-
Články
- Časopisy
- Kurzy
- Témy
- Kongresy
- Videa
- Podcasty
Primary perineal endometriosis – a case report and literature review
Primární perineální endometrióza – kazuistika a přehled literatury
Endometrióza je běžné gynekologické onemocnění způsobené usazením aktivních buněk endometria vně děložní dutiny. Ve většině případů se endometrióza vyskytuje v pánvi, tedy v oblasti vaječníků, Douglasova prostoru nebo uterosakrálního vazu. Ve vzácných případech může mimopánevní endometrióza vzniknout v perineu, močových cestách, gastrointestinálním traktu, nervovém systému, hrudníku, podkoží a kůži. Endometrióza perineaobyvkle vzniká sekundárně po poranění při porodu, např. při laceraci perinea nebo episiotomii. Dosud bylo zaznamenáno jen málo případů spontánní endometriózy perinea. V tomto článku popisujeme vzácný případ spontánní hluboké endometriózy perinea. Pozoruhodné je, že pacientka měla typické symptomy v podobě pravidelné bolesti při menstruaci, a to bez porodu nebo poranění perinea v anamnéze. Po pooperačním podání injekce agonisty hormonu uvolňujícího gonadotropin se pacientka plně uzdravila.
Klíčová slova:
Endometrióza – kazuistika – perineum – primární
Authors: Y. Tian 1; K. Pei 1; J. Bai 1; P. Wang 1,2
Authors place of work: Department of Obstetrics and Gynecology, West China Second University Hospital, Sichuan University, Chengdu, China 1; Key Laboratory of Birth Defects and Related Diseases of Women and Children (Sichuan University), Ministry of Education, Chengdu, China 2
Published in the journal: Ceska Gynekol 2024; 89(1): 40-43
Category: Kazuistika
doi: https://doi.org/10.48095/cccg202440Summary
Endometriosis is a common gynecological disease caused by the implantation of active endometrial cells outside the uterine cavity. In most cases, endometriosis occurs in the pelvic area, such as the ovary, Douglas’ pouch, or uterine sacral ligament. Some rare cases of extrapelvic endometriosis can also occur in the perineum, urinary system, gastrointestinal tract, nervous system, chest, subcutaneous tissue, and skin. Endometriosis of the perineum is usually secondary to obstetric trauma, such as perineal laceration or episiotomy. To date, few cases of spontaneous perineal endometriosis have been reported. Herein, we report a rare case of spontaneous deep perineal endometriosis. Notably, the patient had typical symptoms of regular pain during menstruation with no history of delivery or perineal trauma. The patient recovered well after postoperative gonadotropin releasing hormone agonist injection.
Keywords:
Endometriosis – case report – perineum – primary
Introduction
Endometriosis refers to the presence of endometrial tissue in locations other than the uterine cavity [1]. It is a relatively common disease among women of reproductive age, with an incidence rate of 10–25% [2]. However, extrapelvic endometriosis is relatively rare, thereby accounting for 12% of all endometriosis cases, and perineal endometriosis is even rarer, with an incidence of only 0.3–1% [3]. The first case of perineal endometriosis was reported in 1923; however, since then, there has been limited literature in this area. Perineal endometriosis usually occurs in women with a history of obstetric laceration or episiotomy. The pathogenesis of endometriosis is unclear. However, the most commonly accepted theory of perineal endometriosis is the implantation theory, in which endometrial cells are implanted directly into the perineum from the uterine cavity due to surgery or other trauma [4]. At present, case reports of perineal endometriosis are mostly a result of perineal trauma. In this report, we describe a rare case of non-traumatic perineal endometriosis. The patient had no history of childbirth or perineal trauma, and the pathogenesis could not be explained by the implantation theory.
Case Presentation
A 25-year-old nulliparous woman presented with vaginal pain that was aggravated during her menstrual period. Physical examination revealed a 1.5 - cm painless, solid tubercle, which was palpated in the deep subcutaneous region of the left inferior ramus of the pubis. She had no history of childbirth, perineal trauma, or dysmenorrhea.
After admission, an ultrasound showed a weak echo with a range of 2.8 × 1.1 × 2.0 cm in the subcutaneous muscle layer of the left perineum, which had an unclear boundary, irregular shape, and no obvious blood flow signal detected (Fig. 1). Left perineal muscle layer endometriosis was considered in the ultrasound diagnosis. Serum cancer antigen 125 (CA125) level was 27.2 U/mL.
The patient underwent perineal mass resection. During the operation, a solid nodule was observed in approximately 1.5 cm deep subcutis of the left inferior ramus of the pubis (Fig. 2); this was closely related to the pubis and penetrated the pelvic diaphragm to the lateral rectal space. The mass was approximately 1 × 3 × 2 cm in size, and hard yellow tissue was observed within the mass (Fig. 3, 4).
Intraoperative frozen pathology results showed that the mass was endometriotic tissue. The pathological diag - nosis of postoperative frozen paraffin was also endometriosis (Fig. 5). The patient was discharged on postoperative day four, and was administered gonadotropin releasing hormone agonist (GnRH-a) after the operation. At present, the perineal wound has recovered well after four injections of GnRH-a eight months after the operation.
Fig. 1. Ultrasonic image of the nodule. // Ultrazvukový obraz uzliny. 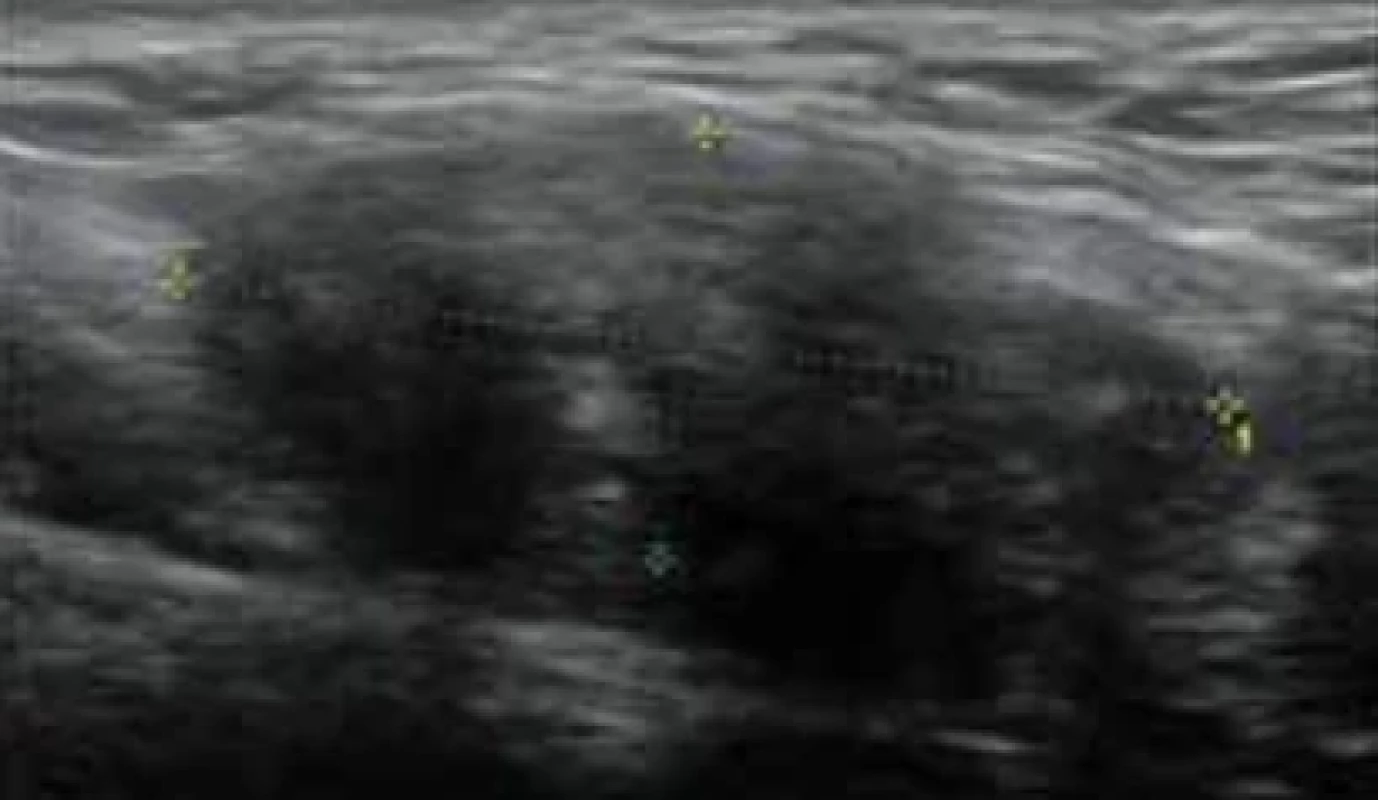
Fig. 2. The solid nodule is located approximately 1.5 cm deep in the subcutis of the left inferior ramus of the pubis. // Pevná uzlina se nachází v asi 1,5 cm hlubokém podkoží levého dolního ramene stydké kosti. 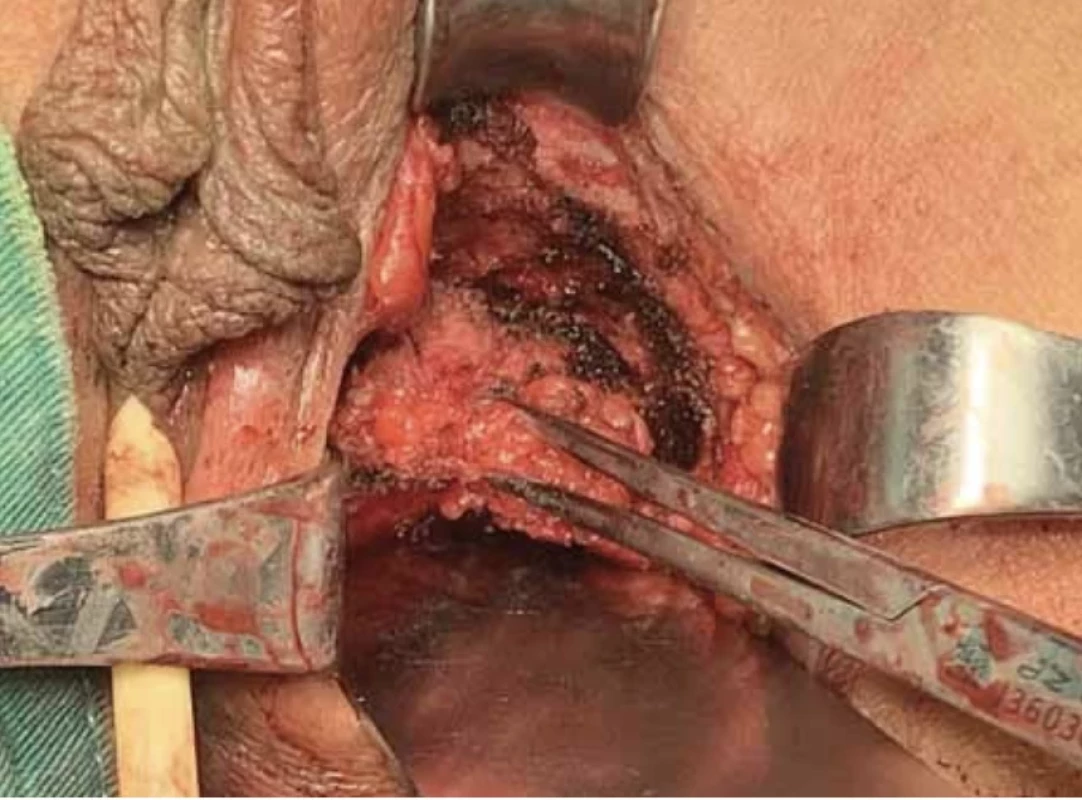
Fig. 3. General image of the nodule. // Obecný obraz uzliny. 
Fig. 4. Cutaway image of the nodule. // Výřezový obraz uzliny. 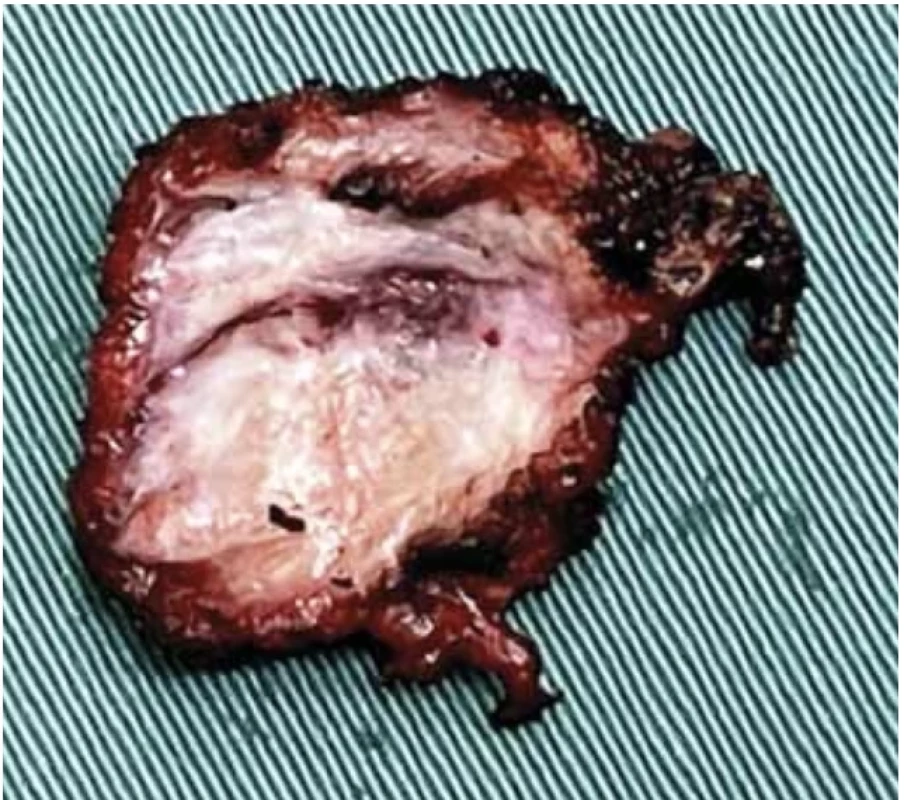
Discussion
According to literature, perineal endometriosis mainly occurs after perineal trauma, usually resulting from a perineal tear or episiotomy during vaginal delivery. Generally, it is considered that the pathogenesis of endometriosis is related with endometrium implantation, coelomic metaplasia, lymphatic metastasis, and vascular metastasis. Because perineal endometriosis is mostly secondary, a primary explanation for the etiology of perineal endometriosis is direct endometriotic implantation in most cases. However, there are few case reports on primary perineal endometriosis [5]. The most likely pathogenesis of this type of endometriosis is lymphatic vascular metastasis. Additionally, multiple factors, such as immune, genetic, and familial factors may be associated with the disease pathogenesis [6]. Perineal endometriosis with a history of perineal trauma often presents as a tender nodule or mass at the perineal lesion, and progressive and cyclic perineal pain; however, primary perineal endometriosis is more difficult to diagnose and requires a more detailed medical and surgical history, as well as a thorough examination.
When it comes to diagnosing perineal endometriosis, we should first perform a detailed gynecological physical examination. Some medical examination such as ultrasonography, magnetic resonance imaging (MRI), tissue biopsy, and some laboratory indicators are also very important for diagnosis. Ultrasonography is the most commonly used and preferred adjuvant examination. It can accurately describe the location and size of the mass in perineal endometriosis. If anal sphincter involvement is considered, endoanal ultrasonography should be performed to determine the extent of a procedure and need for sphincteroplasty [7]. Pelvic MRI has more advantages than other auxiliary examinations, such as ultrasonography, in detecting deep and small masses. Histological examination is the most certain test for a definite diagnosis. The significance of serum CA125 level in the diagnosis of perineal endometriosis is unclear.
Treatment methods for perineal endometriosis includes surgical excision and drug therapy. Complete surgical resection of the lesion is the primary treatment, and adjuvant treatment with hormonal suppressors, such as GnRH-a or oral contraceptives, can reduce the risk of recurrence.
Fig. 5. Histopathological image of the nodule. // Histopatologický obraz uzliny. 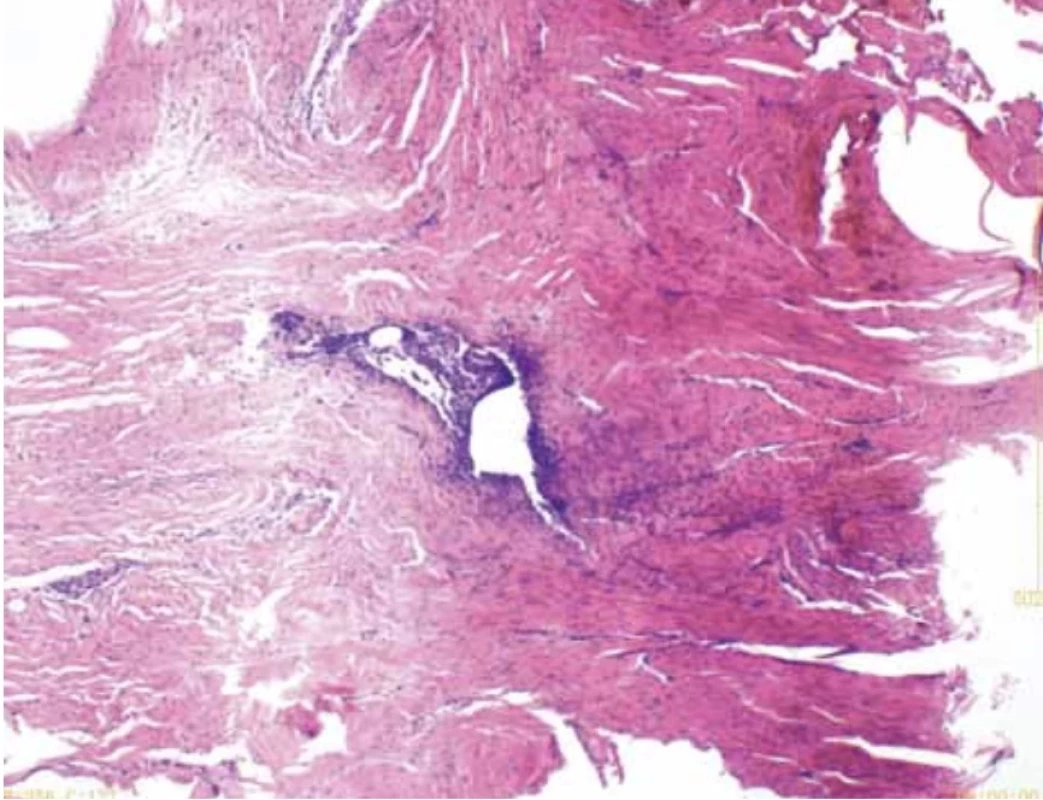
Spontaneous perineal endometriosis is a rare condition. Only a dozen cases have been reported to date, and there are fewer than 10 cases of primary perineal endometriosis. In 2021, Scioscia et al. reported a rare case of primary vulvar endometriosis in a 27-years-old woman. Her lesion was reported in the right mons pubis. An ultrasound-guided percutaneous biopsy was performed, and histological examination confirmed perineal endometriosis [8]. A case of perineal endometriosis without perineal trauma between the left labium major and labium minor was reported by Hamdi et al. in 2015. A firm painless mass was observed in a 23-year-old woman without perineal trauma or sexual intercourse [9]. In 2005, Fulciniti et al. made a retrospective study of 10 cases of cutaneous endometriosis and found one case of primary vulvar endometriosis in a 34-years-old woman [10]. Similarly, in 2020, Yu Liu et al. reported a 27-year-old patient with primary endometriosis in a retrospective study of 35 patients with perineal endometriosis [4]. In 2004, Su et al. reported the youngest case of primary vulvar endometriosis in a 15-year--old patient [11]. In these patients reported in the literature, no recurrences were observed. However, a special case of vulvoperineal endometriosis was reported by Grimstad et al. in 2015. A lesion appeared in her right periclitora, and recurred six years after it was surgically removed [12].
Conclusion
Primary perineal endometriosis is rare and unique. Based on the existing literature, the clinical presentation of primary perineal endometriosis is usually a mass with cyclic perineal pain. Ultrasonography and MRI can be used to assist in the diagnosis, and histological biopsy is the definitive criterion for diagnosis. At present, there are no definite guidelines for the diagnosis and treatment of perineal endometriosis, but the commonly used treatment is surgical treatment of perineal lesions, with or without drug therapy. Most patients have a good prognosis and do not experience recurrence after surgery. Here, we reported a case of primary perineal endometriosis. After surgical resection of the lesion and four injections of GnRH-a, the patient recovered well without recurrence of follow-up so far.
Submitted/Doručeno: 30. 7. 2023
Accepted/Přijato: 1. 9. 2023Ping Wang, MD
Department of Obstetrics and Gynecology
West China Second University Hospital
Sichuan University
No. 20, Section 3
South Renmin Road
Chengdu, Sichuan Province
China
huaxiwangping65@qq.com
Zdroje
1. Matalliotakis M, Matalliotaki C, Zervou MI et al. Abdominal and perineal scar endometriosis: retrospective study on 40 cases. Eur J Obstet Gynecol Reprod Biol 2020; 252 : 225–227. doi: 10.1016/j.ejogrb.2020.06.054.
2. Vellido-Cotelo R, Muñoz-González JL, Oliver - -Pérez MR et al. Endometriosis node in gynecologic scars: a study of 17 patients and the diagnostic considerations in clinical experience in tertiary care center. BMC Womens Health 2015; 15 : 13. doi: 10.1186/s12905-015-0170-9.
3. Dokuzeylül Güngör N, Gürbüz T, Demir MK et al. Endometriosis in an episiotomy scar: case report. TJRMS 2018; 2 (1): 30–34.
4. Liu Y, Pi R, Luo H et al. Characteristics and long-term outcomes of perineal endometriosis: a retrospective study. Medicine 2020; 99 (23): e20638. doi: 10.1097/MD.0000000000020638.
5. Vercellini P, Viganò P, Somigliana E et al. Endometriosis: pathogenesis and treatment. Nat Rev Endocrinol 2014; 10 (5): 261–275. doi: 10.1038/ nrendo.2013.255.
6. Li J, Shi Y, Zhou C et al. Diagnosis and treatment of perineal endometriosis: review of 17 cases. Arch Gynecol Obstet 2015; 292 : 1295–1299. doi: 10.1007/s00404-015-3756-4.
7. Toyonaga T, Matsushima M, Tanaka Y et al. Endoanal ultrasonography in the diagnosis and operative management of perianal endometriosis: report of two cases. Tech Coloproctol 2006; 10 (4): 357–360. doi: 10.1007/s10151-006-0309-7.
8. Scioscia M, Noventa M, Desgro M et al. A rare case of primary vulvar endometriosis: case report and review of the literature. J Obstet Gynaecol 2022; 42 (2): 354–356. doi: 10.1080/01443615.2021.1907559.
9. Hamdi A, Gharsa A, Jaziri D et al. Perineal endometriosis without perineal trauma: a case report. J Clin Exp Dermatol Res 2015; 6 (4): 293. doi: 10.4172/2155-9554.10000293.
10. Fulciniti F, Caleo A, Lepore M et al. Fine needle cytology of endometriosis: experience with 10 cases. Acta Cytol 2005; 49 (5): 495–499. doi: 10.1159/000326194.
11. Su HY, Chen WH, Chen CH. Extra-pelvic endometriosis presenting as a vulvar mass in a teenage girl. Int J Gynaecol Obstet 2004; 87 (3): 252–253. doi: 10.1016/j.ijgo.2004.08.012.
12. Grimstad FW, Carey E. Periclitoral endometriosis: the dilemma of a chronic disease invading a rare location. J Minim Invasive Gynecol 2015; 22 (4): 684–686. doi: 10.1016/ j.jmig.2015.02.002.
Štítky
Detská gynekológia Gynekológia a pôrodníctvo Reprodukčná medicína
Článok vyšiel v časopiseČeská gynekologie
Najčítanejšie tento týždeň
2024 Číslo 1- I „pouhé“ doporučení znamená velkou pomoc. Nasměrujte své pacienty pod křídla Dobrých andělů
- Ne každé mimoděložní těhotenství musí končit salpingektomií
- Gynekologické potíže pomáhá účinně zvládat benzydamin
- Mýty a fakta ohledně doporučení v těhotenství
-
Všetky články tohto čísla
- Předoperační a pooperační staging u karcinomu endometria – prospektivní studie
- Význam vaginální tamponády po laparoskopické sakrokolpopexi – retrospektivní studie
- Diskrepance stagingové a peroperační klasifikace endometriózy pánve dle #Enzian 2021
- Pandemic fear and psychological resilience in pregnant women after the pandemic – a study in Turkey
- Occurrence of acute retrobulbar hemorrhage during birth
- Occult invasive cervical cancer, FIGO stage III, with a negative Pap smear test – clinical presentation and brief review of the literature
- Primary perineal endometriosis – a case report and literature review
- Faktory zvyšující riziko malignity při nálezu endometriálního polypu v ultrazvukovém obraze
- Ženský orgazmus, reprodukce a párové vztahy
- Uterovesical fistula and its treatment in Sub-Saharan Africa
- Pôrodný plán – jeho právne a medicínske implikácie
- Nová doporučení k informování pacientů a dárců gamet v asistované reprodukci
- Diagnostika a léčba endometriózy
- Česká gynekologie
- Archív čísel
- Aktuálne číslo
- Informácie o časopise
Najčítanejšie v tomto čísle- Faktory zvyšující riziko malignity při nálezu endometriálního polypu v ultrazvukovém obraze
- Diagnostika a léčba endometriózy
- Význam vaginální tamponády po laparoskopické sakrokolpopexi – retrospektivní studie
- Ženský orgazmus, reprodukce a párové vztahy
Prihlásenie#ADS_BOTTOM_SCRIPTS#Zabudnuté hesloZadajte e-mailovú adresu, s ktorou ste vytvárali účet. Budú Vám na ňu zasielané informácie k nastaveniu nového hesla.
- Časopisy



