1%), 1 moderate (1%) and 7 mild (7.3%). Vomiting was reported by 5 patients (5.2%), 3 cases being mild (3.1%) and 2 moderate (2.1%).
Tab. 4. Postoperative complications 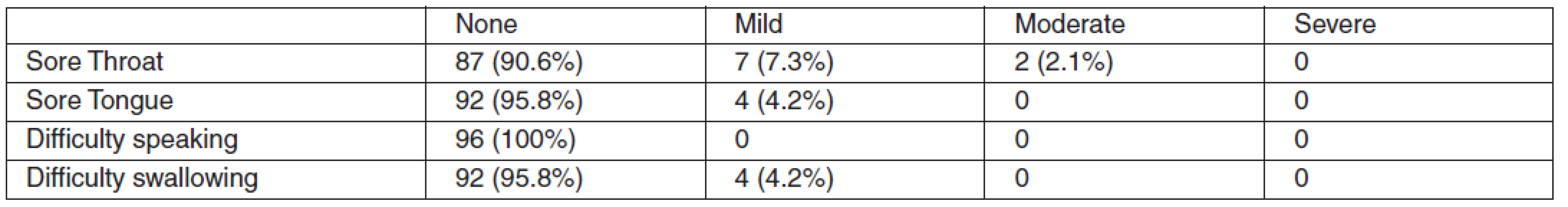
Discussion
This audit aimed to compare the i-gel to known standards for the device with which it is set to compete – the laryngeal mask airway. Since the audit was devised a prospective observational study in female patients has been published using the i-gel in 71 patients [8]. Another study evaluated size 4 i-gels in 100 non-paralysed patients and found the success rate of insertion to be over 90% with a very good percentage of glottic covering [9]. Our recent study compared the i-gel and Aura Laryngeal mask in 204 patients [10]. These studies, therefore, have become the standards to which we have compared our results. Studies involving the LMA have been used in other instances for comparison.
The device was inserted at the first attempt in 86.5% of cases, which is lower than expected. We feel this may be due to the larger depth of the bowl of the device: of those patients requiring reinsertion, 6 out of 13 (46%) had limited mouth opening and 8 of 13 patients (62%) had Mallampati scores of 2 or greater. Another factor was the relative inexperience of some of the operators: 5 of the 13 operators involved in repeated insertions had inserted less than 21 i-gels. The first descriptive study on the i-gel had a first time insertion rate of 97%, yet all of the devices in this study were inserted by senior anaesthesiologists [8]. If, in our audit, we look at ‘experienced operators’ alone (see Table 3) then our first time insertion rate is 90.3%. Excluding all but consultants gives a first time insertion rate of 96%. No opportunity was given in our audit for the assessment of adequate anaesthesia for insertion, for example jaw relaxation, and some of these insertions may have been in patients in too shallow anaesthesia for instrumentation of the airway.
A leak was present in 15 patients. Of these, in 7 patients the correct size of device as recommended by the manufacturers (based on the patient’s weight) [11] was not inserted. In each of these the i-gel inserted was a size too small, which may account for the leak found. Higher incidence of leak was seen in the patients with controlled ventilation. We suppose that in these patients a peak airway pressure exceeded seal pressure of the device. In 17 patients the i-gel required repositioning. Whilst there is some overlap with those in whom there was a leak, we feel inexperience was a factor here also: 9 of the 17 operators had inserted less than 21 devices. We did not evaluate seal/leak pressures of the device, however this parameter has been studied extensively in another studies. Most studies reported the i-gel seal/leak pressures between 24–28 cm H2O which is comparable with the rest of 2nd generation supraglottic airway devices [8,10].
Controlled ventilation was used in the majority (63.5%) of patients. All of the patients in Richez et al’s study were ventilated with intermittent positive pressure ventilation (IPPV) [8]. This represents an increased proportion compared with a large survey of laryngeal masks use in 11910 patients, where IPPV was employed only in 44% of patients [12]. The more frequent use of IPPV with the i-gel over the standard LMA is probably due to a combination of a gastric channel and a better perilaryngeal seal, which should improve its performance as a device for intermittent positive pressure ventilation.
Blood was present on 5 of the devices at removal, which may indicate traumatic insertion. Forceful insertion of the i-gel can even lead to tongue trauma [13]. We did not note any clinically significant aspiration of gastric contents. This has been reported with the i-gel: a case series reported 3 cases of significant gastric regurgitation and aspiration in one patient [14]. The incidence of aspiration with the LMA has been estimated as low as 0.02% [15]. Aspiration has also been reported with the LMA ProSeal airway device [16].
In comparison to Richez et al’s study, our results for postoperative complications differ widely. Whilst they reported only a short coughing episode and a transient moderate sore throat [8], our audit revealed a higher incidence of postoperative complications. The reasons for this are unclear: certainly our audit didn’t stipulate a standardised anaesthetic and therefore it is difficult to say whether the type of anaesthetic (for example, administration of antiemetic agents) may have played a part [17].
In our audit sore throat occurred with an incidence of 9.4%, the majority of which were mild. The incidence of sore throat with laryngeal masks varies widely: in one review from 4% – 50% [17]. In one study, the i-gel showed a lower incidence of postoperative sore throat and neck complaints than the classical disposable LMA [18].
The incidence of nausea was 10.4% and the incidence of vomiting was 5.2%. These data are probably not related to the i-gel use but to the general anaesthesia itself. The incidence of nausea and vomiting post anaesthesia stands at around 30% and can be as high as 70% [19]. The figures from our audit stand, therefore, well within accepted limits.
The results of our audit reflect practice in a district general teaching hospital. We have a wide mix of abilities from beginners in anaesthesia to experienced consultants. When a new device is introduced into practice, one would expect a few teething problems. Our insertion rate needs improving and as our experience in using the i-gel increases – at the time of writing we have now used over 7000 devices – we would expect the incidence of failed first time insertion to decrease. As repeated insertions may be linked to complications such as trauma to tissues, nausea, vomiting and sore throat we would expect these to decrease as well. The incidence of leak and repositioning should improve with adherence to the manufacturer’s guidelines as regards selection of the size of the device.
We feel that the i-gel may offer some advantages over conventional laryngeal masks: The lack of inflatable cuff should decrease the incidence of sore throat and other complications that may stem from inflatable cuffs. The thermoplastic elastomer that comprises the cuff of the i-gel may form a better perilaryngeal seal than does the conventional LMA [1, 9]. The gastric channel may enhance the seal, allows decompression of the stomach and allows early detection of gastric aspiration [14].
We feel that the i-gel may have a place not as a replacement for the LMA but as a device in its own right: It could be utilised as a cheap, disposable conduit to facilitate fibreoptic tracheal intubation or as a device for laparoscopic procedures. It has found its way onto resuscitation trolleys in the UK and paramedics are starting to use it as an alternative to the laryngeal mask, principally because of the lack of inflatable cuff and ease of insertion.
Conclusions
The data on our audit of the i-gel compared favourably with data reported for other supraglottic airways in terms of: success rate, ease of insertion and incidence of postoperative complications. Whether the i-gel performs as well as its other supraglottic cousins in all aspects of clinical practice remains to be seen – it is still a relatively new device and numbers of insertion are accordingly small.
Conflict of interest:
Assoc. Prof. Pavel Michalek has lectured for different companies manufacturing airway equipment, including Ambu Ltd., Intersurgical Ltd. and Intavent Orthofix and received reimbursement for his lectures.
Do redakce došlo dne 20. 11. 2011.
Do tisku přijato dne 11. 3. 2012.
Adresa pro korespondenci:
Dr William Donaldson MBBS FRCA, Consultant Anaesthetist
Department of Anaesthesia, Antrim Area Hospital,
Antrim, BT41 2RL, United Kingdom/Northern Ireland
E-mail: willdonaldson@mac.com
Doc. MUDr. Pavel Michálek, PhD DESA
Klinika anesteziologie resuscitace a intenzivní mediciny
1. lékařská fakulta UK a Všeobecná fakultní nemocnice
120 21 Praha 2, Česká republika
E-mail: pavel.michalek@vfn.cz
Zdroje
1. Levitan, R. M., Kinkle, W. C. Initial anatomic investigations of the I-gel airway: a novel supraglottic airway without inflatable cuff. Anaesthesia, 2005, 60, p. 1022–1026.
2. Jackson, K. M., Cook, T. M. Evaluation of four airway training manikins as patient simulators for the insertion of eight types of supraglottic airway devices. Anaesthesia, 2007, 62, p. 388–393.
3. Gabbott, D. A, Beringer, R. The iGEL supraglottic airway: A potential role for resuscitation? Resuscitation, 2007, 73, p. 161–164.
4. Sharma, S., Rogers, R., Popat, M. The i-gel™ airway for ventilation and rescue intubation. Anaesthesia, 2007, 62, p. 419-20.
5. Michalek, P., Hodgkinson, P., Donaldson, W. J. Fiberoptic intubation through an I-Gel supraglottic airway in two patients with predicted difficult airway and intellectual disability. Anesth. Analg., 2008, 106, p. 1501–1504.
6. Campbell, J., Michalek, P., Deighan, M. I-gel supraglottic airway for rescue airway management and as a conduit for tracheal intubation in a patient with acute respiratory failure. Resuscitation, 2009, 80, p. 963.
7. Donaldson, W., Michalek, P. The use of an i-gel supraglottic airway for the airway management of a patient with subglottic stenosis: a case report. Minerva Anestesiol., 2010, 76, p. 369–372.
8. Richez, B., Saltel, L., Banchereau, F., Torrielli, R., Cross, A. M. A new single use supraglottic airway device with a non-inflatable cuff and oesophageal vent: an observational study of the i-Gel. Anesth. Analg., 2008, 106, p. 1137–1139.
9. Gatward, J. J., Cook, T. M., Seller, C., Handel, J., Simpson, T., Vanek, V., Kelly, F. Evaluation of the size 4 i-gel airway in one hundred non-paralyzed patients. Anaesthesia, 2008, 63, p. 1124–1130.
10. Donaldson, W., Abraham, A., Deighan, M., Michalek, P. I-gelTM versus AuraOnceTM laryngeal mask for general anaesthesia with controlled ventilation in paralyzed patients. Biomed. Pap., 2011, 155, p. 155–163.
11. User Guide – i-gel single use supraglottic airway. Wokingham. Intersurgical Ltd, 2006.
12. Verghese, C., Brimacombe, J. R. Survey of laryngeal mask airway usage in 11,910 patients: safety and efficacy for conventional and nonconventional usage. Anesth. Analg., 1996, 82, p. 129–133.
13. Michalek, P., Donaldson, W. J., Hinds, J. D. Tongue trauma associated with the i-gel supraglottic airway. Anaesthesia, 2009, 64, p. 692–693.
14. Gibbison, B., Cook, T. M., Seller, C. Case series: protection from aspiration and failure of protection from aspiration with the i-gel airway. Br. J. Anaesth., 2008, 100, p. 415–417.
15. Brimacombe, J. R., Berry, A. The incidence of aspiration associated with the laryngeal mask airway. A meta-analysis of published literature. J. Clin. Anesth., 1995, 7, p. 297–305.
16. Koay, C. K. A case of aspiration using the Proseal LMA. Anaesth. Intensive Care, 2003, 31, p. 123.
17. McHardy, F. E., Chung, F. Postoperative sore throat: cause, prevention and treatment. Anaesthesia, 1999, 54, p. 444–453.
18. Keijzer, C., Buitelaar, D. R., Efthymiou, K. M., Sramek, M., ten Cate, J., Ronday, M., Stoppa, T., Huitink, J. M., Schutte, P. F. A comparison of postoperative throat and neck complaints after the use of i-gel and the La Premiere disposable laryngeal mask: a double blinded, randomized, controlled trial. Anesth. Analg., 2009, 109, p. 1092–1095.
19. Gan, T. Risk factors for postoperative nausea and vomiting. Anesth. Analg., 2006, 102, p. 1884–1898.
Štítky
Anestéziológia a resuscitácia Intenzívna medicína
Článek Výborová schůze ČSARIMČlánek Stanovy
Článok vyšiel v časopiseAnesteziologie a intenzivní medicína
Najčítanejšie tento týždeň
2012 Číslo 2- DESATORO PRE PRAX: Aktuálne odporúčanie ESPEN pre nutričný manažment u pacientov s COVID-19
- Realita liečby bolesti v paliatívnej starostlivosti v Nemecku
- MUDr. Lenka Klimešová: Multiodborová vizita je kľúč k efektívnejšej perioperačnej liečbe chronickej bolesti
- Metamizol v liečbe pooperačnej bolesti u opioid-tolerantnej pacientky – kazuistika
- e-Konzilium.cz — Masivní plicní embolie při tromboembolické nemoci
-
Všetky články tohto čísla
-
7. Křivánkovy dny
Abstrakta a synopse - Výborová schůze ČSARIM
- Stanovy
- XV. světový kongres anesteziologů
- Nejbližší odborné konference a kongresy
- Implementace imunologických vyšetření do klinické rutinní praxe u kriticky nemocných
- An audit of the i-gel supraglottic airway for general anaesthesia with spontaneous and controlled ventilation – the effect of ventilation mode and operator experience on device performance
- Validation of factors predicting difficult intubation
- Quality of life one year after discharge from the ICU
- Trefoil factor 1 as an indicator of damage of the intestinal mucosa during sepsis in children
- The course of cytokine response in an animal model of intraabdominal sepsis modified by immunosuppression
- A severe course of acquired haemophilia A – case report
-
7. Křivánkovy dny
- Anesteziologie a intenzivní medicína
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Validation of factors predicting difficult intubation
- Quality of life one year after discharge from the ICU
- A severe course of acquired haemophilia A – case report
-
7. Křivánkovy dny
Abstrakta a synopse
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy